Abstract
Newest 3D software allows measurements directly in the en-face-3D TEE mode. Aim of the study was to ascertain whether measurements performed in the en-face-3D TEE mode are comparable with conventional measurement methods based on 2D TEE and 3D using the multiple plane reconstruction mode with the Qlab® software. En-face-3D TEE is used more frequently in daily clinical routine during cardiac operations. So far measurements could only be done based on 2D images or with the use of multi planar reconstruction mode with additional software. Measurement directly in the 3D image (en-face-3D TEE) would make measurements faster and easier to use in clinical practice. After approval by the local ethic committee and written informed consent from the patients additionally to a comprehensive perioperative 2D TEE examination a real time (RT) 3D zoom- dataset was recorded. Routine measurements of the length of anterior and posterior mitral valve leaflets as well as mitral valve and aortic valve areas were performed in en-face-3D TEE, multiplanar reconstruction mode using Qlab®-software (Philips, Netherlands) and 2D TEE standard views. Twenty nine patients with a mean age of 67 years undergoing elective cardiac surgery/interventions were enrolled in this study. Direct measurements in en-face-3D TEE mode lead to non significant underestimation of all parameters as compared to Qlab® and 2D TEE measurements. Measurements in en-face-3D TEE are feasible but lead to non significant underestimation compared to measurements performed with Qlab® or in 2D TEE views.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
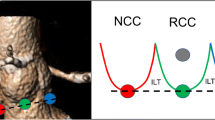
Since the introduction of real time 3D transesophageal echocardiography (RT 3D TEE) its intraoperative use has increased. It makes communication with colleagues easier [1] and creates unique images that are helpful in a variety of clinical scenarios [2]. Measurements of distances, areas and volumes based on real time (RT) 3D datasets have been proven to be more accurate compared to measurements based on two dimensional datasets [3,4,5,6]. Several studies showed the usefulness of RT 3D TEE for guiding mitral valve pathology, procedures and intraoperative assessment of cardiac disease [2, 7, 8]. But all these measurements could only be done with the help of specific software (Qlab®, Philips, Netherland) and using the multiplane reconstruction (MPR) mode that allows displaying 2–3 cross- sectional views (coronal, sagittal and transverse) simultaneously. With Q-lab® software true long and cross-sectional views can be created simultaneously which accounts for the superior accuracy of measurements compared to 2D [9]. Till now the estimation of dimensions and valve areas in RT 3D could only be done using the overlay of a grid with dots of 5 mm equidistant from each other (see Fig. 1). The latest software with RT 3D display, permits direct measurements within the RT 3D dataset, en-face-3D TEE measurements, without the need to export the dataset into special software for offline-analysis (i.e. Qlab®). The drawbacks of en-face-3D TEE measurements in RT 3D datasets, is that they are displayed on a 2D screen. This can cause underestimation of the measurement of distances and valve areas, depending on the alignment of the structure.
To the best of our knowledge no studies have been performed comparing these specific en-face-3D TEE measurements from RT 3D dataset with the standard method (i.e. 2D TEE or using MPR mode in Qlab® software) in routine clinical setting.
The aim of our study was to compare the measurement of mitral valve dimensions, mitral and aortic valve areas, using en-face-3D TEE, MPR mode and 2D images.
Method
After approval by the local ethics committee and written informed consent was received, 29 patients undergoing elective cardiac surgery and interventional cardiac procedures were enrolled in this study. All echocardiography data were anonymised and no patient could be identified by using the data. The research echocardiography data is stored for 7 years in our institutional data bank. After induction of anaesthesia, intubation and establishing routine monitoring, a comprehensive 2D TEE examination was performed in all patients using an X7-2t transducer (iE 33, Philips Amsterdam, The Netherlands) [10]. Additionally a 3D wide sector zoom- dataset of the midesophageal mitral commissural view was recorded for measurements of the mitral valve dimensions and area. During acquisition the focus was on getting the mitral valve as horizontal as possible to avoid errors in measurements due to an oblique display (see Fig. 2a–d). Aortic valve was acquired similarly using the midesophageal long axis view of the aortic valve as the basic 2D view (see Fig. 3). En-face-3D TEE measurements based on RT 3D datasets were done immediately, measurements based on MPR mode with Qlab® software and measurements performed based on the 2D images were done offline at 1-week intervals to avoid bias. The same echocardiographer (S.E.) performed all measurements following the recommendations for reporting perioperative transesophageal echo studies [11]. For the mitral valve the length of the anterior and posterior mitral leaflet, the intercommissural and anterior-posterior distances was measured. Additionally the mitral valve area was determined in mid- diastole and the aortic valve area in mid-systole using planimetry. To obtain en-face-3D TEE measurements of the mitral valve, the RT 3D wide sector zoom mode dataset was rotated 90° counter clockwise around the x-axis and then 90° in plane to acquire the surgical view of the mitral valve with the aortic valve at the top of the image (Figs. 2a, b, 3a, 4a).
Measurements of the mitral valve in 3D and MPR (a–d). Real time 3D short axis view of the mitral valve, seen from the left atrium (a) and left ventricle side (b). Multiplanar reconstruction of the 3D image, which can be cropped in multiple planes (c) to allow an en face measurement of the valve area at the actual orifice (d)
The measurements using Qlab® software (Philips, The Netherlands) and measurements using 2D images were performed in the conventional manner (see Figs. 2c, d, 3b, c, 4b): Qlab® provides the multi planar reconstruction (MPR) mode of the RT image, which features three cross sectional views of the structure of interest. The settings of the MPR mode provide two orthogonal planes intersecting the structure of interest. Using the 3D image for orientation, these planes can be adjusted by the echocardiographer to perform all measurements, which are needed.
Image quality was graded as excellent, satisfactory or poor for all of the three modalities.
Excellent image quality was obtained when no artefacts occurred and all structures needed for measurements were displayed well.
Good image quality meant some small artefacts occurred or parts of the structures to be displayed were difficult to measure owing to echo dropouts.
Poor image quality made measurements of some structures impossible or major artefacts occurred that made measurements in en-face-3D impossible.
Statistical analysis was performed using SPSS Software (Version 17). Quantitative Data were expressed as mean ± SD. Pearson correlation was performed to describe correlations between the different techniques.
P-values < 0.05 were considered statistically significant. To further examine the comparison between the methods of clinical measurements, the method of Bland and Altman was used and the limits of agreement were defined as mean ± 1.96 SD of the average differences between the methods [12].
Results
Study population: 29 patients with a mean age of 67 ± 14 years were enrolled in this study. Left ventricular ejection fraction was 53 ± 14% and the New York heart association functional class was 2.5 ± 0.7.
Seven patients underwent AV replacement, one patient AV repair, four patients CABG and AV replacement, six patients minimally invasive MV repair, one patient MV replacement, five patients a transcatheter mitral valve repair (i.e. MitraClip®), three transcatheter AV replacement were performed, one patient had an ascending aorta replacement and one patient received AV replacement and MV repair.
Twenty two patients were in sinus rhythm and seven patients presented with atrial fibrillation (see Table 1).
Image quality was graded as excellent in 16 patients (55%) using 3D vs. 18 pts (62%) using 2D and 17 pts (58%) using QLab®. Good image quality was described in 7 pts (24%) in 3D vs. 8 pts (28%) in Qlab® and 7 pts (24%) in 2D. Poor image quality was achieved in 6 pts (21%) in 3D, vs. 4 pts (14%) respectively in Qlab® and in 2D.
Calcifications of the aortic valve made planimetry of the aortic valve area were impossible in three patients in all modalities. Measurement of the mitral valve orifice area was impossible in one patient in all three modalities. Measurements in en-face-3D TEE lead to non significant underestimation of all parameters as compared to 2D and Qlab® measurements. (For details see Table 2.)
There were no statistically significant differences in these measurements; Pearson correlation showed a strong correlation (>0.7) for all measurements except for mitral valve orifice area (Table 3). The best correlation could be obtained for the AV orifice area measurements.
Bland Altman Analysis shows agreement for the three methods of measurement (see Fig. 5). There is no systematic deviation (error).
Bland Altman Analysis: en-face-3D vs. 2D; en-face-3D vs. Qlab. Horizontal lines are drawn at the mean difference, and at the limits of agreement. Limits of agreement are defined as the mean difference plus and minus 1.96 times the standard deviation of the differences. A Measurements anterior mitral leaflet length. a Anterior mitral leaflet measurements—en-face-3D TEE vs. 2D TEE. b Anterior mitral leaflet measurements–en-face-3D TEE vs. Qlab. B Measurements posterior mitral leaflet length. a Posterior mitral leaflet measurements—en face-3D TEE vs. 2D TEE. b Posterior mitral leaflet measurements—en face-3D TEE vs. Qlab. C Anterior posterior mitral annulus diameter. a Anterior–posterior diameter measurements—en-face-3D TEE vs. 2D TEE. (b) Anterior–posterior diameter measurements—en-face-3D TEE vs. Qlab. D Intercommissural diameter. a Intercommissural diameter measurements—en-face-3D TEE vs. 2D TEE. b Intercommissural diameter measurements—en-face-3D TEE vs. Qlab. E Mitral valve orifice area. a Mitral valve orifice area measurements—en-face-3D TEE vs. 2D TEE. b Mitral valve orifice area measurements—en-face-3D TEE vs. Qlab. F Aortic valve orifice area. a Aortic valve orifice area measurements—en-face-3D TEE vs. 2D TEE. b Aortic valve orifice area measurements—en-face-3D TEE vs. Qlab
Bland Altman plots indicate that the two methods of en-face-3D and Qlab® provide almost identical values for all types of measurement (Fig. 5). Whereas it showed that the mean bias is similar between en-face-3D and 2D. Only for the aortic valve orifice area all three modalities show comparable values, Fig. 5. Bland Altman plot (AV orifice area 3D/2D mean −0.23, SD ± 0.64; AV orifice area 3D/Qlab® mean −0.13, SD ± 0.45).
For the mitral valve orifice area Bland Altman plots are indicating that en-face-3D and Qlab® (MV orifice area 3D/Qlab mean −0.3, SD ± 0.98) provided almost identical values (Fig. 5e).
Discussion
We could show that measurements in en-face-3D TEE datasets are feasible but result in non-significant underestimation of the parameter compared to measurements in 2D and 3D using MPR mode.
All measurements other than planimetry of the mitral valve area showed a strong correlation between the modalities. The poor correlation of the mitral valve area between RT 3D TEE and 2D TEE is in accordance with the study of Maslow et al. who compared Qlab® measurements and 2D TEE [13]. The mitral valve annulus is not planar but saddle shaped. This non-planar geometry cannot be correctly measured in 2D TEE [14]. This might explain the poor correlation between measurements of the MV orifice area using en-face-3D and 2D TEE. One can argue that planimetry of a non-planar structure is an artefact that can not be avoided. Nevertheless planimetry of the mitral valve opening area is one of the recommended measurements for diagnosis of mitral valve stenosis [15]. The measurements in en-face-3D datasets were performed using a two- dimensional screen therefore the question raises if the measurements would be more accurate if virtual three dimensional shapes would have been used as caliper. That can only be speculated because to the knowledge of the authors no literature exists in the medical field about that problem. If the 3D printing based on 3D echocardiographic datasets [16] may help is not clear now.
RT—3D TEE improves the visualization of MV pathology and increases the accuracy of interpretation by facilitating spatial orientation [17]. One limitation of RT 3D using the wide sector mode might be the poor temporal resolution resulting in a low frame rate. We could demonstrate that, at least in this small patient population, this does not result in significant differences in the measurements. Acquisition of RT wide sector mode 3D images has the advantage to prevent stitch artefacts in patients with atrial fibrillation, because it is a single beat acquisition.
Other potential limitations of 3D TEE are poor 2D TEE images and drop out artefacts, resulting in poor 3D TEE images. We could show that if the 2D TEE images were acceptable there was no additional drop out artefacts in the en-face-3D TEE images that interfered with measurements in this modality. For good 3D TEE images 2D TEE images should be optimized. Post processing in 3D TEE is not possible [18]. Gain needs to be optimized prior acquisition first in the 2D mode and thereafter in the 3D mode. Low gain setting results in dropout, excess gain results in a decrease in resolution and a loss of 3D perspective [2].
Three patients’ aortic valve areas and one patient’s mitral valve area could not be measured in all three of the modalities.
Additionally one of the theoretical limitations of measuring in en-face-3D is that compared to multiplanar reconstruction no correction of the z-axis can be performed. We tried to compensate for this potential limitation during acquisition by ensuring that all the structures were displayed as horizontal as possible. Actually it is not possible to measure definitively in 3D TEE yet. We´ve got 3D TEE loops, but our measurements are performed on a two dimensional display. This is one problem of the actually used 3D software. Lately new methods were investigated. Using 3D datasets for creating 4D datasets. Some companies are investigating in this field. But actually this is not clinical routine. It takes a lot of time to generate a 4D dataset for making measurements and using this datasets. This might be the future but has no clinical relevance today [19]. 3D TEE is already clinical routine in transcatheter procedures like MitraClip® and transcatheter AV replacement [20, 21]. 3D TEE has become beneficial for preparation of operative procedures, intra-procedural guidance as well as monitoring for complications and device function [22]. In our institution 3D TEE is already clinical routine. Especially for mitral valve procedures, like MitraClip® procedures [23] or minimally invasive mitral valve surgery RT 3D TEE and measurements in 3D TEE are used [24]. Measurements in en-face-3D TEE can be performed quickly but lead to non significant underestimation compared to measurements performed with Qlab®. Larger studies are necessary to define the role of this modality in clinical practice.
Limitations
One limitation of this current study is the small sample size. The aim of the study was to assess the feasibility of direct measurements in en-face-3D TEE. We have not performed measurements for interoberserver variability, which is another limitation in our eyes. Studies with larger patient populations are necessary to confirm the results.
Abbreviations
- CV:
-
Chamber view
- TEE:
-
Transesophageal echocardiography
- 2D:
-
Two dimensional
- 3D:
-
Three dimensional
- RT:
-
Real time
- AV:
-
Aortic valve
- MV:
-
Mitral valve
- AML:
-
Anterior mitral leaflet
- PML:
-
Posterior mitral leaflet
- AVA:
-
Aortic valve area
- MVA:
-
Mitral valve area
- pts:
-
Patients
References
Lang RM, Tsang W, Weinert L, Mor-Avi V, Chandra S (2011) Valvular heart disease. The value of 3-dimensional echocardiography. J Am Coll Cardiol 58(19):1933–1944. doi:10.1016/j.jacc.2011.07.035
Lang RM, Badano LP, Tsang W, Adams DH, Agricola E, Buck T, Faletra FF, Franke A, Hung J, de Isla LP, Kamp O, Kasprzak JD, Lancellotti P, Marwick TH, McCulloch ML, Monaghan MJ, Nihoyannopoulos P, Pandian NG, Pellikka PA, Pepi M, Roberson DA, Shernan SK, Shirali GS, Sugeng L, Ten Cate FJ, Vannan MA, Zamorano JL, Zoghbi WA, American Society of E, European Association of E (2012) EAE/ASE recommendations for image acquisition and display using three-dimensional echocardiography. Eur Heart J Cardiovasc Imaging 13(1):1–46. doi:10.1093/ehjci/jer316
Zamorano J, Cordeiro P, Sugeng L, Perez de Isla L, Weinert L, Macaya C, Rodriguez E, Lang RM (2004) Real-time three-dimensional echocardiography for rheumatic mitral valve stenosis evaluation: an accurate and novel approach. J Am Coll Cardiol 43(11):2091–2096. doi:10.1016/j.jacc.2004.01.046
Matsumura Y, Fukuda S, Tran H, Greenberg NL, Agler DA, Wada N, Toyono M, Thomas JD, Shiota T (2008) Geometry of the proximal isovelocity surface area in mitral regurgitation by 3-dimensional color Doppler echocardiography: difference between functional mitral regurgitation and prolapse regurgitation. Am Heart J 155(2):231–238. doi:10.1016/j.ahj.2007.09.002
Cheng TO, Xie MX, Wang XF, Wang Y, Lu Q (2004) Real-time 3-dimensional echocardiography in assessing atrial and ventricular septal defects: an echocardiographic-surgical correlative study. Am Heart J 148(6):1091–1095. doi:10.1016/j.ahj.2004.05.050
Mukherjee C, Tschernich H, Kaisers UX, Eibel S, Seeburger J, Ender J (2011) Real-time three-dimensional echocardiographic assessment of mitral valve: Is it really superior to 2D transesophageal echocardiography? Ann Card Anaesth 14(2):91–96. doi:10.4103/0971-9784.81562
Grewal J, Mankad S, Freeman WK, Click RL, Suri RM, Abel MD, Oh JK, Pellikka PA, Nesbitt GC, Syed I, Mulvagh SL, Miller FA (2009) Real-time three-dimensional transesophageal echocardiography in the intraoperative assessment of mitral valve disease. J Am Soc Echocardiogr 22(1):34–41. doi:10.1016/j.echo.2008.11.008
Agricola E, Oppizzi M, Pisani M, Maisano F, Margonato A (2008) Accuracy of real-time 3D echocardiography in the evaluation of functional anatomy of mitral regurgitation. Int J Cardiol 127(3):342–349. doi:10.1016/j.ijcard.2007.05.010
Ender A, Eibel S, Hasheminejad E, Scholz M, Kaisers UX, Mukherjee C, Ender J (2012) Real-time 3 dimensional full volume data set : benefits in problem focused intraoperative transesophageal echocardiography. Anaesthesist 61(10):875–882. doi:10.1007/s00101-012-2088-z
Shanewise JS, Cheung AT, Aronson S, Stewart WJ, Weiss RL, Mark JB, Savage RM, Sears-Rogan P, Mathew JP, Quinones MA, Cahalan MK, Savino JS (1999) ASE/SCA guidelines for performing a comprehensive intraoperative multiplane transesophageal echocardiography examination: recommendations of the American Society of Echocardiography Council for Intraoperative Echocardiography and the Society of Cardiovascular Anesthesiologists Task Force for Certification in Perioperative Transesophageal Echocardiography. Anesth Analg 89(4):870–884
Feneck R, Kneeshaw J, Fox K, Bettex D, Erb J, Flaschkampf F, Guarracino F, Ranucci M, Seeberger M, Sloth E, Tschernich H, Wouters P, Zamorano J (2010) Recommendations for reporting perioperative transoesophageal echo studies. Eur J Echocardiogr 11(5):387–393. doi:10.1093/ejechocard/jeq043
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–310
Maslow A, Mahmood F, Poppas A, Singh A (2014) Three-dimensional echocardiographic assessment of the repaired mitral valve. J Cardiothorac Vasc Anesth 28(1):11–17. doi:10.1053/j.jvca.2013.05.007
Grewal J, Suri R, Mankad S, Tanaka A, Mahoney DW, Schaff HV, Miller FA, Enriquez-Sarano M (2010) Mitral annular dynamics in myxomatous valve disease: new insights with real-time 3-dimensional echocardiography. Circulation 121(12):1423–1431. doi:10.1161/CIRCULATIONAHA.109.901181
Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP, Iung B, Otto CM, Pellikka PA, Quinones M (2009) Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. Eur J Echocardiogr 10(1):1–25. doi:10.1093/ejechocard/jen303
Giannopoulos AA, Steigner ML, George E, Barile M, Hunsaker AR, Rybicki FJ, Mitsouras D (2016) Cardiothoracic Applications of 3-dimensional Printing. J Thorac Imaging 31(5):253–272. doi:10.1097/RTI.0000000000000217
Hien MD, Rauch H, Lichtenberg A, De Simone R, Weimer M, Ponta OA, Rosendal C (2013) Real-time three-dimensional transesophageal echocardiography: improvements in intraoperative mitral valve imaging. Anesth Analg 116(2):287–295. doi:10.1213/ANE.0b013e318262e154
Hung J, Lang R, Flachskampf F, Shernan SK, McCulloch ML, Adams DB, Thomas J, Vannan M, Ryan T, Ase (2007) 3D echocardiography: a review of the current status and future directions. J Am Soc Echocardiogr 20(3):213–233. doi:10.1016/j.echo.2007.01.010
Noack T, Mukherjee C, Kiefer P, Emrich F, Vollroth M, Ionasec RI, Voigt I, Houle H, Ender J, Misfeld M, Mohr FW, Seeburger J (2015) Four-dimensional modelling of the mitral valve by real-time 3D transoesophageal echocardiography: proof of concept. Interact Cardiovasc Thorac Surg 20(2):200–208. doi:10.1093/icvts/ivu357
Zamorano JL, Badano LP, Bruce C, Chan KL, Goncalves A, Hahn RT, Keane MG, La Canna G, Monaghan MJ, Nihoyannopoulos P, Silvestry FE, Vanoverschelde JL, Gillam LD (2011) EAE/ASE recommendations for the use of echocardiography in new transcatheter interventions for valvular heart disease. J Am Soc Echocardiogr 24(9):937–965. doi:10.1016/j.echo.2011.07.003
Lang RM, Badano LP, Tsang W, Adams DH, Agricola E, Buck T, Faletra FF, Franke A, Hung J, de Isla LP, Kamp O, Kasprzak JD, Lancellotti P, Marwick TH, McCulloch ML, Monaghan MJ, Nihoyannopoulos P, Pandian NG, Pellikka PA, Pepi M, Roberson DA, Shernan SK, Shirali GS, Sugeng L, Ten Cate FJ, Vannan MA, Zamorano JL, Zoghbi WA, American Society of E, European Association of E (2012) EAE/ASE recommendations for image acquisition and display using three-dimensional echocardiography. J Am Soc Echocardiogr 25(1):3–46. doi:10.1016/j.echo.2011.11.010
Morbach C, Lin BA, Sugeng L (2014) Clinical application of three-dimensional echocardiography. Prog Cardiovasc Dis 57(1):19–31. doi:10.1016/j.pcad.2014.05.005
Guarracino F, Baldassarri R, Ferro B, Giannini C, Bertini P, Petronio AS, Di B, V, Landoni G, Alfieri O (2014) Transesophageal echocardiography during MitraClip(R) procedure. Anesth Analg 118(6):1188–1196. doi:10.1213/ANE.0000000000000215
Ender J, Sgouropoulou S (2013) Value of transesophageal echocardiography (TEE) guidance in minimally invasive mitral valve surgery. Ann Cardiothorac Surg 2(6):796–802. doi:10.3978/j.issn.2225-319X.2013.10.09
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
After approval by the local ethics committee and written informed consent was received, 29 patients undergoing elective cardiac surgery and interventional cardiac procedures were enrolled in this study. This study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Rights and permissions
About this article
Cite this article
Eibel, S., Turton, E., Mukherjee, C. et al. Feasibility of measurements of valve dimensions in en-face-3D transesophageal echocardiography. Int J Cardiovasc Imaging 33, 1503–1511 (2017). https://doi.org/10.1007/s10554-017-1141-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-017-1141-z