Abstract
To evaluate the contribution and performance of multimodal imaging in the diagnostic and therapeutic management of cardiac masses. We carried out a monocentric retrospective study on patients referred for cardiac mass assessment between 2006 and 2019, and analyzed the respective contribution of transesophageal echocardiography (TEE), cardiac computed tomography (CT), cardiac magnetic resonance (CMR) and 18F-fluorodeoxyglucose positron emission tomography coupled with CT (18F-FDG PET-CT). For each test, we determined strategy before and after its completion (need for another imaging or decision-making) as well as result on benign, malignant or indeterminate nature. For the 119 patients included, all imaging modalities increased decision-making rates, which rose from 2 to 54%, 23 to 62%, 31 to 85% and 49 to 100% before and after TEE, CT, CMR and 18F-FDG PET-CT, respectively (P < 0.001 before vs. after). TEE was particularly efficient for atrial masses, especially for the left atrium, with a decision rate rising from 0 to 74% (P < 0.001). 18F-FDG PET-CT was the most efficient to differentiate benign and malignant etiologies (area under the curve 0.89 ± 0.06 and 0.94 ± 0.05 for benign and malignant, respectively, P < 0.001). A benign or undetermined result on each modality was associated with a good prognosis, compared to malignant. All modalities studied are useful for cardiac mass decision-making. First-line TEE is particularly efficient for atrial masses, whereas CT and CMR are useful for ventricular masses or suspicion of malignancy. A benign or malignant result for each modality is correlated to survival and 18F-FDG PET-CT is the most effective to define it.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiac masses are rare: a large autopsy series reported an incidence of 0.056% for primary masses and 1.23% for secondary tumors [1]. They represent a heterogeneous group including benign, malignant and non-tumoral masses. Malignant tumors can be divided into primary or secondary (metastasis or local invasion) neoplasms, but metastases are much more frequent [1, 2]. Among primary tumors, benign masses are the most common. The most frequent non-tumoral masses are thrombi or prominent anatomical structures (prominent crista terminalis, lipomatous hypertrophy of the atrial septum) [1].
Diagnosis may be difficult and there are no guidelines on the diagnostic algorithm. The gold standard for diagnosis is histological evidence, which requires surgery or biopsy and can be difficult to perform. Consequently, initial assessment is usually based on non-invasive tools including clinical history, laboratory tests and cardiovascular imaging. Several imaging modalities can be used, with echocardiography, transthoracic (TTE) and then transesophageal echocardiography (TEE) at the forefront. Then come cardiac computed tomography (CT) and cardiac magnetic resonance (CMR), which cannot be performed at the patient's bedside, followed by positron emission tomography with computed tomography using 18F-fluorodesoxyglucose (18F-FDG PET-CT), which is performed by tertiary centers. TTE is usually the first- line test performed to characterize the lesion and seek a hemodynamic repercussion. Regarding the use of other tests, the strategy is adapted on a case-by-case basis, without diagnostic algorithm guidelines due to the lack of performance data in the context of rare diseases. Multidisciplinary management is always required to decide therapeutic management and before any invasive action.
The main aim of our study was to evaluate the performance and the decision-making impact of multimodal imaging, including TEE, cardiac CT, CMR and 18F-FDG PET-CT among patients with cardiac masses.
Methods
Study population
Consecutive patients referred to the Toulouse University Hospital, Toulouse, France, for diagnostic workup or management of a cardiac mass from 2006 to 2019, were retrospectively included. Two distinct databases were crossed to select patients referred for diagnostic assessment or surgical management of cardiac mass (diagnosis related groups of cardiac mass): hospital electronic health record and hospital echocardiographic report database. Patients with valve tumors or infectious endocarditis were then excluded. Obvious thrombi, including masses on central catheter, were also excluded because they presented the least diagnostic challenge.
All the data were collected as part of the standard diagnostic workup. The investigation conforms to the principles outlined in the Declaration of Helsinki. All patients were informed on admission that their clinical data could be used for research purposes and all gave their consent. In accordance with applicable standards in France, this study has received ethics committee approval from the French Data Protection Authority and has been approved by our institutional review board (MR 004-no. 2019-69).
Demographic, clinical and biological data
Patient electronic and paper records were consulted and the following parameters were extracted: age, gender, history of malignancy (active or in remission), cardiovascular risk factors, drugs (anticoagulation, antiplatelet therapy, chemotherapy, radiotherapy), presence or absence of electrocardiographic abnormalities, laboratory results (hemoglobin, creatinine, C reactive protein, natriuretic peptides, troponin), symptoms (asthenia, heart failure, chest pain, palpitations, syncope) and the therapeutic decision.
Cardiac imaging tests
For each patient, all cardiac imaging tests performed including TEE, CMR, CT and 18F-FDG PET-CT, were collected and analyzed for final interpretation and positioning in the diagnostic workup. TTE was considered as the first-line test performed for all patients and was not analyzed. TEE was considered as the second-line test. CT and CMR were considered as the third- line tests, followed by 18F-FDG PET-CT. This choice to prioritize the tests was made with regard to clinical practice, the availability of the tests and in such a way as not to introduce any bias in the analysis, since in many cases, all the tests were carried out together regardless of their mutual results.
Strategy before and after each test was determined as follows: need for further cardiac imaging modalities or decision-making, which could be: biopsy, surgery, anticoagulation, anti-neoplastic treatment (radiotherapy/chemotherapy) or medical follow-up. These options could be associated.
Finally, data on the ability of the test to classify into benign, malign or indeterminate was collected. The benign or malignant nature of the mass on the basis of each modality results was based on the anatomy and signal/density/contrast enhancement of the mass and local–regional extension. For 18F-FDG PET-CT results the benign or malignant nature of the mass was based on radiotracer uptake intensity using qualitative assessment (mass uptake intensity as compared to liver uptake intensity) and presence of other lesion in another localization. All indeterminate results were discussed by expert consensus.
Only masses with a definitive diagnosis have been selected to evaluate the capacity of each imaging modality to determine the benign or malignant nature of the mass.
Gold-standard diagnosis
For each imaging modality, the histological result was considered as the gold standard for the definitive diagnosis. Tissue samples were analyzed in the Department of Pathology of the Toulouse University Hospital, Toulouse, France. Diagnostic doubt and sarcomas were re-analyzed by an expert center and/or reference network.
For suspected thrombus, a compatible aspect with disappearance after a period of anticoagulation was considered as a definitive diagnosis. Concerning lipomas and lipomatous hypertrophy of the atrial septum, in the absence of histological analysis, we considered that a typical aspect on CT and/or CMR was pathognomonic and was a reference diagnosis equivalent.[3]. The same attitude was adopted concerning typical prominent crista terminalis.
Outcome assessment
Follow-up was assessed by electronic chart review or by phone interview of the patient’s general practitioner/cardiologist, patient or family for the clinical endpoint of all-cause mortality. Follow-up was terminated at 100 months. No patient was lost to follow-up.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation. Nominal values were expressed as numbers and percentages. Association between the mean values of continuous variables was compared using the Mann–Whitney rank sum test. Nominal variables were investigated by the Fisher exact test. The accuracy of imaging measures for predicting benign or malign etiologies was assessed by computing the areas under the receiver operating characteristic (ROC) curves and the best cut-off value was defined as the point with the highest sum of sensitivity and specificity. Finally, all-cause mortality was summarized using Kaplan–Meier survival curve with the cut-off of imaging measures previously retained and log rank test was used for initial comparisons. Differences were considered statistically significant for P-values of < 0.05. All analyses were performed using standard statistical software SPSS version 20 (SPSS Inc., Chicago, Illinois).
Results
Baseline characteristics and epidemiology
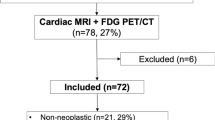
One hundred and nineteen patients with cardiac masses were retrospectively included. Baseline characteristics of the whole population and according to the benign or malignant etiology are presented in Table 1. There were 70 (59%) men and mean age was 58 ± 15 years. Histopathology was available for 96 (81%) patients, through surgery procedure (n = 77, 65%) or transcatheter biopsy (n = 19, 16%). Final diagnosis was obtained for 112 (94%) patients and was divided into 78 (70%) and 34 (30%) benign and malignant etiologies, respectively. The 7 (6%) remaining patients without definitive diagnosis were due to premature death or contraindication for more invasive investigations (patient refusal or comorbidities making exploration unreasonable). Distribution according to the mass etiology is represented in Fig. 1. Among the 78 benign masses, there were 61 (78%) tumors, including 52 myxomas, the most prevalent mass, and 17 non-tumoral masses, mostly thrombi (18%). Among the 34 malignant masses, there were 15 (44%) metastases, 18 (53%) sarcomas and 1 (3%) lymphoma. The primary location of metastases is shown in Table 2.
Localizations of the masses within the heart are shown in Fig. 2. Most of the masses were in the left atrium (50%).
Finally, 77 (65%) patients had surgery (4 patients were contraindicated for intervention and 2 patients refused the operation).
Impact of cardiac imaging tests on decision-making and management
Among the 119 patients, 63 (53%), 71 (60%), 72 (61%) and 43 (36%) underwent TEE, cardiac CT, CMR and 18F-FDG PET-CT, respectively. Cardiac imaging tests performed according to benign and malignant etiology are shown in Table 3. Nine patients had none of the imaging modalities studied: 4 due to surgical emergency, 1 for early death and 4 patients received elective surgery without further imaging examination.
Before- and after-test decision-making rates for TEE, cardiac CT, CMR and 18F-FDG PET-CT were 2 and 54% (P < 0.001), 23 and 62% (P = 0.017), 31 and 85% (P < 0.001), and 49 and 100% (P < 0.001), respectively. Before and after cardiac imaging test decision-making is presented in Fig. 3. In case of decision-making, before- and after-test management strategy for each test is shown in Fig. 4.
Before- and after-test management strategy for each cardiac imaging modality. *P < 0.05; **P < 0.01; ***P < 0.001 after versus before. Antineoplastic treatment chemotherapy and/or radiotherapy, Cardiac CT cardiac computed tomography, CMR cardiac magnetic resonance, TEE transesophageal echocardiography, 18F-FDG-PET18F-fluorodesoxyglucose positron emission tomography
For atrial masses, before- and after-test decision-making rates for TEE, cardiac CT, CMR and 18F-FDG PET-CT were 2 and 58% (P < 0.001), 29 and 76% (P < 0.001), 38 and 92% (P < 0.001), and 59 and 100% (P < 0.001), respectively. TEE was the most effective for left atrium masses, allowing an increase of before- and after-test decision-making rates from 0 to 74% (P < 0.001). For right atrial masses, cardiac CT allowed an increase of before- and after-test decision-making rates from 4 to 61% (P < 0.001), whereas the difference between before- and after-test decision-making rates for TEE was not significant (5 versus 20%, respectively; P = 0.250).
For ventricular masses, before- and after-test decision-making rates for TEE, cardiac CT, CMR and 18F-FDG PET-CT were 0 and 25% (P < 0.001), 10 and 39% (P = 0.07), 14 and 68% (P < 0.001), and 45 and 100% (P < 0.001), respectively. TEE was not useful for right ventricle masses (0%) and only once for left ventricle masses (33%). For ventricular masses, CMR allowed an increase of before- and after-test decision-making rates from 13 to 67% (P = 0.008), whereas the difference between before- and after-test decision-making rates for CT was not significant (17 versus 33%, respectively; P = 0.625). For right ventricle masses, cardiac CT and CMR allowed an increase of before- and after-test decision-making rates from 0 to 44% (P < 0.001) and 14 to 71%, respectively.
Finally, 18F-FDG PET-CT allowed the after-test decision-making rate to reach 100%, whatever the localization, with a before-test decision-making rate of 42%, 80%, 38% and 50% for right atrium, left atrium, right ventricle and left ventricle, respectively. Before- and after- cardiac imaging test decision-making, according to mass localization is presented in Fig. 5.
Before- and after- test decision-making according to mass localization. *P < 0.05; **P < 0.01; ***P ≤ 0.001 after versus before. Cardiac CT cardiac computed tomography, CMR cardiac magnetic resonance, TTE transthoracic echocardiography, TEE transesophageal echocardiography, 18F-FDG PET-CT18-fluorodeoxyglucose positron emission tomography
Performance of cardiac imaging in diagnosing benign or malignant masses
Conclusions of each imaging modality according to the final diagnosis are presented in Table 4. The performances of cardiac imaging techniques in diagnosing benign or malignant masses are presented in Table 5. Based on ROC curves, 18F-FDG PET-CT had the best areas under the curve, which were at 0.89 ± 0.06 and 0.94 ± 0.05 respectively for the diagnosis of benign and malignant tumors. Imaging was not contributive to determining benign or malignant nature for 19 (31%) cases using TEE, 16 (25%) cases using cardiac CT, 9 (13%) cases using CMR, or for 7 (19%) cases using 18F-FDG PET-CT.
Impact of cardiac imaging result on outcomes
Twenty-eight (24%) patients died during the follow-up: 24 (20%), 3 (3%) and 1 (1%) with malignant, benign and indeterminate etiology, respectively. Patients with masses linked to benign etiology based on definitive diagnosis, had a better survival rate than patients with malignant masses. Survival according to final diagnosis and cardiac imaging results is presented in Fig. 6. For each modality, survival of patients with benign or indeterminate etiology was better than for patients with malignant etiology. Among patients diagnosed with benign or undetermined etiology, no death was related to cardiac disease.
Discussion
Our study shows that all non-invasive cardiac imaging modalities (i.e. TEE, cardiac CT, CMR and 18F-FDG PET-CT) are effective in providing a course of action in the management of cardiac masses. TEE provides a therapeutic decision in almost three quarters of left atrial tumors, whereas cardiac CT and CMR are contributive, whatever the location. 18F-FDG PET-CT results in decision-making for all patients after its completion. Anticoagulation indication is not influenced by 18F-FDG PET-CT, suggesting that other modalities are sufficient for cardiac thrombus diagnosis. 18F-FDG PET-CT is the most efficient test to differentiate between benign and malignant etiologies [4]. Finally, a benign or undetermined diagnosis given by each modality is associated with good prognosis, close to those related to pathological findings.
Our study shows the predominant role of TEE in atrial tumor management, in particular of the left atrium. These results can be explained by the high prevalence of myxomas in this cavity, which usually have a typical presentation, without alternative diagnosis, and do not require further investigations before surgery [5, 6].The TEE contribution for right atrial masses appears less obvious, probably because of wider etiologies [6]. TEE appears to be the first-line examination for atrial masses, whereas its contribution for ventricular masses seems more limited [7, 8].
Cardiac CT and CMR appear to be contributive examinations whatever the location and the management perspective. Despite a lower spatial and temporal resolution, soft tissue contrast and extra-cardiac exploration allowed by both cardiac CT and CMR lead to a better performance than echocardiography to characterize a cardiac mass [9, 10]. Although CMR has been widely validated for exploring cardiac masses [11,12,13], there is no study comparing cardiac CT with other imaging modalities for cardiac mass exploration. However, American recommendations for cardiac imaging recommend TTE, TEE, cardiac CT and CMR evaluation without distinction [14].
Finally, 18F-FDG PET-CT is most of the time the last examination before transcatheter biopsy or surgery for histological purpose. However, our methodology making 18F-FDG PET-CT the last line, explains that all decisions were made after its completion and can lead to overestimating its contribution. Performances of 18F-FDG PET-CT overcome the single information by combining radiotracer uptake on the mass, and giving information on local–regional extension and other whole body lesions. To optimize its accuracy, this examination must be carried out under good conditions with preparation (low-carbohydrate and high-fat diet), which can complicate the procedure [15].
Survival analyses show that non-invasive cardiac imaging can detect patients with a good prognosis based on a result indicating a benign or undetermined etiology. Similar findings have already been reported for CMR on a population of 53 patients [16]. Other confounders like complications associated with the management of malignant tumors could impact the overall survival, independently of the mass etiology. However, prognostic performance and comparison of each non-invasive modality had never been explored previously.
Up to now, there is no guideline for the use of non-invasive cardiac imaging in the cardiac masses exploration algorithm. A recent study proposed a decision algorithm focusing on CMR without integrating cardiac CT [11]. Based on our results, we propose a new diagnostic algorithm for the exploration of cardiac masses (Fig. 7) with a choice of the first-line imaging modality based on mass localization.
Proposal of a new diagnostic algorithm. Cardiac CT cardiac computed tomography, CMR cardiac magnetic resonance, TTE transthoracic echocardiography, TEE transesophageal echocardiography, 18F-FDG PET-CT18-fluorodeoxyglucose positron emission tomography. *Depending on local availability and possible contraindications of the patient, CMR should be preferred in case of left ventricular mass. **Histological evidence by biopsy or surgery
The main strength of this study is its originality, as it is the first to compare different imaging modalities available today to explore heart masses. In addition, the population studied is significant for a rare disease. However, the sample is quite small for an epidemiologic study: for example, the sex-ratio of the population, with a preponderance of men in the population (59%), does not seem intuitive since we would expect parity. This slight difference can probably be attributed to a random sampling and should lead to a careful interpretation of the results.
Limitations
Our study has limitations associated with a single-site and retrospective study. We can suppose that site experience could impact the validity of our results: prescription and protocol of imaging tests, interpretation and therapeutic approach. The Interpretation of imaging examinations was not performed blindly. Due to the retrospective design and the impact of the result on the decision-making at the time of the test, it was not possible to perform a standardized or blind review of the tests. As a result, the interpretation of tests is subject to some variability inherent in each modality. The strength of this retrospective work is to show, in a real-life cohort, the contribution of each modality despite this interpretation-induced variability.
There is also a recruitment bias with patients selected only from a tertiary center of cardiology and cardiac surgery. This bias may explain the low proportion of secondary tumors compared to the rate found in epidemiological studies [1, 17]. However, it strengthens the study by selecting more complex diagnostic situations.
Prioritization of examinations by the clinician represents an evident bias on our study, modifying the contribution of the different imaging modalities. In addition, availability of each technique and lack of consensus probably led to the over-prescription of imaging tests.
Finally, temporal changes related to the long inclusion period, may have had an impact on performed tests and therefore on study results.
Conclusion
All non-invasive cardiac imaging techniques are useful for cardiac mass exploration and management, as they make it possible to increase the decision-making rate and to differentiate benign and malignant etiologies. However, the usefulness of each technique is not equal, depending on the location of the mass within the heart. In the first line, TEE is interesting for atrial masses, cardiac CT and CMR for ventricular or suspected malignant masses, and 18F-FDG PET-CT is the most effective test to distinguish between benign and malignant etiologies.. A final classification as benign or indeterminate etiology means a good prognosis.
Abbreviations
- AUC:
-
Area under the curve
- CMR:
-
Cardiac magnetic resonance
- CT:
-
Computed tomography
- ECG:
-
Electrocardiogram
- FDG:
-
Fluorodeoxyglucose
- PET:
-
Positron emission tomography
- 18F-FDG PET-CT:
-
18F-fluorodeoxyglucose positron emission tomography coupled than tomography
- ROC:
-
Receiver operating characteristic
- TCB:
-
Transcatheter biopsy
- TEE:
-
Transesophageal echocardiography
- TTE:
-
Transthoracic echocardiography
References
Lam KY, Dickens P, Chan AC (1993) Tumors of the heart. A 20-year experience with a review of 12,485 consecutive autopsies. Arch Pathol Lab Med 117:1027–1031
Bussani R, De-Giorgio F, Abbate A, Silvestri F (2007) Cardiac metastases. J Clin Pathol 60:27–34. https://doi.org/10.1136/jcp.2005.035105
Díaz Angulo C, Méndez Díaz C, Rodríguez García E, Soler Fernández R, Rois Siso A, Marini DM (2015) Imaging findings in cardiac masses (Part I): study protocol and benign tumors. Radiol Engl Ed 57:480–488. https://doi.org/10.1016/j.rxeng.2015.09.002
Rahbar K, Seifarth H, Schäfers M, Stegger L, Hoffmeier A, Spieker T et al (2012) Differentiation of malignant and benign cardiac tumors using 18F-FDG PET/CT. J Nucl Med 53:856–863. https://doi.org/10.2967/jnumed.111.095364
Alam M, Sun I (1991) Transesophageal echocardiographic evaluation of left atrial mass lesions. J Am Soc Echocardiogr 4:323–330. https://doi.org/10.1016/s0894-7317(14)80442-2
Kuon E, Kreplin M, Weiss W, Dahm JB (2004) The challenge presented by right atrial myxoma. Herz 29:702–709. https://doi.org/10.1007/s00059-004-2571-7
Reeder GS, Khandheria BK, Seward JB, Tajik AJ (1991) Transesophageal echocardiography and cardiac masses. Mayo Clin Proc 66:1101–1109. https://doi.org/10.1016/s0025-6196(12)65788-7
Obeid AI, Mudamgha AA, Smulyan H (1993) Diagnosis of right atrial mass lesions by transesophageal and transthoracic echocardiography. Chest 103:1447–1451. https://doi.org/10.1378/chest.103.5.1447
Araoz PA, Mulvagh SL, Tazelaar HD, Julsrud PR, Breen JF (2000) CT and MR imaging of benign primary cardiac neoplasms with echocardiographic correlation. RadioGraphics 20:1303–1319. https://doi.org/10.1148/radiographics.20.5.g00se121303
Rathi VK, Czajka AT, Thompson DV, Doyle M, Tewatia T, Yamrozik J et al (2018) Can cardiovascular MRI be used to more definitively characterize cardiac masses initially identified using echocardiography? Echocardiography 35:735–742. https://doi.org/10.1111/echo.14017
Zhu D, Yin S, Cheng W, Luo Y, Yang D, Lin K et al (2016) Cardiac MRI-based multi-modality imaging in clinical decision-making: preliminary assessment of a management algorithm for patients with suspected cardiac mass. Int J Cardiol 203:474–481. https://doi.org/10.1016/j.ijcard.2015.09.021
Wu CM, Bergquist PJ, Srichai MB (2019) Multimodality imaging in the evaluation of intracardiac masses. Curr Treat Options Cardiovasc Med 21:55. https://doi.org/10.1007/s11936-019-0756-x
Palaskas N, Thompson K, Gladish G, Agha AM, Hassan S, Iliescu C et al (2018) Evaluation and management of cardiac tumors. Curr Treat Options Cardiovasc Med 20:29. https://doi.org/10.1007/s11936-018-0625-z
Doherty JU, Kort S, Mehran R, Schoenhagen P, Soman P et al (2019) ACC/AATS/AHA/ASE/ASNC/HRS/SCAI/SCCT/SCMR/STS 2019 appropriate use criteria for multimodality imaging in the assessment of cardiac structure and function in nonvalvular heart disease : a report of the american college of cardiology appropriate use criteria task force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and the Society of Thoracic Surgeons. J Nucl Cardiol 26:1392–1413. https://doi.org/10.1007/s12350-019-01751-7
Yi J-E, Yoon HJ, Joo Hyun O, Youn H-J (2018) Cardiac and pericardial 18F-FDG uptake on oncologic PET/CT: comparison with echocardiographic findings. J Cardiovasc Imaging 26:93–102. https://doi.org/10.4250/jcvi.2018.26.e10
Mousavi N, Cheezum MK, Aghayev A, Padera R, Vita T, Steigner M et al (2019) Assessment of cardiac masses by cardiac magnetic resonance imaging: histological correlation and clinical outcomes. J Am Heart Assoc 8:e007829. https://doi.org/10.1161/JAHA.117.007829
Hoffmeier A, Sindermann JR, Scheld HH, Martens S (2014) Cardiac tumors-diagnosis and surgical treatment. Dtsch Arzteblatt Int 111:205–211. https://doi.org/10.3238/arztebl.2014.0205
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lemasle, M., Lavie Badie, Y., Cariou, E. et al. Contribution and performance of multimodal imaging in the diagnosis and management of cardiac masses. Int J Cardiovasc Imaging 36, 971–981 (2020). https://doi.org/10.1007/s10554-020-01774-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-01774-z