Abstract
Purpose
The Risk of Pediatric and Adolescent Cancer Associated with Medical Imaging (RIC) Study is quantifying the association between cumulative radiation exposure from fetal and/or childhood medical imaging and subsequent cancer risk. This manuscript describes the study cohorts and research methods.
Methods
The RIC Study is a longitudinal study of children in two retrospective cohorts from 6 U.S. healthcare systems and from Ontario, Canada over the period 1995–2017. The fetal-exposure cohort includes children whose mothers were enrolled in the healthcare system during their entire pregnancy and followed to age 20. The childhood-exposure cohort includes children born into the system and followed while continuously enrolled. Imaging utilization was determined using administrative data. Computed tomography (CT) parameters were collected to estimate individualized patient organ dosimetry. Organ dose libraries for average exposures were constructed for radiography, fluoroscopy, and angiography, while diagnostic radiopharmaceutical biokinetic models were applied to estimate organ doses received in nuclear medicine procedures. Cancers were ascertained from local and state/provincial cancer registry linkages.
Results
The fetal-exposure cohort includes 3,474,000 children among whom 6,606 cancers (2394 leukemias) were diagnosed over 37,659,582 person-years; 0.5% had in utero exposure to CT, 4.0% radiography, 0.5% fluoroscopy, 0.04% angiography, 0.2% nuclear medicine. The childhood-exposure cohort includes 3,724,632 children in whom 6,358 cancers (2,372 leukemias) were diagnosed over 36,190,027 person-years; 5.9% were exposed to CT, 61.1% radiography, 6.0% fluoroscopy, 0.4% angiography, 1.5% nuclear medicine.
Conclusion
The RIC Study is poised to be the largest study addressing risk of childhood and adolescent cancer associated with ionizing radiation from medical imaging, estimated with individualized patient organ dosimetry.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of medical imaging has increased substantially over the last two decades although at a slower pace in recent years [1, 2]. While computed tomography (CT) has improved diagnostic capabilities, it has also increased patient exposure to ionizing radiation, a known carcinogen [3, 4]. Radiography, fluoroscopy, angiography, and nuclear medicine are other imaging modalities that employ ionizing radiation, and while their rates have declined, use remains high [2]. Exposure to ionizing radiation from medical imaging is especially concerning for children and adolescents whose radiation-induced cancer risks are greater than adults due to rapid cellular turnover and longer life expectancy [5].
Although rare, cancer is the leading cause of death by disease among children in North America. In the United States (U.S.) in 2021, it is estimated that 15,590 children and adolescents age 0 to 19 years will be diagnosed with cancer, and 1,780 will die of their disease [6]. For childhood cancers (age 0–14 years), leukemia is the most common (28%), followed by brain and other nervous system tumors (27%) [6]. For adolescent cancers (age 15–19 years), brain and other nervous system tumors (21%) and lymphoma (19%) are the most common, followed by leukemia (13%) [6]. The causes of most childhood and adolescent cancers are unknown, although genetic mutations, Down syndrome, and fetal and childhood exposure to ionizing radiation are established risk factors, particularly for leukemia [7].
Several epidemiological studies have assessed cancer risk associated with radiation exposure from medical imaging in children, primarily from CT imaging, and each has used a different approach to estimate childhood exposures [4, 8,9,10]. A large retrospective study conducted in the United Kingdom [4] (n = 178,604 for leukemia analysis) collected the CT imaging protocols and average machine parameters and used these data to estimate average patient exposures. A study in the Netherlands [10] (n = 168,394) obtained individual parameters from CT scans to calculate patient-specific doses. Two additional studies from Australia [9] (n = 10,939,680) and South Korea [8] (n = 12,068,821) used administrative claims to assess exposure to CT (and other imaging tests for the South Korean study) without direct quantification of individual organ doses. Overall, these studies found that children and adolescents who underwent CT imaging had a small but statistically significant elevated risk of developing leukemia, brain tumors, and other solid cancers. However, study limitations included lack of detailed information on radiation exposures, no individual dosimetry calculations, and incomplete outcome data. Except for the South Korean study [8], exposures from other imaging modalities were not examined.
In this manuscript, we describe the methods and cohorts for a U.S.-Canadian longitudinal study that we are conducting to determine the association between cumulative exposure to radiation from medical imaging and risk of cancers among children and adolescents followed through age 20 years from six U.S. health care systems and the province of Ontario, Canada. Unlike previous investigations, our study includes detailed individualized organ-specific dosimetry for CT in pregnant women and children, and newly modeled dosimetry to estimate organ absorbed doses associated with other imaging modalities including fluoroscopy, angiography, radiography, and nuclear medicine. Further, we have detailed clinical data on important confounders such as Down syndrome, as well as clinical indication on a subset of the cohort. Our goal is to enrich the evidence base with one of the largest and most comprehensive studies to date in this very important area of clinical care and public health, focusing on radiation-induced cancer risk from medical imaging in children and adolescents.
Methods
Study sites
The Risk of Pediatric and Adolescent Cancer Associated with Medical Imaging (RIC) Study is a multi-site, retrospective longitudinal cohort study that collected patient imaging data for CT, fluoroscopy, angiography, radiography, and nuclear medicine from 1995 to 2016 and incidence data for childhood and adolescent cancers from 1996 to 2017 among individuals enrolled in six U.S. healthcare systems and individuals living in Ontario, Canada who were eligible for the Ontario Health Insurance Plan [2, 11]. The U.S. sites were selected to provide a sample of healthcare systems with sociodemographic and geographic diversity, and for whom we could accurately assess the comprehensive use of medical imaging and cancer outcomes. The U.S. systems include Kaiser Permanente (KP) Northern California (KPNC), Hawaii (KPHI), and Northwest (KPNW), each staff model Health Maintenance Organizations. Also included are KP Washington (KPWA), Marshfield Clinic Health System (MC), and Harvard Pilgrim Health Care (HPHC, contributed data from 2000 to 2017 only), which are mixed model organizations where patients received care and/or health insurance from their health systems. Supplemental Table 1 provides details on the U.S. study sites including geographic coverage. Ontario is the largest province by population in Canada, and nearly all residents are eligible to receive care through the Ontario Health Insurance Plan. Together, these sites were pooled to create a large and diverse North American cohort of individuals with comprehensive health insurance coverage of sufficient sample size to conduct overall and sensitivity analyses as guided by key research questions.
This study was approved by institutional review boards at each participating study site. Given this is a minimal risk, medical record review study, participant informed consent was waived.
Data sources
For U.S. sites, complete medical diagnoses and imaging utilization were available through the Virtual Data Warehouse (VDW), a collaborative data model structure developed by the National Cancer Institute-supported Cancer Research Network and Health Care Systems Research Network [12, 13]. The VDW is a distributed system located behind individual site firewalls and consists of a series of data tables with information on all medical care utilization among enrollees received across delivery settings from clinical and administrative data sources, including the electronic health record (EHR). Imaging received outside the healthcare system is ascertained via claims data. Data for this study were obtained from each site through distributive SAS programs.
For Ontario, complete medical diagnoses and imaging utilization data were ascertained through physician billing records available in the Ontario Health Insurance Plan database, hospital discharge records available in the Discharge Abstract Database, and emergency department visits available in the National Ambulatory Care Reporting System. The Canadian datasets were linked using unique encoded identifiers and analyzed separately before being aggregated with the U.S. data.
Established quality assurance methods including targeted chart review within and across the study sites were used to ensure complete capture of imaging utilization.
Identification of study cohorts
Two study cohorts were developed to examine multiple windows of medical radiation exposure and their possible associations with cancer risk in children and adolescents. These include those exposed only during the fetal period, those exposed only during childhood, and those exposed during both periods. The fetal-exposure cohort includes children for whom fetal exposures could be assessed because their mothers were enrolled in the health care system during gestation, whereas the childhood-exposure cohort includes children born within the healthcare system and with at least 6 months continuous enrollment (Fig. 1).
For the fetal-exposure cohort, eligibility criteria included births with a gestational age between 24 and less than 43 weeks from January 1, 1996 to December 31, 2016 and the mother's enrollment in the health system for the entire pregnancy to ensure complete capture of medical imaging while the child was in utero [11]. The start date of the pregnancy was estimated based on last menstrual period, or if unknown, on the child’s birthdate and gestational age at birth. In the U.S., live births were identified from birth registries, linkages to state birth certificate data, and/or International Classification of Diseases, 9th and 10th Revision (ICD-9, ICD-10) and Current Procedural Terminology (CPT) live birth codes. In Ontario, live births were identified by linking newly registered infants in the health plan with their mothers’ records of delivery. Children were followed until age 21 years, cancer diagnosis, death, or December 31, 2017, whichever came first (Fig. 2).
For the childhood-exposure cohort, eligibility criteria consisted of being born into the health system between January 1, 1996 and April 30, 2016, being continuously enrolled for at least 6 months after birth, being alive and cancer-free at 6 months of life, and having received at least one clinical visit within the health system within first 3 months of life (to exclude children who may be dual-insured). Children were followed until 6 months post-health plan disenrollment (U.S. sites only due to linkage to state cancer registries, see below for details), age 21 years, cancer diagnosis, death, or December 31, 2017, whichever came first. We imposed the 6-month post-disenrollment window because our main risk analyses include a 6-month lag between exposure to medical radiation and potential risk of cancer, and we do not need complete capture of medical imaging during this lag period.
Imaging utilization
Diagnostic imaging in the U.S. cohorts was ascertained using administrative claims based on a combination of Current Procedural Terminology (CPT), International Classification of Disease (ICD-9 and ICD-10), and Healthcare Common Procedure Coding System (HCPCS) billing codes, including modifiers for the technical, physician, or global components. Exams were included irrespective of the physician specialty billing for the study. Included codes were mapped to an anatomic area and modality to ensure consistency over time [2]. In Ontario, Canadian Classification of Health Intervention codes were used to create a crosswalk with the U.S. codes.
Abstraction and estimation of individualized patient-level radiation absorbed doses for computed tomography (CT)
During the study exposure period (1995–2016), the approach for acquiring, recording, and storing CT images changed, transitioning from film to digital. For CTs in the film era (the exact date varied across participating sites), the radiation exposure parameters were manually abstracted by trained staff at each U.S. site (except HPHC did not participate) and Ontario, following a detailed instruction manual. Manually abstracted data were entered into a custom Microsoft Access database which alerted the abstractor of out of range values in real time so they could be corrected immediately as needed. To ensure consistency and accuracy of data across all study sites, a quality assurance program developed in SAS was run on each site’s abstracted data to flag outliers for re-checking. Then each site resolved all outliers prior to data harmonization. For the digital era, the U.S. sites collected radiation parameters in DICOM format using a radiation dose management software (Radimetrics®, Bayer HealthCare LLC, Whippany, NJ). Consistent with the manually abstracted data, outliers in the DICOM data were flagged and resolved prior to data harmonization. KPWA and Ontario manually abstracted data for CTs regardless of digital availability. Given its large study population, Ontario abstracted a sample of 2,294 CTs from primarily the largest pediatric hospital in the province, The Hospital for Sick Children (40%), along with a convenience sample of CTs done at other small hospitals and clinics in the province. Also, HPHC was unable to directly abstract individual CT dose parameters, thus average doses for a given anatomic area imaged, patient age and size, and exam year will be used. This approach will also be used for exams that sites were unable to abstract for various reasons, e.g., the films were destroyed, or the exam was performed outside the healthcare system. Data were harmonized across study sites and time periods, errors and missingness identified, CTs re-abstracted as needed, and a final exposure dataset created.
The following CT acquisition variables were collected for each irradiating event: anatomic area imaged, use of intravenous contrast, scan length, anterior–posterior and lateral body dimensions on the image slice at the center of the scan range, whether a fixed or modulated tube current was employed, mA (milliampere) or (mAs (milliampere-second) [including min, max, and most frequent if a modulated tube current was employed], kVp (kilovoltage peak), tube rotation time, volume CT dose index (CTDIvol), and dose-length product (DLP).
For each abstracted CT exam from the U.S. sites, the patient's closest height and weight measurement to the date of the imaging study, either before or after, was obtained from the EHR. When either height or weight was not available on the day of the imaging examination, its value was imputed using all height/weight measurements available in the EHR before and following the imaging exam date. For pregnant women, we imputed missing heights using a combination of methods depending on how close available height measurements were to the exam date and the age at exam. This included using a model for pregnant women under 18 years of age, and the closest available height for women older than 18 years. We imputed weight for pregnant women using empirical Bayes estimates from a mixed effects model with a fixed effect for gestational age, modeled as piecewise linear regression with a separate slope for gestational days less than 100 days and more than 100 days, and random slopes and intercepts. When we could not estimate a height or weight, the 50th percentile was assumed based on the age at exam.
For imaging performed at any age in full-term infants and for pre-term infants, at a gestational age at birth plus current age of 50 weeks and older, biologically implausible height and weight values were identified and removed using publicly available SAS macros [14, 15]. For pre-term infants with imaging performed at a gestational age at birth plus current age of < 50 weeks, we identified implausible values using the same methods as the SAS macros, with LMS (lambda = skew, mu = median, sigma = standard deviation) parameters obtained from Dr. Tanis Fenton [16]. For children under 3 years of age at time of imaging with at least 5 measurements, we imputed height and weight using a modified exponential restricted growth curve \(Y=a-b{e}^{-ct}\) where the symbol t stands for age, fitted separately for each child using PROC NLMIXED in SAS. For all other children with at least one measurement, we imputed height and weight using functional principal component analysis [17] fit with the fdapace package in R [18]. When we could not estimate a height or weight, the 50th percentile was assumed based on the age at exam. Height and weight data were not available for abstracted CT exams from Ontario. Instead, effective diameter, calculated from the abstracted anterior–posterior and lateral body dimensions on the exam, was available to estimate patient size.
For childhood exposures, the University of Florida/National Cancer Institute (UF/NCI) hybrid computational phantom library was used for patient-dependent organ dose reconstruction based on detailed CT acquisition parameters and patient size [19]. The UF/NCI phantom library includes an array of 168 whole-body anatomic models of pediatric patients (90 males and 78 females) covering a range of body heights and weights consistent with current U.S. body morphometry data. For fetal exposures, 30 hybrid phantoms of the developing fetus [20] and pregnant mother [21] were created corresponding to five weight percentiles for six gestational ages. Study participants were matched to a given phantom within the UF/NCI library based on height, weight, and/or effective diameter, and for fetal exposures, also gestational age [22, 23]. A separate paper describing the dosimetry work is under development.
Estimation of average organ doses for radiography, fluoroscopy, angiography, and nuclear medicine
Average absorbed doses were estimated for radiography, fluoroscopy, angiography, and nuclear medicine. For radiography, a literature review was performed to determine the scanning parameters for the 16 most common pediatric exam types across film, computed, and digital radiography (4 common exam types in pregnant patients), and comparable fetal and child organ dose libraries are being assembled for these radiography exams. For child fluoroscopy, we abstracted dose parameters through detailed chart review from KPNC for a sample of patients who underwent the four most common exam types: upper gastrointestinal series, lower gastrointestinal series, voiding cystourethrogram, and modified barium swallow. Using these dose parameters, the UF team developed an organ dose library for these exam types with each exam modeled on 162 individual pediatric phantoms within the UF/NCI library [24]. The remaining fluoroscopy and angiography exams were modeled from these exams. Fetal fluoroscopy doses were extrapolated from the literature for early pregnancy, and three, six, and nine-month gestational ages [25, 26]. For nuclear medicine, child organ dose estimates for 25 exam types were based on age-specific International Commission on Radiological Protection (ICRP) reference biokinetic models for common diagnostic radiopharmaceuticals using estimated administered activities (AA) obtained from review of sample health plan weight-based dosing guidelines which were further constrained by both minimum and maximum values of the AA [27]. Fetal nuclear medicine doses were estimated from the literature [28] and mapped to the same exam types using the uterine wall dose as a fetal organ dose surrogate for very early stages of pregnancy, and whole-body fetal dose estimates at the end of each trimester for later periods of pregnancy.
Cancer outcome ascertainment
For the U.S. sites, we identified cancer diagnoses from January 1, 1996 to December 31, 2017 primarily from the VDW tumor table at each site, which originates from the individual site’s linkages with the NCI Surveillance, Epidemiology, and End Results (SEER)-affiliated or local accredited health system cancer registries, with additional linkages to state cancer registries. All International Classification of Diseases for Oncology, 3rd Edition (ICD-O-3) histology and topography codes were extracted. For benign brain tumors, which were not reportable until 2001, we identified cases from ICD-9 and ICD-10 codes from each site’s electronic data sources.
Across sites, 40–65% of U.S. patients disenrolled from their health plan prior to the end of the study period. To ensure more complete capture of cancer outcomes in patients who disenrolled from the health plans, we conducted linkages based on geographically close state North American Association of Central Cancer Registries, migration patterns [29], and available resources. KPNC, KPNW, and KPWA did a multi-site linkage with the California, Oregon, and Washington state cancer registries. KPNC conducted an additional linkage with the Texas State Cancer Registry based on migration patterns from California. KPHI conducted a linkage of their disenrolled cohort members with the Hawaii Tumor Registry, MC conducted linkages of all their cohort members with the Wisconsin Cancer Reporting System, and HPHC conducted linkages of all their cohort members with the Massachusetts Cancer Registry.
For Ontario, the Ontario Cancer Registry (OCR) and Pediatric Oncology Group of Ontario Networked Information System (POGONIS) were accessed for cancer diagnoses using the same ICD-O-3 codes. The OCR is a population-based legislatively mandated registry that records all incident malignant tumors within the province. The identification of benign tumors was done through POGONIS only, a population-based active cancer registry that collects data on all tumors that are diagnosed and/or treated at one of five tertiary pediatric care centers in the province.
Childhood leukemia classification
We classified leukemia morphology codes into five categories using a modification of the SEER mapping to International Classification of Childhood Cancer, 3rd Edition (ICCC-3) categories updated for hematopoietic codes based on the World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues (2008) [30, 31]. The five categories are acute lymphoid leukemia, acute myeloid leukemia, chronic leukemia and myeloproliferative disease, myelodysplastic syndrome (MDS) and other myeloproliferative disease (not including transient), and unspecified and other specified leukemias. The SEER mapping was modified to create “chronic myeloproliferative disorders and leukemias” a separate category from acute leukemias (Supplemental Table 2). Given that MDS was not reportable in SEER until 2001, we used ICD-9 codes to identify these cases in our electronic data sources followed by confirmation via chart review.
Key confounders
Children with cancer susceptibility syndromes, most importantly Down syndrome, are at increased risk of childhood leukemia [8, 32, 33]. Children with Down syndrome were identified from ICD-9 code 758.0 and ICD-10 diagnosis codes Q90.0, Q90.1, Q90.2, and Q90.9 in the U.S. sites and ICD-10 diagnosis codes only from Ontario [33]. Future analyses will be run excluding children with cancer susceptibility syndromes. Socioeconomic status (SES) [34, 35] and race/ethnicity [36,37,38] have also been found to be associated with childhood leukemia. Neighborhood-level SES measures including median household income, education, and neighborhood deprivation index [39] were collected in the U.S. sites using the U.S. Census Bureau American Community Survey 5-year estimate data. Addresses for children at the time of birth were geocoded and linked to SES data at the census-tract level. In Ontario, neighborhood income quintile was measured using postal codes at time of birth for children linked to Canadian census income data. Race/ethnicity data were available in the U.S. sites only for future subgroup analyses. These data were not available in Ontario as residents are not asked to report this information.
Statistical analysis
The current paper reports primarily descriptive characteristics. The cumulative incidence rates for leukemia, other cancer, and death were estimated treating the other two outcomes as competing risks and censoring individuals at the end of follow-up [40]. All analyses were run in SAS 9.4 (SAS Institute, Cary, NC).
Results
Description of the two cohorts
The fetal-exposure cohort includes 3,474,000 children who were born between 24 and 42 weeks of gestation (median 40 weeks, 1st and 3rd quartiles = 38 and 40 in the U.S. sites; median 40 weeks, 1st and 3rd quartiles = 39 and 40 in Ontario) from 3,417,597 unique pregnancies and 2,170,104 women (Table 1). These children were followed through age 20 years or the end of the study period for a median of 11 years (1st and 3rd quartiles = 6 and 16) in the U.S. sites and 10 years (1st and 3rd quartiles = 5 and 16) in Ontario. There were slightly more males (51%) than females (49%). The U.S. children were predominantly white (63%), followed by Asian (24%), Black (9%), Hawaiian/Pacific Islander (3%), and Other (0.7%), with 17% Hispanic ethnicity. A very small proportion of children had Down syndrome (0.1%). Children in the U.S. sites were more likely to live in neighborhoods with higher median household income than the U.S. population, with only 7% having incomes less than the 3rd quartile, whereas the income distribution in Ontario cohort matched the quartiles of the population in that province.
The childhood-exposure cohort includes 3,724,632 children. The median age at end of follow-up was 5 years (1st and 3rd quartiles = 2 and 9) in the U.S. sites and 11 years (1st and 3rd quartiles = 6 and 16) in Ontario (Table 1). The sex, Down syndrome, and racial/ethnic distributions were nearly identical to the fetal cohort.
Childhood cancer and all-cause mortality
In the fetal-exposure cohort, 2,394 childhood leukemia cases, among whom 1,776 were acute lymphoid leukemia and 557 were acute myeloid leukemia, were confirmed over 37,659,582 person-years of follow-up, leading to an estimated cumulative incidence rate through age 20 years of 94/100,000 children in the U.S. and 114/100,000 in Ontario (Table 2). A total of 4,212 other childhood cancers were confirmed with a cumulative incidence rate of 229/100,000 children in the U.S. sites and 297/100,000 children Ontario. There were 10,950 all-cause deaths with a cumulative incidence rate of 429/100,000 children in the U.S. and 509/100,000 children in Ontario.
In the childhood-exposure cohort, 2,372 childhood leukemia cases, among whom 1,810 were acute lymphoid leukemia and 521 were acute myeloid leukemia, were confirmed over 36,190,027 person-years of follow-up (Table 2). The cumulative incidence rate through age 20 years was 114/100,000 children in the U.S. and 111/100,000 in Ontario. A total of 3,986 other childhood cancers were confirmed with a cumulative incidence of 256/100,000 children in the U.S. and 282/100,000 in Ontario. There were 4,915 all-cause deaths with a cumulative incidence rate of 344/100,000 children in the U.S. and 324/100,000 in Ontario.
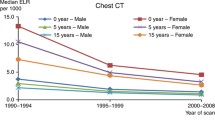
Utilization of CT imaging exams
For the fetal-exposure cohort, 0.5% of children’s mothers had at least one CT exam during pregnancy, which was more common during the first (33.8%) and third trimesters (31.4%) (Table 3). The majority were CTs of the head and/or neck (48.2%) followed by chest (25.5%) and abdomen (19.4%). 4.1% of exams imaged multiple areas.
For the childhood-exposure cohort, 5.9% had at least one CT exam (Table 3). About 19.4% of CT exams occurred in children less than one year of age, 44.0% in children age 1–9 years, and 36.7% in children age 10–20 years. The majority of CTs were head and/or neck (70.9%) followed by abdomen (13.0%). 4.7% of exams imaged multiple areas.
Utilization of non-CT imaging exams
In the fetal-exposure cohort, 4.0% of mothers had at least one radiography exam, 0.4% had at least one fluoroscopy exam, 0.04% had at least one angiography exam, and 0.2% had at least one nuclear medicine exam (Table 4). In the childhood-exposure cohort, 61.1% had at least one radiography exam, 6.0% had at least one fluoroscopy exam, 0.4% had at least one angiography exam, and 1.5% had at least one nuclear medicine exam (Table 4).
Results for the six individual U.S. sites can be found in Supplemental Tables 3–6.
Discussion
Diagnostic imaging is an important medical advancement that contributes to accurate disease diagnosis and improved treatment. However, potential harmful health effects of medical imaging must also be understood so they can be weighed against diagnostic benefit. We have previously reported that rates of imaging with ionizing radiation remains high in pregnant women and children [2, 11]. While awareness exists in the U.S. and Canada that medical imaging must be justified and imaging exams in children should be reduced, our previous studies suggest that rates of imaging in children continues to be elevated compared to earlier periods, and use of relatively high-dose exams such as CT continues [1, 2, 41]. The risk of cancer from exposure to routine medical imaging is not fully understood. The RIC Study is using extensive data resources spanning 1995–2017 on exposure to medical imaging in the U.S. and Ontario, Canada, complete capture of member health care utilization, follow-up for cancer diagnosis of members who disenrolled from the U.S. health systems, and detailed demographic and cancer diagnosis information to examine these critical clinical care and public health issues in a vulnerable population. No such study has been conducted in North America to date.
Significance of the RIC Study
Ionizing radiation is one of the most comprehensively studied carcinogens with extensive evidence linking it to cancer risk. However, many past studies have focused on specific human populations, such as Japanese atomic bomb survivors [42], those exposed to radon and environmental accidents [43], and patients receiving cancer radiation treatment [44, 45]. These specialized populations differ from the general North American population undergoing routine medical imaging.
Several large retrospective studies on medical radiation exposure from CT imaging and childhood and adolescent cancer risk have been conducted. The UK-NCI Study, Dutch Pediatric CT Study, and Australia study reported increased risks of brain cancer [10] or both brain cancer and leukemia [4, 9] with CT exposure. Two studies in South Korea [8] and Taiwan [46] reported elevated risks of myeloid leukemias, myelodysplasia, breast cancer, and thyroid cancer (South Korea), and benign brain tumors (Taiwan). The EPI-CT consortium is a retrospective cohort from 1977 to 2015 of 948,174 children and young adults who had underwent a CT exam at least once before the age of 22 years with no prior history of cancer and includes patients from nine countries including the UK-NCI Study and Dutch Pediatric CT Study [47]. When comparing characteristics of our RIC childhood-exposure cohort to the EPI-CT consortium, among 948,174 children who had at least one CT exam in EPI-CT, 714,860 (75.4%) had only one exam in EPI-CT vs. 220,436 (77.7%) in RIC, yet children tended to be younger at the time of imaging in RIC (63.4% age 0–9 years) vs. EPI-CT (46.5% age 0–9 years). For both cohorts, the most common scanned anatomical region was head and/or neck (70.9% RIC vs. 65.9% EPI-CT). Direct comparison of childhood cancer incidence between the two cohorts will be interesting once the EPI-CT results are published.
A key limitation to most of these previous studies is radiation dose exposures were based on estimates such as the number of CT scans [8, 46, 48], using average organ dose libraries [4, 9], and protocol-based (e.g., hospital average) doses [49]. In contrast, a significant strength of our forthcoming RIC Study is the collection of individual radiation technique parameters from CT exams, enabling the calculation of individual patient-specific organ doses using modern dose estimation methods. We will also be able to compare previous methods of dose estimation to more precise methods, to help assess the potential for bias in previous reports.
Strengths and limitations of the RIC Study
Our study is one of the largest and most contemporary to examine risk of childhood cancers associated with medical radiation from in utero and childhood exposure over a 22-year span comparing an exposed group to an unexposed group. To ensure the most complete capture of medical imaging exposure possible, the fetal-exposure cohort required pregnant women to be health plan members during their entire pregnancy, and the childhood-exposure cohort required children to be born into the health plan with censoring after disenrollment. CT imaging parameters were collected for a large proportion of exams and will be used to calculate patient-specific absorbed radiation organ doses for those exams. We were unable to collect CT parameters for all exams, especially in Ontario in which data on a sample of 2,300 exams were obtained to represent over 300,000 exams. However, we will use patient-specific absorbed doses to estimate doses for other exams based on several covariates including exam year. Unlike prior studies, our study will include a comprehensive assessment of all imaging modalities that use ionizing radiation, with data obtained from health plan electronic data sources; however, mean doses are being applied for all modalities aside from CT. Finally, we acknowledge that examining the association of medical radiation exposure with risk of solid cancers in the U.S. sites is a limitation given a large proportion of children left the U.S. health plans at a median age of five years.
One major criticism for these types of studies has been the potential for confounding by indication [50, 51]. While we were unable to collect clinical indication for all exams, we were able to obtain this information for a proportion of the exams to assess confounding by indication. In preliminary analyses, the most common indications appear to be related to craniosynostosis and trauma.
Our study provides a unique representation of the U.S. population insured by similar integrated health care systems, and a complete, population-based view of all residents of Ontario, Canada. Imaging exams performed external to the U.S. health systems could potentially introduce measurement error; however, outside claims for imaging services are routinely included in each U.S. health plan’s EHR and are thus trackable as part of the patient’s clinical care. In Ontario, given that health care is organized as a single-payer system, exams outside the system would be exceedingly rare. Finally, we did not have individual-level income data and relied on census-based measures.
Future plans of the RIC Study
The primary RIC Study analyses on the association between radiation dose and risk of childhood cancers are forthcoming. Looking toward the future, we have established a rich resource of medical imaging data, radiation dose assessment methods, key covariates, childhood and adolescent cancer outcomes, and large patient cohorts on which to build ancillary research projects at relatively modest cost. Finally, our study is poised to bring further awareness surrounding the topic of medical imaging, its potential overuse or misuse, and its effects on population health.
Data availability
The data that support the findings of this study are not openly available due to institutional data sharing policies and are available from the corresponding author upon reasonable request as well as appropriate institutional review board approvals and data sharing agreements.
Code availability
Not applicable.
References
Smith-Bindman R et al (2012) Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996–2010. JAMA 307(22):2400–2409
Smith-Bindman R et al (2019) Trends in use of medical imaging in US health care systems and in Ontario, Canada, 2000–2016. JAMA 322(9):843–856
BEIR VII (2006) Health risks from exposure to low levels of ionizing radiation, in Committee to Assess Health Effects from Exposure to Low Levels of Ionizing Radiation. National Research Council, Washington, DC
Pearce MS et al (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380(9840):499–505
Preston DL et al (2008) Solid cancer incidence in atomic bomb survivors exposed in utero or as young children. J Natl Cancer Inst 100(6):428–436
Siegel RL et al (2021) Cancer Statistics, 2021. CA Cancer J Clin 71(1):7–33
https://www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
Hong JY et al (2019) Association of exposure to diagnostic low-dose ionizing radiation with risk of cancer among youths in South Korea. JAMA Netw Open 2(9):e1910584
Mathews JD et al (2013) Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 346:f2360
Meulepas JM et al (2018) Radiation exposure from pediatric CT scans and subsequent cancer risk in the Netherlands. J Natl Cancer Inst 111:256–263
Kwan ML et al (2019) Trends in medical imaging during pregnancy in the United States and Ontario, Canada, 1996 to 2016. JAMA Netw Open 2(7):e197249
Ross TR et al (2014) The HMO research network virtual data warehouse: a public data model to support collaboration. EGEMS (Wash DC) 2(1):1049
Hornbrook MC et al (2005) Building a virtual cancer research organization. J Natl Cancer Inst Monogr 35:12–25
https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm
https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas-who.htm
Fenton TR, Kim JH (2013) A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr 13:59
Chen K, Zhang X, Petersen A, Muller H-G (2017) Quantifying infinite-dimensional data: functional data analysis in action. Stat Biosci 9:582–604
Geyer AM et al (2014) The UF/NCI family of hybrid computational phantoms representing the current US population of male and female children, adolescents, and adults–application to CT dosimetry. Phys Med Biol 59(18):5225–5242
Maynard MR et al (2011) The UF family of hybrid phantoms of the developing human fetus for computational radiation dosimetry. Phys Med Biol 56(15):4839–4879
Maynard MR et al (2014) The UF Family of hybrid phantoms of the pregnant female for computational radiation dosimetry. Phys Med Biol 59(15):4325–4343
Stepusin EJ et al (2017) Physical validation of a Monte Carlo-based, phantom-derived approach to computed tomography organ dosimetry under tube current modulation. Med Phys 44(10):5423–5432
Stepusin EJ et al (2017) Assessment of different patient-to-phantom matching criteria applied in Monte Carlo-based computed tomography dosimetry. Med Phys 44(10):5498–5508
Marshall EL et al (2019) A scalable database of organ doses for common diagnostic fluoroscopy procedures of children: procedures of historical practice for use in radiation epidemiology studies. Radiat Res 192(6):649–661
McCollough CH et al (2007) Radiation exposure and pregnancy: when should we be concerned? Radiographics 27(4):909–917
https://www.unscear.org/docs/publications/2000/UNSCEAR_2000_Annex-D.pdf
Niwa O et al (2015) ICRP publication 131: stem cell biology with respect to carcinogenesis aspects of radiological protection. Ann ICRP 44(3–4):7–357
Stabin MG (2018) New-generation fetal dose estimates for radiopharmaceuticals. J Nucl Med 59(6):1005–1006
https://seer.cancer.gov/siterecode/icdo3_dwhoheme/index.html
Steliarova-Foucher E et al (2005) International classification of childhood cancer, third edition. Cancer 103(7):1457–1467
Hasle H, Clemmensen IH, Mikkelsen M (2000) Risks of leukaemia and solid tumours in individuals with Down’s syndrome. Lancet 355(9199):165–169
Marlow EC et al (2021) Leukemia risk in a cohort of 3.9 million children with and without Down syndrome. J Pediatr 234:172
Buffler PA et al (2005) Environmental and genetic risk factors for childhood leukemia: appraising the evidence. Cancer Invest 23(1):60–75
Poole C et al (2006) Socioeconomic status and childhood leukaemia: a review. Int J Epidemiol 35(2):370–384
Chow EJ et al (2010) Childhood cancer in relation to parental race and ethnicity: a 5-state pooled analysis. Cancer 116(12):3045–3053
Lim JY et al (2014) Genomics of racial and ethnic disparities in childhood acute lymphoblastic leukemia. Cancer 120(7):955–962
Linabery AM, Ross JA (2008) Trends in childhood cancer incidence in the U.S. (1992–2004). Cancer 112(2):416–432
Messer LC et al (2006) The development of a standardized neighborhood deprivation index. J Urban Health 83(6):1041–1062
Gooley TA et al (1999) Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 18(6):695–706
Miglioretti DL et al (2013) The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr 167(8):700–707
Grant EJ et al (2017) Solid Cancer Incidence among the Life Span Study of Atomic Bomb Survivors: 1958–2009. Radiat Res 187(5):513–537
Moysich KB, Menezes RJ, Michalek AM (2002) Chernobyl-related ionising radiation exposure and cancer risk: an epidemiological review. Lancet Oncol 3(5):269–279
Hauptmann M et al (2016) Increased pancreatic cancer risk following radiotherapy for testicular cancer. Br J Cancer 115(7):901–908
Levi F et al (2006) Cancer risk after radiotherapy for breast cancer. Br J Cancer 95(3):390–392
Huang WY et al (2014) Paediatric head CT scan and subsequent risk of malignancy and benign brain tumour: a nation-wide population-based cohort study. Br J Cancer 110(9):2354–2360
Bernier MO et al (2018) Cohort Profile: the EPI-CT study: a European pooled epidemiological study to quantify the risk of radiation-induced cancer from paediatric CT. Int J Epidemiol 48:379
Krille L et al (2015) Risk of cancer incidence before the age of 15 years after exposure to ionising radiation from computed tomography: results from a German cohort study. Radiat Environ Biophys 54(1):1–12
Journy N et al (2015) Are the studies on cancer risk from CT scans biased by indication? Elements of answer from a large-scale cohort study in France. Br J Cancer 112(1):185–193
Boice JD Jr (2015) Radiation epidemiology and recent paediatric computed tomography studies. Ann ICRP 44(1 Suppl):236–248
Walsh L et al (2014) Risks from CT scans–what do recent studies tell us? J Radiol Prot 34(1):E1-5
Acknowledgments
We thank Dr. Jonathan Ducore, MD, MPH and Dr. Stacy Month, MD for their pediatric oncology consultation in reviewing our classification of childhood cancers. We also thank our study staff who performed film CT abstraction and database programming support: Zobeyda Otero, Aleyda Solorzano Pinto, Kiara Bell, Andrea Volz, Mary Lyons, Donna Gleason, Arthur Truong, Ali Moin, Mohammed Mamun, Diane Kohnhorst, and Deborah Seger.
Funding
This study was supported by the National Cancer Institute at the National Institutes of Health (R01CA185687 and R50CA211115). The Ontario, Canada portion of the study was also supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). The analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
Author information
Authors and Affiliations
Contributions
All authors whose names appear on the submission: (1) made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; (2) drafted the work or revised it critically for important intellectual content; (3) approved the version to be published; and (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was approved by institutional review boards at each participating study site. Given this is a minimal risk, medical record review study, participant informed consent was waived.
Consent to participate
This study was approved by institutional review boards at each participating study site. Given this is a minimal risk, medical record review study, participant informed consent was waived.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kwan, M.L., Miglioretti, D.L., Bowles, E.J.A. et al. Quantifying cancer risk from exposures to medical imaging in the Risk of Pediatric and Adolescent Cancer Associated with Medical Imaging (RIC) Study: research methods and cohort profile. Cancer Causes Control 33, 711–726 (2022). https://doi.org/10.1007/s10552-022-01556-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-022-01556-z