Abstract
Purpose
Studies have shown consistent associations between youth e-cigarette use and subsequent smoking uptake. However, it remains unclear why, as limited evidence exists regarding the mechanisms underlying these associations. Our study investigated whether having one or more smoking friends mediated the association between e-cigarette use and cigarette smoking onset among a longitudinal sample of Canadian youth who were never smokers at baseline.
Methods
A longitudinal sample of youth that participated in three waves of the COMPASS study (2015–2016 to 2017–2018) was identified (N = 5,535). The product of coefficients method was used to assess whether having one or more smoking friends mediated the association between: (1) past 30-day e-cigarette use and cigarette smoking onset and (2) past 30-day e-cigarette use and subsequent dual use of e-cigarettes and cigarettes.
Results
Having one or more smoking friends did not mediate the association between (1) past 30-day e-cigarette use and cigarette smoking onset (β = 0.38, 95% CI − 0.12, 0.89) or (2) past 30-day e-cigarette use and subsequent dual use (β = 0.46, 95% CI − 0.16, 1.07). Post hoc tests indicated that smoking friends significantly predicted past 30-day e-cigarette use and cigarette smoking at wave 3 (aOR 1.68 and 2.29, respectively).
Conclusion
Having smoking friends did not explain the association between e-cigarette use and smoking uptake despite being a common risk factor for both e-cigarette use and cigarette smoking. Prevention efforts should consider how best to incorporate effective programming to address these social influences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
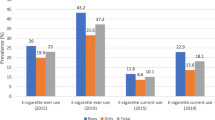
Tobacco smoking is a major preventable cause of many chronic conditions, including several types of cancer, cardiovascular disease, and respiratory illnesses [1]. Despite steady declines in cigarette smoking observed in Canada, the tobacco and nicotine product market has been evolving, with an increase in the number and use of alternative products [2]. Specifically, the emergence of electronic cigarettes (e-cigarettes) has proliferated among youth, internationally and within Canada [3,4,5,6]. National data indicate that among Canadian students in grades 10 to 12, e-cigarette use in the past 30 days has doubled from 14.6% in 2017 to 29.4% in 2019 [2, 7]. The use of e-cigarettes among youth has raised concerns regarding the potential public health implications of this behavior.
Our previous work has demonstrated an association between e-cigarette use and cigarette smoking uptake among Canadian youth [8, 9]. Using longitudinal data from the COMPASS study, our first study found that non-smoking youth who used e-cigarettes in the past 30 days were twice as likely to report trying cigarettes one year later [8]. Our second study showed similar findings: among a sample of youth never smokers, e-cigarette users were at a greater risk of smoking uptake after a two-year follow-up [9]. This association was also observed among low-risk youth who were not susceptible to smoking in the future [10]. Overall, these studies contribute to a growing evidence base showing a consistent association between youth e-cigarette use and smoking uptake [8,9,10,11,12,13,14,15,16,17].
Currently, it remains unclear why youth e-cigarette use is associated with smoking uptake, as there is limited evidence on possible mechanisms underlying this association. To date, only two studies have investigated possible mediating factors between e-cigarette use and smoking uptake [13, 18]. The first study conducted among a sample of 1,152 English youth found that escalation of e-cigarette use did not explain the association between e-cigarette use and subsequent smoking behaviors [13]. The second study conducted among 2,238 students in Hawaii found that the association between e-cigarette use and smoking onset was partly attributable to changes in smoking-related expectancies and affiliations with smoking friends [18].
There are several possible explanations for the associations between youth e-cigarette use and subsequent smoking uptake. Some have argued that exposure to nicotine via e-cigarettes may result in nicotine dependence and an increased liability to use other nicotine products [19, 20]. In contrast, the Common Liability Theory argues that associations between e-cigarette use and smoking may be a result of unmeasured common risk factors (e.g., risk-taking tendencies) that increase an individual’s likelihood of using both e-cigarettes and smoking [21].
Other theories have drawn attention to the role of social contexts (e.g., peer circles) in influencing e-cigarette use and smoking behaviors [22]. Having friends who smoke has been shown to be a strong predictor of smoking uptake [23, 24]. Furthermore, a large proportion of youth who use e-cigarettes also smoke cigarettes, and e-cigarette users tend to have friends that also use e-cigarettes [3, 25]. It may be that non-smoking youth who use e-cigarettes are more likely to have smoking friends. E-cigarette users with smoking friends may be a greater risk of taking up smoking due to increased contact and exposure to smokers who model smoking behaviors and provide access to cigarettes [22, 26, 27].
Building off our initial work that demonstrated an association between initial e-cigarette use and smoking uptake among a sample of Canadian youth [8, 9], this follow-up aimed to investigate potential mediating factors linking these two behaviors. Thus, using three waves of longitudinal data from a sample of Canadian youth never smokers, we examined whether having smoking friends mediated the association between (1) past 30-day e-cigarette use and cigarette smoking onset and (2) past 30-day e-cigarette use and subsequent dual use (e-cigarette use and cigarette smoking). We hypothesized that the association between (1) past 30-day e-cigarette use and cigarette smoking onset and (2) past 30-day e-cigarette use and subsequent dual use would be mediated by having friends who smoke.
Methods
Design
COMPASS is a prospective cohort study designed to follow a sample of grade 9–12 students attending Canadian secondary schools, aged approximately 13–18 years old [28]. Specifically, COMPASS collects data on how changes in the school environment (policies, programs, built environment) influence student health behaviors [28]. Data regarding student health behaviors are gathered during class-time using the COMPASS questionnaire [28]. The questionnaire was created to gather data from students relating to demographics and various health behaviors, including tobacco and e-cigarette use [28]. Additional details on COMPASS methodology can be found here [28] (www.compass.uwaterloo.ca).
Study sample
This study used data from Ontario and Alberta schools in Year 4 (2015–2016), Year 5 (2016–2017), and Year 6 (2017–2018) of COMPASS. Year 4 will be referred to as ‘wave 1,’ Year 5 as ‘wave 2,’ and Year 6 as ‘wave 3.’ The sample consisted of students attending schools in Ontario and Alberta who participated in waves 1 to 3. Details regarding the procedures used to form the longitudinal sample can be found elsewhere [29]. Students who reported ever having smoked a cigarette at wave 1 were excluded from the sample (n = 655), resulting a final longitudinal sample of 5,535 students who were never smokers at wave 1.
With respect to missing data, non-response rates for outcome measures including past 30-day cigarette smoking and dual use were low: 0.5% and 0.9%, respectively. Similarly, non-response rates for baseline demographic and behavioral covariates were also quite low (< 1%).
Measures
Past 30-day e-cigarette use
“On how many of the last 30 days did you use an e-cigarette?” Students who reported using e-cigarettes within the past month were classified as past 30-day e-cigarette users; otherwise, they were categorized as non-past 30-day users.
Past 30-day cigarette smoking
“On how many of the last 30 days did you smoke one or more cigarettes?” Students who reported smoking cigarettes within the past month were classified as past 30-day smokers; otherwise, they were categorized as non-past 30-day smokers.
Past 30-day dual use
A derived variable for dual use was created based on measures of past 30-day e-cigarette use and cigarette smoking. Students who reported smoking cigarettes and using e-cigarettes were classified as past 30-day dual users; otherwise, they were classified as ‘other.’
Smoking friends
“Your closest friends are the friends you like to spend the most time with. How many of your closest friends smoke cigarettes?”, with response options ranging from ‘None’ to ‘5 or more friends’. Response options were dichotomized as: ‘having at least one friend’ versus ‘none’, given the low proportion of students who reported having more than one close friend who smoked.
Demographic covariates
Gender (male, female), grade (9, 10, 11, 12), ethnicity (White, Black, Asian, Latin American, Other) and weekly spending money ($0, $1–20, $20–100, over $100, I don’t know), and province (Ontario, Alberta).
Behavioral covariates
Students were asked how often they used cannabis in the past year. Those who had used cannabis within the past month were classified as past 30-day cannabis users; otherwise, they were classified as non-past 30-day cannabis users. Students were also asked how often they had 5 or more drinks of alcohol on one occasion in the past year. Those who had had 5 or more drinks of alcohol on one occasion in the past month were classified as past 30-day binge drinkers; otherwise, they were classified as non-past 30-day binge drinkers.
Analysis
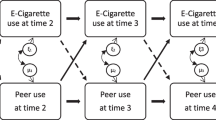
Descriptive statistics were used to examine the sociodemographic and behavioral characteristics of the sample at wave 1. To address our main research objectives, a series of multi-level logistic regression models were used to examine whether having smoking friends at wave 2 mediates the association between: (a) past 30-day e-cigarette use at wave 1 and past 30-day cigarette smoking at wave 3 and; (b) past 30-day e-cigarette use at wave 1 and past 30-day dual use at wave 3 (Refer to Fig. 1a, b). Specifically, the products of coefficient method were used to estimate the potential mediating effect of smoking friends [30]. This approach is based on the rationale that mediation depends on the extent to which e-cigarette use leads to having smoking friends, \(\widehat{{\varvec{a}}}\), and the extent to which having smoking friends leads to cigarette smoking, \(\widehat{{\varvec{b}}}\). The products of coefficients approach involves estimating the product of \(\widehat{{\varvec{a}}}\) and \(\widehat{{\varvec{b}}}\), \(\widehat{{\varvec{a}}}\widehat{{\varvec{b}}}\), to form the mediated effect [30]. To estimate the standard error of the mediated effect, the Sobel test was used [31]. In order to evaluate the statistical significance of the mediated effect, the estimate of the mediated effect was divided by the standard error of the mediated effect; this value was then compared with the normal distribution [30]. All mediation models adjusted for demographic and behavioral covariates are described above. Students with missing data for the outcome or any covariates were excluded from regression models using listwise deletion.
Given the absence of significant mediating effects (described below), post hoc analyses were also conducted to test whether having smoking friends was a confounding variable in the association between e-cigarette use and subsequent smoking uptake. Specifically, the Change-in-Estimate criterion was used to statistically test the potential confounding influence of smoking friends [32]. Using the CIE criterion, a change of ≥ 10% in the effect of e-cigarette use on smoking onset between unadjusted regression models and regression models adjusted for having smoking friends was used as a cut-off for identifying whether smoking friends was a confounding variable [32]. We also examined whether having smoking friends met the two criteria to qualify as a confounding variable: (1) it is associated with the exposure (i.e., past 30-day e-cigarette use) and (2) it is a predictor of the outcome of interest (i.e., past 30-day cigarette smoking/dual use). All analyses were conducted using SAS 9.4.
Results
Table 1 reports the demographic and behavioral characteristics of the sample of never smokers at wave 1. Within our study sample, 53.4% of students were females and 73% were identified as White. 95.1% of students within the sample were from Ontario and 27.1% reported having at least twenty dollars in weekly spending money.
As shown in Table 2, the direct effect of being a past 30-day e-cigarette user at wave 1 significantly predicted past 30-day cigarette smoking and dual use at wave 3 (p < 0.05 for both). However, the effect of past 30-day e-cigarette use on subsequent past 30-day cigarette smoking was not mediated by having friends who smoke at wave 2 (β = 0.38, 95% CI − 0.12, 0.89, z = 1.48. Similarly, the effect of past 30-day e-cigarette use on subsequent dual use was not mediated by having friends who smoke at wave 2 (β = 0.46, 95% CI − 0.16, 1.07, z = 1.45).
Post hoc tests that were conducted to investigate the role of smoking friends in the association between e-cigarette use and subsequent smoking showed that having friends who smoke was a confounding factor: a change of ≥ 10% was observed in parameter estimates between unadjusted models and models adjusting for having friends who smoke (Table 3). These findings were reinforced by post hoc tests showing that having friends who smoke at wave 1 was significantly associated with past 30-day e-cigarette use (i.e., exposure of interest) and predictive of past 30-day cigarette smoking (i.e., outcome of interest; Supplementary Table S1).
Discussion
This is the first study to investigate what role having one or more smoking friends has on the association between e-cigarette use and subsequent cigarette smoking onset using three waves of data from a large, longitudinal sample of youth. Our findings showed that past 30-day e-cigarette use was significantly associated with cigarette smoking onset. However, contrary to our initial hypotheses, having one or more smoking friends did not mediate the association between past 30-day e-cigarette use and cigarette smoking onset. Rather, the study findings indicated that having one or more friends who smoked was a significant predictor of both past 30-day e-cigarette use and past 30-day cigarette smoking. Overall, these findings suggest that having smoking friends represents a confounding factor in the e-cigarette use-cigarette smoking pathway.
The associations observed between past 30-day e-cigarette use and subsequent smoking onset in our study are consistent with recent systematic reviews and meta-analyses [17, 33]. Our findings regarding the role of smoking friends in the e-cigarette use-smoking pathway are inconsistent with earlier evidence [18], but align with more recent work [34]. Overall, our findings are in line with the Common Liability Theory that argues that there are common underlying risk factors (e.g., shared social or environmental factors) that increase an individual’s propensity to use nicotine [21]; having one or more close friends who smoke appears to represent a common risk factor that is associated with using both e-cigarettes and cigarettes according to our findings. It is possible that having smoking friends may provide a shared access point for both products (i.e., e-cigarettes and cigarettes); in this way, the presence of smoking friends may offer increased opportunities for youth to use both products.
The study findings did not support the role of smoking friends as a mediating factor in the association between past 30-day e-cigarette use and subsequent past 30-day dual use. However, a significant association between having one or more close friends who smoke and subsequent past 30-day dual use was observed among never smokers. This is noteworthy as it may be the case that having at least one close friend who smokes represents a proxy/marker for which youth will eventually go on to engage in multiple risky behaviors. The clustering of risky behaviors has been widely documented in various youth-based studies [5, 35,36,37].
Implications for programming and research
Our findings indicate that having one or more close friends who smoke represents a key social factor that is linked to both past 30-day e-cigarette use and past 30-day cigarette smoking. Our findings suggest the need to consider the role of social influences within the design of future interventions focused on preventing youth uptake of e-cigarettes and cigarettes. Prevention programs combining social competence (i.e., teaching problem-solving and cognitive skills to resist personal and media influences) and social influence curricula (i.e., teaching skills to resist offers of tobacco/deal with peer pressure) have been shown to be effective in preventing youth smoking uptake [38]. Involvement of influential student leaders within the design of prevention initiatives has also been shown to be a key component of effective tobacco programming [39, 40]. Specifically, previous evaluations have shown that student-led interventions aimed at de-normalizing smoking behaviors can be effective in reducing smoking uptake [39, 40]. Future prevention efforts should consider how best to incorporate key components of evidence-based tobacco programming noted above. Given the currently limited evidence base to inform the design of e-cigarette prevention programs, future work would also benefit from identifying key components of effective e-cigarette programming moving forward.
Study strengths and limitations
The strengths of our study include the use of a large, three-year longitudinal sample of youth from two Canadian provinces: Ontario and Alberta. Furthermore, our study makes use of an under-utilized analytic approach within applied health research to investigate mediating factors that may explain the association between youth e-cigarette use and smoking uptake. Our study also had some limitations. First, we did not have measures to assess whether students were using nicotine or non-nicotine containing e-cigarettes. As such, we could not examine whether there were potential differences in these associations among subgroups of e-cigarette users. We also did not have access to other social norm measures that may have played a role in the e-cigarette use-cigarette smoking pathway (e.g., having friends who use e-cigarettes, having a sibling/family member who uses e-cigarettes/smokes). Lastly, the study relied on non-probability sampling methods; as such, the results may not be representative of all Ontario and Alberta secondary schools.
Conclusions
Our findings indicate that having one or more smoking friends does not explain the association between past 30-day e-cigarette use and cigarette smoking onset. Rather, it represents a common risk factor that is linked to past 30-day use of both products. These findings suggest the need to consider the role of social influences within the design of future prevention intervention efforts.
Availability of data and materials
Data from the COMPASS study is not publicly available. Researchers interested in gaining access to COMPASS data must complete the COMPASS data usage application form (https://uwaterloo.ca/compass-system/information-researchers).
References
U.S. Department of Health and Human Service (2014) The health consequences of smoking—50 years of progress: a report of the surgeon general. Smoking Health. https://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf
Reid J, Hammond D, Tariq U, Burkhalter R, Rynard V, Douglas O (2019) Tobacco use in Canada : patterns and trends, 2019 Edition. Can Cancer Soc. https://www.tobaccoreport.ca/2013/TobaccoUseinCanada_2013.df
Montreuil A, MacDonald M, Asbridge M, Wild TC, Hammond D, Manske S et al (2017) Prevalence and correlates of electronic cigarette use among Canadian students: cross-sectional findings from the 2014/15 Canadian Student Tobacco, Alcohol and Drugs Survey. CMAJ Open 5(2):E460–E467. https://doi.org/10.9778/cmajo.20160167
Hammond D, Reid JL, Rynard VL, Fong GT, Cummings KM, McNeill A et al (2019) Prevalence of vaping and smoking among adolescents in Canada, England, and the United States: repeat national cross sectional surveys. BMJ. https://doi.org/10.1136/bmj.l2219
Zuckermann AME, Williams G, Battista K, de Groh M, Jiang Y, Leatherdale ST (2019) Trends of poly-substance use among Canadian youth. Addict Behav Rep 10:100189. https://doi.org/10.1016/j.abrep.2019.100189
Arrazola RA, Singh T, Corey CG, Husten CG, Neff LJ, Apelberg BJ et al (2015) Tobacco use among middle and high school students: United States, 2011–2014. MMWR Morb Mortal Wkly Rep 64(14):381–385
Health Canada (2019) Summary of results for the Canadian Student Tobacco, Alcohol and Drugs Survey 2018–2019. https://www.canada.ca/en/health-canada/services/canadian-student-tobacco-alcohol-drugs-survey/2018-2019-summary.html
Hammond D, Reid JL, Cole AG, Leatherdale ST (2017) Electronic cigarette use and smoking initiation among youth: a longitudinal cohort study. Can Med Assoc J 189(43):E1328–E1336. https://doi.org/10.1503/cmaj.161002
Aleyan S, Cole A, Qian W, Leatherdale ST (2018) Risky business: a longitudinal study examining cigarette smoking initiation among susceptible and non-susceptible e-cigarette users in Canada. BMJ Open. https://doi.org/10.1136/bmjopen-2017-021080)
Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD (2015) Progression to traditional cigarette smoking after electronic cigarette use among us adolescents and young adults. JAMA Pediatr 169(11):1018–1023
Barrington-Trimis JL, Urman R, Berhane K, Unger JB, Cruz TB, Pentz MA et al (2016) E-cigarettes and future cigarette use. Pediatrics 138(1):e20160379–e20160379. https://doi.org/10.1542/peds.2016-0379
Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR et al (2015) Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA 314(7):700–707
East K, Hitchman SC, Bakolis I, Williams S, Cheeseman H, Arnott D et al (2018) The association between smoking and electronic cigarette use in a cohort of young people. J Adolesc Heal 62(5):539–547. https://doi.org/10.1016/j.jadohealth.2017.11.301
Barrington-Trimis JL, Kong G, Leventhal AM, Liu F, Mayer M, Cruz TB et al (2018) E-cigarette use and subsequent smoking frequency among adolescents. Pediatrics 142(6):e20180486. https://doi.org/10.1542/peds.2018-0486
Best C, Haseen F, Currie D, Ozakinci G, MacKintosh AM, Stead M et al (2017) Relationship between trying an electronic cigarette and subsequent cigarette experimentation in Scottish adolescents: a cohort study. Tob Control 27:373–378
Conner M, Grogan S, Simms-Ellis R, Flett K, Sykes-Muskett B, Cowap L et al (2017) Do electronic cigarettes increase cigarette smoking in UK adolescents? Evidence from a 12-month prospective study. Tob Control 27:365–273
Khouja JN, Suddell SF, Peters SE, Taylor AE, Munafò MR (2020) Is e-cigarette use in non-smoking young adults associated with later smoking? A systematic review and meta-analysis. Tob Control. https://tobaccocontrol.bmj.com/content/early/2020/03/01/tobaccocontrol-2019-055433.abstract
Wills TA, Gibbons FX, Sargent JD, Schweitzer RJ (2016) How is the effect of adolescent e-cigarette use on smoking onset mediated: A longitudinal analysis. Psychol Addict Behav 30(8):876–886. https://doi.org/10.1037/adb0000213
Yuan M, Cross SJ, Loughlin SE, Leslie FM (2015) Nicotine and the adolescent brain. J Physiol 593(16):3397–3412
Counotte DS, Smit AB, Pattij T, Spijker S (2011) Development of the motivational system during adolescence, and its sensitivity to disruption by nicotine. Dev Cogn Neurosci 1(4):430–443
Vanyukov MM, Tarter RE, Kirillova GP, Kirisci L, Reynolds MD, Kreek MJ et al (2012) Common liability to addiction and “gateway hypothesis”: theoretical, empirical and evolutionary perspective. Drug Alcohol Depend 123(Suppl 1):S3–S17. https://doi.org/10.1016/j.drugalcdep.2011.12.018
Bandura A (1987) Social foundations of thought and action: a social-cognitive view. Acad Manag Rev
Liu J, Zhao S, Chen X, Falk E, Albarracín D (2017) The influence of peer behavior as a function of social and cultural closeness: a meta-analysis of normative influence on adolescent smoking initiation and continuation. Psychol Bull 143(10):1082–1115. https://doi.org/10.1037/bul0000113
Wellman RJ, Dugas EN, Dutczak H, O’Loughlin EK, Datta GD, Lauzon B et al (2016) Predictors of the onset of cigarette smoking: a systematic review of longitudinal population-based studies in youth. Am J Prev Med 51(5):767–778. https://doi.org/10.1016/j.amepre.2016.04.003
Azagba S, Kah K, Latham K (2019) Frequency of E-cigarette use and cigarette smoking among Canadian students. Prev Med. https://doi.org/10.1016/j.ypmed.2019.105769
Kong G, Morean ME, Cavallo DA, Camenga DR, Krishnan-Sarin S (2017) Sources of electronic cigarette acquisition among adolescents in Connecticut. Tob Regul Sci 3(1):10–16
Sussman S, Pokhrel P, Ashmore RD, Brown BB (2007) Adolescent peer group identification and characteristics: a review of the literature. Addict Behav 32(8):1602–1627
Leatherdale ST, Brown KS, Carson V, Childs RA, Dubin JA, Elliott SJ et al (2014) The COMPASS study: A longitudinal hierarchical research platform for evaluating natural experiments related to changes in school-level programs, policies and built environment resources. BMC Public Health 14(1):1–7
Qian W, Battista K, Bredin C, Brown KS, Leatherdale ST (2015) Assessing longitudinal data linkage results in the COMPASS study. Compass Tech Rep Ser. https://uwaterloo.ca/compass-system/publications#technical
MacKinnon DP (2008) Introduction to statistical mediation analysis. APA Handb Res methods Psychol Vol 2 Res Des Quant Qual Neuropsychol Biol
Sobel ME (1982) Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol 13:290–312
Greenland S, Pearce N (2015) Statistical Foundations for Model-Based Adjustments. Annu Rev Public Health 36:89–108. https://doi.org/10.1146/annurev-publhealth-031914-122559
Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA et al (2017) Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults a systematic review and meta-analysis. JAMA Pediatr 171:788–797
Conner M, Grogan S, Simms-Ellis R, Scholtens K, Sykes-Muskett B, Cowap L et al (2019) Patterns and predictors of e-cigarette, cigarette and dual use uptake in UK adolescents: evidence from a 24-month prospective study. Addiction 114(11):2048–2055. https://doi.org/10.1111/add.14723
Azagba S (2018) E-cigarette use, dual use of e-cigarettes and tobacco cigarettes, and frequency of cannabis use among high school students. Addict Behav 79:166–170
Milicic S, Leatherdale ST (2017) The associations between E-cigarettes and binge drinking, marijuana use, and energy drinks mixed with alcohol. J Adolesc Heal 60(3):320–327. https://doi.org/10.1016/j.jadohealth.2016.10.011
Mehra VM, Keethakumar A, Bohr YM, Abdullah P, Tamim H (2019) The association between alcohol, marijuana, illegal drug use and current use of E-cigarette among youth and young adults in Canada: results from Canadian Tobacco, Alcohol and Drugs Survey 2017. BMC Public Health 19:108
Thomas RE, McLellan J, Perera R (2015) Effectiveness of school-based smoking prevention curricula: Systematic review and meta-analysis. BMJ Open 5(3):e006976
Macarthur GJ, Sean H, Deborah MC, Matthew H, Rona C (2016) Peer-led interventions to prevent tobacco, alcohol and/or drug use among young people aged 11–21 years: a systematic review and meta-analysis. Addiction 111(3):391–407. https://doi.org/10.1111/add.13224
Campbell R, Starkey F, Holliday J, Audrey S, Bloor M, Parry-Langdon N et al (2008) An informal school-based peer-led intervention for smoking prevention in adolescence (ASSIST): a cluster randomised trial. Lancet 371(9624):1595–1602
Funding
The COMPASS study has been supported by a bridge grant from the CIHR Institute of Nutrition, Metabolism and Diabetes (INMD) through the “Obesity – Interventions to Prevent or Treat” priority funding awards (OOP-110788; awarded to SL), an operating grant from the CIHR Institute of Population and Public Health (IPPH) (MOP-114875; awarded to SL), a CIHR project grant (PJT-148562; awarded to SL), a CIHR bridge Grant (PJT-149092; awarded to KP/SL), a CIHR project Grant (PJT-159693; awarded to KP), and by a research funding arrangement with Health Canada (#1617-HQ-000012; contract awarded to SL). The COMPASS-Quebec project additionally benefits from funding from the Ministère de la Santé et des Services sociaux of the province of Québec, and the Direction régionale de santé publique du CIUSSS de la Capitale-Nationale. Dr. Leatherdale is a Chair in Applied Public Health funded by the Public Health Agency of Canada (PHAC) in partnership with the Canadian Institute of Health Research (CIHR). Dr. Ferro holds the Canada Research Chair in Youth Mental Health and is supported by an Early Researcher Award from the Ministry of Research, Innovation, and Science. The funding sources noted above had no involvement in the study design, collection, analysis, interpretation of data, and writing of the report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Aleyan, S., Ferro, M.A., Hitchman, S.C. et al. Does having one or more smoking friends mediate the transition from e-cigarette use to cigarette smoking: a longitudinal study of Canadian youth. Cancer Causes Control 32, 67–74 (2021). https://doi.org/10.1007/s10552-020-01358-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-020-01358-1