Abstract
Purpose
Secretory phospholipase A2 group IIA (sPLA2−IIA) concentration and activity are associated with increased risk of cardiovascular events in acute coronary syndrome (ACS) patients. This study evaluated baseline differences in sPLA2-IIA concentration and other inflammatory markers in ACS patients with and without diabetes, and the inflammatory biomarker response to selective sPLA2 inhibition.
Methods
The effects of the sPLA2 inhibitor varespladib methyl 500 mg daily and placebo on serial changes in inflammatory and lipid biomarkers were examined in 624 ACS patients who were treated with standard of care including atorvastatin 80 mg daily.
Results
Compared with non-diabetic patients, diabetic patients had higher baseline concentrations of sPLA2-IIA (p = 0.0066), hs-CRP (p = 0.0155), and IL-6 (p = 0.009). At 8 weeks of treatment (primary endpoint), varespladib methyl reduced median sPLA2-IIA levels by -83.6% in diabetic patients and by −82.4% in non-diabetic patients (p = 0.33). Median hs-CRP and IL-6 levels were reduced in both varespladib methyl-treated diabetic and non-diabetic patients, but these differences were not statistically significantly different at 8 weeks (p = 0.57 and p = 0.97 respectively).
Conclusions
Varespladib significantly reduces the post-ACS inflammatory response in those with and without diabetes. These responses were greater in diabetic subjects compared to non-diabetic subjects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Low-grade inflammation has been implicated in the pathogenesis of rupture-prone atherosclerotic lesions, which are more common in patients with diabetes than without diabetes [1–4]. High levels of high-sensitivity C-reactive protein (hs-CRP), a non-specific systemic inflammatory marker, are associated with higher risk of cardiovascular events in type 2 diabetes; [5, 6] however, elevated hs-CRP levels do not differentiate risk in ACS patients with and without diabetes [7, 8].
Secretory phospholipase A2 (sPLA2) represents a family of isoenzymes that contribute directly and indirectly to atherosclerosis [9]. The culprit coronary atherosclerotic lesions of patients presenting with acute myocardial infarction contain sPLA2 group IIA (sPLA2-IIA), which is detected both intracellularly in intimal macrophages and vascular smooth muscle cells and in extracellular deposits [10]. High sPLA2-IIA levels and increased sPLA2 activity identify ACS patients with increased cardiovascular events and all-cause mortality [11–16].
We hypothesized that ACS patients with diabetes have higher levels of sPLA2-IIA and other inflammatory markers than non-diabetic patients, and that they would have an enhanced anti-inflammatory response to selective sPLA2 inhibition with varespladib methyl. This hypothesis was tested by performing a sub-group analysis of the data from the Fewer Recurrent Acute Coronary events with Near-term Cardiovascular Inflammation Suppression (FRANCIS) trial [17].
Methods
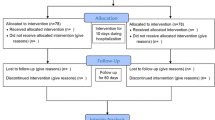
The design of FRANCIS (NCT00455546) has been reported previously [17]. Briefly, 624 patients with ACS were randomized and treated with varespladib methyl (500 mg daily) or placebo within 96 h of a qualifying ACS event and were followed for a minimum of 6 months. All patients were treated with atorvastatin 80 mg daily. The primary endpoint of FRANCIS was the change in LDL cholesterol after 8 weeks of therapy. All patients provided written informed consent and the study protocol was approved by local and national ethics committees.
hs-CRP levels (Quest Diagnostics, Van Nuys, CA USA), sPLA2-IIA concentration (Cayman Chemical, Ann Arbor, Michigan, USA with modification by CLASS Laboratories, University of Michigan, Ann Arbor, Michigan, USA), and IL-6 levels (R&D Systems, Inc., Minneapolis, MN, USA) were measured as described previously [17].
Statistical analyses
Due to non-normality, changes in sPLA2-IIA, hs-CRP, and IL-6 concentrations were analyzed on natural log-transformed data using an ANCOVA model with baseline value as a covariate and factors for treatment group and country. The dependent variable was the difference of the logarithm of the follow-up value and the logarithm of the baseline value.
For each of the inflammatory biomarkers (sPLA2-IIA, hs-CRP, and IL-6), baseline values were split into groups above and below the median. A logistic regression model was then fitted for each of these 3 two-level variables using a stepwise selection procedure from the following variables: diabetes, age, gender, type of index event (unstable angina/STEMI versus STEMI), body mass index, country, baseline LDL cholesterol level, baseline triglyceride level, history of hypertension, MI, angina, metabolic syndrome, hyperlipidemia, and smoking status (current versus former/never).
SAS software version 9.1.3 (SAS Institute, Inc., Cary, NC, USA) was used to perform the data analysis.
Results
Of the 624 patients enrolled in the trial who received study drug, 171 (27.4%) had diabetes at baseline. The clinical features of patients with and without diabetes in the varespladib methyl and placebo groups are listed in Table 1. Patients with diabetes, compared to those without, were slightly older and more likely to be female; they were more likely to have hypertension and the metabolic syndrome.
As shown in Table 2, patients with diabetes had higher baseline median levels of sPLA2-IIA (306 pmol/L (IQR: 249) vs. 231 pmol/L (IQR: 196), p = 0.0066), IL-6 (6.03 ng/L (11.69) vs. 4.79 ng/L (7.70), p = 0.009), hs-CRP (10.2 mg/L (40.2) vs. 8.0 mg/L (24.9), p = 0.0155). In a multivariate model, the presence of diabetes was a statistically independent predictor of baseline sPLA2-IIA level (p = 0.019) and IL-6 level (p = 0.011), and of borderline statistical significance as a predictor of hs-CRP level (p = 0.055).
The effects of varespladib methyl compared to placebo on levels of sPLA2, hs-CRP, and IL-6 from baseline to the end of treatment at 24 weeks are shown in Figs. 1, 2, and 3, respectively. By 2 weeks, sPLA2-IIA levels were reduced by 80-85% in varespladib methyl-treated patients either with or without diabetes, and these differences persisted throughout the trial (Fig. 1). At 8 weeks of treatment (primary endpoint), varespladib methyl treatment reduced median sPLA2-IIA levels by −83.6% in diabetic patients and by −82.4% in non-diabetic patients; these changes were not statistically different (p = 0.33).
Effects of varespladib methyl 500 mg daily and placebo on concentrations of secretory phospholipase A2 groups IIA (sPLA2-IIA) at various times in the trial. The p-values represent differences in sPLA2-IIA concentrations between diabetic and non-diabetic subgroups who were treated with either placebo (solid lines) or varespladib methyl (dashed lines)
Effects of varespladib methyl 500 mg daily and placebo on concentrations of hs-CRP at various times in the trial. The p-values represent differences in hs-CRP concentrations between diabetic and non-diabetic subgroups who were treated with either placebo (solid lines) or varespladib methyl (dashed lines)
Effects of varespladib methyl 500 mg daily and placebo on concentrations of interleukin-6 (IL-6) at various times in the trial. The p-values represent differences in IL-6 concentrations between diabetic and non-diabetic subgroups who were treated with either placebo (solid lines) or varespladib methyl (dashed lines)
Among patients with diabetes, hs-CRP levels decreased more with varespladib methyl treatment compared to placebo at 2 (−58.8% vs. −11.0%, p = 0.0004), 4 (−83.0% vs −51.1%, p = 0.0013), 8 (−82.8% vs. −67.6%, p = 0.0299), 16 (−83.6% vs. −72.4%, p = 0.078), and 24 weeks (−89.5% vs. −76.1%, p = 0.031, Fig. 2). In patients without diabetes, varespladib methyl treatment was associated with lower hs-CRP levels only at 16 weeks (−81.1%, vs. −71.1% p = 0.012). At 8 weeks (primary endpoint), changes in hs-CRP in varespladib methyl-treated patients with and without diabetes were not statistically different (p = 0.57).
Similarly, in diabetic patients, the IL-6 reduction with varespladib methyl compared to placebo was statistically significant at weeks 2 (−21.8% vs. +3.5%, p = 0.0019) and 4 (−47.1% vs. −23.9%, p = 0.026) but dissipated thereafter (Fig. 3). There was no varespladib methyl effect on IL-6 in patients without diabetes. At 8 weeks, differences in IL-6 levels in varespladib methyl-treated patients with and without diabetes were not statistically different (p = 0.97).
Associations between baseline glucose values and inflammatory makers were more pronounced in diabetic than non-diabetic patients. In patients with diabetes, the correlations between inflammatory markers and glucose were: sPLA2-IIA r = 0.15, p = 0.06; hs-CRP r = 0.23, p = 0.003; and IL-6 r = 0.17, p = 0.03. In patients without diabetes, the correlations between inflammatory markers and glucose were: sPLA2-IIA r = 0.10, p = 0.03; hs-CRP r = 0.14, p = 0.004; and IL-6 r = 0.09, p = 0.07.
The trial was not powered to detect a significant treatment effect on clinical events. Major adverse cardiovascular events (unstable angina, non-fatal myocardial infarction, non-fatal stroke and death) occurred in 15 of 171 patients with diabetes (8.8%). In patients with diabetes, the overall event rate was 9.5% (8 of 84) in the varespladib–treated patients and 8.0% (7 of 87) in placebo-treated patients. In patients without diabetes, the overall event rate was lower at 7.1% (32 of 453) with a rate of 6.6% (15 of 229) in varespladib-treated patients and 7.6% (17 of 224) in placebo-treated patients.
Among patients with diabetes, treatment-emergent adverse events occurred in 66 (79%) of the varespladib-treated patients and 67 (77%) of the placebo-treated patients as previously reported (17). Corresponding numbers in patients without diabetes were 154 (67%) and 169 (75%). Two patients with diabetes who were treated with varespladib methyl (2.4%) and 4 treated with placebo (4.6%) withdrew due to an adverse event.
Discussion
These results indicate that after an ACS event, patients with diabetes have higher levels of sPLA2-IIA, IL-6, and hs-CRP compared with patients without diabetes. Higher sPLA2 concentration and activity have been linked to worse outcomes after an ACS [11–16], and the risk associated with an elevated IL-6 concentration (>10 ng/mL) was even higher in patients with diabetes [7].
The risk of a recurrent event is highest in the early period post-ACS, but declines over the ensuing weeks in parallel with the decline in CRP levels [18–21]. In the Myocardial Ischemia Reduction with Acute Cholesterol Lowering (MIRACL) trial [16], neither baseline sPLA2-IIA concentration nor sPLA2 activity was associated with recurrent cardiovascular events. However, treatment-related reductions in sPLA2 concentration and activity were significantly less in subjects who had an ischemic event compared to those who did not have an event.
sPLA2 isoenzymes are expressed in arterial smooth muscle cells and hepatocytes [9]. The hydrolysis of phospholipids from cell membranes generates arachidonic acid and lysophospholipids that work in association with other bioactive lipids produced from oxidized lipoproteins to activate inflammatory pathways in various cells in the vessel wall such as tumor necrosis factor-alpha, interleukin-1 beta, and interleukin-6, which in turn induce hepatic and myocardial CRP production [22–24].
FRANCIS (NCT00743925) is a recently completed phase 2 trial that was designed to examine the effects of varespladib methyl on inflammatory biomarkers in 624 patients with ACS who were treated with atorvastatin 80 mg daily [17]. Overall, treatment with varespladib methyl 500 mg daily was accompanied by significant reductions in levels of the inflammatory biomarkers sPLA2-IIA and hs-CRP but not with a statistically significant reduction in IL-6. In this analysis of FRANCIS patients with diabetes, treatment with varespladib methyl, an inhibitor of groups IIA, V, and X sPLA2 isoenzymes suppressed elevated levels of sPLA2-IIA, IL-6 and hs-CRP throughout the follow-up period. As compared with IL-6, changes in hs-CRP with varespladib methyl treatment showed a more treatment consistent effect in the diabetic group, which is probably due to less analytical variability of this measure [25]. For these reasons, hs-CRP has been considered a more useful biomarker of inflammatory activity. Although we postulated an enhanced anti-inflammatory response to varespladib methyl in ACS patients with diabetes, 8-week differences in these biomarkers were not statistically different from non-diabetes patients.
Consistent with established associations between glycemic status and transcriptional activation of inflammatory pathways in the arterial wall of patients with diabetes [1, 4, 26], we report higher correlations between baseline glucose concentrations and the inflammatory markers in patients with diabetes than in patients without diabetes.
Conclusions
Varespladib methyl significantly reduced the post-ACS inflammatory response in patients with and without diabetes [17]; however, this subgroup analysis indicates that the anti-inflammatory effect was limited to patients with diabetes. Further corroboration of the differences in the anti-inflammatory effects of varespladib methyl in diabetic and non-diabetic patients requires further investigation in the larger VISTA-16 trial [27].
The association between glycemic status and inflammation is consistent with established pathways documenting increased transcriptional pro-inflammatory activation in patients with poorly controlled diabetes. Thus, it might be anticipated that the anti-inflammatory effect of sPLA2 inhibition might be greater in patients with more advanced and poorly controlled diabetes. Although we did not demonstrate larger changes in circulating inflammatory biomarkers with varespladib methyl treatment, this trial does not preclude the possibility of a larger anti-inflammatory effect in the vessel wall of patients with diabetes. The potential effects of these biomarker changes in varespladib methyl-treated ACS patients with diabetes will require investigation in an event-driven clinical trial.
References
Burke AP, Kolodgie FD, Zieske A, et al. Morphologic findings of coronary atherosclerotic plaques in diabetics: a postmortem study. Arterioscler Thromb Vasc Biol. 2004;24:1266–71.
Silva JA, Escobar A, Collins TJ, Ramee SR, White CJ. Unstable angina: a comparison of angioscopic findings between diabetic and nondiabetic patients. Circulation. 1995;92:1731–6.
Nasu K, Tsuchikane E, Katoh O, et al. Plaque Characterization by virtual histology intravascular ultrasound analysis in type 2 diabetic patients. Heart. 2008;94:429–33.
Cipollone F, Iezzi A, Fazia M, et al. The receptor RAGE as a progression factor amplifying arachidonate-dependent inflammatory and proteolytic response in human atherosclerotic plaques: role of glycemic control. Circulation. 2003;108:1070–7.
Soinio M, Laasko M, Lehto S, Ronnemaa T. High-sensitivity C-reactive protein and coronary heart disease mortality in patients with type 2 diabetes. Diabetes Care. 2006;29:329–33.
Schulz M, Rimm E, Li T, Rifai N. C-reactive protein and incident cardiovascular events among men with diabetes. Diabetes Care. 2004;27:889–94.
James SK, Lindahl B, Timmer JR, et al. Usefulness of biomarkers for predicting long-term mortality in patients with diabetes mellitus and non-ST-elevation acute coronary syndromes (a GUSTO IV substudy). Am J Cardiol. 2006;97:167–72.
Biasucci LM. Liuzzo ‘g, Della Bona R, et al. Different apparent prognostic value of hsCRP in type 2 diabetic and nondiabetic patients with acute coronary syndromes. Clin Chem. 2009;55:365–8.
Rosenson RS, Gelb MH. Secretory phospholipase A2: a multifaceted family of proatherogenic enzymes. Curr Cardiol Rep. 2009;11:445–51.
Nijmeijer R, Meuwissen M, Krijnen PAJ, et al. Secretory type II phospholipase A2 in culprit coronary lesions is associated with myocardial infarction. Eur J Clin Invest. 2008;38:205–10.
Kugiyama K, Ota Y, Sugiyama S, et al. Prognostic value of plasma levels of secretory type II phospholipase A2 in patients with unstable angina pectoris. Am J Cardiol. 2000;86:718–22.
Porela P, Pulkki K, Voipio-Pulkki LM, et al. Level of circulating phospholipase A2 in prediction of the prognosis of patients with suspected myocardial infarction. Basic Res Cardiol. 2000;29:413–7.
Mallat Z, Steg PG, Benessiano J, et al. Circulating secretory phospholipase A2 activity predicts recurrent events in patients with severe acute coronary syndromes. J Am Coll Cardiol. 2005;46:1249–57.
Hartford M, Wiklund O, Mattsson Hultén L, et al. CRP, Interleukin-6, Secretory phospholipase A2 group IIA, and intercellular adhesion molecule-1 during the early phase of acute coronary syndromes and long-term follow-up. Int J Cardiol. 2006;108:55–62.
Simon T, Benessiano J, Mary-Krause M, et al. Impact of circulating secretory phospholipase A2 (sPLA2) and lipoprotein-associated phospholipase A2 (Lp-PLA2) activities on 6 months survival, recurrent AMI, and incident stroke in patients with AMI. Eur Heart J. 2008;29:195.
Ryu SK, Mallat Z, Schwartz GG, et al. The effect of high dose statin therapy on lipoprotein-associated and secretory phospholipase A2 mass and activity and ischemic events in patients with acute coronary syndromes. J Am Coll Cardiol. 2010;55:A165.E1546.
Rosenson RS, Hislop C, Elliott M, et al. Effects of varespladib methyl on biomarkers and major cardiovascular events in acute coronary syndrome patients. J Am Coll Cardiol. 2010;56:1079–88.
Kinlay S, Schwartz GG, Olsson AG, et al. High-dose atorvastatin enhances the decline in inflammatory markers in patients with acute coronary syndromes in the MIRACL study. Circulation. 2003;108:1560–6.
Ridker PM, Morrow DA, Rose LM, et al. Relative efficacy of atorvastatin 80 mg and pravastatin 40 mg in achieving the dual goals of low-density lipoprotein cholesterol <70 mg/dl and C-reactive protein <2 mg/l: an analysis of the PROVE-IT TIMI-22 trial. J Am Coll Cardiol. 2005;45:1644–8.
Ridker PM, Cannon CP, Morrow D, et al. Pravastatin or atorvastatin evaluation and infection therapy-thrombolysis in myocardial infarction 22 (PROVE IT-TIMI 22) investigators. C-reactive protein levels and outcomes after statin therapy. N Engl J Med. 2005;352:20–8.
Morrow DA, de Lemos JA, Sabatine MS, et al. Clinical relevance of C-reactive protein during follow-up of patients with acute coronary syndromes in the Aggrastat-to-Zocor trial. Circulation. 2006;114:281–8.
Baeuerle PA, Henkel T. Function and activation of NF-kappa B in the immune system. Annu Rev Immunol. 1994;12:141–79.
Thomas G, Bertrand F, Saunier B. The differential regulation of group II(A) and group V low molecular weight phospholipases A(2) in cultured rat astrocytes. J Biol Chem. 2000;275:10876–86.
Thommesen L, Sjursen W, Gåsvik K, et al. Selective inhibitors of cytosolic or secretory phospholipase A2 block TNF-induced activation of transcription factor nuclear factor-kappa B and expression of ICAM-1. J Immunol. 1998;161:3421–30.
Smith Jr SC, Anderson JL, Cannon RO, Yazid F, Koenig W, Libby P, et al. CDC/AHA workshop on inflammatory markers and cardiovascular disease: application to clinical and public health practice report from the clinical practice discussion group. Circulation. 2004;110:e550–3.
Moreno PR, Murcia AM, Palacios IF, et al. Coronary composition and macrophage infiltration in atherectomy specimens from patients with diabetes mellitus. Circulation. 2000;102:2180–4.
Rosenson RS. After FRANCIS: next steps in the clinical evaluation of varespladib methyl. Future Cardiol. 2011;7:11–8.
Conflicts of interest
Drs. Fraser and Hislop are employees of Anthera Pharmaceuticals and they have ownership interest in Anthera Pharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosenson, R.S., Fraser, H., Goulder, M.A. et al. Anti-Inflammatory Effects of Varespladib Methyl in Diabetic Patients with Acute Coronary Syndrome. Cardiovasc Drugs Ther 25, 539–544 (2011). https://doi.org/10.1007/s10557-011-6344-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-011-6344-2