Abstract
We performed this study to compare the sensitivity and specificity of multi-slice computed tomography (MSCT) to coronary angiography (CA) in detecting coronary total occlusion (CTO) lesion characteristics. Moreover, we analyzed the association between these characteristics and the risk of revascularization failure. Fifty patients with confirmed CTO diagnosis were tried for revascularization using the antegrade (all 50) or retrograde (in failed nine antegrade interventions) approaches. Each patient underwent CA and MSCT before the intervention and data from both modalities were compared using the SPSS software. Successful revascularization occurred in 36 (72%) and 6 (66.7%) patients of the antegrade and retrograde groups, respectively. Compared to CA, MSCT exhibited high sensitivity in detecting CTO segment calcification (100%), size of the affected vessel (100%, area under the curve [AUC] = 0.82), distal filling of the affected segment (97.7%) and side-branching at the CTO segment (93.3%). However, it had lower sensitivity in detecting collaterals (75%) and the length of the affected segment (87.5%, AUC = 0.77). According to MSCT data, increased occlusion length > 18 mm (p = 0.01), atherosclerotic vessel wall (p = 0.02), small distal vessel size ≤ 2.75 mm (p = 0.002), proximal side-branching (p = 0.01) and calcification of the proximal cap (p = 0.007) or distal stump (p = 0.01) were associated with an increased risk of revascularization failure. MSCT exhibited high sensitivity in identifying several CTO lesion characteristics, such as lesional calcification and size of the affected vessel. However, further research is needed to improve the diagnostic accuracy of this modality and define the predictors of revascularization failure in CTO patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic total occlusion (CTO) in the coronary circulation indicates complete blockage of a coronary artery for 30 days or more [1]. Among patients with different clinical profiles who had coronary angiography (CA), CTO prevalence ranges between 18 and 52% [2]. Recent meta-analyses reported that successful CTO revascularization was associated with a significant reduction in the risk of mortality, subsequent coronary artery bypass grafting (CABG) and recurrent angina [3, 4]. In the past, CTO patients required CABG; however, as a result of advanced technology, percutaneous coronary intervention (PCI) showed favorable outcomes in clearing the coronary blockage with success rates between 55 and 85% [5, 6].
Despite the current advances in interventional cardiology, the recanalization of CTO lesions remains a major challenge in clinical practice [7, 8]. Therefore, a comprehensive assessment of CTO lesions is essential before PCI. This includes obtaining a detailed medical history and thorough physical examination and investigations [9, 10]. Recently, non-invasive imaging techniques, including multi-slice/detector computed tomography (MSCT) and magnetic resonance angiography have been developed for the assessment of coronary lesions [11].
With single-detector CT, a narrow beam of radiation is emitted. Therefore, as the radiation source rotates 360° once, one image of a single tissue slice is produced [12]. Increasing the number of detector rows widens the radiation beam into a broad cone shape, which results in gathering redundant data and improving the image temporal resolution [13]. Moreover, increasing the number of detector rows results in shorter scan times and more comfortable breath hold. However, the number of detector rows has no effect on the in-plane spatial resolution [12].
Several studies were conducted to test the diagnostic utility of MSCT before PCI and identify the predictors of procedural success according to MSCT data [14,15,16,17,18]. These studies showed that MSCT improves the chances of PCI success and developed different scores to predict it, such as J-CTO and KCCT scores. However, data on the diagnostic accuracy of MSCT in identifying specific CTO lesion features and revascularization failure risk factors remain limited. In this investigation, our aim was to compare the diagnostic accuracy of MSCT to CA in identifying CTO lesion characteristics and analyze the association between different CTO lesion characteristics and the risk of revascularization failure.
Materials and methods
Study population
Fifty patients with a confirmed CTO diagnosis in least one coronary artery were recruited from Al-Azhar University Hospitals and the Specialized Heart Center at Kobri El-Kobba Military Hospital during the period from April 2015 to March 2017. Chronic total obstruction was defined as complete obstruction of a native coronary artery for > 30 days and was confirmed by CA before patients underwent selective PCI [19]. The institutional review board at Al-Azhar University reviewed and approved the study protocol. We followed the STAndards for the Reporting of Diagnostic accuracy studies (STARD) checklist during the reporting of this study (Supplementary file 1).
After obtaining written informed consent, each patient was subjected to full history taking, thorough clinical examination and resting 12-lead electrocardiography (ECG). Patients were excluded if they had any of the following: previous CTO lesion stenting, unstable cardiovascular condition (such as heart failure, atrial fibrillation or acute coronary syndrome), renal insufficiency or known allergy to contrast media.
Study procedure
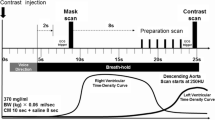
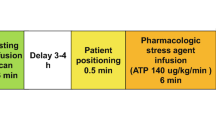
The following precautions were undertaken before performing MSCT studies: (a) beta-blockers were used if the heart rate was > 70 beats/min; (b) all images were acquired during an inspiratory breath hold; (c) tube voltage was set at 120 kV and the tube current was adjusted according to body mass index; and (d) a digitized ECG was continuously monitored during the procedure for retrospective data analysis.
Imaging was performed using a dual source CT machine (Two X-ray tubes and two detectors, arranged at an angular offset of 95°) obtained from Somatom Definition Flash, Siemens Healthcare, Forchheim, Germany. With 64 rows (of 0.6 mm width) in each detector, Z-axis coverage of 38.4 mm, a Z flying focal spot, and a gantry rotation time of 0.28 s for the system, this device allows (a) simultaneous data acquisition in 2 × 128 slices and (b) a 75 ms temporal resolution in the center of the field of view after a half-scan reconstruction.
Vessel opacification was achieved through automated iopromide (60–80 ml) injection (370 mg I/ml Ultravist®, Bayer Schering Pharma AG, Germany), using a power injector (Medrad Stellant®) at a flow rate of 5–6 ml/s plus a 40–60 ml saline flush. Quantitative evaluation of the coronary artery calcium was performed on the Agatston score (a standard threshold of 120 HU), using a half-scan reconstruction algorithm (of 3.0 mm slice thickness and 1.5 mm increment) and a medium sharp reconstruction kernel (Siemens B35f).
We acquired CT angiography datasets, using either prospective ECG-triggered acquisitions (for patients with heart rates 60–70 bpm) or retrospective ECG-gated acquisitions with tube current modulation (for patients with higher heart rates and post CABG patients). In case of retrospective ECG-gated studies, reconstruction was performed at the end-diastolic phase, while systolic phases were utilized when needed. Acquired datasets were reconstructed by 3D volume-rendered (VR), thin-slab MIP and MPR images, at a slice thickness of 0.75 mm. The variables for which datasets were analyzed by an experienced operator included the following:
-
Characters of the proximal segment to CTO lesion: shape (healthy or atherosclerotic), proximal stump (blunt or tapered), side-branching within 3 mm from the CTO segment and the presence of calcification or tortuosity (defined as bending at an angle ≤ 45°).
-
Characters of the totally occluded segment: site (ostial, proximal, mid, or distal), length (mm), evidence of dye filling, side-branching from within the segment and calcification within the segment or the proximal and distal arterial caps.
-
Characters of the distal segment to CTO lesion: size, healthy or atherosclerotic and whether it can be visualized or not. Moreover, the presence of sizable intercoronary collaterals to supply the affected area was evaluated.
Coronary angiography was performed in all enrolled patients and the following parameters were recorded: shape of the proximal segment to the CTO segment and the presence of a proximal stump, side-branching at CTO segment, ante/retrograde filling of the distal segment to the CTO lesion and the presence of sizable collaterals.
All patients underwent PCI procedures, performed by highly-skilled operators in CTO interventions and the following procedural data were collected: Used equipment, approach (antegrade or retrograde), the incidence of procedural success (defined as attainment of a residual diameter stenosis < 20% and a TIMI flow rate of grade 2 or 3) or failure and procedural complications.
Statistical analysis
We used the statistical package for social sciences (SPSS) software [version 23.0 for windows] for data analysis. Data were presented as mean ± standard deviation (SD) or frequency and percentage. The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of MSCT in identifying different CTO lesion characteristics were calculated in comparison with CA as a standard test. Categorical variables were compared using the Chi square (χ2) and Fisher’s exact tests. We used the two-tailed student’s t test to compare continuous variables of parametric data and the Mann–Whitney U test for non-parametric data. The level of significance was accepted if the p value was < 0.05.
Results
Baseline data
We enrolled 50 patients who were diagnosed with CTO in at least one native coronary artery by CA. All patients underwent revascularization using the antegrade approach. Of them, 36 experienced successful revascularization and 14 failed. Among the latter, nine patients were tried for revascularization using the retrograde approach (six successes and three failures) and five could not be re-allocated due to the lack of sizable collaterals (Fig. 1). The sample included 39 males and the mean age of enrolled patients was 53.8 ± 6.5 years. No significant differences were observed between patients with successful and failed revascularization in terms of the prevalence of comorbidities, including diabetes mellitus, hypertension or previous myocardial infarction. Table 1 summarizes the baseline characteristics of enrolled patients.
Comparison of CA and MSCT data
Considering CA as the reference standard, MSCT exhibited high sensitivity in detecting CTO segment calcification (100%), size of the affected vessel (100%, area under the curve [AUC] = 0.82, optimal cut-off ≤ 2.75), distal filling of the affected segment (97.7%), side-branching at the CTO segment (93.3%), and proximal cap tapering (93.3%). However, it had lower sensitivity in detecting collaterals (75%) and the length of the affected segment (87.5%, AUC = 0.77, optimal cut-off > 18) (Table 2; Fig. 2).
Moreover, MSCT showed high specificity in identifying CTO lesion collaterals (93.3%). However, its specificity was lower in identifying the other aforementioned parameters (Table 2). Data underlying the calculation of sensitivity and specificity results are illustrated in Supplementary file 2.
Comparison of MSCT data in success and failure groups
Proximal to the CTO segment
There was no significant difference between the success and failure groups regarding vessel tortuosity. However, there was a statistically significant increase in failure rate in the presence of side branches (p = 0.013), proximal cap calcification (p = 0.007), blunt proximal cap (p = 0.01) and atherosclerotic vessels (p = 0.021).
The CTO segment
We detected no significant difference between the success and failure groups regarding which artery is affected, site of CTO and the presence of calcification or side branches within the segment. However, there was a statistically significant increase in failure rate in longer occluded segments > 18 mm (p = 0.001).
Distal to the CTO segment
Our analysis showed no significant difference between the success and failure groups in terms of distal filling, presence of diseased vessels and tapering of the distal cap. However, there was a statistically significant increase in failure rate in the presence of distal cap calcification (p = 0.01) and smaller vessel size ≤ 2.75 mm (p = 0.002). Data on MSCT variables in the success and failure groups are illustrated in Supplementary file 3.
Discussion
Although angiographic imaging remains a fundamental part of CTO revascularization procedures [20, 21], this modality has several limitations including: (1) providing incomplete information on the vessel morphology in totally occluded segments and (2) inability to identify ostial occlusions and lower visibility of long tortuous vessels [22, 23]. On the other hand, CT angiography with 2D and 3D reconstruction technologies can reliably visualize the occluded segment and identify the anatomical (e.g. tortuosity and length) and morphological (e.g. calcification) characteristics of the lesion [24].
Our study included 50 patients with angiographically confirmed CTO lesions. Data analysis showed that MSCT has slightly lower sensitivity than invasive CA in visualizing CTO proximal stump, side-branching from CTO segment, the artery distal to CTO segment and sizable collaterals. This can be attributed to the higher spatial resolution of CA over MSCT, even with the recent technological advances in the latter modality. Future improvements in MSCT technology may improve the diagnostic accuracy in this regard. Other non-invasive coronary assessment tools have been developed and showed comparable diagnostic accuracy to MSCT, such as intravascular ultrasound [25] and combination of these diagnostic modalities may improve the assessment of coronary lesions.
In our study, we tried to identify the cut-off values at which the highest sensitivity and specificity of MSCT can be reached. We found that a lesion length > 18 mm and a vessel size ≤ 2.75 mm carry an increased risk of failure. In a study by Choi et al. on 186 CTO lesions, the PCI success rates decreased significantly with increased occlusion length (> 18 mm) [26]. In another study by Mollet et al. on 45 CTO patients, blunt stump (by CA), occlusion length > 15 mm and severe calcification (by MSCT) were identified by multivariate analysis as independent predictors of revascularization failure [27].
Limitations and recommendations
The small sample size in our study may have underestimated the significance in some variables. Therefore, our data should be interpreted with caution, especially those on the risk factors for revascularization failure. Moreover, revascularization of CTO lesions is highly operator-dependent i.e. there is a room for inter-operator and even Intra-operator variability in different circumstances [28]. We could not enroll patients with ostial CTO lesions and this should be considered in future studies. Future studies should consider using a larger sample size, enrolling patients with ostial lesions and investigating the cost-efficiency benefits of using MSCT in CTO patients.
Conclusion
Multi-slice CT was less sensitive than CA in detecting proximal stump details, presence of side branches, distal arterial visualization, and sizable collaterals. However, it was as sensitive as CA in detecting CTO segment calcification. Further improvements in MSCT technology are warranted. Several factors, such as increased length of the occlusion, small distal vessel size, atherosclerotic vessel wall, proximal side-branching and calcification of proximal cap or distal stump were associated with an increased risk of PCI failure in CTO patients. However, these results should be interpreted with caution and require confirmation in future studies.
Abbreviations
- CA:
-
Coronary (conventional) angiography
- CTA:
-
Computed tomography angiography
- CTO:
-
Chronic total occlusion
- MSCT:
-
Multi-slice computed tomography
- PCI:
-
Percutaneous coronary intervention
References
Stone GW, Reifart NJ, Moussa I et al (2005) Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part II. Circulation 112:2530–2537
Bardají A, Rodriguez-lópez J, Torres-sánchez M (2014) Chronic total occlusion: to treat or not to treat? World J Cardiol 6:621–629
Joyal D, Afilalo J (2010) Interventional cardiology effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am Heart J 160:179–187
Gao L, Wang Y, Liu Y, Cao F, Chen Y (2017) Long-term clinical outcomes of successful revascularization with drug-eluting stents for chronic total occlusions: a systematic review and meta-analysis. Catheter Cardiovasc Interv 89:574–581
Elias J, Van Dongen IM, Hoebers LP, Ouweneel DM, Claessen BEPM., Råmunddal T, Laanmets P, Eriksen E, Van Der Schaaf RJ, Ioanes D, Nijveldt R, Tijssen JG, Hirsch A, Henriques JPS (2017) Improved recovery of regional left ventricular function after PCI of chronic total occlusion in STEMI patients: a cardiovascular magnetic resonance study of the randomized controlled EXPLORE trial. J Cardiovasc Magn Reson 19:53
Rathore S, Katoh O, Matsuo H et al (2009) Retrograde percutaneous recanalization of chronic total occlusion of the coronary arteries: procedural outcomes and predictors of success in contemporary practice. Circ Cadiovasc Interv 11:108
Brilakis E, Karmpaliotis D, Minh N (2014) Advances in the management of coronary chronic total occlusions. J Cardiovasc Transl Res 7:426–436
Prasad A, Rihal CS, Lennon RJ, Wiste HJ, Singh M, Holmes DR (2007) Trends in outcomes after percutaneous coronary intervention for coronary total occlusions: a 25-year experience from the Mayo Clinic. J Am Coll Cardiol 49:1611–1618
Stone GW, Kandzari DE, Mehran R, Colombo A, Schwartz RS, Bailey S, Moussa I, Teirstein PS, Dangas G, Baim DS (2005) Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part I. Circulation 112:2364–2372
Dash D (2016) Complications encountered in coronary chronic total occlusion intervention: prevention and bailout. Indian Heart J 68:737–746
Schuetz GM, Zacharopoulou NM, Schlattmann P et al (2010) Meta-analysis: noninvasive coronary angiography using computed tomography versus magnetic resonance imaging. Ann Int Med 152:167–177
Bardo DME, Brown P (2008) Cardiac multidetector computed tomography: basic physics of image acquisition and clinical applications. Curr Cardiol Rev 4:231
Kagadis GC (2005) CT of the heart: principles and applications. Med Phys 32:1453
Fujino A, Otsuji S, Hasegawa K, Arita T, Takiuchi S, Fujii K, Yabuki M, Ibuki M, Nagayama S, Ishibuchi K, Kashiyama T, Ishii R, Tamaru H, Yamamoto W, Hara M, Higashino Y (2017) Accuracy of J-CTO score derived from computed tomography versus angiography to predict successful percutaneous coronary intervention. JACC Cardiovasc Imag 11:209–217
Helge R, Rolf A, Werner GS, Schuhba A, Hamm CW, Achenbach S (2013) Preprocedural coronary CT angiography significantly improves success rates of PCI for chronic total occlusion. Int J Cadiovasc Imag 29:1819–1827
Li Y, Xu N, Zhang J et al (2015) Procedural success of CTO recanalization: comparison of the J-CTO score determined by coronary CTangiography to invasive angiography. J Cardiovasc Comput Tomogr 9:578–584
Yu C, Lee H, Suh J (2017) Coronary computed tomography angiography predicts guidewire crossing and success of percutaneous intervention for chronic total occlusion korean multicenter CTO CT registry score as a tool for assessing. Circ Cardiovasc Imag 10:e005800
Opolski MP, Knaapen P, Witkowski A, Min JK (2017) Coronary computed tomography angiography to predict successful percutaneous coronary intervention for chronic total occlusion. JACC Cardiovasc Imag 10:1206–1208
Dash D (2018) Coronary chronic total occlusion intervention: a pathophysiological perspective. Indian Heart J. https://doi.org/10.1016/j.ihj.2018.01.021
Gopakumar KS, Iype M, Viswanathan S, Koshy AG, Gupta PN, Sivaprasad K, Radhakrishnan VV (2017) Angiographic predictors of success in antegrade approach of chronic total occlusion interventions in a South Indian population in the contemporary era. Indian Heart J. https://doi.org/10.1016/j.ihj.2017.09.002
de Feyter PJ, Serruys PW, Davies MJ, Richardson P, Lubsen J, Oliver MF (1991) Quantitative coronary angiography to measure progression and regression of coronary atherosclerosis: value, limitations, and implications for clinical trials. Circulation 84:412–423
Li P, Gai L, Yang X, Sun Z, Jin Q (2010) Computed tomography angiography-guided percutaneous coronary intervention in chronic total occlusion. J Zhejiang Univ Sci B 11:568–574
Hildick-Smith DJR, Lowe MD, Walsh JT, Ludman PF, Stephens NG, Schofield PM, Stone DL, Shapiro LM, Petch MC (1998) Coronary angiography from the radial artery—experience, complications and limitations. Int J Cardiol 64:231–239
Magro M, Schultz C, Simsek C, Garcia-Garcia HM, Regar E, Nieman K, Mollet N, Serruys PW, van Geuns RJ (2010) Computed tomography as a tool for percutaneous coronary intervention of chronic total occlusions. EuroInterv J Eur Collab Work Gr Interv Cardiol Eur Soc Cardiol 6:G123–G131
Leber AW, Knez A, von Ziegler F et al (2005) Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 46:147–154
Choi J-H, Bin Song Y, Hahn J-Y, Choi SH, Gwon H-C, Cho JR, Jang Y, Choe Y (2011) Three-dimensional quantitative volumetry of chronic total occlusion plaque using coronary multidetector computed tomography. Circ J 75:366–375
Mollet NR, Hoye A, Lemos PA, Cademartiri F, Sianos G, McFadden EP, Krestin GP, Serruys PW, de Feyter PJ (2005) Value of preprocedure multislice computed tomographic coronary angiography to predict the outcome of percutaneous recanalization of chronic total occlusions. Am J Cardiol 95:240–243
Martín-Yuste V, Barros A, Leta R, Ferreira I, Brugaletta S, Pujadas S, Carreras F, Pons G, Cinca J, Sabate M (2012) Factors determining success in percutaneous revascularization of chronic total coronary occlusion: multidetector computed tomography analysis. Rev Española Cardiol (English Ed) 65:334–340
Acknowledgements
The authors would like to acknowledge the Medical and Teaching staff at Al-Azhar Faculty of Medicine and Kobri El-Kobba Military hospital for their support during conducting the study. Preliminary data from this study were presented at the 13th Annual Complex Cardiovascular Catheter Therapeutics, Florida (USA), 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Abdelmoneim, I., Sadek, A., Mosaad, M.A. et al. Diagnostic accuracy of multi-slice computed tomography in identifying lesion characteristics in coronary total occlusion. Int J Cardiovasc Imaging 34, 1813–1818 (2018). https://doi.org/10.1007/s10554-018-1392-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-018-1392-3