Abstract
Objective
To assess the association between serum triglyceride levels and cancer risk.
Methods
The metabolic syndrome and cancer project (Me-Can) includes cohorts from Norway, Austria, and Sweden; the current study included data on 257,585 men and 256,512 women. The mean age at study entry was 43.8 years for men and 44.2 years for women. The mean follow-up time was 13.4 years (SD = 8.5) for men and 11.9 years (SD = 7.2) for women. Excluding the first year of follow-up, 23,060 men and 15,686 women were diagnosed with cancer. Cox regression models were used to calculate relative risk (RR) of cancer for triglyceride levels in quintiles and as a continuous variable. RRs were corrected for random error by use of regression dilution ratio.
Results
Relative risk for top quintile versus bottom quintile of triglycerides of overall cancer was 1.16 (95% confidence interval 1.06–1.26) in men and 1.15 (1.05–1.27) in women. For specific cancers, significant increases for top quintile versus bottom quintile of triglycerides among men were found for cancers of the colon, respiratory tract, the kidney, melanoma and thyroid and among women, for respiratory, cervical, and non-melanoma skin cancers.
Conclusion
Data from our study provided evidence for a possible role of serum triglycerides in cancer development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High levels of serum triglycerides (STG) in blood are related with coronary heart disease [1–6], however, the relationship between serum triglycerides and cancer is less well known. Several pathological and molecular mechanisms suggested a link between triglycerides, as part of the metabolic syndrome, and risk of cancer [7–9]. However, prospective studies on the relation of serum triglycerides to overall and site-specific cancers are rare [10, 11]. Although a few studies have reported on the association with site-specific cancer such as colorectal, breast, and prostate, results are contradictory [12–17].
Differences in the study populations, length of follow-up, study endpoints and statistical adjustment for confounding may all have contributed to the conflicting patterns of association seen in earlier studies. Consistent results may also be lacking due to small sample sizes and infrequent events in several previous investigations. Moreover, the role of regression dilution bias in long-term prospective studies of incident diseases in relation to baseline risk factors measured at single occasion was not considered before [18].
The aim of the study was to investigate the association between serum triglycerides and overall and site-specific cancer risk in a large prospective cohort of 514,097 participants with 38,746 incident cancers. To our knowledge, this is the largest cohort study to date to prospectively investigate the association of STG with overall and site-specific cancer risk in men and women.
Materials and methods
Study population
The Metabolic syndrome and Cancer project (Me-Can) includes data from population-based cohorts in Norway, Austria, and Sweden. A detailed description of the project has recently been published [19, 20]. In brief, seven existing cohorts from Austria (the Vorarlberg Health Monitoring and Prevention Programme-VHM&PP), Norway (the Oslo study, the Norwegian Counties study-NCS, the Cohort of Norway-CONOR and the Age 40 programme-40-y) and Sweden (the Västerbotten Intervention Project-VIP and the Malmö Preventive Project-MPP) were pooled in 2006. Participants in the cohorts had undergone one or more health examination(s), and information on life style and socio-demographic factors had been recorded. Altogether, data on 514,097 men and women were used in this study.
Measurements
Measurements of height, weight, smoking status (current, former, never), serum triglycerides have been obtained for the study participants in various health examinations. Anthropometric measurements were conducted in a similar way in all Me-Can cohorts, with participants wearing light indoor clothes and no shoes. For smoking status, participants (except in VHM&PP) were asked to fill in a questionnaire regarding smoking habits. In VHM&PP, questions regarding smoking were asked by the examining physician, and answers were recorded.
Different fasting times before blood draw were used in the different cohorts [19]. In the Norwegian cohorts, fasting was not required before the examination, and fasting time was recorded as less than 1 h, 1–2, 2–4, 4–8, or more than 8 h. Fasting time in the VIP was recorded as less than 4 h, 4–8, or more than 8 h, and from 1992, participants were asked to fast for at least 8 h before the examination. In the MPP and after the initial 3 years in the VHM&PP, a minimum of 8 h of fasting was used as standard procedure. Serum levels of triglycerides were measured with a non-enzymatic method in the Oslo and NCS cohorts, and with an enzymatic method in all other cohorts. Levels measured with the non-enzymatic method have been transformed according to formulas: 0.90 (triglyceride level)–0.11 and are presented in mmol/L [19].
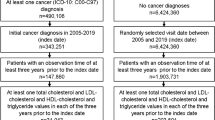
Selection of subjects
Selection of subjects for the study is described in Fig. 1. The full Me-Can dataset included 924,801 participants with 1,566,553 health examinations after an initial data cleaning process as shown in the figure. We selected the first observation for each individual, and if data from a fasting state and data on smoking status were available, the first of these observations was selected. Thus, for each individual, data were included from the first health examination with complete data to comprise the baseline set of measurements. Further exclusions were made for observations without data on fasting time and observations with fasting time 4–8 h. The latter is based on reports showing that triglycerides reach their peak postprandial level within 4 h of ingestion, and clearance from serum occurs slowly reaching a fasting state 8–12 h after ingestion [3, 21]. Subjects were further excluded from the Norwegian cohorts due to policy restrictions imposed by the Norwegian Institute of Public Health that the proportion of Norwegian subjects in Me-Can studies should not exceed approximately 50%. Exclusions were made for observations with time less than 1 year after measurement in order to avoid the effect of short-term reverse causation. The final data set used in this study included 514,097 subjects.
End points
Each of the cohorts was linked to the respective National registers for identification of cancer diagnosis, emigration (except for Austria), vital status and cause of death. Incident cancer cases were identified through linkages with national cancer registries of the respective countries. End-points were the date of the first cancer diagnosis, emigration, death or December 31, 2003 (Austria), 2005 (Norway), and 2006 (Sweden), whichever occurred first. Cancers were categorized according to the International Classification of Diseases, seventh revision (ICD-7).
Statistical analysis
We used Cox proportional hazard regression to estimate hazard ratios, denoted as relative risks (RR), for triglyceride levels with risk of incident cancer. Age was used as time variable, and all estimates were stratified by sub-cohort and categories of birth date: ≤1929, 1930–1939, 1940–1949, 1950–1959 and ≥1960. We estimated RR for triglycerides levels in quintiles calculating cut-off levels separately for sub-cohort, sex, and fasting time. Linear tests for trend were performed using triglyceride quintiles as an ordinal variable. Secondary analysis was done using triglycerides as a logarithmically transformed (due to the skewed distribution) continuous variable. All analyses included adjustment for age at baseline measurement (continuous), BMI (categories: ≤20.0, 20.01–, 25.01–, 30.01 kg/m2) and smoking status (categories: never smoker, ex-smoker, and current smoker). All models were further adjusted for fasting time in the secondary analysis where triglycerides were used as continuous variable. Lag-time analyses leaving out the first 5–10 years of follow-up were performed to check for reverse causation effects.
We calculated regression dilution ratio (RDR) in order to adjust RRs for random measurement error [22, 23]. RDR was calculated based on data from repeated health examinations in 133,820 subjects, including 406,364 observations, in the full Me-Can cohort. Only repeated measurements with the same fasting time and in the same cohort as in the baseline, and with data on smoking status, were used. Mean time between the baseline measurement and repeated measurements was 6.9 years (standard deviation, SD = 3.9). We used a linear mixed effects model, similar to that described by Wood et al. [23].
We checked the Cox proportional hazards assumption for triglycerides, BMI, and smoking status by the statistical test of Schoenfeld residuals. For some cancers, there was an indication of violation of proportionality for BMI or smoking status; however, RRs with and without stratification of the variables within the model were very similar. Thus, BMI and smoking status were not kept as stratum in the model. Statistical analyses were performed with Stata (version 10, StataCorp LP, College Station, Texas) and R (version 2.7.2, used for RDR calculation).
Results
The mean age at study entry was 43.8 years for men and 44.2 years for women. The mean follow-up time was 13.4 years (SD = 8.5) for men and 11.9 years (SD = 7.2) for women. (Table 1) During follow-up, 38,746 incident invasive cancer cases were identified. Out of a total of 514,097 study participants 270,727 (52.7%) had fasted more than 8 h and 243,370 (47.3%) had fasted for less than 4 h before the blood sampling. The Norwegian cohorts accounted for 91.2% of the individuals who have fasted for less than 4 h. Baseline age, BMI and total cancer risk increased with higher triglyceride quintiles. Among fasting individuals, the proportion of participants with abnormal triglyceride levels, defined as a value greater or equal to 1.7 mmol/L (21) ranged from 27.8% in MPP to 35.0% in VHM&PP in men and 12.0 to 29.4% in MPP and VHM&PP in women, respectively (Supplementary Table 1). The prevalence of overweight or obesity, i.e., BMI 25 kg/m2 or higher, among men ranged between 40% in the Oslo cohort to 62% in the CONOR cohort and among women between 34% in NCS to 47% in the CONOR cohort.
Table 2 shows associations of STG adjusted for age at baseline, smoking and BMI, stratified by sub-cohorts and year of birth with overall and site-specific cancer risk in men. Compared with the 1st quintile, STG concentrations in 5th quintile were significantly associated with increased risk of total cancer, colon cancer, cancer of the respiratory system, renal cell carcinoma, melanoma of the skin, and thyroid cancer. In contrast, high STG concentrations were inversely associated with risk prostate cancer and non-Hodgkin’s lymphoma.
In Table 3, associations are shown for women. Relative risk for 5th quintile, when compared to the 1st quintile, was associated with increased risk of total cancer, cancer of the respiratory system, cervical cancer, non-melanoma skin cancer, and other non-specified cancers.
In men, increased risk of cancer for one log-unit increment of STG adjusted for age at baseline, smoking, BMI and fasting time, and stratified by sub-cohort and year of birth was seen for total cancer, cancers of the lip, oral cavity, pharynx, colon, respiratory tract, kidney and leukemia. Significant inverse associations were observed for prostate cancer and non-Hodgkin’s lymphoma. In women, significant association per one log-unit increment was seen for total cancer, cancers of the lip, oral cavity, pharynx, rectum/anus, respiratory tract, cervix, and other non-specified cancers (Tables 2, 3).
Furthermore, data in Tables 2 and 3 show that BMI adjustment had very little effect on relative risk in the association between one log-unit increment of STG and cancer incidence.
We checked for possible interaction between smoking and serum triglycerides as the latter showed significant association with respiratory cancers. However, we found no significant interactions with p interaction = 0.052 and 0.36 for men and women, respectively.
There were no significant interactions between triglycerides and the different cohorts on the risk of overall incident cancer either in men or in women: (p interaction = 0.82 and 0.06, respectively). For specific cancer types, we found significant interaction only for respiratory cancers in men (p interaction = 0.02). The RR per log unit increment of triglycerides ranged between 0.96 (0.81–1.15) in the CONOR cohort, and 1.28 (1.11–1.39) in the VHM&PP.
Lag-time analysis leaving out the first 5 years of follow-up showed that the significant inverse association observed between STG and non-Hodgkin’s lymphoma in men disappeared (RR per log unit increment of serum triglycerides: 0.85; 95% CI, 0.73–1.00). For prostate cancer, the association remained statistically significant when we excluded the first 5 years of follow-up but disappeared when 7 years were excluded (RR: 0.93; 95% CI, 0.88–0.98) and (RR: 0.94; 95% CI, 0.88–1.00), respectively.
Separate sub-analyses for fasting and non-fasting individuals revealed only a few important differences in comparison with the main analysis. The association of STG with colon cancer in men was more pronounced in fasting individuals showing a relative risk of (RR: 2.70; 95% CI, 1.63–4.53) when compared to non-fasting individuals (RR: 1.63; 95% CI, 1.12–2.40). In women, we observed a significant association for non-melanoma skin cancer of (RR: 4.31; 95% CI, 1.56–11.9) versus (RR: 0.96; 95% CI, 0.40–2.36) and a borderline significant effect for corpus uteri of (RR: 1.74; 95% CI, 0.99–3.09) versus (RR: 1.07; 95% CI, 0.65–1.72) for fasting versus non-fasting STG, respectively. In contrast, only non-fasting STG showed a significant association with renal cell cancer (RR: 2.23; 95% CI, 1.14–4.37) versus (RR: 1.42; 95% CI, 0.72–2.83) and thyroid cancer (RR: 6.60; 95% CI, 1.40–30.66) versus (RR: 1.24; 95% CI, 0.17–8.47) in men and with cervical cancer (RR: 2.64; 95% CI, 1.29–5.52) versus (RR: 1.04; 95% CI, 0.37–2.77) in women.
Discussion
In this pooled population-based cohort study of more than 500,000 participants, elevated serum triglyceride levels were associated with significantly increased risk of cancer in general and at several specific sites. The relative risk of total cancer for increasing levels of triglycerides, observed both in men and women, was a modest one, but for several specific sites, the increase in relative risk was quite formidable. Although our study is the first to show significant association between STG and overall cancer in men and women separately, some of our results of site-specific cancers are in accordance with the other previous prospective studies [11, 12, 24].
We observed a comparatively strong positive association between STG levels and colon cancer in men. Although several previous studies investigated this association, results have been inconsistent [10, 12, 13, 24]. Several reports suggested positive associations between triglycerides and obesity in relation to colorectal cancer indicating possible confounding effects [7, 8, 12]. In our study, however, the models were adjusted for BMI, suggesting a strong link between STG and colon cancer irrespective of obesity. This association was not seen among women speculatively due to a protective effect of estrogen and progesterone on colon cancer [25, 26].
We also observed an association between STG and increased risk of cancers of the respiratory tract among men and women. The association of STG and respiratory cancer may possibly be related to the fact that smoking is associated with higher STG concentrations [27], and thus, residual confounding due to smoking may contribute to the association between STG concentrations and lung cancer risk as well as cancers of lip, oral cavity and pharynx.
The significant positive association of serum triglycerides with cervical cancer was also observed in other prospective studies [10, 11]. According to Cowey et al. increased levels of free fatty acids (FFAs) may be associated with reduced production of sex hormone–binding globulins (SHBGs) by the liver. Low levels of SHBGs are associated with increased availability of bioactive estradiol (E2) which in turn are considered to be mitogenic growth factors for some hormone-dependent cancers [9].
Although transformation of androgens to estrogens in obese men might be a possible explanation for the inverse association between STG and prostate cancer [9], cohort studies assessing metabolic syndrome and triglycerides in relation to prostate cancer so far have not shown any significant association [16, 17]. Moreover, we cannot rule out a possible reverse causality as the significance of the association disappeared in a sub-analysis that excluded the first 7 years of follow-up.
Other possible mechanistic evidence relating elevated triglycerides with cancer risk are speculations that hypertriglyceridemia is associated with development of oxidative stress and reactive oxygen species (ROS) [9]. Low levels of ROS regulate cellular signaling and play an important role in normal cell proliferation and are increased in cancer cells [28, 29]. Although increased oxidative stress in fat has been shown to be an important pathogenic pathway in the metabolic syndrome, further research at molecular level is required to show the exact mechanism of triglycerides in carcinogenesis [9].
A report on the role of fasting versus non-fasting serum triglyceride measurement suggested that collection of specimen at a specified postprandial state (2–4 h) could be more predictive of cardiovascular risk than in the fasting state [3, 30]. It is not known if the same implication goes for risk of cancer. Although our study showed differences on cancer risk across fasting status, it is difficult to draw conclusions about these differences based on the respective fasting time, as the fasting status of the participants in this study was non-uniform among the sub-cohorts. However, these differences are not ignorable and indicate the need to assess the situation in a data where fasting status is presented in unbiased manner.
Our study considered the role of regression dilution bias caused by random fluctuations in baseline measurements in long-term prospective studies which might underestimate the true risk. Long-term effects of triglyceride levels on coronary heart disease that occurred more than 20 years after the baseline measurement have been reported to be underestimated by 50% [18]. Although the effects of correction with RDRs are modest for overall cancer risk, they were more pronounced for sites for which there was a significant association. For example, there was a 42% increased risk of colon cancer in men in the 5th quintile of STG when compared to the 1st without correction for random error and 96% increased risk when corrected. Similar effects were found for several statistically significantly associated cancer sites for both men and women (Tables 2, 3 & supplementary Table 2).
However, our study was limited by the lack of data on drug use and other behavioral aspects like dietary habits, physical activity, and alcohol consumption which could be associated with triglycerides [31]. The slight differences in measurement methods in the cohort are limitations that we tried to overcome by using cohort specific cut-points in analysis of exposures by quintiles and by stratifying for cohort in all the analyses.
Strengths of our study include the large sample size from seven population-based cohorts in Europe with essentially complete capture of cancer cases and the correction of risk estimates for intra-individual variation of triglyceride levels. In all cohorts, data were available for BMI and smoking status, and these factors were used as adjustment in the analyses. The long follow-up period provided the opportunity to undertake lag-time sub-analysis helping to rule out possible reverse causalities.
In summary, in this pooled study of 514,097 men and women, we found significant associations between serum triglycerides and risk of cancer overall and at several sites. While further research is needed to shed light on the underlying pathophysiological mechanisms, the pattern of association seen in the present study provides epidemiological evidences for possible role of serum triglycerides in cancer incidence irrespective of obesity.
References
Sarwar N, Danesh J, Eiriksdottir G et al (2007) Triglycerides and the risk of coronary heart disease: 10, 158 incident cases among 262, 525 participants in 29 Western prospective studies. Circulation 115(4):450–458
Bansal S, Buring JE, Rifai N, Mora S, Sacks FM, Ridker PM (2007) Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. JAMA 298(3):309–316
Ridker PM (2008) Fasting versus non-fasting triglycerides and the prediction of cardiovascular risk: do we need to revisit the oral triglyceride tolerance test? Clin Chem 54(1):11–13
Iso H, Naito Y, Sato S et al (2001) Serum triglycerides and risk of coronary heart disease among Japanese men and women. Am J Epidemiol 153(5):490–499
Cambien F, Jacqueson A, Richard JL, Warnet JM, Ducimetiere P, Claude JR (1986) Is the level of serum triglyceride a significant predictor of coronary death in “normocholesterolemic” subjects? The Paris Prospective Study. Am J Epidemiol 124(4):624–632
Fontbonne A, Eschwège E, Cambien F et al (1989) Hypertriglyceridaemia as a risk factor of coronary heart disease mortality in subjects with impaired glucose tolerance or diabetes. Results from the 11-year follow-up of the Paris Prospective Study. Diabetologia 32(5):300–304
Giovannucci E (2007) Metabolic syndrome, hyperinsulinemia, and colon cancer: a review. Am J Clin Nutr 86(3):836–842
Giovannucci E (2001) Insulin, insulin-like growth factors and colon cancer: a review of the evidence. J Nutr 131:3109–3120
Cowey S, Hardy RW (2006) The metabolic syndrome: a high-risk state for cancer? Am J Pathol 169:1505–1522
Tulinius H, Sigfússon N, Sigvaldason H, Bjarnadóttir K, Tryggvadóttir L (1997) Risk factors for malignant diseases: a cohort study on a population of 22, 946 Icelanders. Cancer Epidemiol Biomarkers Prev 6(11):863–873
Ulmer H, Borena W, Rapp K et al (2009) Serum triglyceride concentrations and cancer risk in a large cohort study in Austria. Br J Cancer 101(7):120–126
McKeown-Eyssen G (1994) Epidemiology of colorectal cancer revisited: are serum triglycerides and/or plasma glucose associated with risk? Cancer Epidemiol Biomarkers Prev 3(8):687–695
Tsushima M, Nomura AM, Lee J, Stemmermann GN (2005) Prospective study of the association of serum triglyceride and glucose with colorectal cancer. Dig Dis Sci 50(3):499–505
Manjer J, Malina J, Berglund G, Bondeson L, Garne JP, Janzon L (2001) Breast cancer risk in ex-smokers in relation to body mass index, weight gain and blood lipid levels. Eur J Cancer Prev 10(3):281–287
Gaard M, Tretli S, Urdal P (1994) Risk of breast cancer in relation to blood lipids: a prospective study of 31, 209 Norwegian women. Cancer Causes Control 5(6):501–509
Lund HL, Wisloff TF, Holme I, Nafstad P (2006) Metabolic syndrome predicts prostate cancer in a cohort of middle-aged Norwegian men followed for 27 years. Am J Epidemiol 164:769–774
Tande AJ, Platz EA, Folsom AR (2006) The metabolic syndrome is associated with reduced risk of prostate cancer. Am J Epidemiol 164:1094–1102
Emberson JR, Whincup PH, Morris RW, Walker M, Lowe GD, Rumley A (2004) Extent of regression dilution for established and novel coronary risk factors: results from the British Regional Heart Study. Eur J Cardiovasc Prev Rehabil 11(2):125–134
Stocks T, Borena W, Strohmaier S et al (2009) Cohort profile: the metabolic syndrome and cancer project (Me-Can). Int J Epidemiol 39(3):660–667
Borena W, Stocks T, Strohmaier S et al (2009) Long-term temporal trends in cardiovascular and metabolic risk factors. Wien Klin Wochenschr 121(19–20):623–630
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2001) Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 106(25):3143–3421
Clarke R, Shipley M, Lewington S, Youngman L, Collins R, Marmot M, Peto R (1999) Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. Am J Epidemiol 150:341–353
Wood AM, White I, Thompson SG, Lewington S, Danesh J (2006) Regression dilution methods for meta-analysis: assessing long-term variability in plasma fibrinogen among 27, 247 adults in 15 prospective studies. Int J Epidemiol 35:1570–1578
Inoue M, Noda M, Kurahashi N et al (2009) Impact of metabolic factors on subsequent cancer risk: results from a large-scale population-based cohort study in Japan. Eur J Cancer Prev 18(3):240–247
Al-Azzawi F, Wahib M (2002) Estrogen and colon cancer: current issues. Climacteric 5(1):3–14
Crandall CJ (1999) Estrogen replacement therapy and colon cancer: a clinical review. J Womens Health Gend Based Med 9:1155–1166
Brunzell JD (2007) Clinical practice. Hypertriglyceridemia. N Engl J Med 357(10):1009–1017
Szatrowski TP, Nathan CF (1991) Production of large amounts of hydrogen peroxide by human tumor cells. Cancer Res 51(3):794–798
Kamata H, Hirata H (1999) Redox regulation of cellular signalling. Cell Signal 11(1):1–14
Warnick GR, Nakajima K (2008) Fasting versus nonfasting triglycerides: implications for laboratory measurements. Clin Chem 54(1):14–16
Yuan G, Al-Shali KZ, Hegele RA (2007) Hypertriglyceridemia: its etiology, effects and treatment. CMAJ 176(8):1113–1120
Acknowledgments
Funding sources of this study are World Cancer Research Fund International (WCRF International) 2007/2009 and the Austrian National Bank Grant OENB-12737 (to H.U.).
Conflict of interest
None declared
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Borena, W., Stocks, T., Jonsson, H. et al. Serum triglycerides and cancer risk in the metabolic syndrome and cancer (Me-Can) collaborative study. Cancer Causes Control 22, 291–299 (2011). https://doi.org/10.1007/s10552-010-9697-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-010-9697-0