Abstract
Hereditary diffuse gastric cancer is an autosomic dominant syndrome associated with E-cadherin protein (CDH1) gene germline mutations. Clinical criteria for genetic screening were revised in 2010 by the International Gastric Cancer Linkage Consortium at the Cambridge meeting. About 40 % of families fulfilling clinical criteria for this inherited disease present deleterious CDH1 germline mutations. Lobular breast cancer is a neoplastic condition associated with hereditary diffuse gastric cancer syndrome. E-cadherin constitutional mutations have been described in both settings, in gastric and breast cancers. The management of CDH1 asymptomatic mutation carriers requires a multidisciplinary approach; the only life-saving procedure is the prophylactic total gastrectomy after thorough genetic counselling. Several prophylactic gastrectomies have been performed to date; conversely, no prophylactic mastectomies have been described in CDH1 mutant carriers. However, the recent discovery of novel germline alterations in pedigree clustering only for lobular breast cancer opens up a new debate in the management of these individuals. In this critical review, we describe the clinical management of CDH1 germline mutant carriers providing specific recommendations for genetic counselling, clinical criteria, surveillance and/ or prophylactic surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Gastric cancer (GC) is a heterogeneous disease and is the second leading cause of cancer death worldwide [1], with approximately 930,000 new cases of GC per year leading to >700,000 deaths. About 90 % of GC cases are sporadic, and familial clustering is observed in the remaining 10 % of the patients [2]. Among these, 1–3 % meets the criteria for hereditary diffuse gastric cancer (HDGC), an inherited condition initially described in three Maori families from New Zealand [3]. This syndrome is an autosomal dominant cancer predisposition, due—in approximately 30 % of individuals meeting the diagnostic criteria for HDGC—to pathogenic germline mutations affecting the gene encoding for the E-cadherin protein (CDH1). More than 100 different germline CDH1 mutations have been identified in HDGC families in a diverse range of ethnic groups [4, 5]. Mutation carriers have a significant risk (of more than 70 % over their lifetime) of developing the diffuse histologic type of GC (DGC), together with a high probability of lobular breast cancer (LBC) in females [6]. The BC cumulative risk was assessed at around 40 % [6].
Prophylactic surgery, as the total gastrectomy, represents the only life-saving procedure for asymptomatic E-cad germline mutation carriers [7–11]. No data are reported on prophylactic mastectomy in E-cad mutation carriers; however, this approach is an emerging question since novel E-cad germline mutations have recently been discovered in the absence of DGCs [12, 13]. Endoscopic surveillance for HDGC has been reported previously to be ineffective; in a series of 23 patients, pre-operative endoscopy failed to detect it in 21 (91 %) patients, as early foci of HDGC are typically subtle and underlie normal mucosa [14]. Chromoendoscopy seems to improve the sensitivity of detection of early HDGC, allowing for direct inspection and biopsy of suspicious areas, in spite of a major difficulty in identification of submucosal lesions as well as sampling bias in a macroscopically normal gastric mucosa [15]. Endoscopic ultrasound examination is not believed to be useful in identifying early lesions.
Unaffected mutation carriers from HDGC families face difficult decisions before prophylactic surgery and should be assisted by a multidisciplinary team. The clinical approach to individuals with a suspicious or confirmed inherited cancer predisposition requires close collaboration between the geneticist, surgeon, gastroenterologist, nutritionist and radiologist for appropriate management.
In this critical review, we aim to provide a multidisciplinary consensus for CDH1 germline asymptomatic mutation carriers, focusing particularly on the clinical and genetic management of DGC and LBC.
2 Clinical criteria
2.1 Hereditary diffuse gastric cancer
Clinical criteria for the definition of HDGC syndrome were established in the last International Gastric Cancer Linkage Consortium (IGCLC) meeting [15]. The Cambridge consensus conference established that E-cad germline mutation screening should be offered to pedigrees with two DGC cases in the family, one confirmed <50 years at onset, and/or three confirmed DGC cases in first- or second-degree relatives independent of age.
2.2 Early-onset sporadic diffuse gastric cancer
EOGC is defined as any GC presenting at the age of 45 or earlier. Germline E-cad mutations are rarely identified in this subset; the frequency of pathogenic alterations is defined as around 3 %. It has established that genetic screening is recommended only in cases with age at onset of less than 35 years [16].
2.3 Lobular breast cancer
For LBC, the Consortium suggested genetic screening only for cases with personal or family history of DGC in association, one with age at onset <50 years [15]. This criterion includes patients affected by synchronous and/ or metachronous DGC and LBC, but excluded cases with sporadic LBC. However, novel CDH1 germline mutations have recently been detected in patients with sporadic and bilateral setting.
3 Genetic counselling
Today, in the context of clinical oncology and cancer prevention, the entire clinical management has changed profoundly. One of the most significant novelties is the modern approach to the risk assessment and counselling of the patient or subject, which is frequently carried out since the very beginning of the therapeutic or prevention pathway.
An increasing number of individuals—affected by cancer or with a significant family history—are referred to cancer centres for risk assessment, therapy and prevention. A multidisciplinary group of specialists should take care of the entire programme of risk assessment and management in high-risk subjects: this must include trained clinical oncologists, geneticists and genetic counsellors, together with psychologists, radiologists, surgeons, endoscopists and so on, preferably in an established high-risk clinic. As the number of risk factors is always high and their combining effect is often complex to evaluate, the risk assessment phase of a subject often requires time, patience, documentation and multiple expertise to be appropriately carried out. Notoriously, only a fraction of patients/subjects is then selected for genetic evaluation in order to investigate their probability of having an inherited susceptibility to cancer. This accurate selection is essential to appropriately perform genetic counselling and testing, employ specialized human and laboratory resources and save costs, and should be adequately explained to referring professionals and candidate counselands.
When deemed appropriate, a genetic assessment may be an essential tool for providing holistic care to patients and families since a genetic evaluation may reveal that an individual has a much higher than average risk of developing cancer (not infrequently multiple and of early onset during lifetime) in various organs and the same risk may be shared by relatives. Indeed, a comprehensive risk assessment may be currently crucial not only for the patients but also for the relatives since more genetic syndromes have been recently identified and many correspondent molecular tests are clinically available [17].
Notably, counselling and testing may have various and sometimes opposite effects. One remarkable example is the result of sample testing in the relatives after the identification of a deleterious germline mutation in the index case: the biological, clinical and psychological implications of being positive or negative have strikingly different impacts, the latter having cancer risks which are equal or much closer to the general population.
Genetic assessment for HDGC syndrome may help significantly to determine the likelihood that an individual will develop gastric and BC. For this, it is required to collect and evaluate as much information as possible about the personal and family history, which may also include non-genetic risk factors (i.e. lifestyle and endocrine and metabolic disorders, exposure to radiation or potential carcinogens and so on, together with physical and instrumental examinations when appropriate). In fact, cancer is always a multifactorial disease, and even a single deleterious genetic mutation may be not enough to cause a malignancy [18].
Genetic assessment should start from patient and family data collection that can facilitate the whole process before the first genetic consultation. In our work model, there is a pre-counselling phase during which a purpose-made Family History Questionnaire (FHQ) is filled out and submitted by the counseland to the genetic counsellor before the first appointment. The FHQ provides information about medical and family history and lifestyle and all the necessary data to draw the pedigree. The family tree analysis may result in the identification of inheritance patterns and high-risk individuals and—importantly—allows the best proband in the family to be identified.
During the first genetic counselling session, by collecting and interpreting cancer risk information, healthcare professionals can help the proband to make a fully informed decision whether to undergo genetic testing and to cope with all the post-test implications. It should be emphasized that in the case of DGC, no specific exogenous risk factors have been recognized so far, and its incidence has not decreased compared to the intestinal type, which suggests that genetic factors do play an important role [19, 20] and that approximately 10 % of GCs present familial clustering but only 1–3 % show an autosomal dominant inherited trait [21].
Since genetic testing is just one of the tools used for a comprehensive cancer risk assessment, a good risk estimate can be important for all subjects, but somehow even more so for those who decline genetic testing at the time. Decliners too need to understand their risk of developing cancer and the inherent strength and weakness associated with tests. Psychosocial assessment may be also useful here.
The most relevant parameters to address regarding referral of a subject for genetic counselling and testing are enclosed in the Brooks-Wilson’s modified criteria [22]:
-
1.
Family history with two or more first-degree relatives with GC, with at least one documented DGC diagnosed before age 50;
-
2.
Family history with three or more first/second-degree relatives with GC, diagnosed at any age, with at least one documented case of DGC;
-
3.
One individual diagnosed with DGC <45 years of age, regardless of family history;
-
4.
Family history with two or more first/second-degree relatives with LBC, with or without DGC.
In families without living affected members, the indication to perform genetic test is still controversial and should be decided case by case. Testing from paraffin-embedded samples may be discussed in very selected cases.
Basically, after verifying the cancer subtype (DGC or signet ring cell carcinoma for GC or lobular histotype for BC), genetic testing for CDH1 is considered first. It should be made clear that the reported detection rate of CDH1 mutations is 25–50 %, even when using CDH1-expert laboratories [4, 15, 23].
High incidence of GC may also be the clinical expression of a few other autosomal dominant inherited disease syndromes: the Li-Fraumeni syndrome, associated with TP53 mutations [24], but the GC incidence in such families is very low (<3 % lifetime risk) [25]; the Lynch syndrome, associated with mismatch repair (MMR) mutations (10 % lifetime risk) [26], and the Peutz-Jeghers syndrome, associated with STK11 mutations [27] (risk at 65 years is 47 %). GC may also be present in hereditary breast and ovarian cancer (HBOC) syndrome (when BRCA2 gene mutations occur); familial adenomatous polyposis (FAP) associated with APC mutations; MUTYH-associated polyposis (MAP); juvenile polyposis (APC associated); and Cowden syndrome (PTEN associated).
Genetic counselling and testing should be initiated in an affected proband, if available. Very rare cases of clinically significant diffuse GC have been reported before the age of 18 years old, and the overall risk of diffuse GC before the age of 20 is still very low [6, 28]. It has been agreed that genetic testing should be mostly performed after the age of 18 years old. The indications to perform genetic test when all affected members are not alive is controversial, but testing from paraffin-embedded samples may be discussed in very selected cases.
The results are then discussed with the proband during the second genetic counselling session. There are three possibilities: a deleterious mutation, an unknown variant mutation, and wild type. With a deleterious mutation, the risk category is well defined and it is advised to test all the relatives beginning with the first degree. Sample tests of variants of unknown clinical significance (where the risk level cannot be clearly set) may be carried out only for research purposes, while for those resulting wild type, the testing is not proposed to the relatives. Only occasionally based on the family tree, a new genetic test can be offered to a second proband within the family.
Once the risk level is categorized, different strategies can be offered to manage the risk. The strategies range from an adequate annual endoscopic surveillance programme for the best possible early detection to healthy lifestyle programmes, chemoprevention research protocols, up to prophylactic surgery. It should be made clear to CDH1 mutation carriers that the most effective preventive strategy at the moment remains prophylactic total gastrectomy (PTG). In non-PTG declining subjects, the decision should always be extensively discussed involving all the members of the multidisciplinary panel, including the psychologist and the dietician.
A coherent surveillance programme based on age and sex should be planned for the proband who results as a carrier of a CDH1 mutation. For the healthy relatives who result as carriers, individualized counselling is also recommended, followed again by an extensive discussion with the multidisciplinary team to coordinate all the different prevention aspects.
Thus, the management options usually discussed with mutation carriers are the following:
-
Gastric endoscopic surveillance, according to the “Cambridge Protocol” (in CDH1 mutation carriers from 20 years until prophylactic gastrectomy is performed);
-
Prophylactic gastrectomy, to be suggested according to the age at onset in the affected family members [29];
-
Breast surveillance, starting at age 35 or earlier based on the family history, with breast MRI, mammography and clinical examination every 12 months, while breast US can be recommended every 6 months.
There is no clear evidence for efficacy, but the family history could be sometimes useful to consider surveillance of other organs (such as ovaries).
In conclusion, in presence of the HDGC syndrome, counsellors should clearly explain the lack of reliable methods to find cancer precursors and to ensure very early stage detection. Chemopreventive strategies are still not validated. Endoscopic surveillance for high-risk families should always be performed in specialized centres with access to, and expertise of, new endoscopic techniques (e.g. HD, chromoendoscopy).
A consistent approach for referral to genetic counselling, DNA testing, tailored surveillance and prophylactic surgery may help in optimizing medical care for these very high-risk individuals.
4 Managing CDH1 missense mutations
HDGC is an autosomal dominant cancer disease [30–32]. The direct proof of a molecular basis for this type of GC was demonstrated in 1998, when germline mutations of the CDH1 gene were described in Maori families from New Zealand. In one of these families, several patients showed early-onset diffuse gastric, some of them in the second decade of life [3]. Since then, a large number of germline mutations have been identified in families with different ethnic backgrounds [4, 33, 34].
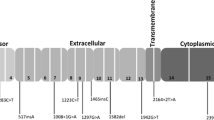
Until now, germline loss-of-function mutations in the CDH1 gene are the only genetic causative events described and occur in approximately 30 % of all HDGC families [3, 31, 32]. The most common CDH1 germline mutations include frameshift (28.7 %), splice-site (27.0 %) and non-sense mutations (19.7 %), which result in a loss of E-cadherin expression [35]. In about 18 % of the families, germline CDH1 mutations are of the missense type and retain aberrant E-cadherin expression with functional impact [4, 35–37]. These types of CDH1 germline variants represent a problem for genetic counselling and clinical surveillance of the mutant carriers and their families since their pathogenic relevance is not simple to determine [36]. Thus, evaluating the impact of the variants on protein regulation, conformation, localization and function is a laboratory and a clinical challenge.
In recent years, increasing efforts have been made to improve the classification of E-cadherin germline missense variants [36, 38–41]. A multidisciplinary approach that combines familial and population data, in silico and in vitro analyses, is currently available [34, 36, 39].
Regarding population and familial evaluation, it is recommended that one takes into account parameters such as mutation frequency in healthy control population, co-segregation of the mutation within the pedigree and recurrence of the mutation in independent families [38, 39]. Unfortunately, in most cases, it is not possible to perform these studies due to the lack of biological material or to the small size of the pedigree.
The in silico predictions may be performed rapidly, and the results estimate the degree of conservation of that nucleotide within species, the effect of those missense mutations on splicing and also their putative impact on protein structure [39]. The Sorting Intolerant from Tolerant (SIFT) software uses sequence homology to predict whether an amino acid substitution will affect protein function, assuming that essential amino acids will be conserved among species [39]. Still, this approach does not take into account the possible compensatory effects of neighbouring positions because the degree of conservation among species of each amino acid position is considered separately. To evaluate the effect of CDH1 missense variants on protein conformation, structural modelling has become an imperative tool and presently it covers the major part of E-cadherin structure [39, 40].
The biochemical and the in vitro functional assays reflect the impact of CDH1 missense alterations in protein structure, trafficking, signalling and, consequently, in E-cadherin function. The CHO (Chinese hamster ovary) cell line, that is negative for E-cadherin expression, is used as a “test tube” to evaluate the two main functions of E-cadherin: cell-cell adhesion and invasion suppression [36]. Upon transfection with wild-type E-cadherin or its mutant forms, slow aggregation on soft agar and cell invasion into matrigel matrix have been performed to assess the functional impact of CDH1 germline missense mutations [4, 23, 29, 36, 37, 42–48]. Recently, and in an attempt to offer a more accurate evaluation, Figueiredo et al. proposed, as a complementary approach, the use of proximity ligation assays (PLA) to study how a mutant protein binds to crucial regulators and interactors of E-cadherin, namely p120, β-catenin, PIPKIγ and Hakai [41].
So far, 49 germline CDH1 missense mutations have been reported to IPATIMUP (Porto), a reference laboratory of IGCLC, to be functionally analysed. The vast majority of them was classified as pathogenic since they remain unable to induce cell-cell adhesion and to suppress invasion [4, 23, 29, 36, 37, 42–48], reinforcing the potential of these functional approaches in predicting the pathogenic relevance of unclassified variants.
As a tumour invasion suppressor gene, E-cadherin not only provides a physical link within tissues but also orchestrates proper adhesion, cell division and the maintenance of a differentiation epithelial programme, implicating it as a component of the cellular signalling network [49]. One important pathway, relevant in cell motility, which is abnormally activated in the presence of HDGC-related E-cadherin mutations, is EGF-EGFR signalling. It was demonstrated that mutations affecting the extracellular domain of E-cadherin lead to the activation of EGFR upon EGF stimulation as well as its downstream effectors (RhoA, Src kinase and p38 MAPK) [50–52]. Importantly, this subset of HDGC patients may benefit from treatment with EGFR inhibitors [50]. Another interesting therapeutic target of E-cadherin loss of function, in the subset of germline missense mutations, is the aberrant activation of Notch signalling and upregulation of Bcl-2 that renders mutant cells more resistant to apoptotic stimuli (Fig. 1) [53, 54].
Illustration of the development of diffuse gastric cancer in E-cadherin mutation carriers and its signalling associated pathways. a Normal gastric glands (left panel). In situ signet ring cell carcinoma: glands with intact basement membrane lined by signet ring cells with depolarized nuclei (middle panel). Pagetoid spread of signet ring cells below the preserved epithelium of the glands (middle panel). Invasive intramucosal carcinoma constituted by signet ring cells (right panel). b In a homeostatic situation, E-cadherin is expressed at the adherens junctions playing a crucial role in cell-cell adhesion and in the polarized architecture of the tissue. c CDH1 mutations can, however, induce loss of E-cadherin function and abnormally activate a number of mechanisms and signalling pathways. Mutated proteins present severe structural abnormalities, resulting in protein misfolding that is recognized and degraded by ERAD. At the plasma membrane, mutant proteins cannot establish the cytoplasmic catenin complex, allowing its rapid internalization and degradation. E-cadherin loss results in abnormal activation of EGFR and Notch pathways, with consequences on cell motility, invasion and resistance to apoptotic stimuli
Recently, Simões-Correia and colleagues demonstrated that E-cadherin mutants are critically modulated by mechanisms of protein quality control (PQC) leading to protein destabilization [40, 46]. These events are likely to result from the presence of misfolded mutant proteins that are recognized by the endoplasmic reticulum-associated degradation (ERAD) system and lead to loss of E-cadherin expression and function [40]. The identification of this molecular mechanism of regulation represents a new therapeutic option for cancers harbouring destabilizing E-cadherin mutations. In fact, by treating the E-cadherin mutant cells with chemical chaperones (CCs), it was possible to restore E-cadherin expression, regular localization and function reversing their pathogenic behaviour [46, 55]. The mechanism underlying this effect involves the modulation of key trafficking molecules such as Arf6 and PIPKIγ [55]. Arf6 downregulation leads to a significant accumulation of the protein at the plasma membrane, inhibiting E-cadherin endocytosis, recycling and degradation. In turn, PIPKIγ binding is responsible for the improvement of E-cadherin exocytosis, transport and stabilization [55].
Altogether, these findings demonstrate that, despite the subtle nature of missense mutations, these single amino acid changes can dramatically compromise E-cadherin function, expression and localization, supporting its pathogenic role in HDGC. Therefore, identifying the molecular mechanism of cadherin-dependent signalling and the key molecules interacting with E-cadherin for cancer cell invasion are of crucial importance in developing new approaches for the clinical management of HDGC patients.
5 Prophylactic total gastrectomy
Because of the lack of effective endoscopic screening and surveillance programmes, PTG is now strongly recommended for carriers of CDH1 germline mutations [15]. In total, there have been roughly 100 patients with CDH1 mutation who have undergone PTG and for whom results have been reported in the English language literature, due to the rarity of this germline mutation and the magnitude of proposed surgery. In accordance with recent investigations, PTG should be recommended in each case of an “asymptomatic” CDH1 mutation carrier, as a significant difference in prognosis between asymptomatic and symptomatic patients was demonstrated in a prospective study of PTG for CDH1-positive HDGC [56]. All asymptomatic patients were cured of GC after PTG in this study, while four of five symptomatic patients had tumour recurrence or metastases, and three (60 %) died within 2 years, thus stressing the importance of early PTG, whereby the gastric mucosa is removed before the further development of carcinoma foci. It is estimated that the risk of advanced HDGC is less than 1 % at age 20, and some authors have proposed PTG during the second decade of life [57], when cancer foci are hopefully small and confined to gastric mucosa. This period of T1 N0 signet ring cell cancer may have a long latency, and the tumour may require another trigger before it progresses to a symptomatic, more aggressive disease. Although the majority of patients have normal endoscopies before surgery, more than 90 % have intramucosal or superficially invasive carcinoma identified in the gastrectomy specimen, with more than 80 % of multifocal disease. The entire stomach has to be fixed and the entire mucosa mapped and examined microscopically; this may require up to 600 sections. In addition, it is essential to document the complete removal of gastric mucosa by pathologically identifying rims of oesophageal and duodenal mucosa at the two ends of the surgical specimen. This may be quite easily obtained by intraoperative frozen sections of the proximal and distal margins or by intraoperative oesophagoscopy. However, in some cases the exact location of the cardio-esophageal junction being the problem to be solved by the surgeon.
Although no formal lymph node dissection is usually performed, D1 stations (1 to 6) are routinely removed in the vast majority of treated cases as part of the gastrectomy specimen, with the number of removed nodes usually ranging from 10 to 25. Almost all nodes of asymptomatic patients submitted to a “real” PTG do not show any metastatic involvement. The potential need for any lymphadenectomy which is more extensive than a D1 procedure can be inferred from the Japanese data documenting the frequency of nodal metastases in early GC treated with D2 procedures. The prevalence of nodal involvement in cases of GC limited to the organ mucosa is 5 % instead of 16 % in cases of submucosal infiltration. Western series of early GC document up to 28 % of lymph node metastases, thus underlining the role of an adequate N dissection and limiting the application of sentinel node mapping [58]. Sentinel node mapping for the staging of nodal disease has been described using radiotracer with gamma probe localisation in patients with T1N0 or T2N0 GC. A sentinel node was present in 95.2 % of the cases with metastases documented in 7.8 % of the patients [59]. Non-sentinel node metastases were detected in only 0.3 % of the cases. A similar report using blue dye and radionucleotide tracer demonstrated that a sentinel node could be identified in nearly 100 % of the patients [60].
Apart from complications associated with all elective GI surgical resections, such as bleeding or infection, the most significant side effect of a PTG results from a potential leak at the oesophago-jejunal anastomosis. There is sufficient evidence from randomized controlled trials that the incidence of an anastomotic leak, operative mortality, overall morbidity and length of hospital stay are not statistically different when a stapled versus a hand-sewn anastomosis is performed. Pooled data coming from 14 controlled randomized trials of gastric reconstruction after total gastrectomy confirm a mortality rate ranging from 0 to 22 % [61], even though the majority of current investigations from high-volume centres report mortality figures less than 3 %. Moreover, since all documented CDH1 carriers are likely to be young—and otherwise healthy candidates—morbidity and mortality figures are expected significantly lower when compared to gastrectomy for sporadic, invasive disease. Other relevant consequences of the operation include decrease in vitamin B12 and protein absorption, bacterial overgrowth due to loss of parietal and chief cells of the stomach, reflux, dumping and weight loss. This nadirs after 3–6 months and averages about 20 % of pre-operative weight. Attempts to limit these problems have produced a number of proposed reconstructive procedures to establish intestinal continuity after PTG [62]. Many technical variations for interposition have been reported, and none appear more effective than the traditional Roux-en-Y oesophagojejunostomy in eliminating the above-mentioned quality of life issues. Nearly all available variations in reconstructive techniques involve the efficacy and the length of a side-to-side-stapled jejunal pouch. These approaches were proposed under the idea that loss of the gastric reservoir is responsible for the majority of post-operative consequences. Unfortunately, almost all randomized trials comparing total gastrectomy with and without a pouch for interposition did not account for expected variations in caloric intake after surgical procedure, and little can be therefore concluded about the impact of the pouch in restoring nutritional failures. A small benefit of jejunal pouches in terms of early food intake, which diminishes over time, was detected in some studies and denied in others [63]. Even less conclusive evidence can be drawn about the influence of minimal changes in pouch length, length of the R–Y limb and potential inclusion of the duodenum from the reconstructed alimentary route. In fact, reconstruction is generally performed with a Roux-en-Y technique with at least a 50-cm Roux limb to prevent bile reflux.
Another possible issue—so far poorly investigated—is the vagal-sparing technique, which can be associated with PTG, maintaining the vagal fibres intact, which are not directed to the stomach wall. The length of hospital stay and the incidence of major complications was significantly reduced with a vagal-sparing oesophagectomy, compared with a transhiatal or en bloc resection, in a retrospectively investigated large series of patients with intramucosal adenocarcinoma. Furthermore, post-vagotomy dumping and diarrhoea symptoms were significantly less common, and weight was better maintained post-operatively with a vagal-sparing oesophagectomy [64]. These preliminary findings merit further investigation, especially if the application of a vagal-sparing technique could be able to limit the extent of a due lymphadenectomy.
Laparoscopic- or robot-assisted total gastrectomy has been initiated recently in cases of early GC or HDGC [65, 66]. With regard to the laparoscopic/robot-assisted versus open technique, definite conclusions cannot be drawn from isolated phase II clinical series or very small controlled randomized trials. Nevertheless, most reports support the fact that early outcomes, like time to first flatus, time to initial oral intake and post-operative hospital stay, were significantly shorter in laparoscopic/ robot-assisted total gastrectomy compared to open procedures, with no additional advantages so far identified for robot-assisted vs laparoscopic procedures. A recent meta-analysis—including nine studies with 1221 participants—concluded that laparoscopic-assisted total gastrectomy is suitable and feasible for early GC and that the main advantage is a shorter recovery time [67].
6 Health-related quality of life after prophylactic total gastrectomy
The effect of PTG on the health-related quality of life of healthy individuals is so far undocumented, although it is well known that recovery of cancer patients from therapeutic gastrectomy leads to a significant comorbidity of up to 100 %, including diarrhoea, dumping syndrome and loss of approximately 10 to 20 % of the original body weight. The University of Cambridge (UK) [68] has recently published a large prospective cohort study on this topic. A total of 32 individuals fulfilling HFGC criteria underwent PTG. Questionnaires, including the European Organization for Research and Treatment for Cancer Quality-of-Life Questionnaire (EORTC QLQ C30), the GC specific module (EORTC QLQ STO22) and the 36-item short form health survey version 2.0 were completed before surgery and at regular intervals after surgery. At baseline, there was no significant difference in mental health depending on CDH1 mutation status and treatment preference (6 patients out of 38 had a CDH1 mutation, but refused PTG). Physical functioning reduced in the first month after surgery but recovered to baseline by 12 months. Similarly, mental functioning reduced in the first month after surgery, but recovered by 3 to 9 months. Specific symptoms were identified, such as diarrhoea (70 %), fatigue (63 %), discomfort when eating (81 %), reflux (63 %), eating restriction (45 %) and body image change (44 %), which persisted after PTG. The authors’ main conclusion was that patients contemplating PTG can be reassured about the long-term health-related quality of life outcomes, but some residual symptoms require adjustment. Challenges remain, however, including life-long follow-up of PTG patients, which may reveal more negative effects, given the inability to carry out a full comparison over time of the health-related quality of life issues between those who opted for surveillance and those who undertook PTG.
In conclusion, until there is a breakthrough in gene therapy, PTG will continue to offer the only potential cure for GC in CDH1 mutation carriers, and it is essential that we optimize the quality of life for patients undergoing PTG.
7 CDH1 germline mutation and lobular breast cancer
Apart from the well-documented association between LBC and HDGC syndrome, novel E-cadherin germline mutations have recently been discovered in women affected by LBCs without a history of DGC. The IGCLC criteria suggest E-cad screening in LBC cases associated with a personal or family history of DGC (one with age <50 years) [15]. However, recent studies have provided evidence that early-onset LBC might be the first manifestation of HDGC; Benusiglio et al. [12] identified E-cad germline deleterious mutations in three bilateral LBC cases (age at onset <50 years) not fulfilling the IGCLC criteria, negative for DGC in first- and second-degree relatives and without BRCA1 and BRCA2 alterations. Moreover, E-cad mutations have been identified in four bilateral early-onset LBCs (age at onset <51 years) with no family history for DGC [13]. These results suggest that germline E-cad screening should also be offered in cases with sporadic early-onset LBCs without family history of DGCs, with particular attention for cases with bilateral manifestation.
In detail, 482 cases of LBCs have been screened for CDH1 constitutional mutations and 14 novel alterations (2.9 %) have been reported. Although the overall frequency of E-cadherin germline mutation is a rare event, genetic testing should be suggested in these cases in order to clarify the impact of CDH1 in the familial LB carcinogenesis. No prophylactic mastectomies have been described in CDH1 mutation carriers.
8 Endoscopic surveillance
The management of hereditary diffuse-type GC revolves around surveillance biopsies and the timing of prophylactic gastrectomy. In the absence of a validated surveillance biopsy protocol, and clinical trials on which to base recommendations for surveillance or screening in HDGC, consensus guidelines for clinical management were published in 2010 [15].
The consensus reached at the workshop was that individuals who resulted positive for a CDH1 mutation should be advised to consider prophylactic gastrectomy regardless of any endoscopic findings, whereas the management for those with clinical features suggestive of HDGD or those without CDH1 mutation should have screening. Moreover, consensus recommended that yearly endoscopic surveillance should also be offered to families who fulfil the criteria for HDGC. However, all patients should be advised that in view of the very focal nature of these endoscopically invisible lesions, it is quite possible that they will not be detected by random biopsies. For this reasons, the clinical benefit of endoscopic surveillance is not fully established.
Individuals should be offered an annual endoscopy, which should ideally be performed in a centre with expertise in this condition. The endoscopy should be performed using a white-light high-definition endoscope in a dedicated session to allow for a careful inspection taking at least 30 min and to allow time for multiple biopsies to be taken [15].
The role of gastroscopy in HDGC is somewhat problematic because of the inherent limitations of trying to reliably detect early DGC, which typically infiltrates beneath an intact surface epithelium without producing ulceration or elevation of the mucosa. In keeping with this, in nearly all prophylactic gastrectomies, despite normal pre-operative gastroscopy, microscopic foci of early HDGC are found, even though in the majority of cases the foci are smaller than 3 mm [69].
Due to the tiny microscopic foci of signet ring cells, multiple biopsies are required to maximize the likelihood of diagnosing them [70]. During surveillance gastroscopy, an accurate bioptic mapping of the transitional zone of the stomach between the body and antrum has been suggested to increase the diagnostic yield since in New Zealand Maori families, the neoplasia has been reported to occur in this area of the stomach [28, 71]. By contrast, in North American and European families, early invasive carcinoma was identified throughout the stomach, without evidence of clustering in a specific region [7–9, 70, 72]. Rogers et al. reported in a case series that 70 % of the total foci were localized in the proximal third of the stomach [73]. In a UK series, the highest number of foci was again observed in the fundus (44.7 %) and the body (40.2 %) [70]. Therefore, it is recommended that any endoscopically visible lesions are targeted and in addition that at least six random biopsies be taken for each of the following gastric zones: antrum, transitional zone, body, fundus and cardia. Thus, a minimum of 30 biopsies in all are recommended [15].
Recently, two studies contributed to further knowledge on gastroscopic surveillance. In the first study, calculations were made on bioptic diagnostic yield on the basis of the topographic distribution of cancer foci in a series of 10 gastrectomies in CDH1-mutation carriers: 1817 slides were evaluated for the presence of in situ, intramucosal or submucosal diffuse-type carcinoma, and detailed maps determined the density of cancer foci on the basis of the number of sampled glands per biopsy in routine surveillance pre-operative endoscopy. Based on the number of glands per stomach and the average number of glands sampled during surveillance biopsy (28.7 ± 1.7; range, 0 to 79; n = 112), the theoretical number of biopsies necessary to capture at least one cancer focus was estimated to be 1768 (range, 50 to 5832) to assure a 90 % detection rate. The highest density of cancer foci was shown in the proximal fundus (64 %) [74].
The second study is a prospective, observational cohort study with the aim of determining the natural history and outcomes of patients with HDGC undergoing endoscopy. A surveillance programme using high-resolution white-light endoscopy with autofluorescence and narrow-band imaging (NBI) combined with targeted and multiple random biopsies assessed by an expert histopathologist was undertaken. A total of 29 patients from 17 families underwent 70 surveillance endoscopies with the primary endpoint to determine the endoscopic yield of microscopic signet ring cell carcinoma according to patient mutation status and subsequent decision to undergo surgery. The secondary endpoint was the additional yield of targeted biopsies compared with random biopsies. Signet ring cell carcinoma foci were identified in 14 of 22 (63.6 %) patients with confirmed CDH1 mutations and 2 of 7 (28.6 %) with no pathogenic mutation identified. Eleven of 16 (9 CDH1-positive) patients proceeded to gastrectomy in a median of 5.7 months. In one patient, advanced GC developed 40.2 months after the first endoscopic findings. The authors concluded that careful white-light examination with targeted and random biopsies combined with detailed histopathology can identify early lesions and help to inform decision-making with regard to gastrectomy. Autofluorescence and narrow-band imaging are of limited utility [75].
Summarizing the updated consensus and the findings from above studies, gastroscopic surveillance is obligatory in family members of HDGC. Endoscopic surveillance is not fully consistent, even with accurate stomach mapping in a dedicated centre and with more advanced endoscopic techniques, i.e. NBI, thus calling into question the validity of endoscopic surveillance as an alternative to prophylactic gastrectomy.
9 Breast surveillance
Lobular lesions have, in most cases, an atypical imaging presentation related to their histological features.
“Classical” ILC (invasive lobular carcinoma) typically comprises small bland cells that infiltrate along and around ducts in single file without destroying the underlying architecture. In most ILCs (90 %), the expression of E-cadherin is lost contributing to the lack of tumour cell cohesion and to the diffuse growth pattern [76, 77].
The loss of E-cadherin in most ILCs results in fewer cancer cells and more low-density fat per unit volume of tumour, compared with IDCs, which are a compact, dense cancer and are therefore relatively opaque to X-rays, and possibly more easily palpable [76].
Detection is also compromised because ILC often has a density less than or equal to normal fibroglandular breast tissue on mammography due to its diffuse growth pattern, leaving the pre-existing breast architecture largely intact, and a low tendency to induce a desmoplastic reaction [78–80].
Conventional imaging such as mammographic screening may present some difficulties in the identification of lobular lesions; consequently at diagnosis, the mean tumour size of ILC is slightly larger than that in patients with IDC [78].
The sensitivity of mammography for ILC is correlated to breast density and ranges between 64 and 92 % [81, 82].
On mammograms, the commonest abnormal findings were localized spiculated mass (42–53 %), architectural distortion (14–16 %); discrete non-spiculated mass (about 7 %) or asymmetrical density (about 4 %), which is sometimes difficult to see in the absence of previous mammograms [76, 83].
Microcalcifications are not a feature of pure ILC (presents only in 3–13 % of cases) but may be present in mixed tumours, in an associated component of DCIS or in pleomorphic lobular carcinoma in situ. Microcalcifications are also mostly observed around areas of sclerosing adenosis and apocrine metaplasia juxtaposed to tumour areas, and they facilitate diagnosis of lobular neoplasia by radiology [84, 85].
Because of the low rate or the absence of suspicious calcification and its tendency to be of low opacity, the mammography may be normal in about 30 % of cases with a false-negative rate ranging from 19 to 66 % [79, 86].
Ultrasound imaging is more sensitive than mammography in the visualization of ILC; with this tool, the sensitivity grows to 98 % (range 86–98 %) [82, 87].
Lobular lesions may appear at ultrasound as an irregular hypoechoic mass with posterior shadowing (68–84 %) or without shadowing (about 20 %), shadowing only (13–17.5 %), well-circumscribed mass (about 4 %), infiltrative pattern (about 4 %), focal hyperechoic lesion (1–5 %) or no abnormality (2–4 %) [76, 88]. Infiltrative pattern is due to the extension of ILC into Cooper’s ligaments creating bizarre us-images called “Golden Gate sign”, “gloved hand” or “cactus”.
Ultrasound is moreover the guidance method of choice in the case of fine needle aspiration cytology (FNAC) or biopsy. The positivity of FNAC may be lower than expectations: in the literature, 60–80 % is reported, this being due to the sparse cellularity and the presence of small relatively normal-appearing cells [76, 79, 89].
Both mammography and ultrasound tend to underestimate lesion size and are therefore not optimal for staging purposes [81, 90].
Tomosynthesis is a new technique that seems to have a higher sensitivity and specificity than digital mammography in the detection of lesions in dense breast parenchyma according to the reduced or eliminated overlapping breast tissue [91, 92]. It seems to be a promising tool; however, there is no significant published data in the literature and further studies are needed.
Compared to conventional imaging, MRI seems to be the modality of choice for the evaluation of ILC. It is more sensitive in detecting ILC and determining the size extent and presence of multiple or contralateral foci [81, 93].
A recent meta-analysis conducted on 21 studies shows sensitivity ranging from 83 to 100 % (mean 93.3 %), equal to the overall sensitivity of MRI for malignant lesion of the breast [81].
At MRI evaluation, ILC appears as a mass-like lesion (with irregular or spiculated margins) more frequently than as a non-mass lesion (with abnormal enhancement such as regional, ductal, segmental or diffuse enhancement) [81].
There is data to support how MRI changes surgical management in 28.3 % of cases; however, there is no evidence suggesting an increase in survival for patients with ILC due to the performance of MRI [81, 94].
Recommendations from the European Society of Breast Cancer Specialists (EUSOMA) working group for the staging before treatment planning suggest that MRI should be performed in the pre-operative assessment of patients with biopsy-proven ILC [95]. Similarly, in the UK, the National Institute for Health and Care Excellence (NICE) published clinical guidelines recommending MRI in this group of patients if breast-conserving surgery is being considered [96].
MRI is routinely used for breast screening in high-risk women with BRCA1 or BRCA2 gene mutations. As yet, there are no guidelines regarding MRI use in women with CDH1 mutations.
Breast screening in CDH1-mutated patients should be performed periodically using digital mammography, ultrasound and MRI.
10 Prophylactic mastectomy
BC is the most frequent cancer among women with an estimated 1.38 million new cancer cases diagnosed in 2008 (23 % of all cancers) and ranks second overall (10.9 % of all cancers). About 690,000 new cases are diagnosed every year, and it ranks as the fifth cause of death from cancer overall (458,000 deaths) [1]. Genetic predisposition accounts for only 5 to 10 % of BC, and younger women diagnosed with BC are at a higher risk for a genetic aetiology [97]. In 1998, the National Comprehensive Cancer Network (NCCN) established that genetic counselling should be proposed in the following BC cases: women with age at onset 50 years or younger, triple-negative, two or more events in one individual, male, woman of Ashkenazi Jewish descent and tumours at any age with a family history of breast and/or ovarian cancer [98]. BRCA 1/2 germline mutant carriers are eligible for prophylactic “nipple-sparing mastectomy” (NSM) with immediate plastic reconstruction. This surgical procedure entails nipple-areola complex (NAC) preservation [99]. NSM requires a double-time approach, gland dissection and the reconstructive surgery. The gland is dissected very close to the dermis, retaining a thin layer of subcutaneous fat to preserve the subdermal vascularization [100, 101]. Lateral or inframammary skin surgical incision (4–5 cm) provides a better view during the subcutaneous dissection, and this approach offers an opportunity to check the retroareolar histology. Glandular tissue is removed bordering the retroareolar area to avoid any gland residual tissue [99]. Currently, there is no indication for prophylactic NSM in CDH1 germline asymptomatic mutant carriers. Further studies will clarify the CDH1 genetic penetrance and the LBC risk development, and NSM could be considered in selected patients.
11 Concluding remarks
The clinical approach to individuals with a suspicious inherited predisposition for gastric and breast tumours requires, for targeted management, close collaboration between the geneticist for testing, the surgeon, the gastroenterologist and the pathologist.
The first approach requires the description of a detailed pedigree, providing information about affected members, gender and age at onset, cancer diagnosis, histotype features, outcome and lifestyle. The Cambridge clinical criteria help to understand when GC is sporadic or hereditary; in particular, management of GC with suspicious familial or hereditary firstly requires a pedigree with at least knowledge of three member generations, and when analysed pedigree overlaps the clinical criteria, genetic testing is mandatory. The identification of a germline alteration requires a specific treatment in asymptomatic patients, in particular in CDH1 mutation carriers in the HDGC syndrome. Unfortunately, cases with familial aggregation and without specific gene involvement are the majority and represent an urgent clinical burden considering that familial GC, unlike its sporadic form, shows an increasing trend, in particular, in cases with diffuse gastric carcinoma.
The IGCLC in 2010 recommended PTG for the treatment of asymptomatic truncating CDH1 mutation carriers [15]. To date, more than 100 gastrectomies have been performed in deleterious E-cadherin mutation carriers. The choice of prophylactic surgery or endoscopic surveillance in pathogenic missense mutation carriers is still a subject of ongoing debate. The number of cases with missense mutations treated with prophylactic surgery is rather low to reach a definitive conclusion. However, additional genetic tests, such as in vitro and in silico analyses, are required to assess the pathogenicity of CDH1 germline missense mutations.
With this novel clinical review, we would introduce a new concept of “hereditary breast cancer” associated with the E-cadherin germline mutations, never defined so far. In particular, LBC is a CDH1-associated cancer disease, forming part of the HDGC syndrome. However, recent studies have led to the discovery of novel CDH1 germline mutations in LBC patients in the absence of family history for GC. Further genetic studies should define whether LBC represents an independent cancer syndrome, offer a definitive treatment for these patients and define the BC risk in unaffected young women. At present, in CDH1 germline mutation carriers, there is no indication for prophylactic mastectomy. Nonetheless, we have strongly suggested clinical and instrumental follow-up of the breast. Firstly, this report described in detail the clinical management for asymptomatic CDH1 germline mutation carriers with the only family history for LBC.
References
Ferlay, J., Shin, H. R., Bray, F., Forman, D., Mathers, C., Parkin, D. M., et al. (2010). Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. International Journal of Cancer, 127(12), 2893–2917.
Cisco, R. M., Ford, J., & Norton, J. A. (2008). Hereditary diffuse gastric cancer. Implications of genetic testing for screening and prophylactic surgery. Cancer, 113, 1850–1856.
Guilford, P., Hopkins, J., Harraway, J., McLeod, M., McLeod, N., Harawira, P., et al. (1998). E-cadherin germline mutations in familial gastric cancer. Nature, 392(6674), 402–405.
Kaurah, P., MacMillan, A., Boyd, N., et al. (2007). Founder and recurrent CDH1 mutations in families with hereditary diffuse gastric cancer. JAMA, 297, 2360–72.
Gayther, S. A., Gorringer, K. L., Ramus, S. J., Huntsman, D., Roviello, F., Grehan, N., et al. (1998). Identification of germline E-cadherin mutations in gastric cancer families of European origin. Cancer Research, 58(18), 4085–4089.
Pharoah, P. D., Guilford, P., & Caldas, C. (2001). Incidence of gastric cancer and breast cancer in CDH1 (E-cadherin) mutation carriers from hereditary diffuse gastric cancer families. Gastroenterology, 121, 1348–1353.
Huntsman, D. G., Carneiro, F., Lewis, F. R., MacLeod, P. M., Hayashi, A., Monaghan, K. G., et al. (2001). Early gastric cancer in young, asymptomatic carriers of germ-line E-cadherin mutations. New England Journal of Medicine, 344, 1904–1909.
Chun, Y. S., Lindor, N. M., Smyrk, T. C., Petersen, B. T., Burgart, L. J., Guilford, P. J., et al. (2001). Germline E-cadherin gene mutations: is prophylactic total gastrectomy indicated? Cancer, 92, 181–187.
Lewis, F. R., Mellinger, J. D., Hayashi, A., Lorelli, D., Monaghan, K. G., Carneiro, F., et al. (2001). Prophylactic total gastrectomy for familial gastric cancer. Surgery, 130, 612–617. discussion 617–619.
Newman, E. A., & Mulholland, M. W. (2006). Prophylactic gastrectomy for hereditary diffuse gastric cancer syndrome. Journal of the American College of Surgeons, 202(4), 612–617.
Lynch, H. T., Kaurah, P., Wirtzfeld, D., Rubinstein, W. S., Weissman, S., Lynch, J. F., et al. (2008). Hereditary diffuse gastric cancer: diagnosis, genetic counseling, and prophylactic total gastrectomy. Cancer, 112(12), 2655–2663.
Benusiglio, P. R., Malka, D., Rouleau, E., De Pauw, A., Buecher, B., Noguès, C., et al. (2013). CDH1 germline mutations and the hereditary diffuse gastric and lobular breast cancer syndrome: a multicentre study. Journal of Medical Genetics, 50(7), 486–489.
Petridis, C., Shinomiya, I., Kohut, K., Gorman, P., Caneppele, M., Shah, V., et al. (2014). Germline CDH1 mutations in bilateral lobular carcinoma in situ. British Journal of Cancer, 110(4), 1053–1057.
Hebbard, P. C., MacMillan, A., Huntsman, D., Kaurah, P., Carneiro, F., Wen, X., et al. (2009). Prophylactic total gastrectomy (PTG) for hereditary diffuse gastric cancer (HDGC): the Newfoundland experience with 23 patients. Annals of Surgical Oncology, 16, 1890–1895.
Fitzgerald, R. C., Hardwick, R., Huntsman, D., Carneiro, F., Guilford, P., Blair, V., Consortium, I. G. C. L., et al. (2010). Hereditary diffuse gastric cancer: updated consensus guidelines for clinical management and directions for future research. Journal of Medical Genetics, 47, 436–444.
Corso, G., Pedrazzani, C., Pinheiro, H., Fernandes, E., Marrelli, D., Rinnovati, A., et al. (2011). E-cadherin genetic screening and clinico-pathologic characteristics of early onset gastric cancer. European Journal of Cancer, 47(4), 631–639.
Lindor, N. M., McMaster, M. L., Lindor, C. J., & Green, M. H. (2008). Concise handbook of familial cancer susceptibility syndromes—second edition. Journal of the National Cancer Institute Monographs, 38, 1–93.
Schatzkin, A., Goldstein, A., & Freedman, L. S. (1995). What does it mean to be a cancer gene carrier? Problems in establishing causality from the molecular genetics of cancer. Journal of the National Cancer Institute, 87(15), 1126–1130.
Lauren, P. A., & Nevalainen, T. J. (1993). Epidemiology of intestinal and diffuse types of gastric carcinoma. A time-trend study in Finland with comparison between studies from high- and low-risk areas. Cancer, 71, 2926–2929.
El-Rifai, W., & Powell, S. M. (2002). Molecular and biologic basis of upper gastrointestinal malignancy. Gastric carcinoma. Surgical Oncology Clinics of North America, 11, 273–291.
Oliveira, C., Seruca, R., & Carneiro, F. (2009). Hereditary gastric cancer. Best Practice & Research Clinical Gastroenterology, 23(2), 147–157.
Brooks-Wilson, A. R., Kaurah, P., Suriano, G., et al. (2004). Germline E-cadherin mutations in hereditary diffuse gastric cancer: assessment of 42 new families and review of genetic screening criteria. Journal of Medical Genetics, 41(7), 508–517.
Suriano, G., Yew, S., Ferreira, P., Senz, J., Kaurah, P., Ford, J. M., et al. (2005). Characterization of a recurrent germ line mutation of the E-cadherin gene: implications for genetic testing and clinical management. Clinical Cancer Research, 11(15), 5401–5409.
Birch, J. M., Alston, R. D., McNally, R. J., Evans, D. G., Kelsey, A. M., Harris, M., et al. (2001). Relative frequency and morphology of cancers in carriers of germline TP53 mutations. Oncogene, 20(34), 4621–4628.
Corso, G., Marrelli, D., & Roviello, F. (2011). Familial gastric cancer: update for practice management. Familial Cancer, 10(2), 391–396.
Capelle, L. G., Van Grieken, N. C., Lingsma, H. F., Steyerberg, E. W., Klokman, W. J., Bruno, M. J., et al. (2010). Risk and epidemiological time trends of gastric cancer in Lynch syndrome carriers in the Netherlands. Gastroenterology, 138(2), 487–492.
Jeghers, K., McKusick, V. A., & Katz, K. H. (1949). Generalized intestinal polyposis and melanin spots of the oral mucosa, lips and digits; a syndrome of diagnostic significance. New England Journal of Medicine December, 241(26), 1031–1036.
Blair, V., Martin, I., Shaw, D., Winship, I., Kerr, D., Arnold, J., et al. (2006). Hereditary diffuse gastric cancer: diagnosis and management. Clinical Gastroenterology and Hepatology, 4, 262–275.
Kluijt, I., Siemerink, E. J., Ausems, M. G., et al. (2012). CDH1-related hereditary diffuse gastric cancer syndrome: clinical variations and implications for counseling. International Journal of Cancer, 131(2), 367–376.
Lauren, P. (1965). The Two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathologica et Microbiologica Scandinavica, 64, 31–49.
Guilford, P. J., Hopkins, J. B., Grady, W. M., Markowitz, S. D., Willis, J., Lynch, H., et al. (1999). E-cadherin germline mutations define an inherited cancer syndrome dominated by diffuse gastric cancer. Human Mutation, 14(3), 249–255.
Oliveira, C., Seruca, R., & Carneiro, F. (2009). Hereditary gastric cancer. Best Practice & Research Clinical Gastroenterology, 23(2), 147–157.
Roviello, F., Corso, G., Pedrazzani, C., Marrelli, D., De Falco, G., Suriano, G., et al. (2007). High incidence of familial gastric cancer in Tuscany, a region in Italy. Oncology, 72(3–4), 243–247.
Oliveira, C., Senz, J., Kaurah, P., Pinheiro, H., Sanges, R., Haegert, A., et al. (2009). Germline CDH1 deletions in hereditary diffuse gastric cancer families. Human Molecular Genetics, 18(9), 1545–1555.
Oliveira, C., Pinheiro, H., Figueiredo, J., Seruca, R., & Carneiro, F. (2013). E-cadherin alterations in hereditary disorders with emphasis on hereditary diffuse gastric cancer. Progress in Molecular Biology and Translational Science, 116, 337–359.
Suriano, G., Oliveira, C., Ferreira, P., Machado, J. C., Bordin, M. C., De Wever, O., et al. (2003). Identification of CDH1 germline missense mutations associated with functional inactivation of the E-cadherin protein in young gastric cancer probands. Human Molecular Genetics, 12(5), 575–582.
More, H., Humar, B., Weber, W., Ward, R., Christian, A., Lintott, C., et al. (2007). Identification of seven novel germline mutations in the human E-cadherin (CDH1) gene. Human Mutation, 28(2), 203.
Fitzgerald, R. C., & Caldas, C. (2004). Clinical implications of E-cadherin associated hereditary diffuse gastric cancer. Gut, 53(6), 775–778.
Suriano, G., Seixas, S., Rocha, J., & Seruca, R. (2006). A model to infer the pathogenic significance of CDH1 germline missense variants. Journal of Molecular Medicine (Berlin), 84(12), 1023–1031.
Simoes-Correia, J., Figueiredo, J., Lopes, R., Stricher, F., Oliveira, C., Serrano, L., et al. (2012). E-cadherin destabilization accounts for the pathogenicity of missense mutations in hereditary diffuse gastric cancer. PloS One, 7(3), e33783.
Figueiredo, J., Soderberg, O., Simoes-Correia, J., Grannas, K., Suriano, G., Seruca, R., et al. (2013). The importance of E-cadherin binding partners to evaluate the pathogenicity of E-cadherin missense mutations associated to HDGC. European Journal of Human Genetics, 21(3), 301–309.
Suriano, G., Mulholland, D., de Wever, O., et al. (2003). The intracellular E-cadherin germline mutation V832 M lacks the ability to mediate cell-cell adhesion and to suppress invasion. Oncogene, 22(36), 5716–5719.
Brooks-Wilson, A. R., Kaurah, P., Suriano, G., Ferreira, P., Mateus, A. R., Bruyneel, E., et al. (2004). Germline E-cadherin mutations in hereditary diffuse gastric cancer: assessment of 42 new families and review of genetic screening criteria. Journal of Medical Genetics, 41(7), 508–517.
Keller, G., Vogelsang, H., Becker, I., et al. (2004). Germline mutations of the E-cadherin(CDH1) and TP53 genes, rather than of RUNX3 and HPP1, contribute to genetic predisposition in German gastric cancer patients. Journal of Medical Genetics, 41(6), e89.
Corso, G., Roviello, F., Paredes, J., Plaschke, S., Ott, K., Suriano, G., et al. (2007). Characterization of the P373L E-cadherin germline missense mutation and implication for clinical management. European Journal of Surgical Oncology, 33(9), 1061–1067.
Simoes-Correia, J., Figueiredo, J., Oliveira, C., van Hengel, J., Seruca, R., van Roy, F., et al. (2008). Endoplasmic reticulum quality control: a new mechanism of E-cadherin regulation and its implication in cancer. Human Molecular Genetics, 17(22), 3566–3576.
Vogelaar, I. P., Figueiredo, J., van Rooij, I. A., Simões-Correia, J., van der Post, R. S., Melo, S., et al. (2013). Identification of germline mutations in the cancer predisposing gene CDH1 in patients with orofacial clefts. Human Molecular Genetics, 22(5), 919–926.
Garziera, M., De Re, V., Geremia, S., Seruca, R., Figueiredo, J., Melo, S., et al. (2013). A novel CDH1 germline missense mutation in a sporadic gastric cancer patient in north-east of Italy. Clinical and Experimental Medicine, 13(2), 149–157.
Handschuh, G., Candidus, S., Luber, B., Reich, U., Schott, C., Oswald, S., et al. (1999). Tumour-associated E-cadherin mutations alter cellular morphology, decrease cellular adhesion and increase cellular motility. Oncogene, 18(30), 4301–4312.
Mateus, A. R., Seruca, R., Machado, J. C., Keller, G., Oliveira, M. J., Suriano, G., et al. (2007). EGFR regulates RhoA-GTP dependent cell motility in E-cadherin mutant cells. Human Molecular Genetics, 16(13), 1639–1647.
Mateus, A. R., Simoes-Correia, J., Figueiredo, J., et al. (2009). E-cadherin mutations and cell motility: a genotype-phenotype correlation. Experimental Cell Research, 315(8), 1393–1402.
Suriano, G., Oliveira, M. J., Huntsman, D., Heindl, S., Alves, C. C., Suriano, G., et al. (2003). E-cadherin germline missense mutations and cell phenotype: evidence for the independence of cell invasion on the motile capabilities of the cells. Human Molecular Genetics, 12(22), 3007–3016.
Ferreira, P., Oliveira, M. J., Beraldi, E., Mateus, A. R., Nakajima, T., Gleave, M., et al. (2005). Loss of functional E-cadherin renders cells more resistant to the apoptotic agent taxol in vitro. Experimental Cell Research, 310(1), 99–104.
Ferreira, A. C., Suriano, G., Mendes, N., Gomes, B., Wen, X., Carneiro, F., et al. (2012). E-cadherin impairment increases cell survival through Notch-dependent upregulation of Bcl-2. Human Molecular Genetics, 21(2), 334–343.
Figueiredo, J., Simoes-Correia, J., Soderberg, O., Suriano, G., & Seruca, R. (2011). ADP-ribosylation factor 6 mediates E-cadherin recovery by chemical chaperones. PloS One, 6(8), e23188.
Chen, Y., Kingham, K., Ford, J. M., Rosing, J., Van Dam, J., Jeffrey, R. B., et al. (2001). A prospective study of total gastrectomy for CDH1-positive hereditary diffuse gastric cancer. Annals of Surgical Oncology, 18(9), 2594–2598.
Guilford, P., Humar, B., & Blair, V. (2010). Hereditary diffuse gastric cancer: translation of CDH1 germline mutation into clinical practice. Gastric Cancer, 13, 1–10.
Roviello, F., Rossi, S., Marrelli, D., Pedrazzani, C., Corso, G., Vindigni, C., et al. (2006). Number of lymph node metastases and its prognostic significance in early gastric cancer: a multicenter Italian study. Journal of Surgical Oncology, 94(4), 275–280. discussion 274.
Kitagawa, Y., Fujii, H., Mukai, M., Kubota, T., Otani, Y., & Kitajima, M. (2002). Radio-guided sentinel node detection for gastric cancer. British Journal of Surgery, 89, 604–608.
Hayashi, H., Ochiai, T., Mori, M., Karube, T., Suzuki, T., Gunji, Y., et al. (2003). Sentinel lymph node mapping for gastric cancer using a dual procedure with dye- and gamma probe-guided techniques. Journal of the American College of Surgery, 196, 68–74.
Lenhert, T., & Buhl, K. (2004). Techniques of reconstruction after total gastrectomy for cancer. British Journal of Surgery, 91, 528–539.
Sharma, D. (2004). Choice of digestive tract reconstructive procedure following total gastrectomy: a critical reappraisal. Indian Journal of Surgery, 66, 270–276.
Fein, M., Fuchs, K. H., Thalheimer, A., Freys, S. M., Heimbucher, J., Thiede, A., et al. (2008). Long-term benefits of Roux-en-Y pouch reconstruction after total gastrectomy: a randomized trial. Annals of Surgery, 247(5), 759–765.
Peyre, C. G., DeMeester, S. R., Rizzetto, C., Bansal, N., Tang, A. L., Ayazi, S., et al. (2007). Vagal-sparing esophagectomy: the ideal operation for intramucosal adenocarcinoma and Barrett with high-grade dysplasia. Annals of Surgery, 246, 665–671.
Usui, S., Yoshida, T., Ito, K., Hiranuma, S., Kudo, S. E., & Iwai, T. (2005). Laparoscopy-assisted total gastrectomy for early gastric cancer: comparison with conventional open total gastrectomy. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques, 15(6), 309–314.
Yoon, H. M., Kim, Y. W., Lee, J. H., Ryu, K. W., Eom, B. W., Park, J. Y., et al. (2012). Robot-assisted total gastrectomy is comparable with laparoscopically assisted total gastrectomy for early gastric cancer. Surgical Endoscopy, 26(5), 1377–1381.
Chen, K., Xu, X. W., Zhang, R. C., Pan, Y., Wu, D., & Mou, Y. P. (2013). Systematic review and meta-analysis of laparoscopy-assisted and open total gastrectomy for gastric cancer. World Journal of Gastroenterology, 19(32), 5365–5376.
Worster, E., Liu, X., Richardson, S., Hardwick, R.H., Dwerryhouse, S., Caldas, C., et al. (2014). The impact of prophylactic total gastrectomy on health-related quality of life. A prospective cohort study. Ann Surg, Jan 13. [Epub ahead of print].
Blair, V. R. (2012). Familial gastric cancer: genetics, diagnosis, and management. Surgical Oncology Clinics of North America, 21(1), 35–56.
Barber, M. E., Save, V., Carneiro, F., Dwerryhouse, S., Lao-Sirieix, P., Hardwick, R. H., et al. (2008). Histopathological and molecular analysis of gastrectomy specimens from hereditary diffuse gastric cancer patients has implications for endoscopic surveillance of individuals at risk. Journal of Pathology, 216(3), 286–294.
Charlton, A., Blair, V., Shaw, D., Parry, S., Guilford, P., & Martin, I. G. (2004). Hereditary diffuse gastric cancer: predominance of multiple foci of signet ring cell carcinoma in distal stomach and transitional zone. Gut, 53, 814–820.
Carneiro, F., Huntsman, D. G., Smyrk, T. C., Owen, D. A., Seruca, R., Pharoah, P., et al. (2004). Model of the early development of diffuse gastric cancer in E-cadherin mutation carriers and its implications for patient screening. Journal of Pathology, 203, 681–687.
Rogers, W. M., Dobo, E., Norton, J. A., Van Dam, J., Jeffrey, R. B., Huntsman, D. G., et al. (2008). Risk-reducing total gastrectomy for germline mutations in E-cadherin (CDH1): pathologic findings with clinical implications. American Journal of Surgical Pathology, 32, 799–809.
Fujita, H., Lennerz, J. K., Chung, D. C., Patel, D., Deshpande, V., Yoon, S. S., et al. (2012). Endoscopic surveillance of patients with hereditary diffuse gastric cancer: biopsy recommendations after topographic distribution of cancer foci in a series of 10 CDH1-mutated gastrectomies. American Journal of Surgical Pathology, 36, 1709–1717.
Lim, Y. C., di Pietro, M., O’Donovan, M., Richardson, S., Debiram, I., Dwerryhouse, S., et al. (2014). Prospective cohort study assessing outcomes of patients from families fulfilling criteria for hereditary diffuse gastric cancer undergoing endoscopic surveillance. Gastrointestinal Endoscopy. doi:10.1016/j.gie.2013.11.040.
Porter, A. J., Evans, E. B., Foxcroft, L. M., Simpson, P. T., & Lakhani, S. R. (2014). Mammographic and ultrasound features of invasive lobular carcinoma of the breast. Journal of Medical Imaging and Radiation Oncology, 58(1), 1–10.
Moll, R., Mitze, M., Frixen, U. H., & Birchmeier, W. (1993). Differential loss of E-cadherin expression in infiltrating ductal and lobular breast carcinomas. American Journal of Pathology, 143(6), 1731–1742.
Yeatman, T. J., Cantor, A. B., Smith, T. J., Smith, S. K., Reintgen, D. S., Miller, M. S., et al. (1995). Tumor biology of infiltrating lobular carcinoma. Implications for management. Annals of Surgery, 222(4), 549–561.
Le Gal, M., Ollivier, L., Asselain, B., Meunier, M., Laurent, M., Vielh, P., et al. (1992). Mammographic features of 455 invasive lobular carcinomas. Radiology, 185(3), 705–708.
Brem, R. F., Ioffe, M., Rapelyea, J. A., Yost, K. G., Weigert, J. M., Bertrand, M. L., et al. (2009). Invasive lobular carcinoma: detection with mammography, sonography, MRI, and breast-specific gamma imaging. American Journal of Roentgenology, 192(2), 379–383.
Mann, R. M., Hoogeveen, Y. L., Blickman, J. G., & Boetes, C. (2008). MRI compared to conventional diagnostic work-up in the detection and evaluation of invasive lobular carcinoma of the breast: a review of existing literature. Breast Cancer Research and Treatment, 107(1), 1–14.
Selinko, V. L., Middleton, L. P., & Dempsey, P. J. (2004). Role of sonography in diagnosing and staging invasive lobular carcinoma. Journal of Clinical Ultrasound, 32(7), 323–332.
Hilleren, D. J., Andersson, I. T., Lindholm, K., & Linnell, F. S. (1991). Invasive lobular carcinoma: mammographic findings in a 10-year experience. Radiology, 178(1), 149–154.
Vlug, E., Ercan, C., van der Wall, E., van Diest, P. J., & Derksen, P. W. (2014). Lobular breast cancer: pathology, biology, and options for clinical intervention. Archivum Immunologiae et Therapiae Experimentalis (Warsz), 62(1), 7–21.
Albayrak, Z. K., Onay, H. K., Karatağ, G. Y., Karatağ, G. Y., & Karatağ, O. (2011). Invasive lobular carcinoma of the breast: mammographic and sonographic evaluation. Diagnostic and Interventional Radiology, 17(3), 232–238.
Krecke, K. N., & Gisvold, J. J. (1993). Invasive lobular carcinoma of the breast: mammographic findings and extent of disease at diagnosis in 184 patients. American Journal of Roentgenology, 161(5), 957–960.
Berg, W. A., Gutierrez, L., NessAiver, M. S., Carter, W. B., Bhargavan, M., Lewis, R. S., & Ioffe, O. B. (2004). Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer. Radiology, 233(3), 830–849.
Jones, K. N., Magut, M., Henrichsen, T. L., Boughey, J. C., Reynolds, C., & Glazebrook, K. N. (2013). Pure lobular carcinoma of the breast presenting as a hyperechoic mass: incidence and imaging characteristics. American Journal of Roentgenology, 201(5), W765–769.
Tan, S. M., Behranwala, K. A., Trott, P. A., Nasiri, N. A., Moskovic, E., Brown, G., et al. (2002). A retrospective study comparing the individual modalities of triple assessment in the pre-operative diagnosis of invasive lobular breast carcinoma. European Journal of Surgical Oncology, 28(3), 203–208.
Watermann, D. O., Tempfer, C., Hefler, L. A., Parat, C., & Stickeler, E. (2005). Ultrasound morphology of invasive lobular breast cancer is different compared with other types of breast cancer. Ultrasound in Medicine and Biology, 31(2), 167–174.
Lei, J., Yang, P., Zhang, L., Wang, Y., & Yang, K. (2014). Diagnostic accuracy of digital breast tomosynthesis versus digital mammography for benign and malignant lesions in breasts: a meta-analysis. European Radiology, 24(3), 595–602.
Mariscotti, G., Houssami, N., Durando, M., Bergamasco, L., Campanino, P. P., Ruggieri, C., et al. (2014). Accuracy of mammography, digital breast tomosynthesis, ultrasound and MR imaging in preoperative assessment of breast cancer. Anticancer Research, 34(3), 1219–1225.
Oliveira, T. M., Elias, J., Jr., Melo, A. F., Teixeira, S. R., Filho, S. C., Gonçalves, L. M., et al. (2014). Evolving concepts in breast lobular neoplasia and invasive lobular carcinoma, and their impact on imaging methods. Insights Imaging, 5(2), 183–194.
Muttalib, M., Ibrahem, R., Khashan, A. S., & Hajaj, M. (2014). Prospective MRI assessment for invasive lobular breast cancer. Correlation with tumour size at histopathology and influence on surgical management. Clinical Radiology, 69(1), 23–28.
Sardanelli, F., Boetes, C., Borisch, B., Decker, T., Federico, M., Gilbert, F. J., et al. (2010). Magnetic resonance imaging of the breast: recommendations from the EUSOMA working group. European Journal of Cancer, 46(8), 1296–1316.
NHS National Institute for Health and Clinical Excellence. NICE clinical guideline 80. Early and locally advanced breast cancer: diagnosis and treatment. Available at: http://www.nice.org.uk/nicemedia/pdf/CG80NICEGuideline.pdf.
Stuckey, A., Febbraro, T., Laprise, J., Wilbur, J.S., Lopes, V., Robison, K. (2014). Adherence patterns to national comprehensive cancer network guidelines for referral of women with breast cancer to genetics professionals. Am J Clin Oncol, Apr 5. [Epub ahead of print].
Winn, R. J., Botnick, W. Z., & Brown, N. H. (1998). The NCCN guideline program–1998. Oncology (Williston Park), 12(11A), 30–34.
Cataliotti, L., Galimberti, V., & Mano, M. P. (2010). The nipple sparing mastectomy (NSM). Attualità in Senologia, 59, 11–20.
Larson, D. L., Basir, Z., & Bruce, T. (2011). Is oncologic safety compatible with a predictably viable mastectomy skin flap? Plastic and Reconstructive Surgery, 127(1), 27–33.
Petit, J. Y., Veronesi, U., Lohsiriwat, V., Rey, P., Curigliano, G., Martella, S., et al. (2011). Nipple-sparing mastectomy—is it worth the risk? Nature Reviews. Clinical Oncology, 8(12), 742–747. 25.
Acknowledgments
We acknowledge Russell Edu Samuel William for the support in editing the draft of this manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Corso, G., Figueiredo, J., Biffi, R. et al. E-cadherin germline mutation carriers: clinical management and genetic implications. Cancer Metastasis Rev 33, 1081–1094 (2014). https://doi.org/10.1007/s10555-014-9528-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-014-9528-y