Abstract
Purpose
We investigated prospectively the relationship between dietary intakes of methionine, B vitamins associated with one-carbon metabolism, and risk of incident and fatal prostate cancer.
Methods
The Melbourne Collaborative Cohort Study recruited 41,514 people aged 40–69 years between 1990 and 1994. During follow-up of 14,620 men for 15 years on average, we ascertained 1,230 incident prostate cancers and 114 prostate cancer deaths. Dietary intakes were estimated using a 121-item food frequency questionnaire. Hazard ratios (HR) and 95 % confidence intervals were estimated using Cox regression.
Results
For overall prostate cancer incidence, HRs for riboflavin intake were significantly increased relative to quintile 1 (except quintile 5), with a peak for quintile 3, HR 1.29 (1.07, 1.57). A similar but non-statistically significant pattern existed between riboflavin intake and prostate cancer mortality. The HR for folate intake and overall incidence was significantly increased for quintile 4, HR 1.21 (1.01, 1.46). No association was observed between prostate cancer mortality and the intake of either folate or any other B vitamin or methionine, and no observed association varied by tumor aggressiveness (all Phomogeneity > 0.1).
Conclusions
We found little evidence of association between dietary intakes of B vitamins or methionine and prostate cancer risk. Weak associations between prostate cancer incidence and dietary intake of riboflavin and folate, and between riboflavin intake and prostate cancer mortality, need corroboration by other studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One-carbon metabolism comprises a complex network of biochemical pathways, involving interactions between several B vitamins, homocysteine and methionine. Disruption of one-carbon metabolism can interfere with DNA replication, DNA repair, and regulation of gene expression through methylation, each of which could promote carcinogenesis [1]. Thus, dietary intake of B vitamins and methionine might play an important role in the development and progression of cancer.
Studies investigating associations between B vitamins and prostate cancer risk have mainly focused on folate and vitamin B12, and a recent meta-analysis concluded that there were positive associations with circulating levels [2], consistent with dietary studies of vitamin B12 [3, 4], whereas other studies of either intake or blood levels of folate have been inconclusive [3–14]. Associations between other B vitamins and prostate cancer risk have been less widely studied, and findings are inconsistent [3, 4, 8, 10, 15, 16].
We investigated prospectively the relationship between dietary intakes of methionine, B vitamins associated with one-carbon metabolism, and risk of incident and fatal prostate cancer.
Methods
The Cohort
The Melbourne Collaborative Cohort Study (MCCS) is a prospective cohort study of 41,514 people (17,045 men, 24,469 women) aged 27–80 at baseline, 99.3 % of whom were aged 40–69 years. Recruitment occurred between 1990 and 1994. Southern European migrants to Australia (including 2,420 Italian and 2,072 Greek men) were over-sampled to extend the range of lifestyle exposures, including diet, and to increase genetic variation. The study protocol was approved by The Cancer Council Victoria’s Human Research Ethics Committee.
Subjects were recruited via the Electoral Rolls (registration to vote is compulsory for adults in Australia), advertisements, and community announcements in local media. Comprehensive lists of Italian and Greek surnames were also used to target southern European migrants in phone books and Electoral Rolls. Follow-up has been conducted by record linkage to Electoral Rolls, electronic phone books and the Victorian Cancer Registry and Victorian death records until 31 December 2009.
Subjects
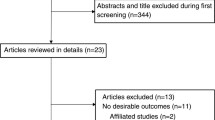
We excluded participants who had a diagnosis of prostate cancer (n = 108) or unknown primary cancer before study entry (n = 1) and were missing data for any of the nutrients of interest (n = 34), and those who reported extreme values (top or bottom percentile) of total energy intake (n = 339). Participants who had reported a diagnosis of angina, heart attack, or diabetes at baseline (n = 1,923) were also excluded as they might have changed their diet due to their diagnosis. Those with missing values for any of the confounders (n = 9) and eleven prostate cancer cases with insufficient information to classify tumor aggressiveness were also excluded, leaving 14,620 men available for the incidence analyses. For the mortality analyses, a further three men who died during follow-up with no cause of death recorded were also excluded, as was one man who died from prostate cancer but was not identified as an incident case, leaving 14,616 men available for these analyses.
Identification of incident prostate cancer cases and deaths
Incident cases were identified from notifications of first diagnoses of prostate cancer (International Classification of Diseases 9th revision rubric 185, or 10th revision rubric C61) to the Victorian Cancer Registry to 31 December 2009 and to the National Cancer Statistics Clearing House to 31 December 2004. Thus, we were unable to follow up those subjects who moved outside of Victoria after 31 December 2004. Only subjects with invasive or metastatic primary cancers of the prostate were counted as cases. Mortality data, including cause of death, were obtained from the Australian Bureau of Statistics, Victorian death records, and National Death Index or were coded by the Victorian Cancer Registry and were used to identify deaths attributed to prostate cancer. Incident cases who subsequently died from prostate cancer by 31 December 2009 were classified as fatal cases regardless of their stage at diagnosis. Aggressive tumors were defined as those with a Gleason score greater than 7 or with poor differentiation, stage 4, or a fatal case; all other tumors were classified as non-aggressive. We identified 1,230 incident prostate cancer cases (average follow-up of 15.1 years) of which 880 were categorized as non-aggressive and 350 as aggressive, and 114 prostate cancer deaths (average follow-up of 15.7 years).
Nutrient measures
Participants completed a 121-item food frequency questionnaire (FFQ) specifically developed for the MCCS using weighed food records of equal numbers of people born in Australia, Italy. and Greece [17] and answered additional questions about milk consumption and alcohol intake. Average portion sizes were assigned to each food item, and daily frequencies of some fruits were seasonally adjusted. Nutrient composition data were derived from the Australian NUTTAB 2006 database [18]. Mean daily intakes for the 5 nutrients (riboflavin (vitamin B2), vitamin B6, folate (vitamin B9), vitamin B12, and methionine) and for lycopene and calcium (potential confounders) were obtained by multiplying the daily frequency of each food item by the nutrient composition for an average portion size. Folate intake only included that occurring naturally in foods.
Measurements
Each participant’s height and weight were measured at study entry according to written protocols based on standard procedures [19]. Weight was measured to 100 g using digital electronic scales and height to 1 mm using a stadiometer. Body Mass Index (BMI) was calculated as weight in kilograms divided by the square of height in meters.
Questionnaire measures
At baseline, information was obtained on country of birth, highest level of education, and alcohol consumption.
Statistical analysis
For the analyses of incident prostate cancer, follow-up began at study entry and continued until date of diagnosis of prostate cancer, date of diagnosis of cancer of an unknown primary site, date of an unconfirmed diagnosis of prostate cancer, date of death, date last known to be in Australia, date last known to be in Victoria if after 2004 or 31 December 2009, whichever came first. For the analyses of prostate cancer mortality, follow-up began at study entry and continued until date of death, date last known to be in Australia, date last known to be in Victoria if after 2004 or 31 December 2009 whichever came first.
Intakes of energy and each nutrient were log transformed and then adjusted for energy intake using the residuals method [20]. Quintiles were obtained for each energy-adjusted nutrient using the whole sample; the lowest quintile was used as the referent category. To estimate linear trends on a log hazard scale, each nutrient variable was fitted as a pseudocontinuous covariate (using the median value in each nutrient quintile). To investigate departures from linearity in the relationship between nutrient intake and overall prostate cancer incidence and mortality, the likelihood ratio test was used to compare the linear and categorical models [21]. We also included a quadratic pseudocontinuous term for each nutrient in these models and assessed the significance of this term using the Wald test. In the competing risk models, a two-way interaction between aggressiveness and a quadratic pseudocontinuous term for each nutrient was included, and the significance of this term was assessed (Wald test) to investigate departures from linearity.
Cox regression models were fitted, with age as the time axis [22], to estimate hazard ratios (HRs) and 95 % confidence intervals separately for prostate cancer incidence and mortality associated with each nutrient measure. To test for heterogeneity in the HRs by tumor aggressiveness (non-aggressive versus aggressive disease), we fitted Cox’s proportional regression models for competing risk using the data duplication method [23].
The decision to include potential confounders in the models was based on a Directed Acyclic Graph (DAG), and all analyses were adjusted for country of birth (Australia, United Kingdom, Greece, and Italy); alcohol consumption (lifetime abstainers, ex-drinkers, low (1–39 g/day), moderate (40–59 g/day), and high intake (≥60 g/day)); education (primary school, some high school, completed high school, and completed degree/diploma); BMI; lycopene intake (μg/day); and calcium intake (mg/day). Additional analyses involved fitting and testing (using the test for homogeneity) two-way interaction terms between tumor aggressiveness and each confounder in the competing risk model. Only the interaction between tumor aggressiveness and BMI was statistically significant and retained in the analyses.
To examine the interaction of each nutrient with alcohol and the interaction of each B vitamin with methionine, nutrient intakes were dichotomized at the medians and alcohol consumption was categorized into three groups [none (never and ex-drinkers), low, and high (moderate and high intake)].
Using a subset of our data, we investigated whether the adjustment of selected models for family history of prostate cancer (in the father or brothers) affected the estimates. Data on family history of prostate cancer were from a postal questionnaire sent 4 years after study entry (sample size, n = 9,983 and 750 cases).
Statistical analyses were performed using Stata/SE 11.0 (Stata Corporation, College Station, TX). p < 0.05 (two-sided) was considered statistically significant. Tests based on Schoenfeld residuals showed no evidence of violation of the proportional hazards assumption. All analyses were repeated excluding the first 2 years of follow-up to eliminate the possibility that the observed relationships were influenced by pre-existing disease.
Results
By 31 December 2009, 53 (0.4 %) eligible participants had left Australia, 59 (0.4 %) had left Victoria between 1 January 2005 and 31 December 2009, and 2,258 (15.4 %) had died. The mean age at diagnosis was 68 years, and the mean age at death from prostate cancer was 74 years. Demographic characteristics and mean daily energy-adjusted nutrient intakes for the study sample are shown in Table 1.
Spearman correlation coefficients between the energy-adjusted B vitamins and methionine are shown in Table 2. Moderate correlations were observed between intakes of riboflavin and folate (ρ = 0.39), vitamin B12 and vitamin B6 (ρ = 0.63), and vitamin B12 and methionine (ρ = 0.50).
Table 3 shows the HRs for prostate cancer incidence and mortality in relation to B vitamins and methionine intake. There was evidence of a departure from linearity in the relationship between riboflavin intake and incidence of all prostate cancer (p = 0.03) and non-aggressive disease (p = 0.05) but not for any other nutrient in any of the models (all p > 0.08). We found no significant linear associations between dietary intake of any B vitamin or methionine and prostate cancer incidence or mortality. The inclusion of a quadratic nutrient term suggested an inverse U-shaped relationship between riboflavin intake and all prostate cancer incidence (p = 0.004), non-aggressive disease (p = 0.05), and prostate cancer mortality (p = 0.02) and between all prostate cancer incidence and folate (p = 0.05).
The HRs for prostate cancer occurrence for each quintile of riboflavin intake relative to the first were significantly increased except for quintile 5 [HR 1.23 (1.01, 1.49), HR 1.29 (1.07, 1.57), and HR 1.23 (1.01, 1.49) for quintiles 2–4, respectively]. A similar pattern was observed for prostate cancer mortality (except HR for quintile 5 was less than unity), with a peak for quintile 3, HR 1.74 (0.95, 3.21), but no HR reached statistical significance.
The HR for all prostate cancer incidence was significantly elevated for quintile 4 of folate intake, HR 1.21 (1.01, 1.46), but not for the other quintiles. Conversely, non-statistically significant reduced HRs for mortality were observed across all quintiles of folate intake. No associations were observed for any other B vitamin or methionine.
Table 4 shows HRs associated with interactions between selected nutrients and alcohol and methionine. For all prostate cancer incidence, we observed significant interactions between folate intake and alcohol (p = 0.04) and between folate and methionine intake (p = 0.01). A significantly increased risk was associated with high folate/high alcohol relative to low folate/high alcohol, HR 1.58 (1.19, 2.08) and for low methionine/high folate relative to low methionine/low folate, HR 1.33 (1.13, 1.56).
For prostate cancer mortality, we observed a significant interaction between alcohol intake and riboflavin (p = 0.01) (Table 4). A significantly lower risk was observed for high riboflavin/high alcohol relative to low riboflavin/high alcohol, HR 0.19 (0.05, 0.83).
We found no other significant interactions between any of the other B vitamins or methionine and alcohol (all p > 0.2) or between any other B vitamin and methionine intake (all p > 0.18). We did not investigate these interactions further in the competing risk models due to small numbers and because tests of homogeneity in the HRs between non-aggressive and aggressive tumors were not significant (all p > 0.1).
Further adjustment of the models for family history of prostate cancer using a subset of our data did not substantially change the HRs neither did additional analyses excluding the first 2 years of follow-up.
Discussion
Overall, we detected no linear associations between dietary intakes of either methionine or B vitamins and prostate cancer risk or mortality. There was suggestive evidence of an inverse U-shaped relationship between incidence and both riboflavin and folate intake and between mortality and riboflavin intake. We observed statistically significant interactions between folate and alcohol and all prostate cancer risk, high alcohol/high folate being associated with the highest risk; and between folate and methionine intake, low methionine/high folate being associated with the highest risk. For prostate cancer mortality, we observed a significant interaction between alcohol and riboflavin intake, reduced risk being associated with high alcohol/high riboflavin intake, and increased risk with low alcohol/high riboflavin intake. Alcohol and methionine intake did not appear to substantially modify any of the other observed associations. Some observed associations might have been due to chance, given the number of comparisons performed.
Generally, consistent with other studies, we observed no variation in association by disease severity [2, 4, 10, 14, 24]. The only report of significant heterogeneity by disease severity is from the EPIC (European Prospective Investigation into Cancer and Prevention) study in regard to circulating vitamin B12, a positive association being observed with advanced prostate cancer and a null association with localized disease; on the other hand, EPIC reported no significant heterogeneity between low and high grade disease [15].
We had virtually complete follow-up in this prospective study as the identification of incident prostate cancers was performed by record linkage to the Australian-based cancer registries that have complete coverage of the cohort participants. Although the interstate linkage is complete only to the end of 2004, only six cases were diagnosed interstate between 1990 and 2004; thus, it is unlikely that we have missed many interstate cases. Only 0.4 % of participants left Australia during follow-up, and hence, we would not expect to have missed many cases or deaths. Analyses excluding the first 2 years of follow-up gave similar associations to those reported; thus, it is unlikely that our findings were influenced by pre-existing disease. Further, adjustment of our models using a subset of data regarding family history of prostate did not substantially affect our results.
Our study’s limitations include the fact that information on diet and potential confounding variables was only collected at baseline and might not be relevant to the full time period. We could not account for any change in dietary habits over follow-up, although older people tend to have stable diets [25]. Further, inter-correlations between B vitamins and methionine [26] make it difficult to estimate the effect of a single nutrient. For some subgroups, particularly for mortality and for interaction analyses, the small number of cases led to low precision. Voluntary folic acid fortification of foods has been progressively introduced in Australia, and fortification of bread flour has been mandatory since 2009 [27]; we were unable to account for this. Some misclassification of nutrient intake is inevitable since we only assessed dietary intake and did not have data on B vitamins supplement use. However, less than 13 % of our sample used multivitamins, so it is unlikely that this lack of information would have affected our estimates substantially. Intakes of B vitamins are estimated from FFQs with considerable error; a fact supported by the low correlations between dietary and serum levels of nutrients reported by the ATBC (α-Tocopherol, β-Carotene Cancer Prevention) study [4], although metabolic effects may also contribute to variations in circulating levels. Misclassification of dietary intakes will attenuate any estimate of association between diet and cancer and could, thus, contribute to differences in the results of studies using dietary intakes or biomarkers.
Riboflavin deficiency interferes with the metabolism of other B vitamins through flavin coenzyme activity [28]. Riboflavin is a co-factor of methylenetetrahydrofolate reductase, and there appears to be some evidence for an interaction between riboflavin status, folate status and genotype in determining plasma homocysteine as a marker of folate status [29]. In Western diets, cereals, milk, dairy products, meat (especially offal), and fatty fish are good sources of riboflavin intake, and reasonably high concentrations can be found in some fruits and dark-green leafy vegetables [28]. In Australia, breads and cereal are often fortified with riboflavin [30]; this was accounted for in the calculation of riboflavin intake.
Consistent with our findings, a small, European case–control study reported an elevated prostate cancer risk associated with higher riboflavin intakes but no overall linear association [3]. In contrast to the elevated mortality risks we observed with riboflavin intake, Kasperzyk et al. [8] found no association with prostate cancer survival. The increased risk for men with higher riboflavin intakes in the present study is consistent with the results reported for circulating riboflavin, choline, and betaine by the Northern Sweden Health and Disease Cohort Study, supporting a role for methyl availability in prostate cancer development [15]. We are aware of only one other study that investigated the interaction between riboflavin and alcohol and, in contrast to ours, this study reported no association with prostate cancer survival [8].
A recent review has explored several mechanisms by which folate might be related to carcinogenesis including altered DNA and RNA methylation and disruption of DNA integrity and repair [31]. Evidence from experimental studies suggests that folate deficiency might promote initial stages of carcinogenesis, whereas excess folic acid might stimulate existing neoplasms [32–34], which is not supported by our findings. Folate is found naturally in green leafy vegetables, fruit, legumes, and cereals.
Consistent with our findings, others have reported no linear associations between dietary folate and prostate cancer incidence [4, 5, 9, 13]. One of these studies reported elevated risks of all prostate cancer with higher folate intake [5] whereas another reported higher folate intake only to be associated with a non-significant decreased risk of advanced prostate cancer [13]. Although we reported slightly elevated risks for overall prostate cancer (only statistically significantly for quintile 4) and non-significant reduced risks for prostate cancer mortality, we detected no clear associations with risk of aggressive prostate cancer. A recent meta-analysis that included the EPIC and ATBC studies [2] reported elevated risks of prostate cancer associated with higher circulating folate levels. We are aware of only two studies that have investigated relationships between folate status and prostate cancer mortality: a positive association with serum folate was reported by an Australian cohort [11] whereas a null association with folate intake was reported by a Swedish cohort [8].
Our study provides weak evidence that the association between folate status and prostate cancer risk might be modified by alcohol intake. Alcohol is known to interfere with folate absorption [35]; thus, we might expect to see a protective effect associated with higher folate intakes for men with high alcohol consumption, which was not apparent in our study. Our findings are in contrast to the reduced risks reported by an Italian case–control study (although the overall interactions were not significant) [10] and null associations reported by others [2, 4, 8, 12, 16].
Methionine and folate are required in the production of S-adenosylmethionine, the primary methyl donor. When methionine levels are low, more folate is used as methyltetrahydrofolate to form methionine, and the resulting lower levels of methyltetrahydrofolate might affect DNA synthesis [36]. Thus, we might expect to see a protective effect associated with higher folate levels for men with low methionine intake, which is in contrast to the significantly increased risk we observed in our study. We observed a significant interaction between folate and methionine intake, in contrast to the null association reported by Pelucchi et al. [10]. In this same study, a significantly reduced prostate cancer risk was associated with a high methionine/high folate intake versus high methionine/low folate, whereas we found no association with this combination.
We found no association between vitamin B6 intake and prostate cancer risk, consistent with reports from two case–control studies [3, 10], for circulating B6 from the EPIC study [15] and for serum B6 from the ATBC study [16] that was in contrast to the inverse association reported for vitamin B6 intake in this same cohort [4]. We found no association between vitamin B6 and prostate cancer mortality, in contrast to the inverse association reported by a Swedish cohort [8]. In contrast to our null findings for vitamin B12, others have reported positive associations between prostate cancer risk and dietary B12 [3, 4] and a recent meta-analysis, for circulating B12 [2]. Consistent with our findings, Kasperzyk et al. [8] reported no association with mortality. Also consistent with our study, others have reported null associations for methionine intake and prostate cancer risk [4, 10] and mortality [8].
Given the slow progression of prostate tumors and that neoplastic transformation occurs several years before diagnosis, the conflicting evidence in the literature is not surprising. The direction of the relative risks associated with B vitamin or methionine intakes might depend on the time between measuring intake and diagnosis.
Conclusions
Our findings suggest a weak inverse U-shaped association between prostate cancer risk and riboflavin and folate intakes, and between prostate cancer mortality and riboflavin intake. These associations need to be confirmed by other prospective studies.
References
Kim YI (2004) Folate and DNA methylation: a mechanistic link between folate deficiency and colorectal cancer? Cancer Epidemiol Biomarkers Prev 13:511–519
Collin SM, Metcalfe C, Refsum H, Lewis SJ, Zuccolo L, Smith GD et al (2010) Circulating folate, vitamin B12, homocysteine, vitamin B12 transport proteins, and risk of prostate cancer: a case-control study, systematic review, and meta-analysis. Cancer Epidemiol Biomarkers Prev 19:1632–1642
Vlajinac HD, Marinkovic JM, Ilic MD, Kocev NI (1997) Diet and prostate cancer: a case-control study. Eur J Cancer 33:101–107
Weinstein SJ, Stolzenberg-Solomon R, Pietinen P, Taylor PR, Virtamo J, Albanes D (2006) Dietary factors of one-carbon metabolism and prostate cancer risk. Am J Clin Nutr 84:929–935
Aune D, Deneo-Pellegrini H, Ronco AL, Boffetta P, Acosta G, Mendilaharsu M et al (2011) Dietary folate intake and the risk of 11 types of cancer: a case-control study in Uruguay. Ann Oncol 22:444–451
Beilby J, Ambrosini GL, Rossi E, de Klerk NH, Musk AW (2010) Serum levels of folate, lycopene, beta-carotene, retinol and vitamin E and prostate cancer risk. Eur J Clin Nutr 64:1235–1238
Figueiredo JC, Grau MV, Haile RW, Sandler RS, Summers RW, Bresalier RS et al (2009) Folic acid and risk of prostate cancer: results from a randomized clinical trial. J Natl Cancer Inst 101:432–435
Kasperzyk JL, Fall K, Mucci LA, Hakansson N, Wolk A, Johansson JE et al (2009) One-carbon metabolism-related nutrients and prostate cancer survival. Am J Clin Nutr 90:561–569
McCann SE, Ambrosone CB, Moysich KB, Brasure J, Marshall JR, Freudenheim JL et al (2005) Intakes of selected nutrients, foods, and phytochemicals and prostate cancer risk in western New York. Nutr Cancer 53:33–41
Pelucchi C, Galeone C, Talamini R, Negri E, Parpinel M, Franceschi S et al (2005) Dietary folate and risk of prostate cancer in Italy. Cancer Epidemiol Biomarkers Prev 14:944–948
Rossi E, Hung J, Beilby JP, Knuiman MW, Divitini ML, Bartholomew H (2006) Folate levels and cancer morbidity and mortality: prospective cohort study from Busselton. West Aust Ann Epidemiol 16:206–212
Shannon J, Phoutrides E, Palma A, Farris P, Peters L, Forester A et al (2009) Folate intake and prostate cancer risk: a case-control study. Nutr Cancer 61:617–628
Stevens VL, Rodriguez C, Pavluck AL, McCullough ML, Thun MJ, Calle EE (2006) Folate nutrition and prostate cancer incidence in a large cohort of US men. Am J Epidemiol 163:989–996
Johansson M, Appleby PN, Allen NE, Travis RC, Roddam AW, Egevad L et al (2008) Circulating concentrations of folate and vitamin B12 in relation to prostate cancer risk: results from the European prospective investigation into cancer and nutrition study. Cancer Epidemiol Biomarkers Prev 17:279–285
Johansson M, Van Guelpen B, Vollset SE, Hultdin J, Bergh A, Key T et al (2009) One-carbon metabolism and prostate cancer risk: prospective investigation of seven circulating B vitamins and metabolites. Cancer Epidemiol Biomarkers Prev 18:1538–1543
Weinstein SJ, Hartman TJ, Stolzenberg-Solomon R, Pietinen P, Barrett MJ, Taylor PR et al (2003) Null association between prostate cancer and serum folate, vitamin B(6), vitamin B(12), and homocysteine. Cancer Epidemiol Biomarkers Prev 12:1271–1272
Ireland P, Jolley D, Giles G, O’Dea K, Powles J, Rutishauser I et al (1994) Development of the Melbourne FFQ: a food frequency questionnaire for use in an Australian prospective study involving an ethnically diverse cohort. Asia Pac J Clin Nutr 3:19–31
FSANZ (2006) Food standards Australia New Zealand. NUTTAB
Lohman TG, Roche AF, Martorell R (1988) Anthropometric standardization reference manual. Human Kinetic Books, Champaign, IL, USA
Willett W, Stampfer MJ (1986) Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 124:17–27
Kirkwood BR, Sterne JAC (2003) Essential medical statistics, 2nd edn. Blackwell Science, Malden, MA, USA
Korn EL, Graubard BI, Midthune D (1997) Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol 145:72–80
Lunn M, McNeil D (1995) Applying Cox regression to competing risks. Biometrics. 51:524–532
Hultdin J, Van Guelpen B, Bergh A, Hallmans G, Stattin P (2005) Plasma folate, vitamin B12, and homocysteine and prostate cancer risk: a prospective study. Int J Cancer 113:819–824
Jungjohann SM, Luhrmann PM, Bender R, Blettner M, Neuhauser-Berthold M (2005) Eight-year trends in food, energy and macronutrient intake in a sample of elderly German subjects. Br J Nutr 93:361–378
Key T (1994) Micronutrients and cancer aetiology: the epidemiological evidence. Proc Nutr Soc 53:605–614
FSANZ (2009) Food Standards Australia New Zealand 2.1.1. From http://www.comlaw.gov.au/Details/F2009C00811. Accessed April 2012
Powers HJ (2003) Riboflavin (vitamin B-2) and health. Am J Clin Nutr 77:1352–1360
Powers HJ (2005) Interaction among folate, riboflavin, genotype, and cancer, with reference to colorectal and cervical cancer. J Nutr 135:2960S–2966S
FSANZ (2011) Food Standards Australia New Zealand 1.3.2. From http://www.comlaw.gov.au/Details/F2011C00541. Accessed April 2012
Choi SW, Mason JB (2000) Folate and carcinogenesis: an integrated scheme. J Nutr 130:129–132
Ebbing M, Bonaa KH, Nygard O, Arnesen E, Ueland PM, Nordrehaug JE et al (2009) Cancer incidence and mortality after treatment with folic acid and vitamin B12. JAMA 302:2119–2126
Kim YI (2007) Folate and colorectal cancer: an evidence-based critical review. Mol Nutr Food Res 51:267–292
Ulrich CM, Potter JD (2007) Folate and cancer–timing is everything. JAMA 297:2408–2409
Hillman RS, Steinberg SE (1982) The effects of alcohol on folate metabolism. Annu Rev Med 33:345–354
Blount BC, Mack MM, Wehr CM, MacGregor JT, Hiatt RA, Wang G et al (1997) Folate deficiency causes uracil misincorporation into human DNA and chromosome breakage: implications for cancer and neuronal damage. Proc Natl Acad Sci U S A 94:3290–3295
Acknowledgments
This study was made possible by the contribution of many people, including the original investigators and the diligent team who recruited the participants and who continue working on follow-up. We would also like to express our gratitude to the many thousands of Melbourne residents who continue to participate in the study. Cohort recruitment was funded by VicHealth and The Cancer Council Victoria. This work was supported by infrastructure from the Cancer Council Victoria and grants from the National Health and Medical Research Council (209057, 251533, 520316).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bassett, J.K., Severi, G., Hodge, A.M. et al. Dietary intake of B vitamins and methionine and prostate cancer incidence and mortality. Cancer Causes Control 23, 855–863 (2012). https://doi.org/10.1007/s10552-012-9954-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-012-9954-5



