Abstract
Background
It is not clear whether the correction of anemia with erythropoietin (rhuEpo) in patients with chronic kidney disease (CKD) has any benefit on cardiac function and geometry. Most studies are based on indices of systolic function and left ventricular mass (LVM) and the results are conflicting.
Patients and methods
We sought to investigate the effect of rhuEpo on LV systolic and diastolic performance using conventional and novel echocardiographic indices. Thirty one patients with CKD (stage 3 or 4) were included. Fifteen patients (group I) treated with rhuEpo targeting at Hb ≥13.0 g/dL, while the remaining (group II) were not treated. Clinical and laboratory parameters were recorded at baseline and 1 year later. Ejection fraction (EF) and LVM were carefully determined. Diastolic function was assessed by mitral inflow indices (E and A wave velocities, Edt deceleration time and E/A) and novel indices of mitral annulus motion using Tissue Doppler Imaging (Em, Am, and E/Em). An index of global cardiac function (Tei) was also calculated.
Results
At baseline, the 2 groups had comparable clinical and laboratory characteristics. After 1 year, a significant improvement in Hb levels (13.6 ± 1.2 vs 10.3 ± 1.2 g/dL, p < 0.05) as well as in systolic and diastolic function indexes was observed in group I compared to group II patients: EF (70.5 ± 7.6 vs 63.4 ± 9.3%, p < 0.05), LVM (116.5 ± 34.9 vs 155.6 ± 51.6 g/m2, p < 0.05), Edt (233.9 ± 98.6 vs 166.9 ± 45.1 ms, p < 0.05), Tei index (0.35 ± 0.12 vs 0.51 ± 0.17, p < 0.01) and E/Em (9.7 ± 2.4 vs 14.8 ± 5.2, p < 0.05), respectively. Blood pressure and heart rate did not show significant changes.
Conclusions
Correction of anemia with rhuEpo in patients with CKD seems to improve cardiac performance and geometry.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cardiovascular disease is the main cause of morbidity and mortality in patients with chronic kidney disease (CKD) not yet requiring dialysis as well as in those on chronic renal replacement therapy [1–3]. Prominent features of cardiovascular involvement in CKD patients (stages 2–5) are left ventricular hypertrophy (LVH) and dysfunction [4–6]. LVH is recognized as a powerful independent predictor of death and morbidity in CKD patients, along with anemia, hypertension, malnutrition, hyperparathyroidism and an elevated calcium x phosphorus product [7–10].
Chronic anemia, usually observed when creatinine clearance decreases below 40 ml/min (CKD stage 3 or 4), may adversely affect cardiovascular function inducing a long-term hyperdynamic circulatory state with increased cardiac output leading to LVH [6, 11, 12]. Therefore, therapies that can reverse the development of LVH among patients with CKD (stage 2–4) may help to reduce the increased cardiovascular risk.
It has been suggested that the correction of renal anemia using recombinant human erythropoietin (rhuEpo) could be associated with an improvement of cardiac function and a reduction of LV mass. However, the effect of long-term administration of rhuEpo on cardiac structure and performance in predialysis patients has not been well studied while some inconsistent results have been published in the literature [13–19]. Moreover, no study to date has investigated the effect of such a treatment on LV diastolic function.
We therefore sought to investigate the effects of long-term rhuEpo treatment on cardiac function (systolic and diastolic) and structure in CKD patients (stage 3 or 4) in a nested sub-study performed in the framework of our recently published prospective randomized clinical study [20].
2 Patients and methods
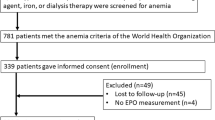
Thirty one predialysis patients recruited from our center (17 males) aged 64.3 ± 19.5 (range 35–81) years, out of 88 CKD patients who were enrolled in our published multicenter prospective randomized clinical study [20] were included in this study. Inclusion criteria were: CKD stage 3 or 4 [creatinine clearance 30–59, 15–29, respectively] (creatinine clearance was estimated using the Cockroft–Gault formula [21]), age >18 years, Hb <12 g/dL, no apparent heart disease and patients who had not previously received rhuEpo treatments. Patients with arrhythmias, angina, myocardial infarction, cerebrovascular disease, uncontrolled hypertension, hepatic insufficiency, active hepatitis, uncontrolled hypothyroidism, chronic alcoholism, congestive heart failure (New York Heart Association class III or IV), severe obesity (body mass index >40 kg/m2), diabetes mellitus, systemic diseases, infections or inflammatory conditions that might inhibit the effect of rhuEpo had been excluded from the study.
The causes of primary kidney disease of the patients were: glomerulonephritis 5, urolithiasis 1, polycystic kidney disease 4 and unknown 21.
Monitoring of arterial blood pressure and treatment of hypertension was performed according to established standards, aiming at blood pressure levels ≤135/85 mm Hg whenever possible, using restricted salt intake, and appropriate drug therapy (avoiding drugs that inhibit the renin–angiotensin axis), at the discretion of the treating clinician. Protein intake was generally restricted to less than 1 g/kg/day based on appropriate dietary instructions given to the patients. The patients who received rhuEpo, also received oral iron supplements (100 mg of element iron /day) to maintain ferritin levels of ≥150 μg/L and a transferring saturation index ≥20%. Intravenous iron was not used. All patients were followed in the CKD outpatients clinic of the University Hospital of Ioannina, Greece. Written informed consent was obtained from all patients prior to participation in the study and the Hospital’s Ethics Committee approved the study protocol. Randomization was done using a computerized sequence kept at the coordinating center at the University of Ioannina, Greece.
2.1 Study design
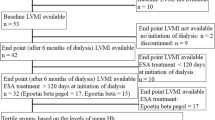
Patients were randomized in one to one fashion to each treatment group between November 2000 and February 2002. Fifteen patients (group I) were received rhuEPO-alpha at a dose of 50 U/kg subcutaneously, once per week targeting at Hb levels 13 g/dL. For patients exceeding this target the dose of rhuEpo was down-titrated to 25 U/kg/week, or remained the same according to the discretion of the clinician. The others (group II) were not treated with rhuEpo until decrease of Hb levels below 9 g/dL.
In November 2002, the indication of subcutaneous rhuEPO-alpha administration in chronic renal failure patients was withdrawn because pure red-cell aplasia cases were reported [22]. Although no such adverse events had been recorded in any of the enrolled patients in our study, all patients were notified of this modification and subcutaneous rhuEPO-alpha was discontinued. Patients could then use an alternative form of rhuEPO (e.g. subcutaneous rhuEPO beta or darbepoietin) at the discretion of their treating physicians. The study was terminated 1 year after the recruitment of the last patient.
2.2 Clinical and laboratory characteristics
Patients were seen at baseline and consequently monthly on an outpatient basis. The mean values of clinical and laboratory characteristics of the patients at baseline and after 12 months are presented in Table 1. Resting blood pressure and heart rate were obtained using standard methods. Blood samples were obtained after overnight fasting and the following laboratory parameters were recorded: Hb levels, serum creatinine, calcium (Ca+2), phosphorus, intact parathormone, albumin (ALB), and the lipid profile [Total cholesterol (T-chol), HDL-cholesterol (HDL-chol), Triglycerides (TG)]. LDL cholesterol (LDL-chol)] was calculated by the Friedewald equation [23].
The Hb values were determined by an automatic hematological analyzer (Coulter Counter). Serum creatinine and sCa+2 were assessed by photometric methods (Olympus AV 600, Olympus, USA), while sALB was measured by a photometric BCG method (Olympus AV 600, Olympus, USA). Intact parathormone was measured by a chemiluminescent immunoassay (Immulite 200, Diagnostica products, Los Angeles, CA, USA). Concentrations of T-chol and TG were determined enzymatically using an Olympus AV 600 clinical chemistry analyzer (Olympus Diagnostica, Hamburg, Germany). Our laboratory is currently participating in the Murex Clinical Chemistry Quality Assessment Programme. The coefficient of variation values in this program in the past 2 years ranged between 0.99 and 2.44% for cholesterol and between 1.73 and 3.36% for TG. HDL-chol was determined by a direct assay (Olympus Diagnostica, Hamburg, Germany).
2.3 Echocardiographic measurements
An echocardiographic examination was performed at baseline and after 12 months using a cardiac ultrasound unit (HD1 5000, Philips, USA) with a 2–3.5 MHz transducer in the M-mode and in the Doppler bidimensional model. Moreover, Tissue Doppler Imaging (TDI) was performed in all patients. The same experienced operator performed all the echocardiographic studies being unaware of each patient’s treatment.
All recordings and measurements were performed in accordance with the recommendations of the American Society of Echocardiography [24] using the average value of three measurements. The echocardiographic window used was obtained in the 3–4 intercostal space with the patient in the 30-degree decubitus position.
-
M-mode measurements
Using the M-mode technique we assessed the following parameters: end-diastolic diameter of the left ventricular chamber, the inter-ventricular septum thickness and the thickness of the left ventricular posterior wall. Care was taken to avoid misalignment and angulation in obtaining measurements. Left ventricular mass was calculated from end-diastolic LV dimensions using the formula of Devereux et al [25]. The LV mass was adjusted for body surface area and expressed as LV mass index. The LV ejection fraction was determined by 2D echocardiography using the modified biplane Simpson’s method.
-
Doppler measurements
The diastolic filling of LV (LV inflow) was examined using Doppler echocardiography. The peak velocity of early diastolic filling (E) and the peak velocity of atrial filling (A) were recorded and the E to A ratio (E/A) was calculated. The deceleration time of the E wave (DcT) was also measured. The index of global cardiac function Tei index, was also calculated using mitral inflow and ejection time assessed by conventional Doppler echocardiography [26].
-
TDI measurements
Tissue Doppler Imaging (TDI) was also used to assess LV diastolic function. Pulse-wave diastolic velocities (early, Em; late, Am) were obtained from the apical 4-chamber view at the septal position of the mitral annulus. Gain settings were adjusted carefully, and the direction of longitudinal motion was aligned with the scan line direction. Signals were obtained from 3 end-expiratory cycles, and averages were made for the diastolic velocities.
2.3.1 Statistical analysis
All analyses are based on intention-to-treat. Comparisons of discrete and continuous variables between groups were performed by the chi-square test with continuity correction and the t-test, respectively.
All data were analyzed using the SPSS 11.5 software (SPSS, Inc., Chicago, IL). All p-values are two-tailed. A p value <0.05 was considered statistically significant.
3 Results
3.1 Clinical parameters
The baseline clinical parameters were similar between the 2 groups (Table 1). No statistical significant difference was observed in body surface area, body weight and systolic and/ or diastolic blood pressure (Table 1).
3.2 Laboratory parameters
The Hb values at baseline were similar between the two groups. At the end of the 12-month study period patients treated with rhuEpo (n = 14, 1 patient had died due to myocardial infarction) had increased Hb levels while in the group II patients (n = 13, 1 patient died due to myocardial infarction, and 2 due to septic shock) remained almost unchanged (Table 1). No patient in group II required erythropoietin administration according to our prespecified criteria (Hb <9 g/dl).
Moreover, the renal function as estimated by creatinine clearance remained unchanged in patients treated with rhuEpo, while a statistically significant reduction was noticed in group II patients (p < 0.05) (Table 1). We did not observe any significant differences with the exception of HDL-chol (Table 1).
3.3 Echocardiography
At the end of the follow-up period an improvement in cardiac performance was demonstrated in patients treated with rhuEpo. Specifically:
-
M-mode parameters
We observed a statistically significant reduction in left ventricular mass (LVM) index (p < 0.01) accompanied by an increase of left ventricular ejection fraction (LVEF) (p < 0.01) in group I patients (Table 2). In group II patients we observed an increase of LVM while the LVEF remained almost unchanged (Table 2). These changes showed a statistically significant difference between the 2 groups (Table 2).
-
Doppler parameters
We did not observe any significant alterations in conventional Doppler parameters in group I patients (Table 2). On the other hand, a significant increase of E and E/A, and a decrease in DT parameter was evident in untreated patients (Table 2). A significant difference in the values of E, A, DT between the 2 groups was evident (Table 2).
-
TDI parameters
The assessment of diastolic LV performance using novel techniques (TDI) disclosed some remarkable changes. Particularly, we observed an increase in Em/Am ratio in group I patients while in group II the E/Em ratio was increased (Table 2). Statistically significant differences between the 2 groups were noted in the Em/Am, and in the E/Em ratio (Table 2).
-
Tei index
Finally, an improvement of global (systolic and diastolic) cardiac function, as assessed by the Tei intex, was demonstrated in group I patients (Table 2).
4 Discussion
In the present study, we observed a significant decrease of LVM and an improvement of systolic and diastolic cardiac performance in patients with CKD stage 3 or 4 who were treated with rhuEpo. To the best of our knowledge, no study to date has examined modern echocardiographic indexes evaluating both systolic and diastolic LV function in this setting. Moreover, in this population a decline of renal function was evident in patients who did not receive rhuEpo.
Renal anemia, uremia, secondary hyperparathyreoidism and other factors favor promote the development of LVH [27, 28]. Moreover, renal anemia correlates significant with the LVM in dialysis patients [28] and the relative risk of LVH is increased (duplicated) for every 1 g/dL decrease of Hb level [29]. Although there is evidence for the association between Hb levels and LVM in CKD, the underlying causality has been questioned [18].
Our results support the findings of previous studies evaluating patients with CKD stage 3 or 4. In these studies mean decrease of LVM was 14–42 g/m2 the reported at 12–month and at least 6-month follow-up periods [13, 14, 16]; thus our finding of a mean decrease in LVM of 27 g/m2 after 12 months of rhuEpo therapy are in agreement with the above mentioned studies. Furthermore, a recent study showed that treatment with rhuEpo can prevent further progression of LVH in CKD patients with mild to moderate anemia [17]. On the other hand, another study of patients with CKD stage 3 or 4 did not show a significant change of LVM over 2 years using rhuEpo, although there appeared to be a decrease in LVM in the subgroup with LVH at study entry [15]. In this context, 2 further studies failed to demonstrate that correction of anemia with Epo ameliorates or delays LVH in this setting [18, 19]. Different study designs and populations may account for these disparities. Importantly, 2 recent randomized controlled trials failed to show that complete correction of anemia favours better clinical cardiovascular outcomes [19, 30]. Increased blood pressure, thrombosis, vasoconstriction, blood viscocity, ventricular afterload, and oxidative stress have been proposed as potential mechanisms for this apparent paradox and might offset the benefits of improved myocardial and peripheral oxygenation [31]. However, it should be acknowledged that a considerable proportion of patients in these studies had a history of heart failure while the underlying etiology and the ejection fraction (EF) were not reported. Thus, it is believed that the findings are inconsistent and point to the need for adequately powered clinical outcome trials [32].
On the other hand, the mechanisms of improvement of left ventricular performance after rhuEpo administration are not clear. Erythropoietin is increasingly recognized as an agent with favourable pleiotropic effects on the cardiovascular system, apart from erythropoiesis [33–35]. Several direct beneficial effects of rhuEpo have been proposed, including inhibition of myocardial cell apoptosis and favorable cardiac remodeling [36], phosphatidylinositol 3’-kinase (P13k)/Akt-mediated protection of cultured myocytes from hypoxia-induced apoptosis [37] and improved left ventricular function and decreased apoptosis following ischemia/reperfusion (I/R) injury in the myocardium [38, 39]. Another operating mechanism could be the increased neovascularization leading to increased capillary density [40]. The value of this mechanism in improving LV performance has been recently demonstrated in a rat model of post-myocardial infarction heart failure [41].
Patients with anemia seem to have normal conventional indices of diastolic function because of a pseudo-normalization phenomenon which is a result of increased preload. TDI has been demonstrated to provide relevant additive information about left ventricular systolic and diastolic performance. Most importantly, mitral annular velocities derived form TDI seem to be less load dependent than conventional mitral inflow variables [42]. In addition, it has been shown that the ratio of the peak early diastolic mitral inflow velocity over the peak early diastolic annulus velocity (E/Em) allow an accurate estimation of filling pressures in different subsets of patients [43].
Tei index combines systolic and diastolic time intervals and it has been demonstrated to predict the prognosis of patients with idiopathic dilated cardiomyopathy and cardiac amyloidosis [26, 44]. Thus, these newer cardiac markers (Tei index and E/Em ratio) are stronger predictors of future cardiac events than conventional parameters of systolic and diastolic cardiac performance [45].
Our population had no evidence of heart failure with conventional parameters, but the E/Em ration (≥10) was consistent with diastolic dysfunction, whereas the Tei index (>0.35) indicated a global cardiac (systolic and diastolic) impairment. Our results showed that the administration of rhuEpo retarded the progression of heart failure as expressed by the E/Em and Tei indices, while in patients not treated a progression of cardiac dysfunction was noted.
It could be therefore concluded that correction the renal anemia, along with control of blood pressure and volume status, might favourably affect cardiac geometry and structure as well as systolic/diastolic function in patients with advanced CKD.
The correction of renal anemia using rhuEpo may have benefits that extend beyond the effects on LVH and cardiac function. Small studies demonstrated benefits of Hb normalization on sleep [46], exercise capacity and well being [47, 48] and quality of life [49] in dialysis patients. Moreover, the use of rhuEpo in predialysis patients (CKD stage 3 or 4) has been reported to be associated with favourable effects on serum creatinine and creatinine clearance in randomized control studies [20, 49]. Potential mechanisms of preserved renal function include the correction hypoxia of tubular cells, and the attenuation of apoptotic processes [20].
Our results are in agreement with the above mentioned studies; although two recent studies showed that the progression of renal failure was not retarded in patients treated with rhuEpo [15, 16]. This disagreement is possibly due to the inclusion of a significant number of subjects with diabetes mellitus in the latter studies.
Finally, we observed a significant increase in the HDL cholesterol levels in the treated group. This favourable antiatherogenic effect could be attributed to the anti-inflammatory activity of rhuEpo as well as to the improvement in tissue oxygenation owing to correction of anemia [50].
4.1 Limitations
We believe that our study adds to the clarification of the role of rhuEpo in cardiac performance. However, some limitations should be mentioned. Firstly, the study population was relatively small. Secondly, it is unclear whether our findings are operative in patients with other stages of CKD. Thirdly, we performed measurements of Em only in the septal wall. During the study period this measurement was considered of equal value compared to the lateral mitral annular position. Only recently, some papers indicate that the assessment of lateral mitral annular velocities by TDI may be a little bit better for the evaluation of left ventricular filling pressures. Finally, in the majority of patients the cause of CKD was unknown. However, in many patients seen in our center the size of the kidneys (small size—shrinked kidneys) and the presence of increased echogenicity did not permit the performance of renal biopsy.
5 Conclusions
In conclusion, the administration of rhuEpo in CKD patients with renal anemia seems to have beneficial effects on cardiac performance and structure. Further studies with larger populations and longer follow-up are needed in order to elucidate the impact of this strategy on the LV systolic and diastolic function.
References
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risk of death, cardiovascular events, and hospitalization. N Engl J Med 2004;351:1296–305.
Vanholder R, Massy Z, Argiles A, et al. Chronic kidney disease as cause of cardiovascular morbidity and mortality. Nephrol Dial Transplant 2005;20:1048–56.
Fort J. Chronic renal failure: a cardiovascular risk factor. Kidney Int 2005;68:S25–9.
Parfrey PS, Foley RN, Harnett JD, Kent GM, Murray DC, Barre PE. Outcome and risk factors for left ventricular disorders in chronic uraemia. Nephrol Dial Transplant 1996;11:1277–85.
Levin A, Singer J, Thompson CR, Ross H, Lewis M. Prevalent left ventricular hypertrophy in the predialysis population: identifying opportunities for intervention. Am J Kidney Dis 1996;27:347–54.
Levin A, Thompson CR, Ethier J, Carlisle EJ, Tobe S, Mendelssohn D, et al. Left ventricular mass index increase in early renal disease: impact of decline in hemoglobin. Am J Kidney Dis 1999;34:125–34.
Silberberg JS, Barre PE, Prichard SS, Sniderman AD. Impact of left ventricular hypertrophy on survival in end-stage renal disease. Kidney Int 1989;36:286–90.
Foley RN, Parfrey PS, Morgan J, Barre PE, Cambell P, Cartier P, et al. Effect of hemoglobin levels in hemodialysis patients with asymptomatic cardiomyopahty. Kidney Int 2000;58:1325–35.
Ma JZ, Ebben J, Xia H, Collins AJ. Hematocrit level and associated mortality in hemodialysis patients. J Am Soc Nephrol 1999;10:610–9.
Block GA, Hulbert-Shearon TE, Levin NW, Port FK. Association of serum phosphorus and calcium X phosphate product with mortality risk in chronic hemodialysis patients: a national study. Am J Kidney Dis 1988;31:607–7.
Foley RN, Parfrey PS, Harnett JD, Kent GM, Martin CJ, Murray DC, Barre PE. Clinical and echocardiographic disease in patients starting end-stage renal disease therapy. Kidney Int 1995;47:186–92.
Foley RN, Parfrey PS, Kent GM, Harnett JD, Murray DC, Barre PE. Serial change in echocardiographic parameters and cardiac failure in end-stage renal disease. J Am Soc Nephrol 2000;11:912–6.
Portoles J, Torralbo A, Martin P, Rodrigo J, Herrero JA, Barrientos A. Cardiovascular effects or recombinant human erythropoietin in predialysis patients. Am J Kidney Dis 1997;29:541–8.
Hayashi T, Suzuki A, Shoji T, Togawa M, Okada N, Tsubakihara Y, Imai E, Hori M. Cardiovascular effect of normalizing the hematocrit level during erythropoietin therapy in predialsyis patients with chronic renal failure. Am J Kidney Dis 2000;35:250–6.
Roger SD, McMahon LP, Clarkson A, Disney A, Harris D, Hawley C, et al. Effects of early and late intervention with epoetin alpha on left ventricular mass among patients with chronic kidney disease (stage 3 or 4): results of a randomized clinical trial. J Am Soc Nephrol 2004;15:148–56.
Ayus JC, Go AS, Valderrabano F, Verde E, Garcia de Vinuesa S, Achinger SG, Lorenzo V, Arieff AI, Luno J. Effects of erythropoietin on left ventricular hypertrophy in adults with severe chronic renal failure and hemoglobin <10 g/dL. Kidney Int 2005;68:788–95.
Eckart KU, Mcdougall I, Locatelli F, Tsakiris D, Clyne N, Drueke T. Effects of epoetin beta on left ventricular mass in patients with chronic kidney disease: echocardiographic results of the CREATE study. J Am Soc Nephrol 2005;16:37A.
Levin A, Djurdjev O, Thompson C, Barrett B, Ethier J, et al. Canadian randomized trial of haemoglobin maintenance to prevent or delay left ventricular mass growth in patients with CKD. Am J Kidney Dis 2005;46:799–11.
Drueke TB, Locatelli F, Clyne N, Eckardt KU, Macdougall IC, Tsakiris D, et al. Normalization of haemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med 2006;355:2071–84.
Gouva C, Nikolopoulos P, Ioannidis JP, Siamopoulos KC. Treating anemia early in renal failure patients slows the decline of renal function: a randomized controlled trial. Kidney Int 2004;66:753–60.
Cockroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976;16:31–41.
Eckardt KU, Casadevall N. Pure red-cell aplasia due to anti-erythropoietin antibodies. Nephrol Dial Transplant 2003;18:865–9.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18:499–502.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005;18:1440–63.
Devereux R, Reichek N. Echocardiographic determimation of left ventricular mass in man. Circulation 1997;55:1325–50.
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ, et al. New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function—a study in normals and dilated cardiomyopathy. J Cardiol 1995;26:357–66.
Natsume T. Therapeutic advances in the treatment of LVH. Eur Heart J 1993;14:D33–7.
London GM, Marchais SJ, Guerin AP, Metivier F, Bruno P. Cardiac hypertrophy and arterial alterations in ESRD: hemodynamic factors. Kidney Int 1993;43:S42–9.
Foley RN, Parfrey PS, Harnett JD, Kent GM, Murray DC, Barre PE. The impact of anemia on cardionyopahty, morbidity, and mortality in end-stage renal disease. Am J Kidney Dis 2003;41:520–1.
Singh AK, Szczech L, Tang KL, Barnhart H, Sapp S, Wolfson M, Reddan D. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med 2006;355:2085–98.
Remuzzi G, Ingelfinger JR. Correction of anemia—payoffs and problems. N Engl J Med 2006;355:2144–6.
Van Veldhuisen DJ, McMurray JJV. Are erythropoietin stimulating proteins safe and efficacious in heart failure? Why we need an adequately powered randomised outcome trial. Eur J Heart Fail 2007;9:110–2.
Maiese K, Li F, Chong ZZ. New avenues of exploration for erythropoietin. JAMA 2005;293:90–5.
Bogoyevitch MA. An update on the cardiac effects of erythropoietin cardioprotection by erythropoietin and the lessons learnt from studies in neuroprotection. Cardiovasc Res 2004;63:208–16.
Henry DH, Bowers P, Romano MT, Provenzano R. Epoetin alfa. Clinical evolution of a pleiotropic cytokine. Arch Intern Med 2004;164:262–76.
Ogilvie M, Yu X, Nicolas-Metral V, Pulido SM, Liu C, Ruegg UT, Noguchi CT. Erythropoietin stimulates proliferation and interferes with differentiation of myoblasts. J Biol Chem 2000;275:39754–61.
Tramontano AF, Muniyappa R, Black AD, Blendea MC, Cohen I, Deng L, Sowers JR, Cutaia MV, El-Sherif N. Erythropoietin protects cardiac myocytes from hypoxia-induced apoptosis through an AKT dependent pathway. Biochem Biophys Res Commun 2003;112:990–4.
Cai Z, Manalo DJ, Wei G, Rodriguez ER, Fox-Talbot K, Lu H, Zweier JL, Semenza GL. Hearts from rodents exposed to intermittent hypoxia or erythropoietin are protected against ischemia–reperfusion injury. Circulation 2003;108:79–85.
Moon C, Krawczyk M, Paik D, Coleman T, Brines M, Juhaszova M, Sollott S, Lakatta EG, Talan MI. Eryhtropoietin reduces myocardial infarction and left ventricular functional decline after coronary artery ligation in rats. Proc Natl Acad Sci U S A 2003;100:11612–7.
Madeddu P, Emanueli C. Switching on reparative angiogenesis: essential role of the vascular erythropoietin receptor. Circ Res 2007;100:599–601.
Westenbrink BD, Lipsic E, van der Meer P, van der Harst P, Oeseburg H, Du Marchie Sarvaas GJ, et al. Erythropoietin improves cardiac function through endothelial progenitor cell and vascular endothelial growth factor mediated neovascularization. Eur Heart J 2007;28:2018–7.
Sohn DW, Chai IH, Lee DJ, Kim HC, Kim HS, Oh BH, et al. Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol 1997;30:474–80.
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Tajik AJ. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-chatheterization study. Circulation 2000;102:1788–94.
Dujardin KS, Tei C, Yeo T, Hodge DO, Rossi A, Seward JB. Prognostic value of a Doppler index combining systolic and diastolic performance in idiopathic-dilated cardiomyopahty. Am J Cardiol 1998;82:1071–6.
Acil T, Wichter T, Stypmann J, Janssen F, Paul M, Grude M, Scheld HH, Breithardt G, Bruch C. Prognostic value of tissue Doppler imaging in patients with chronic congestive heart failure. Int J Cardiol 2005;103:175–81.
Benz RL, Pressman MR, Hovick ET, Peterson DD. A preliminary study of the effects of correction of anemia with recombinant human erythropoietin therapy on sleep, sleep disorders, and daytime sleepiness in hemodialysis patients (the SLEEPO study). Am J Kidney Dis 1999;34:1089–95.
McMahon LP, McKenna MJ, Sangkabutra T, Mason K, Sostaric S, Skinner SL, Burge C, Murphy B, Crankshaw D. Physical performance and associated electrolyte changes after haemoglobin normalization: a comparative study in haemodialysis patients. Nephrol Dial Transplant 1999;14:1182–7.
McMahon LP, Mason K, Skinner SL, Burge CM, Grigg LE, Becker GJ. Effects of haemoglobin normalization on quality of life and cardiovascular parameters in end-stage renal failure. Nephrol Dial Transplant 2000;15:1425–30.
Kuriyama S, Tomonari H, Yoshida H, Hashimoto T, Kawaguchi Y, Sakai O. Reversal of anemia by erythropoietin therapy retards the progression of chronic renal failure, especially in nondiabetic patients. Nephron 1997;77:176–85.
Siamopoulos KC, Gouva C, Katopodis KP, Tzallas C, Nikolopoulos P, Papavasiliou EC, Tselepis AD. Long-term treatment with EPO increases serum levels of high-density lipoprotein in patients with CKD. Am J Kidney Dis 2006;48:242–9.
Acknowledgement
The authors wish to thank Mrs. Aleka Papageorgiou for the skilled secretarial assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pappas, K.D., Gouva, C.D., Katopodis, K.P. et al. Correction of Anemia with Erythropoietin in Chronic Kidney Disease (stage 3 or 4): Effects on Cardiac Performance. Cardiovasc Drugs Ther 22, 37–44 (2008). https://doi.org/10.1007/s10557-007-6075-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-007-6075-6