Abstract
To evaluate the accuracy and feasibility of right ventricular function parameters measurement using 320-slice volume cardiac CT. Retrospective analysis of 50 consecutive patients (23 men, 27 women) with suspected pulmonary diseases was performed in electrocardiogram (ECG)-gated cardiac CT and cardiac magnetic resonance (CMR). Parameters including right ventricular end-diastolic volume (RVEDV), right ventricular end- systolic volume (RVESV), right ventricular stroke volume (RVSV), right ventricular cardiac output (RVCO), and right ventricular ejection fraction (RVEF) were semi-automatically and separately calculated from both CT and CMR data. Significant difference between measurements was measured by paired t test and two-variable linear regression analysis with Pearson’s correlation coefficient. Bland–Altman analysis was performed in each pair of parameters. There was little variability between the measurements by the two observers (kappa = 0.895–0.980, P < 0.05). There was good correlation between all parameters obtained by CT and CMR (P < 0.001): RVEDV (108.5 ± 21.9 ml, 113.5 ± 24.8 ml, r = 0.944), RVESV (69.8 ± 33.4 ml, 73.2 ± 35.4 ml, r = 0.972), RVSV (39.0 ± 13.2 ml, 40.2 ± 13.3 ml, r = 0.977), RVCO (2.6 ± 0.7 l, 2.6 ± 0.7 l. r = 0.958), RVEF (38.8 ± 19.1 %, 39.1 ± 19.3 %, r = 0.990), and there was no significant difference between CT and CMR measurements in RVEF (n = 50, t = −0.677, P > 0.05). 320-slice volume cardiac CT is an accurate non-invasive technique to evaluate RV function.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The right ventricle (RV) is affected by and contributes to a number of cardiovascular disease processes. Therefore, assessment of right ventricular function is of pivotal importance in selecting the optimal treatment method and predicting prognosis in clinic [1]. However, the complex geometric shape of the RV and heavy trabeculation of the free wall complicate edge recognition [2]. The importance of the RV is recognized in certain conditions, such as in follow-up of some corrected and non-corrected congenital heart diseases [3, 4]. Non-invasive methods for evaluating RV function include 2-dimensional (2D) and 3-dimensional (3D) echocardiography and cardiac radionuclide, which still have some limitations [5]. Cardiac magnetic resonance (CMR) can be used to accurately assess RV volume and has been regarded as the reference standard for RV function assessment. The drawbacks of CMR include long examination time, exclusion of patients with metal implants, claustrophobia, etc. Cardiac CT, because of increased spatial and temporal resolution, has been well established for evaluation of the left ventricle function, as it can accurately calculate the left ventricular (LV) volume and LV ejection fraction [6–8]. The assessment of the right heart on chest CT can give additional information with regard to some diseases, such as pulmonary embolism and pulmonary hypertension. This comprehensive evaluation of pulmonary parenchyma, vessels, and heart has emerged as a new trend in thoracic imaging [9–11].
Many studies have reported that CMR and multi-detector row CT (MDCT) were the most accurate techniques to measure the RV volume and ejection fraction because of their high spatial and temporal resolution [12, 13], but it is still hard to achieve “iso-tropic” and “iso-phasic” in conventional multi-slice CT (MSCT). 320-slice volume cardiac CT has 175 ms temporal resolution with 160 mm of Z axis length, which could cover the entire heart in one single scan. The purpose of this study was to evaluate the feasibility and accuracy of right ventricular function parameter measurements using ECG-gated 320-slice volume cardiac CT in comparison to cardiac MR imaging.
Materials and methods
Retrospective analysis of 50 consecutive patients (23 men and 27 women, mean age 55 ± 9.6 years) with clinically suspected pulmonary artery diseases was performed during August and December 2009. All patients provided informed consent. All cases underwent both 320-slice volume cardiac CT and CMR on the same day.
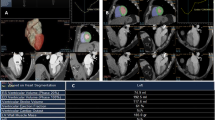
During a single breath hold (lasting 5 s or less), single heartbeat ECG-gated 320-slice volume cardiac CT (Aquilion ONE, Toshiba Medical Systems, Otawara, Japan) was performed with the following volume scanning parameters: 100 kVp, 250 mA, collimation 0.5 mm, rotation time 0.35 s, range 160 mm, field-of-view 320 mm. Automatic tube current monitoring technology was used to reduce the radiation exposure and ensure the image quality. No β-blocker preparation was used. All patients had a regular ventricular rhythm during the examination. Contrast injection was done using 45 ml nonionic contrast agent (Omnipaque 350 mgI/ml, GE, USA) at a flow rate of 4.5 ml/s, followed by 45 ml saline at the same flow rate. From early systole to late diastole (0–95 % R–R interval), volume data from 20 phases were reconstructed at 5 % intervals with slice thickness of 0.5 mm. The RV volume was defined from RV apex to tricuspid valve level. The RV outflow tract to the pulmonary valve was included. Semi-automatic contour detection of the RV was performed, as well as manual correction if necessary. RV function-related parameters including right ventricular end-diastolic volume (RVEDV), right ventricular end- systolic volume (RVESV), right ventricular stroke volume (RVSV), right ventricular cardiac output (RVCO), and right ventricular ejection fraction (RVEF) were calculated using Cardiac Function Analysis (CFA) software in VITAL-fx workstation (Toshiba, Japan) (Figs. 1, 2).
All the patients were examined on a 1.5T whole body MR scanner (Magnetom Sonata, Siemens, Germany) on the same day. An eight-element phase-array torso coil was used, and true fast imaging with steady precession (True FISP) sequence (TR/TE, 29.28 ms/1.08 ms; flip angle, 50°) with retrospective ECG-gated was used to acquire dynamic cine loops of RV. The RV was entirely imaged from the base to the apex in 10–14 short-axis cine images, composed of section thickness of 5 mm with no gap and a 450 mm field-of-view. The cine loops were blindly analyzed offline with commercial software (Argus, Siemens Medical Solution, Germany). Endocardial contour at end-systole and end-diastole were manually drawn in a similar fashion as volume cardiac CT (Fig. 3).
All of these measurements were blindly measured by two experienced observers. The data was analyzed using SPSS11. All variables were recorded as mean ± SD. The consistency between two observers was analyzed via kappa test. Significance of differences between the measurements was analyzed by a paired t test and two-variable linear regression analysis with Pearson’s correlation coefficient.
Results
RVEDV (108.5 ± 21.9 ml, 113.5 ± 24.8 ml; r = 0.944), RVESV (69.8 ± 33.4 ml, 73.2 ± 35.4 ml; r = 0.972), RVSV (39.0 ± 13.2 ml, 40.2 ± 13.3 ml; r = 0.977), RVCO (2.6 ± 0.7 l, 2.6 ± 0.7 l; r = 0.958), RVEF (38.8 ± 19.1 %, 39.1 ± 19.3 %; r = 0.990). And there was no significant difference between CT and CMR measurements in RVEF (n = 50, t = −0.677, P > 0.05), but differences of RVEDV, RVESV, RVSV and RVCO were significant (n = 50, t = −4.177 to 2.518, P < 0.05) (Table 2).
The distribution of demographics was described in Table 1. The consistency between the two observers was favorable (κ = 0.895–0.980, P < 0.05). RVEDV (108.5 ± 21.9 ml, 113.5 ± 24.8 ml; r = 0.944), RVESV (69.8 ± 33.4 ml, 73.2 ± 35.4 ml; r = 0.972), RVSV (39.0 ± 13.2 ml, 40.2 ± 13.3 ml; r = 0.977), RVCO (2.6 ± 0.7 l, 2.6 ± 0.7 l; r = 0.958), RVEF (38.8 ± 19.1 %, 39.1 ± 19.3 %; r = 0.990). And there was no significant difference between CT and CMR measurements in RVEF (n = 50, t = −0.677, P > 0.05), but differences of RVEDV, RVESV, RVSV and RVCO were significant (n = 50, t = −4.177 to 2.518, P < 0.05) (Table 2). Compared with CMR, the systematic errors (mean difference) and the 95 % limits of agreement (1.96 SD around the difference) were as follows: RVEDV (−4.9 ml; 95 % CI, 11.4 to −21.3 ml), RVESV (−3.5 ml; 95 % CI, 12.8 to −19.7 ml), RVSV (−1.3 ml; 95 % CI, 4.3 to −6.8 ml), RVCO (−0.07L; 95 % CI, 0.31 to −0.45 l) and RVEF (−0.3 %; 95 % CI, 5.1 to −5.6 %) (Fig. 4). Except RVEF and RVCO, the volume CT measurements underestimated CMR in all parameters. The mean radiation dose was 2.7 ± 0.5 mSv with a conversion factor of 0.014.
Discussion
Because we utilized whole heartbeat acquisition without small blood vessel structure analysis, the data of single complete R–R interval image reconstruction and degree of contrast enhancement did not affect the RV function measurement by 320-slice volume cardiac CT, even though some of the patients had high heart rates ranging from 70 to 80 beats per minute. In our study, we found excellent agreement between the 320-slice volume cardiac CT and CMR. The results of our studies illustrate that 320-slice volume cardiac CT allows reliable assessment of RV function when compared with CMR. It also shows that there is no significant difference between 320-slice volume cardiac CT and CMR measurements in RVEF. Compared with CMR, it showed good agreement with the values of RVEF and RVCO, while the other data were slightly underestimated.
The factors contributing to difference in RV analysis were analyzed as follows. (1) Limited temporal resolution. High temporal resolution was needed to overcome motion artifacts and to allow accurate measurement of RV function. Although we could use two or three heartbeats per acquisition to reduce temporal resolution to 50 ms, this was not done as the radiation dose and amount of contrast agent needed would significantly increase. (2) CMR has the advantage of enabling cardiac functional assessment. However, cardiac CT was not the first line examination for our assessment. It could possibly affect the adequacy of the data of cardiac function assessment due to increases in the preload and volume. (3) It was still difficult to accurately detect the outline of the right ventricular myocardium as the soft tissue resolution of volume cardiac CT is lower than CMR. We drew the shape of the right ventricular endocardium including papillary muscles and trabeculae in order to improve consistency. (4) In order to avoid the potential influence on cardiac function, rate-controlling drugs such as beta-blockers were not used in this study.
There are several advantages in 320-slice volume cardiac CT. First, there are almost no contraindications, except iodine contrast agent allergy and renal dysfunction. It additionally enables a comprehensive application in cardiovascular diseases. Second, there is only a 1-s scanning time and 5-s breathhold for the whole examination. Third, Manses believed [14] that half-segmental reconstruction was the most appropriate method for image quality and temporal resolution in cardiac functional assessment in MSCT. Thus, there is a significant advantage of the super-wide detectors and 16-cm coverage of volume CT for the cardiac function assessment as in our study. The radiation dose and the amount of contrast agent were much lower than conventional cardiac CT. In our study, a total of 45 ml of contrast agent were used in 320-slice volume cardiac CT, which is significantly lower than 80–100 ml contrast agents in conventional cardiac CT [15]. Mean radiation dose was 2.7 ± 0.5 mSv, which is also much lower than conventional MSCT. Finally, RV function is an important prognostic factor not only in the right heart and pulmonary circulation diseases, but also in various left heart diseases, which are currently of increasing concern.
There are several limitations to this study. First, the sample size was small and should be increased in the future study. Secondly, most of the current cardiac function software is for left ventricular function analysis, which leads to difficulty in RV contour detection. The software for RV function analysis needs to improve.
Conclusion
320-slice volume cardiac CT is an accurate and non-invasive technique to evaluate RV function.
References
Menzel T, Kramm T, Bruckner A, Mohr-Kahaly S, Mayer E, Meyer J (2002) Quantitative assessment of right ventricular volumes in severe chronic thromboembolic pulmonary hypertension using transthoracic three-dimensional echocardiography: changes due to pulmonary thromboendarterectomy. Eur J Echocardiogr 3(1):67–72
Liang L, Xu W, Li K, Du X, Gao Y (2009) Assessment of right ventricular function with 64-detector CT. Chin J Med Imaging Technology 25(6):1025–1028
Oldershaw P (1992) Assessment of right ventricular function and its role in clinical practice. Br Heart J 68(1):12–15
Goldstein J (2005) The right entricle: what’s right and what’s wrong. Coron Artery Dis 16:1–3
Barkhausen J, Ruehm SG, Goyen M, Buck T, Laub G, Debatin JF (2001) MR evaluation of ventricular function: true fast imaging with steady-state precession versus fast low-angle shot cine MR imaging: feasibility study. Radiology 219(1):264–269
Mogelvang J, Stubgaard M, Thomsen C, Henriksen O (1988) Evaluation of right ventricular volumes measured by magnetic resonance imaging. Eur Heart J 9(5):529–533
Grothues F, Moon JC, Bellenger NG, Smith GS, Klein HU, Pennell DJ (2004) Interstudy reproducibility of right ventricular volumes, function, and mass with cardiovascular magnetic resonance. Am Heart J 147(2):218–223. doi:10.1016/j.ahj.2003.10.005
Helbing WA, Bosch HG, Maliepaard C, Rebergen SA, van der Geest RJ, Hansen B, Ottenkamp J, Reiber JH, de Roos A (1995) Comparison of echocardiographic methods with magnetic resonance imaging for assessment of right ventricular function in children. Am J Cardiol 76(8):589–594
Danilouchkine MG, Westenberg JJ, de Roos A, Reiber JH, Lelieveldt BP (2005) Operator induced variability in cardiovascular MR: left ventricular measurements and their reproducibility. J Cardiovasc Magn Reson 7(2):447–457
Ghaye B, Ghuysen A, Bruyere PJ, D’Orio V, Dondelinger RF (2006) Can CT pulmonary angiography allow assessment of severity and prognosis in patients presenting with pulmonary embolism? What the radiologist needs to know. Radiographics 26(1):23–39. doi:10.1148/rg.261055062 discussion 39–40
Hoey ET, Gopalan D, Agrawal SK, Screaton NJ (2009) Cardiac causes of pulmonary arterial hypertension: assessment with multidetector CT. Eur Radiol 19(11):2557–2568. doi:10.1007/s00330-009-1460-0
Spencer KT, Garcia MJ, Weinart L, Vignon P, Lang R (1999) Assessment of right ventricular and right atrial systolic and diastolic performance using automated border detection. Echocardiography 16(7, Pt 1):643–652
Thorne MC (1992) 1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP 21(1–3):51–52. doi:0306-4549(92)90053-E
Manzke R, Grass M, Nielsen T, Shechter G, Hawkes D (2003) Adaptive temporal resolution optimization in helical cardiac cone beam CT reconstruction. Med Phys 30(12):3072–3080
Wintersperger BJ, Nikolaou K (2005) Basics of cardiac MDCT: techniques and contrast application. Eur Radiol 15(Suppl 2):B2–B9
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huang, X., Pu, X., Dou, R. et al. Assessment of right ventricular function with 320-slice volume cardiac CT: comparison with cardiac magnetic resonance imaging. Int J Cardiovasc Imaging 28 (Suppl 2), 87–92 (2012). https://doi.org/10.1007/s10554-012-0156-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-012-0156-8