Abstract
Purpose
The objective of this study is to document the prevalence of traditional, complementary, and alternative medicine (TCAM) use by adult cancer patients at a national teaching hospital in Malawi. We aim to document the products/therapies used, the reason for use, as well as patient-reported satisfaction with TCAM practitioners and modalities.
Methods
We conducted investigator-administered interviews with adult cancer patients presenting to the Kamuzu Central Hospital (KCH) Cancer Clinic in Lilongwe, Malawi between January and July 2018. The KCH is a national teaching hospital in the capital of Lilongwe, which serves patients with cancer from the northern half of Malawi. Descriptive statistics were used to describe TCAM use and logistic regression was applied to identify predictors of TCAM.
Results
A total of 263 participants completed the survey, of which 70% (n = 183) were female and average age was 45 (SD 14) years old. The prevalence of overall TCAM use was 84% (n = 222), and 60% (n = 157) of participants reported combining TCAM with conventional cancer treatment. The majority of patients used TCAM to directly treat their cancer versus for symptom management. Patients reported using faith-based healing (64%, n = 168), herbal medicine (56%, n = 148), diet change (46%, n = 120), and vitamins/minerals (23%, n = 61). Participants reported the highest satisfaction for physicians among practitioners and diet change for modalities. Female gender was found to be a predictor of TCAM with conventional treatment use, no other significant predictors were observed.
Conclusion
There is a high prevalence of TCAM use among an adult population with cancer in Malawi, and a wide variety in the TCAM modalities used among patients. Additional studies are needed to identify risks and benefits of TCAM use to assist with policy and public health, patient safety, and holistically address the global burden of cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is the second leading cause of death globally, accounting for an estimated 9.6 million deaths in 2018 [1]. While significant advances have been made in cancer prevention, diagnostics, and treatment, low- and middle-income countries (LMICs) remain unprepared and lack resources to address this significant public health concern [2]. Only 26% of low-income countries have diagnostic pathology services, and only 30% have cancer treatment services available [3]. There also exists a disparity in cancer incidence and mortality among country income levels. Greater than 60% of new cancer cases occur in regions with high concentrations of LMICs including Africa, Asia, Central America, and South America [4]. These same regions account for greater than 70% of cancer deaths worldwide [4]. Only one in five LMICs have cancer data and monitoring available (i.e., cancer registration) to make informed policy decisions [3]. With high cancer burden and limited cancer care infrastructure available, patients in LMICs often rely on traditional, complementary, or alternative medicine (TCAM) for their cancer treatment and support.
Traditional medicine is loosely defined as, “the sum total of the knowledge, skills and practices based on the theories, beliefs and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health, as well as in the prevention, diagnosis, improvement or treatment of physical and mental illnesses”[5]. Traditional medicine, complementary medicine, and alternative medicine are terms often used interchangeably or concurrently. Common treatment modalities of TCAM include herbal medicine, vitamins/minerals, faith-based practices, and dietary change [5].
In Africa, TCAM is commonly used to treat a variety of ailments including cancer, diabetes, mental health disorders, and prenatal conditions [6,7,8,9]. There is a lack of data on the prevalence of TCAM in low-income countries, especially in sub-Saharan Africa (SSA) [10]. The prevalence of TCAM in low-income countries is estimated at 40–71% for all uses, and in SSA is estimated at 58% [11,12,13,14,15]. The median prevalence of TCAM use for cancer in LMICs is 55%, and 50% in SSA [10]. TCAM tends to be less expensive in comparison to Western conventional medicine and remains more accessible to populations in LMICs [11].
High income countries often have data monitoring systems in place to identify TCAM modalities used among cancer patients [16,17,18]. However, there is limited information on the specific modalities and products used by cancer patients in LMICs [10]. A systematic review of TCAM use among cancer patients found peer-reviewed TCAM data available from only 9.7% of all low-income countries and 21.2% lower-middle-income countries [10]. The review found only 20 studies worldwide provided information on specific TCAM products and modalities used by cancer patients in low and lower-middle-income countries, with herbal medicine and spiritual/religious healing being the only two modalities documented among all world regions. Documenting TCAM may help improve the delivery of conventional cancer treatment (chemotherapy, surgery, radiation) by acknowledging cultural norms, addressing herb/drug interactions [19], improving TCAM disclosure to providers [20, 21], and identifying potentially harmful practices. [22,23,24] To our knowledge, there is no peer-reviewed research on the TCAM modalities and products used by cancer patients in Malawi.
Although public sector health facilities are located throughout Malawi, access to these facilities and services available at these facilities can be limited. For many cancer patients, receiving more advanced medical treatment requires travel to a larger city in Malawi such as Lilongwe or Blantyre. This travel requires time, payment for transportation, and payment for services at the urban referral centers. Moreover, recent findings from a qualitative study by our group in Malawi indicated that TCAM is much more widely available throughout communities and represents a more affordable option than conventional care, due to both reduced transportation expenses and lower treatment costs [24]. Therefore, we sought to describe patient-reported frequency of traditional medicine use among adult patients with cancer to help inform the cancer treatment process in Malawi. The objective of this study is to document traditional, complementary, and alternative medicines used for cancer treatment and/or support by adult patients with cancer at a national teaching hospital in Lilongwe, Malawi.
Methods
Setting and Recruitment
We conducted investigator-administrated surveys among adult cancer patients presenting to the Kamuzu Central Hospital (KCH) Cancer Clinic between January and July 2018. The KCH is a national teaching hospital in the capital of Lilongwe, which serves cancer patients from the northern half of Malawi, with a catchment area of approximately 9 million. The KCH Cancer Clinic was initiated by UNC (University of North Carolina) Project Malawi, and at the time of this study staffed by two oncologists and four internists. The clinic provides diagnostic pathology and medical oncology services including chemotherapy, with multidisciplinary involvement of surgeons as needed. Currently, there is no radiotherapy in Malawi.
We used purposive sampling of cancer patients and approached them to inquire interest in completing the survey in the waiting room or treatment area of the KCH cancer clinic. Participants expressing interest were explained the details of the study and presented with a written informed consent, which was required for participation in the study. Participants either signed the consent form or provided a fingerprint with accompanying witness signature if the participant was illiterate. Eligibility requirements included the following: (1) being at least 18 years old; (2) previous or current diagnosis of cancer; (3) willingness to provide informed consent; and (4) mentally and physically able to participate. All participants received the equivalent of 5 USD in Malawian Kwacha for completing the study. This study was approved by the UNC Institutional Review Board and the National Health Science Research Committee of Malawi.
Survey
Author’s JH, RS, QL, SG, and JSS contributed to survey creation. The survey for this study was an expanded and adapted version of the International Complementary and Alternative Medicine Questionnaire (I-CAM-Q) [25]. It was available in both English and Chichewa and data collection was completed using REDCap software on tablet computers in real time by author AM. Four domains were used to structure the survey, include the following: (1) patient demographics and medical history part 1, (2) participant’s use of traditional, complementary, or alternative medicine and types of practitioners seen, (3) timing of symptoms, seeking a traditional healer, and seeking care at the KCH hospital, and (4) patient demographics and medical history part 2. For each provider seen, participants were asked the number of times which they saw the provider in the past 3 months, reason for seeing provider (e.g., to directly treat cancer, to treat cancer symptoms, to treat both the cancer and symptoms, or other) and satisfaction with provider. Provider type definitions were provided to participants if needed. For each TCAM product/therapy used, participants were asked if they are currently using the therapy, number of times using the therapy in the past 3 months, reason for use (to directly treat cancer, to treat cancer symptoms, to treat both the cancer and symptoms, or other), and satisfaction with that modality. Use of either TCAM or conventional cancer care (chemotherapy, surgery, radiation) was defined as using any modality related to TCAM or conventional care at least 1 time for managing symptoms of cancer and/or for directly treating cancer. The survey used for this study is available in supplemental data Table 1.
Our target sample size was not predetermined due to pragmatic constraints such as the lack of information on expected number of cancer patients who will present to the clinic and be available for study participation, and lack of similar studies within Malawi to help determine an adequate sample size. Therefore, data collection was set for 6 months with 1 interviewer available 5 days weekly to conduct interviews. We assessed for data saturation (defined as obtaining an estimated < 5% of new information to reach a new information threshold) after 6 months of data collection and determined our sample size was sufficient to reach saturation.
Statistical analysis
To decide which variables to include in the logistic regression analysis we reviewed current literature for variables which have previously been shown to be related to the use of complementary, integrative, and/or traditional medicine. To identify predictors for overall usage of TCAM, we first tested the bivariate associations between various covariates and the response (TCAM use) by using the Pearson’s chi-squared test for categorical covariates (gender, marital status, education, residence (village vs city), socioeconomic status (running water and electricity in house), and ethnic group) and the two-sample t-test for continuous covariate (age). Then, we fitted a logistic regression model using all above covariates to predict the odds of being a TCAM user. To identify predictors for combined use of TCAM and conventional cancer care, the same analyses were performed. That is, we first performed bivariate association analyses between these groups, then we fitted another logistic regression model using all above covariates to differentiate combined treatment users and subjects receiving only conventional cancer care. Descriptive statistics, including counts and percentages for categorical variables, and mean and standard deviation for continuous variables, were used to present all other data. Descriptive statistics were calculated using Excel, and all other analyses were performed using the R program.
Results
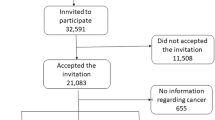
A total of 279 participants were approached to participate in the survey, of which 263 provided consent and completed the survey. The following were reasons provided by participants who declined to participate: did not have cancer/could not confirm they have cancer (n = 5), did not have time to participate (n = 4), not ready/comfortable providing informed consent (n = 2), no reason provided (n = 2), not comfortable discussing topic (n = 1), not old enough to participate (n = 1), not physically able to participate (n = 1). None of the participants declined to finish the survey once started.
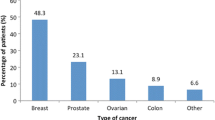
Complete demographic data for the survey participants are shown in Table 1. The participants were 70% (n = 183) female with a mean age of 45 years old (SD 14). The majority were married (57%, n = 151) with a varied range of completed education; from no education (23%, n = 60) to completing college (7%, n = 18). The most common cancer type was cervical cancer (35%, n = 91) followed by hematological (21%, n = 56), breast (15%, n = 40), and skin/Kaposi sarcoma (11%, n = 28). A relatively large percent of participants did not know their cancer type (10%, n = 25). Most participants lived in villages outside of the urban city setting (71%, n = 188), and the median distance to the nearest healthcare facility was 3 km (range 0.1–70). Access to running water and electricity in the home were documented as indicators of socio-economic status. Most participants did not have access to running water in their homes (72%, n = 189) or have access to electricity in their homes (79%, n = 209). Just over one-third of survey participants were HIV-positive (33%, n = 88) and most survey participants identified with the Chewa ethnic/tribal group (52%, n = 138).
Prevalence of TCAM use, reasons for seeking care, and perceived satisfaction with care provided
When including prayer as a traditional medicine, 84% (n = 222) of participants reported using a TCAM modality for either cancer symptom reduction or to directly treat cancer (Table 2). When discounting prayer as a traditional medicine, 77% (n = 202) of participants report using TCAM for their cancer care. A total of 60% (n = 157) of participants reported combining a TCAM modality with their conventional cancer care at the time of the survey, and 40% (n = 106) reported using conventional medicine alone.
All participants reported seeing a physician for their cancer treatment since the survey was completed at KCH while participants received care. TCAM providers sought by participants are listed in Table 2. No participants reported seeking an acupuncturist or homeopath. The average number of times participants visited each provider in the past 3 months are: Physician (3.7 visits), Herbalist/Sing’anga (0.7 visits), Prophet (2.2 visits), Faith-Based Healer (2.1 visits), and Chiropractor (1 visit). For this study, we define Prophet as a spiritual healer who speaks on behalf of a divine being and/or foresees future events, and when reported by participants is not associated with a specific religion. A faith-based healer is defined as a spiritual leader of an established religion (ex. Christianity, Islam). Table 3 details participant reasons for seeing various providers. Table 4 summarizes participant-reported satisfaction with providers, with highest satisfaction attributed to physicians (70%, n = 185 reported being very satisfied), and lowest satisfaction attributed to local traditional healers (1%, n = 1 reported very satisfied).
The TCAM modalities used for cancer are provided in Table 5. The percent of participants who reported currently using the following modalities at the time of the survey include herbal medicine (21%, n = 48), vitamins and minerals (25%, n = 17), faith-based healing (54%, n = 102), and diet change (92%, n = 95). Table 3 provides the reported reasons each participant used TCAM modalities, and Table 4 summarizes patient-reported satisfaction for these modalities, with the highest satisfaction attributed to diet change (88%, n = 91 reporting very satisfied), and lowest satisfaction attributed to herbal medicine (16%, n = 37 reporting very satisfied). Only one individual reported the potential use of animal medicine, but was not certain if the medicine was actually derived from an animal. Therefore, animal medicine was not included in our analysis.
TCAM therapies and treatments used for cancer care
Table 5 lists the most common types of faith-based healing practices, herbal medicines, diet changes, and vitamins and minerals used for cancer care. Participants reported a wide range of TCAM products and practices used, including 49 different forms of herbal medicine and 23 different dietary changes. A full list of reported products and practices for all TCAM modalities can be found in supplemental data Table 2. Products used for herbal and vitamin and mineral treatments were largely unknown, and participants were often unaware or intentionally not informed of the names or other specifics regarding the products they purchased or were provided during treatment. Several participants reported combination herbal products. For this study, we report herbal products and vitamins/minerals individually according to number of mentions, regardless of if they were used independently or in combination with other products.
Predictors of TCAM use
Table 6 provides the results of our logistic regression models to examine predictors of overall TCAM use and TCAM use concomitantly with conventional treatment. Female gender was found to be a predictor of TCAM with conventional treatment use (p = 0.02), no other significant predictors were observed.
Discussion
To our knowledge, this is the first study to document specific TCAM modalities and providers used among adult patients with cancer in Malawi, and one of the few studies documenting TCAM in SSA. Overall, we found most participants use a variety of TCAM services for disease management, both independently and in combination with conventional care. Our findings represent an important step in understanding how TCAM is used to treat cancer (a non-communicable disease), as well as how two of the most common, although distinct, healthcare services in Malawi are used in parallel. Our findings share similarities with previous studies of TCAM in the SSA region. Erku et al. documented traditional medicine use among 195 patients with cancer receiving chemotherapy in Ethiopia using cross-sectional questionnaires and found 72% reported using herbal medicine, 39% special foods/diet change, 36% spiritual healing, and 22% dietary supplements [26] . A total of 79% of participants reported using a form of TCAM in the Ethiopian study, similar to our 84% of participants reporting TCAM use [26]. In addition, Ezeome et al. interviewed 160 patients with cancer who presented to the University of Nigeria Teaching Hospital and found 65% of patients reported TCAM use, including 52% reporting herbal medicine use and 49% using faith-based healing [27] . The prevalence of TCAM reported among 119 patients with cancer during structured interviews in the radiotherapy department of the Muhimbili Medical Center in Tanzania was 45%, with 36% reporting the use of herbal medicine [28] . In a systematic review including studies from Nigeria, Ethiopia, and Ghana, 73% of patients with cancer reported using TCAM, and 55% of the general population throughout SSA countries used TCAM and conventional care concurrently, similar to our finding of 60% of patients combining TCAM with conventional cancer treatment [15] . It is also worth highlighting previous efforts to build collaboration between traditional healers and biomedical organizations [29], which is an effort supported by the World Health Organization Traditional Medicine Strategy [14] .
Our study population was well represented across age (18–81 years old) but was mostly female (70%). The most common cancer types were cervical, hematological, and breast, which is likely influenced by the majority female study population, high incidence of cervical and breast cancers among women in Malawi, as well as lack of adequate cancer screening and prevention methods in Malawi such as HPV testing, vaccination, and mammography [30, 31]. Our population was of lower socioeconomic status, as indicated by limited access to running water and electricity in the home. A high prevalence of HIV-positive patients was documented, likely due to a high burden of HIV-related malignancies in Malawi [32, 33] . Of interest, none of our demographic covariates used in the regression analysis were found to be predictors of general TCAM use for cancer care. This is in contrast to studies in higher-income countries which found age, education, and female gender predict use of complementary medicine [34]. However, our study did find female gender does predict combining TCAM with conventional medicine. This is also supported by qualitative focus groups among adult patients with cancer in Malawi as well [24].
The most common form of TCAM reported was faith-based healing, described almost exclusively as some form of prayer. All forms of faith-based prayer, such as prophetic (provided by a spiritual healer who speaks on behalf of a divine being and/or foresees future events) as well as prayer associated with a larger established religion (ex. Christianity, Islam), were included in the modality analyses. However, seeking a prophet versus a faith-based healer (pastor, priest, bishop, etc.) was separated for the analysis for type of practitioners patronized. Faith-based healers were the most used provider for TCAM; however, only about half of those who discussed using faith-based healing reported seeing a faith-based healer. This is likely due to self-administration of faith-based practices, or the delivery of faith-based practices by someone not considered an official healer. This is similar among the other forms of TCAM [24].
Herbal medicines were used by over half of participants, although practitioners sought for these treatments was again lower. Herbal medicine is of particular importance when considering the greater impact TCAM may have on the treatment of cancer in Malawi due to the potential of herb/drug interactions, toxic herbal products, as well as the significant percent of our participants reporting they did not know which herbs they were using. Focus groups conducted among this same study population reported herbalist often do not disclose which herbs they supply to patients to maintain proprietary rights to their herbal formulas as well as prevent patients from self-gathering and administering herbal products [24]. This could be considered a significant public health issue that prevents the safe use and clinical management of herbal products.
Satisfaction with traditional healers and herbal medicines was relatively low among our study participants. Participants expressed frustration with traditional healers and herbal medicine due to an inability to control symptoms, inability to formally diagnose cancer, and/or inability to cure them of their cancer [24] . Often, participants first seek traditional healers when experiencing symptoms of cancer, and only reflexively seek conventional care when traditional methods are unable to provide adequate results [24]. This may lead to dissatisfaction with traditional healing once a pathological diagnosis of cancer is provided. Evidence from our current study supports this hypothesis as participants report that, in the majority of cases, the reason they sought a TCAM practitioner and/or used a TCAM modality was to directly treat their cancer, and not for symptom management.
Unfortunately, because this is patient-reported data, we are unable to verify the species names of most of the plants/herbs mentioned by our participants. This is beyond the scope of this study and would require additional resources and methodology. We are also unable to identify a few herbs that were only reported using local Chichewa names. There are variations in the Chichewa terminology used for herbal products. We consulted with local providers regarding the herbs reported in local terminology, but they were also unable to identify a specific plant/herb associated with the names reported. Further investigation to identify the herbs mentioned in this study is an avenue for future research and could lead to laboratory-based analysis of herbal products to help avoid herb/drug interactions or toxicity, and/or help investigate any oncologist-initiated inquiry regarding discussion of herbal medicines in the clinical setting.
Dietary measures were another form of TCAM that was widely used for cancer care, with 46% (n = 120) reporting a change in diet and 23% (n = 61) noting vitamin and mineral use. These findings are in line with others from the region which describe faith- and biological-based treatments as the most common TCAM modalities used throughout SSA [15] . Participants expressed strong satisfaction with their diet change. In addition, diet change was common among participants actively receiving conventional treatment for their cancer. However, our survey was unable to capture who advised our participants to change their diet. Given the high prevalence and satisfaction as well as limited risk of side effects, diet change appears to be a strong candidate for future research efforts and potential interventions to support adult patients with cancer.
Strengths of our study include a sample of patients with a variety of cancer types, large age range, as well as collecting data on the specific TCAM modalities used by patients. In addition, we were able to capture why patients use TCAM as well as their satisfaction with TCAM, which is often not recognized in similar studies. A limitation of our study includes selection bias since our study population was recruited while in the waiting room or treatment area of the KCH cancer clinic. We were also unable to capture data on patients in more rural locations who may not present to a hospital for treatment. The KCH has a catchment area of 9 million people, and Malawi has a population of 18 million people (2018), and; therefore, our results are not representative of the total cancer population in Malawi. In addition, the investigator-administered interview study design presents the possibility of investigator bias when designing the interview guide or conducting the interviews. To reduce the risk of investigator bias we developed our structured survey based off the previously validated International Complementary and Alternative Medicine Questionnaire (I-CAM-Q). A large portion of our survey was closed-ended quantitative questions to reduce the risk of investigator interpretation. The local interviewer (author AM) also underwent extensive training by members of the research team with experience conducting research interviews on the appropriate conduct of administering surveys and methods to reduce and avoid bias. The interviewer also completed mock-interviews to demonstrate competency with delivering interviewer-administered surveys.
Conclusion
This study highlights the importance of considering TCAM practices and practitioners for cancer care in LMICs. Prevalence of TCAM use among our adult Malawian population with cancer at the KCH is notably high, with wide variation in the types of modalities and practitioners seen for cancer care. Additional studies are needed to capture a nationally representative sample and support policy development and the expansion of new cancer control programs, ideally with productive collaboration between TCAM and conventional providers in LMICs to maximize benefits and minimize harms.
Data availability
See supplemental data files for survey materials used for this study.
References
Global Cancer Observatory (n.d.) http://gco.iarc.fr/ . Accessed 28 Jan 2020
Cancer. World Health Organization 2018. https://www.who.int/news-room/fact-sheets/detail/cancer . Accessed 28 Jan 2020
World Health Organization WHO Cancer Factsheet 2018. http://www.who.int/mediacentre/factsheets/fs297/en/ Accessed 20 Dec 2016
Stewart B, Wild C (2014) World Health Organization World Cancer Report 2014
World Health Organization (2000) General guidelines for methodologies on research and evaluation of traditional medicine. World Health Organization, Geneva
Mureyi DD, Monera TG, Maponga CC (2012) Prevalence and patterns of prenatal use of traditional medicine among women at selected harare clinics: a cross-sectional study. BMC Complement Altern Med. https://doi.org/10.1186/1472-6882-12-164
Kpobi L, Swartz L (2018) ‘That is how the real mad people behave’: beliefs about and treatment of mental disorders by traditional medicine-men in Accra, Ghana. Int J Soc Psychiatry 64:309–316. https://doi.org/10.1177/0020764018763705
Lunyera J, Wang D, Maro V, Karia F, Boyd D, Omolo J et al (2016) Traditional medicine practices among community members with diabetes mellitus in Northern Tanzania: an ethnomedical survey. BMC Complement Altern Med. https://doi.org/10.1186/s12906-016-1262-2
Stanifer JW, Patel UD, Karia F, Thielman N, Maro V, Shimbi D et al (2015) The determinants of traditional medicine use in northern Tanzania: a mixed-methods study. PLoS ONE 10:e0122638. https://doi.org/10.1371/journal.pone.0122638
Hill J, Mills C, Li Q, Smith JS (2019) Prevalence of traditional, complementary, and alternative medicine use by cancer patients in low income and lower-middle income countries. Glob Public Health 14:418–430. https://doi.org/10.1080/17441692.2018.1534254
Bodeker G, Kronenberg F (2002) A public health agenda for traditional, complementary, and alternative medicine. Am J Public Health 92:1582–1591
Bannerman R, Burton J, Chien W (1993) Traditional medicine and healthcare coverage. World Health Organization, Geneva
World Health Organization (2002) WHO traditional medicine strategy 2002–2005. WHO Traditional Medicine Strategy World Health Organization, Geneva
World Health Organization (2013) WHO traditional medicine strategy 2014–2023. World Health Organization, Geneva
James PB, Wardle J, Steel A, Adams J (2018) Traditional, complementary and alternative medicine use in Sub-Saharan Africa: a systematic review. BMJ Glob Health 3:895. https://doi.org/10.1136/bmjgh-2018-000895
John GM, Hershman DL, Falci L, Shi Z, Tsai WY, Greenlee H (2016) Complementary and alternative medicine use among US cancer survivors. J Cancer Surviv 10:850–864. https://doi.org/10.1007/s11764-016-0530-y
Wode K, Henriksson R, Sharp L, Stoltenberg A, Hök NJ (2019) Cancer patients’ use of complementary and alternative medicine in Sweden: a cross-sectional study. BMC Complement Altern Med 19:62. https://doi.org/10.1186/s12906-019-2452-5
Berretta M, Della Pepa C, Tralongo P, Fulvi A, Martellotta F, Lleshi A et al (2017) Use of complementary and alternative medicine (CAM) in cancer patients: an Italian multicenter survey. Oncotarget 8:24401–24414. https://doi.org/10.18632/oncotarget.14224
Block KI, Gyllenhaal C (2002) Clinical corner: herb-drug interactions in cancer chemotherapy: theoretical concerns regarding drug metabolizing enzymes. Integr Cancer Ther 1:83–89. https://doi.org/10.1177/1534735402001001007
Davis EL, Oh B, Butow PN, Mullan BA, Clarke S (2012) Cancer patient disclosure and patient-doctor communication of complementary and alternative medicine use: a systematic review. Oncologist 17:1475–1481. https://doi.org/10.1634/theoncologist.2012-0223
Obrist M, Osei-Bonsu E, Awuah B, Watanabe-Galloway S, Merajver SD, Schmid K et al (2014) Factors related to incomplete treatment of breast cancer in Kumasi, Ghana. Breast 23:821–828. https://doi.org/10.1016/j.breast.2014.08.014
Dunyo SK, Ahorlu CK, Simonsen PE (1997) Scarification as a risk factor for rapid progression of filarial elephantiasis. Trans R Soc Trop Med Hyg 91:446
Letsyo E, Jerz G, Winterhalter P, Beuerle T (2017) Toxic pyrrolizidine alkaloids in herbal medicines commonly used in Ghana. J Ethnopharmacol 202:154–161. https://doi.org/10.1016/J.JEP.2017.03.008
Hill J, Seguin R, Phanga T, Manda A, Chikasema M, Gopal S et al (2019) Facilitators and barriers to traditional medicine use among cancer patients in Malawi. PLoS ONE. https://doi.org/10.1371/journal.pone.0223853
Quandt SA, Verhoef MJ, Arcury TA, Lewith GT, Steinsbekk A, Kristoffersen AE et al (2009) Development of an international questionnaire to measure use of complementary and alternative medicine (I-CAM-Q). J Altern Complement Med (New York, NY) 15:331–339. https://doi.org/10.1089/acm.2008.0521
Erku DA (2016) Complementary and alternative medicine use and its association with quality of life among cancer patients receiving chemotherapy in Ethiopia: a cross-sectional study. Evid-Based Complement Altern Med 2016:1–8. https://doi.org/10.1155/2016/2809875
Ezeome ER, Anarado AN (2007) Use of complementary and alternative medicine by cancer patients at the University of Nigeria Teaching Hospital, Enugu, Nigeria. BMC Complement Altern Med 7:28. https://doi.org/10.1186/1472-6882-7-28
Alexander GA (1982) A survey of traditional medical practices used for the treatment of malignant tumors in an East African population. Soc Sci Med 1985(20):53–59
Kayombo EJ, Uiso FC, Mbwambo ZH, Mahunnah RL, Moshi MJ, Mgonda YH (2007) Experience of initiating collaboration of traditional healers in managing HIV and AIDS in Tanzania. J Ethnobiol Ethnomed 3:6. https://doi.org/10.1186/1746-4269-3-6
Msyamboza KP, Phiri T, Sichali W, Kwenda W, Kachale F (2011) Cervical cancer screening uptake and challenges in Malawi from 2011 to 2015: Retrospective cohort study. BMC Public Health 2016:16. https://doi.org/10.1186/s12889-016-3530-y
Pfaff C, Singano V, Akello H, Amberbir A, Berman J, Kwekwesa A et al (2018) Early experiences in integrating cervical cancer screening and treatment into HIV services in Zombacentral hospital, Malawi. Malawi Med J 30:211–214. https://doi.org/10.4314/mmj.v30i3.14
Rohner E, Kasaro M, Msadabwe-Chikuni SC, Stinson K, Mohamed Z, Tweya H et al (2017) Treatment and outcome of AIDS-related Kaposi sarcoma in South Africa, Malawi and Zambia: an international comparison. Pan Afr Med J 28:261. https://doi.org/10.11604/pamj.2017.28.261.11300
Shumay DM, Maskarinec G, Gotay CC, Heiby EM, Kakai H (2002) Determinants of the degree of complementary and alternative medicine use among patients with cancer. J Altern Complement Med 8:661–671. https://doi.org/10.1089/107555302320825183
Gross AM, Liu Q, Bauer-Wu S (2007) Prevalence and predictors of complementary therapy use in advanced-stage breast cancer patients. J Oncol Pract 3:292–295. https://doi.org/10.1200/jop.0762001
Funding
University of North Carolina, Chapel Hill, Lineberger Comprehensive Cancer Center Tier 1 Pilot Development Award. The Research Fellowship in Complementary and Integrative Health (5T32AT003378-12) from the National Center for Complementary and Integrative Health provided salary support for Dr. Hill.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Disclaimer
This work was completed while Dr. Satish Gopal was employed at the University of North Carolina at Chapel Hill. The opinions expressed in this article are the authors own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States Government.
Ethical approval
This study has been approved by the University of North Carolina Institutional Review Board (Protocol #17-0933) as well as the National Health Science Research Committee of Malawi (Protocol #21711).
Consent for participation
All study participants provided written informed consent for participation.
Consent for publication
Consent for publication was included in the written informed consent signed by each participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hill, J., Seguin, R., Manda, A. et al. Prevalence of traditional, complementary, and alternative medicine (TCAM) among adult cancer patients in Malawi. Cancer Causes Control 33, 1047–1057 (2022). https://doi.org/10.1007/s10552-022-01563-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-022-01563-0