Abstract
The right ventricular longitudinal strain (RVLS) of pulmonary hypertension (PH) patients and its relationship with RV function parameters measured by echocardiography and hemodynamic parameters measured by right heart catheterization was investigated. According to the WHO functional class (FC), 66 PH patients were divided into FC I/II (group 1) and III/IV (group 2). RV function parameters were measured by echocardiographic examinations. Hemodynamic parameters were obtained by right heart catheterization. Patients in group 2 had higher systolic pulmonary artery pressure (sPAP; P < 0.05) than patients in group (1) significant between-group differences were observed in global RVLS (RVLSglobal), free wall RVLS (RVLSFW; P < 0.01), and RV conventional function parameters (all P < 0.05). Moreover, mPAP and PVR increased remarkably and CI decreased significantly in group (2) RVLSglobal had a positive correlation with 6-min walking distance (6MWD; r = 0.492, P < 0.001) and N-terminal pro-brain natriuretic peptide (NT-proBNP; r = 0.632, P < 0.001), while RVLSFW had a positive correlation with 6MWD (r = 0.483, P < 0.001) and NT-proBNP (r = 0.627, P < 0.001). Hemodynamics analysis revealed that RVLSglobal had a positive correlation with mPAP (r = 0.594, P < 0.001), PVR (r = 0.573, P < 0.001) and CI (r = 0.366, P = 0.003), while RVLSFW had a positive correlation with mPAP (r = 0.597, P < 0.001), PVR (r = 0.577, P < 0.001) and CI (r = 0.369, P = 0.002). According to receiver operating characteristic curves, the optimal cut-off values of RVLSglobal (–15.0%) and RVLSFW (–15.3%) for prognosis detection with good sensitivity and specificity. Evidence has shown that RVLS measurement can provide the much-needed and reliable information on RV function and hemodynamics. Therefore, this qualifies as a patient-friendly approach for the clinical management of PH patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary hypertension (PH) is a life-threatening disease associated with poor outcomes. It is a pathophysiological disorder that involves multiple clinical conditions, and may worsen co-occurring cardiovascular and respiratory diseases [1]. Standard parameters for diagnosis involve the assessment of pulmonary hemodynamics, that is, mean pulmonary arterial pressure (mPAP) or pulmonary vascular resistance (PVR) [2]. Furthermore, this necessitates invasive right heart catheterization (RHC), which may give significant economic burden to patients [3]. Therefore, there is a need for a noninvasive approach that can reliably reflect the changes in pulmonary hemodynamics.
Transthoracic echocardiography has been a widely used noninvasive method for the evaluation of PH [4]. First, it helps in determining pulmonary arterial pressure (PAP) by measuring the tricuspid valve regurgitation velocity. Second, echocardiography is a widely used approach for evaluating right ventricular (RV) function. RV function in PH patients is influenced by increased afterload, and is associated with adverse outcomes. In patients with PH, progressive right heart failure has been the main cause of death. Conventional parameters for evaluating RV function include the RV index of myocardial performance (RIMP), tricuspid annular plane systolic excursion (TAPSE), RV fractional area change (RVFAC), and tricuspid annular systolic velocity (s′) [5]. Recently, the measurement of RV longitudinal strain (RVLS) by two-dimensional speckle tracking imaging (2D-STI) has gained attention for estimating global and regional systolic RV function [5, 6]. It helps quantify complex cardiac motions based on the frame-to-frame tracking of ultrasonic speckles in gray-scale images. Moreover, angle-independent imaging makes 2D-STI a better choice compared to diffusion tensor imaging in the clinical setting [6]. The term RVLS usually refers to either the average of RV free wall and septal segments or RV free wall segments alone.
In this study, we determined RVLS using 2D-STI, and analyzed its correlations with hemodynamic parameters measured through RHC and RV function parameters by echocardiography. Furthermore, this study proposes its clinical application for evaluating RV function and hemodynamics in PH patients.
Materials and methods
Patient enrolment
Consecutive adult patients with definite PH verified by RHC between April 2015 and January 2016 at Beijing Chaoyang Hospital were retrospectively studied. Mean patient age was 47.1 ± 13.7 years. Among these patients, 41 patients had chronic thromboembolic PH, 23 patients had pulmonary arterial hypertension, and two patients had hypoxic PH. These patients were evaluated according to standard guidelines. Exclusion criteria were: (1) pregnant and lactating patients, (2) patients with left-sided heart failure, coronary artery disease, moderate to severe aortic and/or mitral valval disease, and atrial fibrillation/flutter, and (3) patients (four) whose endocardium was not visible. Patients were divided into two groups according to the WHO PH Functional Class: group 1 (WHO FC I/II) and group 2 (WHO FC III/IV). This study was conducted in accordance with the guidelines of the Declaration of Helsinki and was approved by the ethics committee of Beijing Chaoyang Hospital. Written informed consent was obtained from all participants.
Echocardiographic examination
Echocardiographic examinations were performed on all patients to assess right heart function. Images were obtained with the patient at left lateral decubitus position using a Philips EPIQ 7C (Philips Healthcare, MA, USA). The evaluation of RV function was based on the recommendations of the guidelines for the echocardiographic assessment of the right heart in adults [7]. Images of the RV-focused apical four-chamber view were obtained for further analysis, and TAPSE was acquired in M-mode. Systolic displacement was measured from end-diastole to end-systole. Furthermore, RV end-diastolic area (RV EDA) and RV end-systolic area (RV ESA) were obtained by two-dimensional echocardiography. The RVFAC was calculated as: (RV diastolic area−RV systolic area)/RV diastolic area × 100%. The tricuspid s′ was measured by tissue Doppler imaging in the apical four-chamber view. RIMP was calculated as the ratio of isovolumic time to ejecting time, which was measured during pulsed tissue Doppler imaging. According to the 2015 American Society of Echocardiography guidelines and standards for cardiac chamber quantification by echocardiography in adults, the criteria for RV dysfunction were TAPSE < 17 mm, RIMP > 0.54, FAC < 35%, and s′ < 9.5 cm/s [5].
2D-STI analysis
Apical four-chamber views were specifically optimized to visualize the right ventricle and obtain echocardiographic cine loops by recording three consecutive heart cycles (>61 frames per second). Data were stored in a mobile device in DICOM format, and offline analyses were performed using QLAB 10.3 software (Philips Healthcare). After entering the aCMQ interface to determine the apical four-chamber view and choosing the AP4 option, a region of interest was traced with a point-and-click approach on the endocardium at end-diastole in the right ventricle from the RV-focused view. Then, a larger region of interest was generated and manually adjusted near the epicardium. Special care was taken to fine-tune the region of interest using visual assessment during cine loop playback, in order to ensure that the segments were tracked appropriately. After computational analysis, global RVLS (RVLSglobal) and free wall RVLS (RVLSFW) were obtained (Fig. 1).
Measurement of the RVLS by two-dimensional speckle tracking echocardiography. Global RVLS (RVLSglobal) was obtained from RV free wall and septal segments. Free wall RVLS (RVLSFW) was obtained from three segments of the free wall. a Measurement of RVLSglobal in WHO FC II patients. b Measurement of RVLSFW in WHO FC II patients. c Measurement of RVLSglobal in WHO FC IV patients. d Measurement of RVLSFW in WHO FC IV patients
Right heart catheterization
All patients underwent RHC for hemodynamic measurements. Venous access was obtained by inserting an introducer into the internal jugular vein. Swan–Ganz standard thermodilution pulmonary artery catheters were placed at the right inferior pulmonary artery. The measured indices were mPAP, pulmonary capillary wedge pressure (PCWP), PVR and central venous pressure (CVP). Cardiac output was determined using the Fick method, and PVR was reported in Wood units. A 6MWD was performed according to the American Thoracic Society protocol [8]. The time interval between echocardiography and right heart catheterization was 0–21 days (median: 3.5 days).
Statistical analyses
Continuous variables are expressed as mean ± standard deviation. Normality was evaluated using the one-sample Kolmogorov–Smirnov test. Independent sample t-test was performed to compare the results of group 1 and group 2. Linear regression analysis was used to study the relationships between two variables. The optimal cut-off values and the ability of RVLS (RVLSglobal and RVLSFW) to predict ominous prognosis was assessed using the area under the curve (AUC) of receiver operating characteristic (ROC) curves. The optimal cut-off value was defined as closest to 1 in the top left corner. The ROC curves of RVLS (RVLSglobal and RVLSFW) were statistically compared against those of the conventional echo markers (s′ and TAPSE) using the method of DeLong. Interobserver and intraobserver intraclass correlation coefficients (ICCs) of RVLSglobal and RVLSFW were calculated using a two-way mixed model with 95% CIs. The agreement between interobserver and intraobserver reproducibility was tested using the Bland–Altman method. P < 0.05 was considered statistically significant. SPSS (version 17.0 for Windows; SPSS Inc., Chicago, IL, USA) was used for statistical analysis and graphical presentation.
Results
Patient characteristics
A total of 66 consecutive patients with definite PH were enrolled into this study. As shown in Table 1, the study population included 17 male and 49 female subjects with an average age of 47.1 ± 13.7 years. This cohort consisted of 41 patients with chronic thromboembolic PH, 23 patients with pulmonary arterial hypertension, and two patients with hypoxic PH. Forty-three patients were assigned to group 1 and 23 patients were assigned to group 2. Both groups revealed no significant differences in age, gender and body surface area. The enlargement of the right ventricle was more obvious in group 2 than in group 1, which manifested as larger RV EDA and RV ESA indexed to BSA and a significantly higher eccentricity index and RVD/LVD (P < 0.05).
RV function
sPAP was more significantly elevated in group 2 than in group 1 (P < 0.05). Furthermore, RVLSglobal and RVLSFW remarkably differed between these two groups (P < 0.01, Table 2), with group 2 demonstrating significantly reduced RVLSglobal and RVLSFW (Fig. 2).
With regard to the traditional parameters of RV function, significant differences were observed in TAPSE, RIMP, RVFAC and s′ between these two groups (P < 0.05, Table 2). These indices revealed a significant reduction in patients in group 2, with a worse heart function (WHO FC III/IV).
RVLSglobal had a positive correlation with 6MWD (r = 0.492, P < 0.001) and LogNT-proBNP (r = 0.632, P < 0.001), while RVLSFW had a positive correlation with 6MWD (r = 0.483, P < 0.001) and LogNT-proBNP (r = 0.627, P < 0.001; Fig. 3a–d).
Right heart catheterization
Patients in group 2 manifested higher mPAP, PVR and central venous pressure (CVP) than patients in group 1, which coincided with a remarkable decline in CI (P < 0.05). However, pulmonary capillary wedge pressure (PCWP) did not show a significant statistical difference (P > 0.05, Table 3).
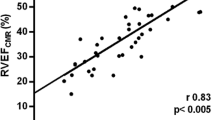
RV strain and RHC parameters
RVLSglobal was positively correlated with mPAP (r = 0.594, P < 0.001), CI (r = 0.366, P = 0.003) and PVR (r = 0.573, P < 0.001). The same was observed in RVLSFW with mPAP (r = 0.597, P < 0.001), CI (r = 0.369, P = 0.002) and PVR (r = 0.577, P < 0.001) (Fig. 4a–f).
Predictive value of RV strain (RVLSglobal and RVLSFW) for ominous prognosis in patients with PH
Areas under the curve (AUCs; Table 4; Fig. 5a–c) show the ability of RVLS (RVLSglobal and RVLSFW) and traditional echocardiographic parameters (s′ and TAPSE) to predict RV dysfunction based on NT-proBNP, 6MWD and CI. The AUCs of ROC curves indicated that RVLSglobal and RVLSFW are useful predictive parameters of RV dysfunction based on NT-proBNP, CI and 6MWD. From the ROC curves, the optimal cut-off values of RVLSglobal and RVLSFW for prognosis detection with sensitivity and specificity were as follows: NT-proBNP > 1400 ng/l, CI < 2.0 l min/m2 and 6MWD < 440 m (Tables 5, 6).
Reproducibility
The interobserver reliability of RVLS was assessed using measurements from ten patients by different observers and by examiners blinded to the patient types (Table 7; Fig. 6a–d). One of the two observers is an expert in echocardiography.
Discussion
Despite recent advances in the treatment of PH, its long-term prognosis remains poor as PH has been often associated with serious complications and mortality. In fact, the long-term survival rates of WHO FC I/II PH patients were better than that of PH patients in higher functional classes [3]. Not all clinical hemodynamic parameters can be applied to PH patients in the assessment of disease severity. Since the level of PAP is influenced not only by an increase in PVR but also by changes in RV function, the correlation between PAP and prognosis in late severe pulmonary arterial hypertension patients is very poor. Therefore, decision making with regard to treatment shall not depend solely on the level of PAP. An objective evaluation of the severity, stability and prognosis of the disease should be performed on the basis of various parameters. Humbert et al. demonstrated that PH screening for systemic sclerosis patients can help identify patients with milder forms of PH, leading to earlier therapeutic interventions and better survival [9]. By comparing the RHC parameters in this study, mPAP, PVR and CVP were higher in group 2 than in group 1, and CI was significantly reduced; indicating that RV function declined more significantly in patients in group 2. According to two-dimensional speckle tracking parameters, changes in RV function were more obvious in patients in group 2, suggesting that RVLS measured by 2D-STI is more sensitive than traditional RV function parameters in evaluating the disease severity among PH patients.
In our study, both RVLSglobal and RVLSFW positively correlated with 6MWD and NT-proBNP, suggesting that RVLS has the power to predict the prognosis of RV function in PH patients. A fatal increase in RV afterload may inhibit RV contractility, leading to hemodynamic instability in PH patients. The interaction between the right ventricle and PA or the correlation between RV contractility and afterload determines the performance of the right heart constriction [10]. More attention should be given to changes in right heart function and hemodynamics in patients with PH. Vascular constriction, vascular remodeling, and in situ thrombosis, at the onset and development of PH, together lead to an increase in PVR [11]. Our correlation analysis indicated that both RVLSglobal and RVLSFW positively correlated with mPAP, PVR and CI, which were measured by RHC. Thus, the measurement of RVLS can indirectly reflect hemodynamic changes and hence is a noninvasive approach for evaluating myocardial longitudinal RV function. Under normal contractions, the shortening of the longitudinal direction of the RV myocardium would contribute greatly to the RV stroke volume, than the shortening of the circumferential direction [12, 13]. A study [14] has found that inherent mechanical characteristics and microstructures of myocardial cells change due to the accumulation of extra tissues [14]. Differences in levels of myocardial coupling in longitudinal and circumferential directions may indicate that an heterogeneous reaction is obvious across different stages of PH [14].
Compared to TAPSE and DTI-derived s′, the angle independency of STE-derived RVLS is an advantage. TAPSE and s′ assume that a single segment represents the function of a complex 3D structure. RVLS is a useful parameter for estimating RV global and regional systolic function. It depends on RV loading conditions as well as RV size and shape and is less confounded by the overall heart motion.
ESC/ERS guidelines recommend the regular assessment of PH patients [1]. A comprehensive assessment of RV function and prognostic information are useful in the management of patients. In clinical practice, although 6MWD can be influenced by several factors, NT-proBNP appears to be a stronger predictor of prognosis [15]. Following clinical guidelines, we analyzed the predictive value of the RVLS for ominous prognosis in patients with PH. In our study, RVLSglobal below −15.0% and RVLSFW below −15.3% indicated poor long-term prognosis in PH patients.
Some scholars argue that the division of ventricular septum into left and right components cannot reliably be differentiated by echocardiography. Therefore, the inclusion of the septum will necessarily include left ventricular strain values that may not directly affect the right ventricle [16]. In our cohort, there were no obvious differences between using either RVLS global or free wall. Dahhan et al. reported that both global and free wall RVLS are associated with outcomes on multivariable analyses after accounting for age, gender and systolic blood pressure in acute pulmonary embolism [17]. Park et al. revealed that the global longitudinal strain of RV demonstrates a significant correlation with PVR calculated using right heart catheterization and echocardiographic parameters [18]. RV free wall strain also revealed similar results. Wright et al. reported that both RV free wall strain and FAC are helpful in detecting the acuity of RV pressure overload [19]. Meanwhile, the inclusion of RV free wall strain provided an incremental value to clinical and traditional echocardiographic variables.
Study limitations
We acknowledge a few potential limitations in our study. First, despite the retrospective and observational nature of this study, the relatively small number of PH patients was a major limitation. Second, possible bias in subject identification could have influenced the outcomes of this study. Third, it was not possible to simultaneously perform echocardiographic studies and RHC. Fourth, we included different types of PH, thereby making the study more heterogeneous rather than homogenous. Future studies with a larger sample size and a more comprehensive analysis between subgroups are needed; meanwhile, attention must also be paid to the reproducibility of RVLS.
Given the complex nature of the right ventricle, the measurement of strain by 3D speckle tracking, compared to 2D speckle training, may better reflect the true nature of contraction, because it includes a larger portion of the right ventricle and more strain vectors [16]. Previously, several studies have used the 3D strain to evaluate the RV dysfunction and clinical outcomes in sheep as well as in humans with PH [16, 20,21,22]. Kind et al. found that, compared to longitudinal motion, transverse motion at mid-RV reveals a significantly stronger relationship with RVEF and hence might be a better predictor of RV function [23].
Conclusions
RVLS can indirectly and sensitively reflect RV function and hemodynamic changes in PH patients, and provide a diagnosis for patients with adverse prognosis. Furthermore, it can help in the clinical evaluation of the status and severity of the disease, as well as provide more valuable information for treatment decisions for PH patients.
References
Galie N, Humbert M, Vachiery JL et al (2016) 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: the joint task force for the diagnosis and treatment of pulmonary hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 37:67–119
Lindqvist P, Soderberg S, Gonzalez MC, Tossavainen E, Henein MY (2011) Echocardiography based estimation of pulmonary vascular resistance in patients with pulmonary hypertension: a simultaneous Doppler echocardiography and cardiac catheterization study. Eur J Echocardiogr 12:961–966
Ikeda S, Tsuneto A, Kojima S, Koga S, Nakata T, Yoshida T, Eto M, Minami T, Yanagihara K, Maemura K (2014) Longitudinal strain of right ventricular free wall by 2-dimensional speckle-tracking echocardiography is useful for detecting pulmonary hypertension. Life Sci 111:12–17
Bossone E, Bodini BD, Mazza A, Allegra L (2005) Pulmonary arterial hypertension: the key role of echocardiography. Chest 127:1836–1843
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1–39):e14
Biswas M, Sudhakar S, Nanda NC, Buckberg G, Pradhan M, Roomi AU, Gorissen W, Houle H (2013) Two- and three-dimensional speckle tracking echocardiography: clinical applications and future directions. Echocardiography 30:88–105
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories (2002) ATS statement: guidelines for the six-min walk test. Am J Respir Crit Care Med 166:111–117
Humbert M, Yaici A, de Groote P et al (2011) Screening for pulmonary arterial hypertension in patients with systemic sclerosis: clinical characteristics at diagnosis and long-term survival. Arthritis Rheum 63:3522–3530
Ryan JJ, Huston J, Kutty S, Hatton ND, Bowman L, Tian L, Herr JE, Johri AM, Archer SL (2015) Right ventricular adaptation and failure in pulmonary arterial hypertension. Can J Cardiol 31:391–406
Vonk-Noordegraaf A, Haddad F, Chin KM et al (2013) Right heart adaptation to pulmonary arterial hypertension: physiology and pathobiology. J Am Coll Cardiol 62:D22–D33
Carlsson M, Ugander M, Heiberg E, Arheden H (2007) The quantitative relationship between longitudinal and radial function in left, right, and total heart pumping in humans. Am J Physiol Heart Circ Physiol 293:H636–H644
Stephensen S, Steding-Ehrenborg K, Munkhammar P, Heiberg E, Arheden H, Carlsson M (2014) The relationship between longitudinal, lateral, and septal contribution to stroke volume in patients with pulmonary regurgitation and healthy volunteers. Am J Physiol Heart Circ Physiol 306:H895–H903
Hill MR, Simon MA, Valdez-Jasso D, Zhang W, Champion HC, Sacks MS (2014) Structural and mechanical adaptations of right ventricle free wall myocardium to pressure overload. Ann Biomed Eng 42:2451–2465
Leuchte HH, El Nounou M, Tuerpe JC, Hartmann B, Baumgartner RA, Vogeser M, Muehling O, Behr J (2007) N-terminal pro-brain natriuretic peptide and renal insufficiency as predictors of mortality in pulmonary hypertension. Chest 131:402–409
Smith BC, Dobson G, Dawson D, Charalampopoulos A, Grapsa J, Nihoyannopoulos P (2014) Three-dimensional speckle tracking of the right ventricle: toward optimal quantification of right ventricular dysfunction in pulmonary hypertension. J Am Coll Cardiol 64:41–51
Dahhan T, Siddiqui I, Tapson VF, Velazquez EJ, Sun S, Davenport CA, Samad Z, Rajagopal S (2016) Clinical and echocardiographic predictors of mortality in acute pulmonary embolism. Cardiovasc Ultrasound 14:44
Park JH, Park MM, Farha S, Sharp J, Lundgrin E, Comhair S, Tang WH, Erzurum SC, Thomas JD (2015) Impaired global right ventricular longitudinal strain predicts long-term adverse outcomes in patients with pulmonary arterial hypertension. J Cardiovasc Ultrasound 23:91–99
Wright L, Dwyer N, Power J, Kritharides L, Celermajer D, Marwick TH (2016) Right ventricular systolic function responses to acute and chronic pulmonary hypertension: assessment with myocardial deformation. J Am Soc Echocardiogr 29:259–266
Murata M, Tsugu T, Kawakami T et al (2016) Prognostic value of three-dimensional echocardiographic right ventricular ejection fraction in patients with pulmonary arterial hypertension. Oncotarget 7:86781–86790
Ozawa K, Funabashi N, Takaoka H, Tanabe N, Yanagawa N, Tatsumi K, Kobayashi Y (2014) Utility of three-dimensional global longitudinal strain of the right ventricle using transthoracic echocardiography for right ventricular systolic function in pulmonary hypertension. Int J Cardiol 174:426–430
Atsumi A, Seo Y, Ishizu T, Nakamura A, Enomoto Y, Harimura Y, Okazaki T, Abe Y, Aonuma K (2016) Right ventricular deformation analyses using a three-dimensional speckle-tracking echocardiographic system specialized for the right ventricle. J Am Soc Echocardiogr 29(402–411):e402
Kind T, Mauritz GJ, Marcus JT, van de Veerdonk M, Westerhof N, Vonk-Noordegraaf A (2010) Right ventricular ejection fraction is better reflected by transverse rather than longitudinal wall motion in pulmonary hypertension. J Cardiovasc Magn Reson 12:35
Acknowledgements
This study was supported by the National Natural Science Foundation of China (Grant No. 81401420), The Fund of Beijing excellent talent training Plan (Grant No. 2013D003034000012), and The Fund of the Beijing health system high level health technology personnel discipline backbone project (Grant No. 2014-3-027).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Li, Y., Wang, Y., Meng, X. et al. Assessment of right ventricular longitudinal strain by 2D speckle tracking imaging compared with RV function and hemodynamics in pulmonary hypertension. Int J Cardiovasc Imaging 33, 1737–1748 (2017). https://doi.org/10.1007/s10554-017-1182-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-017-1182-3