Abstract
Purpose
This study aimed to evaluate the cost-effectiveness of statins for primary prevention of stroke and myocardial infarction (MI) in the elderly in Singapore.
Methods
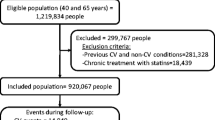
A Markov model was developed to investigate the lifetime costs, quality-adjusted life years (QALYs) and incremental cost-effectiveness ratios (ICERs) of statin treatment in those aged 65 years and older without a history of stroke or MI from the perspective of Singapore’s healthcare system, using elderly-specific clinical data and local costs from hospital databases. A lifetime horizon was used and all costs and health outcomes were discounted at 3 % annually.
Results
In the base-case analysis, statin treatment prevented an additional four strokes and eight MIs among 1,000 “healthy” elderly individuals compared with no treatment. Statin treatment resulted in a QALY gain of 0.26 and additional costs of SGD 11,314 per person, yielding an ICER of SGD 43,925 (USD 33,495) per QALY gained. The results were sensitive to statin effectiveness, particularly statins’ effect on all-cause mortality, and cost of statin medication. Probabilistic sensitivity analysis demonstrated that the probability of statin treatment being cost-effective was 72 % at a willingness-to-pay threshold of SGD 65,000 (USD 49,546) per QALY gained. Shortening the time horizon from lifetime to 10 years (simulating limited life expectancy) considerably increased the ICER to SGD 291,313 (USD 167,171) per QALY. Female gender and younger age were also associated with higher ICERs owing to a lower baseline risk of cardiovascular disease (CVD) and higher costs to manage events in these subgroups.
Conclusions
Statin treatment for the primary prevention of CVD in the elderly was cost-effective. However, treatment warrants re-evaluation when the prognosis of the individual is considered less than ten years; other goals may take precedence over CVD prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality and morbidity globally [1]. Evidence from randomized, controlled trials supports a net benefit from statin treatment in individuals with CVD to reduce the risks of cardiovascular events and mortality (secondary prevention) [2]. There is also evidence of benefit in primary prevention; statins have been shown to reduce the risk of stroke and myocardial infarction (MI) in people without established CVD [3–5]. In light of this evidence, the 2013 American College of Cardiology/American Heart Association (ACC/AHA) guidelines recommended the use of statins for primary prevention of CVD in people aged 45 to 75 years with ≥ 5 % ten-year risk of CVD, hyperlipidemia or diabetes [6]. An estimated 920 million people fall within these categories globally and the actual figure is likely to be higher, considering the growing prevalence of cardiovascular risk factors worldwide [7].
The expanded scope for statin treatment has cost implications. Previous studies that examined the cost-effectiveness of statin treatment in the setting of primary CVD prevention have yielded conflicting data and conclusions [8–10]. Furthermore, none of these focused on the elderly (≥65 years old) where age-related factors could alter the risk-benefit ratio of preventive treatment with statins. In the United States, the elderly constitute 14 % of the population and this figure is projected to increase to 20 % by 2030 [11]. Over this period, the average life expectancy is expected to soar further, having increased from 75 to 79 years in the last decade [12]. This trend is prevalent worldwide, including Singapore that has one of the fastest ageing populations. Given the limited life span of the elderly, it is unclear whether they derive similar benefits from statin treatment for cardiovascular prevention and whether the cost of treatment can be justified in these individuals. This study therefore aimed to investigate the lifetime benefits and costs of statin treatment for primary prevention of CVD focusing on the elderly, using decision modelling techniques.
Methods
Model Structure
A Markov state-transition model was developed to compare statin treatment and no treatment for the primary prevention of CVD over a lifetime horizon (Fig. 1). The base case was a hypothetical cohort of 65-year-old patients without a history of stroke or MI. All individuals, who entered the model in a healthy state, could experience an acute stroke or MI that could be non-fatal or fatal, or death arising from events that were unrelated to a vascular cause (all-cause death). Survivors from stroke or MI could then progress to a convalescent phase where they remain disabled (i.e., post stroke or post MI states) or die as a result of stroke, MI or unrelated reasons. Individuals in the statin treatment arm were assumed to continue statin treatment indefinitely. Those on statin treatment who experienced adverse effects such as myopathy and rhabdomyolysis were assumed to stop taking statins permanently and progress through the model thereafter in a similar manner as those in the non-statin treatment arm. As the intention of the study was designed for the purpose of primary prevention, a second cardiovascular event was not simulated and all patients were assumed to receive optimal secondary prevention following an incident vascular event. A cycle length of 1 year and a lifetime horizon with a maximum of 35 years were used. The analysis was conducted from the perspective of Singapore’s healthcare system. All costs and health outcomes were discounted at 3 % annually, and half-cycle correction was applied. The model development and analyses were performed using TreeAge Pro Suite 2013 (TreeAge Software, Inc., Williamstown, MA). Model parameters, including base-case values, ranges and references are shown in Table 1.
Markov model structure. All individuals enter the model in the healthy state and can transition to any of the other health states in a given cycle year: Stroke, Myocardial infarction (MI), All-cause death, Myopathy* or Rhabdomyolysis* (*only for those in the statin treatment arm). Stroke or MI survivors progress to post event states
Clinical Inputs
The baseline probabilities of stroke and MI were derived from real-world epidemiological data collected by the National Registry of Diseases Office of Singapore (Fig. 2a to d). They were allowed to change over time to reflect increasing risk for CVD with age. The baseline probabilities of all-cause death were obtained from the 2013 life tables for the Singaporean population (which were generally lower than that in the United Kingdom or United States) (Supplementary Table) [13–15]. These rates were adjusted as the cohort aged over the time horizon of the analysis. A two-fold increased risk of death, based on standardised mortality ratios reported in long-term follow-up studies of first-ever patients with stroke or MI, was applied to the general mortality rates from the life tables to reflect the higher mortality burden following a vascular event (i.e., post stroke or post MI) [16, 17].
Incidence and fatality rates of stroke and MI. a Incidence rates of stroke; b Incidence rates of MI; c Fatality rates of stroke; d Fatality rates of MI. These statistics were obtained from National Registry of Diseases Office in Singapore over the period from 2008 to 2012 and stratified by age and gender
Statin treatment benefits were modelled by applying the relative risk reductions (RRR) for stroke, MI and all-cause mortality to the baseline probabilities described above. These RRRs were derived from our systematic review and meta-analysis of statins for primary CVD prevention in the elderly. To account for non-adherence that is prevalent in real-life clinical setting especially among the elderly, we applied a 50 % non-compliance rate based on reported figures in the literature [18]. Non-compliance was modelled by decreasing the efficacy of statins in reducing the risk of stroke, MI and all-cause mortality and assuming a RRR of 1. The non-compliance factor was assumed to remain constant over time in the absence of long-term data reporting real-world statin non-compliance rates over the time horizon of the analysis. The excess risks for myopathy and rhabdomyolysis – the most common adverse effects associated with statin treatment - were drawn from a review of muscular effects of statins in the elderly [19] and a systematic review of cohort studies and clinical trials that evaluated statins safety [20]. These risks were varied in sensitivity analyses over their 95 % confidence intervals.
Utility Inputs
Utility values range from 1 (perfect health) to 0 (death) and describe the quality of life for different health states according to individuals’ preferences. They are subsequently combined with life expectancy to generate quality-adjusted life years (QALYs). The utilities for stroke and MI health states were obtained from population-based studies including the elderly that assessed health-related quality of life using the European Quality of Life-5 Dimensions instrument [21, 22]. The utility estimates were representative of the health states for the entire cycle in which the event took place. Both stroke and MI were associated with significant impairment in quality of life, with the estimates for stroke (0.64) being lower than that for MI (0.74) indicating lower quality of life. An improvement in utility was observed after the first year for stroke patients (0.70). The utilities for myopathy and rhabdomyolysis were based on clinical judgment and sourced from published cost-effectiveness analyses of statin treatment for primary prevention [23, 24]. A small disutility of 0.001 was included to reflect the decrease in quality of life from the inconveniences of having to take a statin pill daily (clinical assumption) [9, 23]. Utilities were varied across their 95 % confidence intervals in sensitivity analyses.
Cost Inputs
Only direct medical costs (i.e., costs of treatment and complications) were used in the analysis, in accordance with the model’s perspective. Indirect costs representing the loss of productivity were excluded. All cost estimates were obtained from a local tertiary care hospital using 2013 data. Costs were calculated in 2013 Singapore dollars (SGD) (1 SGD = 0.76225 USD, updated December 2014).
Costs of Statin Treatment
The costs associated with statin treatment included costs for medication, associated doctor visits and laboratory tests (lipid panel), based on four visits in a year. The cost of statin treatment was weighted by the average utilization of different statins based on doctors’ prescribing practices locally. The most frequently prescribed statins for this patient population in Singapore were atorvastatin, followed by simvastatin and rosuvastatin. Patients on statin treatment who developed myopathy incurred the cost of an additional doctor visit and creatine kinase test. Patients who developed rhabdomyolysis were assumed to require emergency room visits, doctor consultations, ten-day hospitalization and associated laboratory tests [25, 26]. The estimated costs were varied widely (50 % in each direction for statins cost and 25 % for other cost inputs) in sensitivity analyses to account for variations across countries.
Costs of Cardiovascular Events
The costs associated with cardiovascular events were separated into costs for the first and subsequent years to account for significantly higher costs in the former. The costs incurred during the first year of a stroke or MI comprised emergency room visits, doctor consultations, hospitalizations, procedures (such as percutaneous transluminal coronary angioplasty (PTCA), coronary artery bypass graft for a MI patient), investigations (angiography, chest radiography, echocardiography, electrocardiography (ECG)) and laboratory tests. Among these costs, cardiac procedures contributed to a significant portion for MI management during the first year. Rehabilitation contributed to most of the costs for stroke management during the first year. One-third of stroke survivors required rehabilitation centre stay based on our retrospective analysis of 2013 hospital data for stroke patients. Their median length of stay was 29 days according to a local population study [27]. These costs were stratified by age to take into account treatment variations due to age-associated differences in patients’ clinical characteristics. In the subsequent years following an event, the costs included medication costs, follow-up outpatient visits and laboratory tests, assuming four visits in a year.
Main Outcome Measures
The main outcome measures were the additional number of stroke or MI events prevented, lifetime costs, QALYs gained, and the incremental cost-effectiveness ratios (ICERs). The ICER is a ratio of incremental healthcare costs to incremental QALYs gained and expressed in terms of cost per QALY gained. It is typically compared against a cost-effectiveness threshold that reflects willingness-to-pay (WTP). We used a pre-defined threshold of SGD 65,000 or USD 49,546 (one gross domestic product per capita in Singapore in 2013, as recommended by the World Health Organization) [28, 29]. An ICER below this WTP threshold implies the treatment is cost-effective.
Subgroup Analyses
We conducted additional analyses for other cohorts, namely, males and females at age 65, 75 or 85 years old, over a lifetime or 10 years’ time horizon (simulating limited life expectancy), to investigate the impact of gender, age and time horizon/life expectancy on the cost-effectiveness of statin treatment. These factors were defined a priori as they have been reported to influence the results based on published literature [9]. We adjusted the baseline probabilities of stroke, MI and all-cause deaths according to gender and age; females and younger elderly had lower baseline risks of stroke and MI (Fig. 2). We did not account for gender or age differences in statin treatment effects as available evidence suggests they do not differ between males and females; furthermore, clinical trial data that is stratified by these age groups is sparse [30]. Gender-specific utility values were used to take into account that females tended to have lower utility scores, possibly explained by their higher expectations for recovery, or worse coping or adaptation strategies [31].
Sensitivity Analyses
All model inputs were varied in sensitivity analyses. A Tornado diagram was used to assess the effect of varying the parameters on the ICERs. Probabilistic sensitivity analysis (PSA), using 10,000 Monte Carlo simulations, was conducted to evaluate how the simultaneous uncertainties about model inputs might influence outcomes. The results were presented as a cost-effectiveness acceptability curve that showed the probability that statin treatment is considered cost-effective for various WTP thresholds.
Results
Base-Case Analysis
Statin treatment prevented an additional four strokes and eight MIs among 1,000 65-year-old healthy elderly individuals over a lifetime (Table 2). Treatment was associated with additional mean costs of SGD 11,314 and a mean QALY gain of 0.26 per person. The cost difference was attributable to the cost of statin medication (SGD 399 per person annually, for 35 years), which was partially compensated for by fewer strokes or MIs in the statin treatment arm. The ICER was SGD 43,925 (USD 33,495) per QALY gained for statin treatment compared with no treatment over a lifetime (Table 3).
Subgroup Analyses
Gender Differences
Female gender was associated with higher ICERs. In a 65-year-old male, statin treatment was associated with additional mean costs of SGD 10,210 and a mean QALY gain of 0.28 over a lifetime, yielding an ICER of SGD 36,633 (USD 27,935) per QALY gained compared with no treatment (Table 3). A 65-year-old female incurred higher additional mean costs of SGD 12,380, along with a lower mean QALY gain of 0.24, correspondingly yielding a higher ICER of SGD 52,534 (USD 40,060) per QALY gained (Table 3).
Age Differences
Higher ICERs were observed in the younger than older elderly even when the time horizon was fixed at 10 years for both age groups. The incremental costs were higher while the incremental QALYs gained were lower in the younger elderly; both of these factors significantly increased the ICER associated with the younger elderly and led to a wide disparity in ICERs between the two age groups over the same time horizon [SGD 219,313 (USD 167,237) vs SGD 28,846 (USD 21,997) per QALY gained, respectively] (Table 4).
Time Horizon/ Life Expectancy
Regardless of age or gender, the ICERs were higher when the time horizon was shortened to 10 years. Statin treatment was associated with (high) ICERs of SGD 219,313 (USD 167,237) and SGD 67,353 (USD 51,360) per QALY gained compared with no treatment in a 65-year-old and 75-year-old, respectively, with remaining 10 years’ life expectancy, and not considered to be cost-effective (Table 4).
Sensitivity Analyses
One-way sensitivity analyses showed that the results were sensitive to assumptions on statin effectiveness (i.e., RRRs for all-cause mortality, MI and stroke, in this order) and cost of statin medication (Fig. 3). The ICER increased from SGD 43,925 (USD 33,495) to SGD 134,031 (USD 102,047) per QALY gained if we assumed no benefit on all-cause death (RR = 1.03, based on upper limit of 95 % CI as per the meta-analysis). The ICERs increased to SGD 65,529 (USD 49,892) and SGD 62,168 (USD 47,333) per QALY gained when we assumed no benefit from statin treatment on MI (RR = 0.92) and stroke (RR = 1.05), respectively. Varying the cost of statin medication by +/− 50 % affected the ICER by SGD 9,752 in either direction. The results were insensitive to variations in risks of myopathy or rhabdomyolysis, utilities and costs of managing events. In all, the ICERs remained below the cost-effectiveness threshold of SGD 65,000 per QALY gained across the range of values and scenarios tested for all model input parameters except for RRR for all-cause mortality. PSA showed that the probability that statin treatment is cost-effective at the pre-defined WTP threshold of SGD 65,000 per QALY gained was 72 % over a lifetime horizon (Fig. 4).
Discussion
This analysis, to our knowledge, is the first to report explicitly the long-term cost-effectiveness of statin treatment for primary CVD prevention using data on treatment effectiveness, utilities and costs that are drawn specifically from the elderly population in an Asian country. Statin treatment was found to be cost-effective for the primary prevention of CVD in the elderly over their lifetime. The ICER of SGD 43,925 (USD 33,495) per QALY gained compared with no treatment was below the pre-defined WTP threshold of SGD 65,000 per QALY gained.
Female gender was associated with higher ICERs. This could be explained by their lower baseline risks of stroke or MI that resulted in (i) fewer events prevented (i.e., lower incremental QALYs gained; females: 0.15–0.24; males: 0.16–0.28) and (ii) less cost savings from fewer events prevented to offset the costs of statin treatment (i.e., higher incremental costs; females: SGD 4,490–12,380; males: SGD 4,021–10,210); both of which contributed to a larger ICER. The ICERs ranged between SGD 30,031 (USD 22,865) and 52,534 (USD 39,998) per QALY gained in females which, although higher than in the males, were below the WTP threshold.
Younger age was associated with higher ICERs compared with older age (65 versus 85 years). The lower baseline risks of CVD in the younger elderly partially accounted for the higher ICER. Added to this were the higher costs of managing events such as MI in the younger elderly whereas an older elderly may be excluded from certain surgical procedures in consideration of their frailty and comorbidities. Our cost analysis revealed that it cost on average twice as much to treat MIs in the 65-year-olds compared with 85-year-olds (SGD 20,292 vs SGD 11,951, respectively). This was attributed to a higher number of cardiac procedures – which accounted for a significant proportion of MI costs – being performed in the younger age group whereas the older age group may not be suitable to undergo a procedure such as PTCA due to reasons such as delayed presentation or abnormal ECG [32, 33]. Both factors contributed to a less favourable ICER in the younger elderly. The ICERs ranged between SGD 36,633 (USD 27,891) – 52,534 (USD 39.998) per QALY in the younger elderly which, although higher than in the older elderly, remained below the WTP threshold.
A shorter time horizon of ten years (compared with lifetime) was associated with considerably higher ICERs. The ICERs of SGD 219,313 (USD 167,237) and SGD 67,353 (USD 51,360) per QALY gained for statin treatment compared with no treatment in a 65 and 75-year-old, respectively, with remaining ten years’ life expectancy, was above the WTP threshold. Extrapolating this further signalled even less favourable cost-effectiveness results when life expectancy is reduced further, particularly at younger ages and in the females (both of these factors were associated with higher ICERs). This suggested that one should consider the life expectancy of the individual when determining whether statin treatment will offer value for money.
Our results were sensitive to the effectiveness (in particular RRR for all-cause mortality) and cost of statin treatment. If statins were less effective or cost of statins was increased above the current estimated annual cost of SGD 399, the ICER would increase above SGD 43,925 (USD 33,495) per QALY and become less favourable. Nonetheless, the price of statins has dropped substantially in recent years and is expected to continue to decrease, with more generics entering the market - a trend which is expected to improve the cost-effectiveness of statins. Statin’s lack of proven benefit in reducing all-cause mortality accounted for the high variability in results depending on the RRR estimate for all-cause mortality used in the model. Our results were otherwise robust to reasonable variation of other parameters during the one-way sensitivity analyses. PSA suggested that the collective uncertainty around model inputs did not threaten the validity of the results for the effect of statin compared with no statin.
Comparison with Published Studies
Our findings were consistent with published studies of statins’ cost-effectiveness in the U.S. and European healthcare setting. An earlier study of low-cost statin treatment (USD 48 per annum) for primary prevention in the U.S. population between 35 to 84 years of age was conducted by Lazar et al. over a lifetime horizon [8]. They concluded that statin treatment was cost-effective for primary prevention in most persons based on a willingness-to-pay of USD 50,000 per QALY. They reported an ICER of USD 37,000 per QALY gained to treat all individuals with at least two risk factors and at 0-10 % ten-year risk of developing CVD. One key difference was that we applied elderly-specific data whereas Lazar et al. used constant utilities and costs for the entire population (i.e., did not distinguish between middle age and elderly).
Another study by Greving et al. reported a different conclusion that statin treatment was not cost-effective for low-risk primary prevention populations (5 % ten-year risk) despite assuming a lower cost of statin at € 9 per annum [9]. This study was conducted among people aged 45 to 75 years in the Netherlands. The ICERs ranged from € 75,237 and € 99,857 per QALY gained, for a 65 year-old male and female, respectively. It is noteworthy that (i) a 10 year time horizon was used and (ii) a non-compliance rate of 67–94 % was applied; these likely accounted for the discrepancy in conclusions drawn between the two studies. Like Greving et al., we incorporated non-compliance and similarly found statin treatment not to be cost-effective in our subgroup analysis with a 10 year time horizon. This highlights the importance to take the time horizon of the analysis into consideration when interpreting the results of these cost-effectiveness analyses.
Strengths
A key strength of our study is that we adopted elderly-specific data for key model parameters, including treatment effect of statins, cost of statin medication, costs and utilities associated with MI and stroke management in the elderly. The treatment effect of statins was derived from a meta-analysis of seven trials of atorvastatin, fluvastatin, pravastatin, rosuvastatin and simvastatin that included elderly subjects from 65 up to 92 years old [34–40]. These RRRs were comparable with that reported in other meta-analyses on statins for primary prevention in adults, which generally favoured statin use. We also modelled treatment non-compliance that is prevalent in this population by decreasing statin efficacy. Real-world costs of statins, according to their average utilization within the local hospital, were used. Other cost inputs were also based on analyses of local hospital databases and stratified by age (65 and 85 years) whereas other models [8–10] grouped older patients together as a single age group, which may obscure important age-associated differences in costs. We also differentiated cardiovascular events into non-fatal and fatal events to capture important differences in associated utilities and costs. We included the healthcare costs of statin-associated adverse events such as myopathy and rhabdomyolysis, though these events were rare enough to have a negligible effect on the ICERs. Although some literature has suggested that statins may have higher risks of adverse effects at older ages [19], adverse effects were found to be weak drivers of cost-effectiveness in our analysis; they need to be very common or very severe to influence the results. We also applied utility estimates elicited from the elderly population and chose a lifetime time horizon for the base-case analysis to ensure the full effects of prevention were captured.
Limitations
Several limitations of our analysis should be acknowledged. First, the treatment effects of statins were assumed to persist beyond the follow-up trial period over the lifetime horizon. This assumption is common in cost-effectiveness models and may be reasonable since patients continue to receive treatment at the end of trial follow-up. The treatment effects were also based on trials conducted primarily in western populations and it remains unknown whether they can be generalised to the Asian population. Second, we did not model the detailed course of patients after their initial events. Instead, we used mean estimates of survival, utility and costs after cardiovascular events and applied optimal secondary prevention to all patients. Our study therefore pertained only to primary prevention. Third, the model did not capture all of the possible beneficial and adverse effects of statins. We did not model the effect of statins on liver disease, renal disease, cancer or dementia because the data supporting such effects were not as strong or conclusive as the data for the main outcomes of interest modelled. Doing so may decrease the cost-effectiveness of statins.
Conclusions
In all, our analysis suggested that statins are a cost-effective intervention in the elderly in the Singapore healthcare setting and supported the recommendations of the ACC/AHA guidelines for the use of statins in primary CVD prevention. Expanded use of statins for primary prevention to include the elderly population is, however, expected to increase overall healthcare costs. Statin treatment may warrant re-evaluation when the prognosis of the individual is considered less than 10 years; other goals may take precedence over CVD prevention.
References
Yusuf S, Reddy S, Ounpuu S, et al. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104:2746–53.
Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–81.
Taylor F, Ward K, Moore TH, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2011; CD004816.
Brugts JJ, Yetgin T, Hoeks SE, et al. The benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: meta-analysis of randomised controlled trials. BMJ (Clin Res ed). 2009;338:b2376.
Mihaylova B, Emberson J, Blackwell L, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–90.
Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American college of cardiology/american heart association task force on practice guidelines. J Am Coll Cardiol. 2014;63:2889–934.
Ioannidis JA. More than a billion people taking statins? Potential implications of the new cardiovascular guidelines. JAMA: J Am Med Assoc. 2014;311:463–4.
Lazar LD, Pletcher MJ, Coxson PG, et al. Cost-effectiveness of statin therapy for primary prevention in a low-cost statin era. Circulation. 2011;124:146–53.
Greving JP, Visseren FL, de Wit GA, et al. Statin treatment for primary prevention of vascular disease: whom to treat? Cost-effectiveness analysis. BMJ (Clin Res ed). 2011;342:d1672.
Ward S, Lloyd Jones M, Pandor A, et al. A systematic review and economic evaluation of statins for the prevention of coronary events. Health Technol Assess. 2007;11:178.
The State of Aging and Health in America 2013. In: Centers for Disease Control and Prevention UDoHaHS, ed. Atlanta, GA, 2013.
Health at a Glance 2013. OECD Indicators. OECD Publishing, 2013.
Department of Statistics, Singapore. Complete life tables 2008–2013 for Singapore Resident Population. Available at: http://www.singstat.gov.sg/publications/publications_and_papers/births_and_deaths/lifetable08-13.pdf. Last accessed 1 December 2014.
Office for National Statistics, United Kingdom. National life tables 2011–2013. Available at: http://www.ons.gov.uk/ons/taxonomy/index.html?nscl=Life+Tables#tab-data-tables. Last accessed 1 December 2014.
Arias E. United States life tables, 2010, National vital statistics reports, vol. 7. 63rd ed. Hyattsville: National Center for Health Statistics; 2014.
Brønnum-Hansen H, Davidsen M, Thorvaldsen P, et al. Long-term survival and causes of death after stroke. Stroke. 2001;32(9):2131–6. September 1, 2001.
Smolina K, Wright FL, Rayner M, et al. Long-term survival and recurrence after acute myocardial infarction in England, 2004 to 2010. Circ: Cardiovasc Qual Outcomes. 2012;5(4):532–40. July 1, 2012.
Ellis JJ, Erickson SR, Stevenson JG, et al. Suboptimal statin adherence and discontinuation in primary and secondary prevention populations. J Gen Intern Med. 2004;19(6):638–45.
Bhardwaj S, Selvarajah S, Schneider EB. Muscular effects of statins in the elderly female: a review. Clin Interv Aging. 2013;8:47–59.
Law M, Rudnicka AR. Statin safety: a systematic review. Am J Cardiol. 2006;97:52C–60C.
Luengo-Fernandez R, Gray AM, Bull L, et al. Quality of life after TIA and stroke: ten-year results of the Oxford vascular study. Neurology. 2013;81:1588–95.
Xie J, Wu EQ, Zheng Z-J, et al. Patient-reported health status in coronary heart disease in the United States: age, sex, racial, and ethnic differences. Circulation. 2008;118:491–7.
Pignone M, Earnshaw S, Tice JA, et al. Aspirin, statins, or both drugs for the primary prevention of coronary heart disease events in men: a cost-utility analysis. Ann Intern Med. 2006;144:326–36.
Pletcher MJ, Lazar L, Bibbins-Domingo K, et al. Comparing impact and cost-effectiveness of primary prevention strategies for lipid-lowering. Ann Intern Med. 2009;150:243–54.
Schreiber DH, Anderson TR. Statin-induced rhabdomyolysis. J Emerg Med. 2006;31:177–80.
Skrabal MZ, Stading JA, Cannella CA, et al. Two cases of rhabdomyolysis associated with high-dose simvastatin. Am J Health Syst Pharm: AJHP: Off J Am Soc Health Syst Pharm. 2003;60:578–81.
Tan WS, Heng BH, Chua KS, et al. Factors predicting inpatient rehabilitation length of stay of acute stroke patients in Singapore. Arch Phys Med Rehabil. 2009;90:1202–7.
Department of Statistics, Singapore. Latest data on GDP per capita. Available at: http://www.singstat.gov.sg/statistics/latest_data.html#1. Last accessed 1 September 2014.
Sachs JD. Macroeconomics and Health: Investing in Health for Economic Development. Report of the Commision on Macroeconomics and Health. Geneva, Switzerland: World Health Organisation, 2011. Available at: http://whqlibdoc.who.int/publications/2001/924154550x.pdf. Accessed on 1 September 2014.
Kostis WJ, Cheng JQ, Dobrzynski JM, et al. Meta-analysis of statin effects in women versus men. J Am Coll Cardiol. 2012;59:572–82.
Bushnell CD, Reeves MJ, Zhao X, et al. Sex differences in quality of life after ischemic stroke. Neurology. 2014;82:922–31.
Alexander KP, Newby LK, Armstrong PW, et al. Acute coronary care in the elderly, part II: ST-segment–elevation myocardial infarction: a scientific statement for healthcare professionals from the American heart association council on clinical cardiology: in collaboration with the society of geriatric cardiology. Circulation. 2007;115:2570–89.
Mehta RH, Rathore SS, Radford MJ, et al. Acute myocardial infarction in the elderly: differences by age. J Am Coll Cardiol. 2001;38:736–41.
Collier DJ, Poulter NR, Dahlof B, et al. Impact of atorvastatin among older and younger patients in the Anglo-Scandinavian cardiac outcomes trial lipid-lowering arm. J Hypertens. 2011;29:592–9.
Bruckert E, Lievre M, Giral P, et al. Short-term efficacy and safety of extended-release fluvastatin in a large cohort of elderly patients. Am J Geriatr Cardiol. 2003;12:225–31.
Neil HA, DeMicco DA, Luo D, et al. Analysis of efficacy and safety in patients aged 65–75 years at randomization: collaborative atorvastatin diabetes study (CARDS). Diabetes Care. 2006;29:2378–84.
Collins R, Armitage J, Parish S, et al. MRC/BHF heart protection study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet. 2003;361:2005–16.
Glynn RJ, Koenig W, Nordestgaard BG, et al. Rosuvastatin for primary prevention in older persons with elevated C-reactive protein and low to average low-density lipoprotein cholesterol levels: exploratory analysis of a randomized trial. Ann Intern Med. 2010;152:488–96. W174.
Nakaya N, Mizuno K, Ohashi Y, et al. Low-dose pravastatin and age-related differences in risk factors for cardiovascular disease in hypercholesterolaemic Japanese: analysis of the management of elevated cholesterol in the primary prevention group of adult Japanese (MEGA study). Drugs Aging. 2011;28:681–92.
Shepherd J, Blauw GJ, Murphy MB, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360:1623–30.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Relationships with Industry: None
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 27 kb)
Rights and permissions
About this article
Cite this article
Lin, L., Teng, M., Zhao, Y.J. et al. Long-term Cost-effectiveness of Statin Treatment for Primary Prevention of Cardiovascular Disease in the Elderly. Cardiovasc Drugs Ther 29, 187–197 (2015). https://doi.org/10.1007/s10557-015-6584-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-015-6584-7