Abstract
Introduction
The Ontario High Risk Breast Screening program follows women aged 30–69 at an increased risk of breast cancer, using a yearly mammography and breast MRI. The aim of this study is to determine the clinical outcomes for the enrolled women.
Methods
Observational cohort study following 2081 participants in the high-risk screening program 2011–2017. The participants were divided into three subgroup according to their risk criteria: (a) known carriers of pathogenic variants (PV) in hereditary breast cancer genes. (b) Previous chest radiotherapy. (c) Estimated life time risk (ELR) ≥ 25%, calculated using the International Breast Cancer Intervention Study (IBIS) tool, with no known mutation or previous radiation. All Breast Cancer (BC) diagnosed during the follow-up time were recorded.
Results
673 women carried PVs in hereditary breast cancer genes, 159 had a history of chest radiotherapy, and 1249 had an ELR ≥ 25%. The total cohort of screening years was 8126. Median age at BC diagnosis was 41 for the first group, 47 for the second group and 51 for the third. BC incidence rate was 18.2 for PV mutation carriers, 17.9 for the chest radiotherapy group and 6.2 for ELR ≥ 25%. Hazard ratio was similar for the first two groups, but significantly lower for the ELR ≥ 25% group. When stratifying by age, the incidence rate in the ELR ≥ 25% increased over time, until it became similar to that of the other subgroups after age 50.
Conclusion
Our findings question the need to screen women with an elevated lifetime risk using the same screening practices used for women who are PV mutation carriers, or with a history of chest radiation, prior to the age of 50.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radiologic screening for breast cancer (BC) is performed in asymptomatic patients with the goal of diagnosing the disease at an earlier stage. Mammography is the only method that has been shown to reduce mortality in randomized clinical trials [1,2,3,4]. In accordance with the goal of early diagnosis there have been specialized screening programs developed for high-risk populations. These programs address women with familial and personal risk factors for breast cancer using additional breast imaging modalities, starting at a younger age and at shorter intervals than the usual screening program that addresses the average–risk population.
Recommendations and guidelines for high-risk screening vary nationally and are largely based on expert panels. Most include women with known BRCA mutations or other less frequent pathogenic variants (PV) in hereditary breast cancer genes, history of chest radiation in childhood and adolescence, or an increased lifetime risk of breast cancer. The latter is defined to be 20–25% or higher as per the American College of Radiology (ACR), and calculated using risk assessment tools such as the Tyrer- Cruzik /IBIS or BOADICEA models [5]. Screening in the high-risk population usually starts between ages 25–30, and includes yearly mammography and supplementary breast magnetic resonance imaging (MRI) or breast ultrasound (for women that qualify for but cannot undergo MRI), with or without adjunct ultrasound [6,7,8,9].
The benefits of specialized screening for high risk women have been supported mostly by studies in BRCA mutation carriers, who are prone to be affected at a young age with high grade, more aggressive tumors [10,11,12,13]. Although studied less extensively, higher sensitivity and earlier stage at diagnosis have also been shown in women with a history of chest radiotherapy [14, 15]. There are some studies showing high risk screening to be of benefit for women with a familial risk of breast cancer without a known PV, however it does come at a cost as it increases the need for follow-up imaging and concomitant biopsies [16,17,18,19].
There is a paucity of data looking at the overall results for a specialized screening program in other high risk groups, and to the best of our knowledge there is no published data about the different subgroups currently eligible for high risk screening and stratification of their clinical outcome. The purpose of this study was to examine the differences in incidence and outcome of BC diagnosis between different cohorts within a large institutional high-risk breast screening program.
Patients and methods
The Ontario breast screening program for women at high risk for breast cancer
The screening program, which was established in 2011, addresses women ages 30–69 who are residents of Ontario, Canada with valid health insurance and fall into one of the following risk categories:
-
1.
Carriers of a PV which increases lifetime risk for breast cancer (e.g., BRCA1, BRCA2, TP53, PTEN, CDH1, NF, CHEK2, PALB2, ATM, STK11)
-
2.
History of radiation therapy to the chest to treat another cancer or condition (e.g., Hodgkin lymphoma) before age 30 and at least 8 years prior to starting screening
-
3.
Have a 25% or greater Estimated Lifetime Risk (ELR) using the IBIS or BOADICEA tools, based on personal or family history, through a genetics assessment.
-
3.1
Do not qualify for genetic testing, or underwent genetic testing but no known PV has been identified.
-
3.1
-
4.
First-degree relatives of a PV carrier that had genetic counseling and chose not to undergo genetic testing
Women who qualify based on one of these criteria and have a history of breast or ovarian cancer are eligible for participation or return to the program once they are back to their routine screening. Participants who underwent bilateral mastectomy, either prophylactic or therapeutic, are excluded from the program.
The screening includes annual breast MRI and two-view each breast full field digital mammography. Screening ultrasound is performed routinely only for women who cannot undergo MRI (i.e., ocular metal implants, claustrophobia, etc.). Participants in our institution could also undergo mammography with digital breast tomosynthesis when breast MRI was not performed.
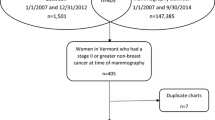
Study cohort
The study was approved by the institutional review board at the University Health Network, Toronto (UHN), Ontario.
A total of 2147 women were screened at the UHN Princess Margaret Cancer Center, a tertiary care cancer center in Ontario, Canada, between December 2011 and January 2018. Inclusion in the program was in accordance with the aforementioned Ontario Breast Screening Program for High Risk Women guidelines. To be included in the study cohort, participants had to undergo at least one round of screening.
The participants’ data was entered into a Microsoft Excel Data base, which was created and updated by the program's nurse navigator. A record was created for each participant upon joining the program, and they were tracked and managed through the screening, and if applicable, cancer treatment trajectory, return to screening or until completion of mastectomies or palliation. The database was used to capture patient’s demographics, screening duration and high risk criteria, as well as cancer diagnosis. Additional information was retrieved from the patients’ charts as needed. Imaging data was obtained from charts. Breast imaging studies were reported by a heterogeneous population of breast radiologists, all board certified and breast imaging fellowship trained. Screening double reading was not performed as per Ontario Breast Screening Program.
Study design
Three subgroups were identified in the cohort, based on the high-risk program inclusion criteria:
-
1.
Patients with PV in hereditary breast cancer genes
-
2.
Patients with a history of chest radiotherapy
-
3.
Women with an ELR of 25% or greater without an identified PV in hereditary breast cancer genes. In our cohort, all the ELR’s were calculated using the IBIS (Tyrer-Cuzick model).
The group of women who were untested first-degree relatives of known PV carriers were excluded from this study, as their lifetime risk was not quantified (66 patients).
In the ELR group, the calculated lifetime risk was documented, as well as the reason for inclusion in the high-risk program. The IBIS score was calculated once at the time of entering the program. All patients in this group met one of these three criteria:
-
1.
Strong family history of breast cancer
-
2.
Personal history of high risk lesions i.e., atypical hyperplasia or Lobular Carcinoma In Situ (LCIS)
-
3.
Both family history and personal history of high risk lesion(s)
Information collected for all participants included age joining the program, high risk criteria, breast cancer diagnosis characteristics including size (as recorded on specimen histopathology), clinical and pathological stage, histology, and mortality (breast cancer related or other).
Statistical analysis
The number of screening years was calculated for each woman. Every 12 months period following an annual imaging test counted as one screening year. Call backs for short term follow-up imaging (less than one year from previous imaging) were not counted.
Breast cancer incidence rate is the number of cases per 1000 screening years. Hazard ratios were calculated using a proportional hazards Cox Regression Model, which was adjusted for age. In addition, the cumulative incidence rates of BC in the PV carriers and the ELR ≥ 25% groups was stratified by age group (≤ 39, 40–49, 50–59, ≥ 60). Gray’s test was used for comparing cumulative incidence [20]. p values < 0.05 were considered significant.
Statistical analyses were conducted using SAS version 9.4 (SAS Institute, NC, USA).
Results
Participants and outcome
A total of 2081 women fitting the inclusion criteria were followed September 2011 to January 2018. Median age entering the program was 43 years old (range 25–72). Median screening years per participant was four years, and the total screening years was 8126.
During the follow-up period 89 breast cancers were diagnosed in 86 women; 88 were screening detected, and one was an interval cancer in a BRCA2 patient who was undergoing mammography with adjunctive screening ultrasound, due to contraindications to MRI.
The majority (66%) of the BC were diagnosed based on findings seen solely on MRI, 28% were seen on both MRI and mammography, and 6% were seen only on mammography. Of the BC seen only on mammography, 3 were DCIS and 2 were IDC. Table 1 details the imaging modality used for diagnosis by risk groups and age.
Sixty-two (70%) of the 89 BCs were invasive, with the median size of 0.9 cm, correlating with a pT1b stage (range 0.14–3.3 cm). Fifty-five cases (62%) were cT1 at diagnosis, and additional 7 (8%) were cT2. No cT3 or cT4 cancers were diagnosed in the cohort. The remaining 27 (30%) cases were Ductal Carcinoma in Situ (DCIS), with the average size of 2.76 cm. All sizes were recorded based on final specimen histopathology. DCIS accounted for almost a quarter of BC cases in the PV carriers and previous chest radiation groups (24% and 23%), and for 43% of the BC cases in the ELR ≥ 25%.
Four patients had positive lymph nodes at diagnosis (6.5% of invasive BC): two with pN1mi, and two patients with pN1a disease.
Thirty-eight women died during the follow-up period. Four deaths were breast cancer related, all in patients with a history of breast cancer prior to joining the screening program. Twenty-nine (76%) deaths were ovarian cancer related, all in BRCA mutation carriers. There was one case each of acute myeloid leukemia, pancreatic carcinoma, gastric carcinoma, myelofibrosis and one unknown cause.
Table 2 displays the participants and outcome covariates within the three high-risk subgroups.
Subgroup analysis
The 8-year cumulative incidence for BC (Fig. 1) was 13.2% for the PV carriers group (95% CI, 9.4–18.4%), 13.4% for the previous chest radiotherapy group (95% CI, 7.4–24.4%), and 4.7% for the ELR ≥ 25% (95% CI, 3.1–7.2%). No significant difference in cumulative incidence was found between the PV carriers and the chest radiotherapy group, however the cumulative incidence in the ELR ≥ 25% group was significantly lower than the other two groups (P < 0·0001).
The hazard ratio (HR) comparing the subgroups and adjusting for age showed no difference between the PV carriers and the chest radiotherapy group (HR 0.91, 95% CI 0.49–2.05). The HR for ELR ≥ 25% was significantly lower than both the PV (HR 0.36, 95% CI 0.22–0.60) and the chest radiation (HR 0.33, 95% CI 0.18–0.63) groups.
Analysis of estimated lifetime risk ≥ 25% subgroup
Median estimated lifetime risk was 29% for the whole group (1249 women). For unaffected participants (1219 women) the median ELR was 29% (range 25%–92.8%). For the affected participants (30 women) the median ELR was 31·5% (range 25%–64%).
In quantile regression, no difference was found between the lifetime risk calculated in the affected and the unaffected group (P = 0.25), showing that higher estimated lifetime risk of cancer did not correlate with higher incidence of BC for this cohort.
Table 3 shows the reasons for referral to the high-risk program. Due to the overall low cumulative incidence of BC in the group, Gray’s Test for Equality of Cumulative Incidence was not calculated. However as shown in Table 3, the participants with high-risk lesions (i.e., Atypical lobular or ductal hyperplasia, or LCIS) had a higher average ELR than the family history group (40% vs. 28%), while they had a lower incidence of BC over the study period (incidence rate 2.33 vs. 6.66).
Stratification by age
When stratifying by age, the difference in the cumulative incidence between the PV group and the ELR ≥ 25% for women under the age of 50 remained significant (P < 0.0001). However, for women older than 50, the groups became closer their cumulative incidence (P = 0.47) (Table 4 and Fig. 2).
Stratification by age was done only for the PV carriers and ELR groups, as the chest radiotherapy group was small, and most patients in it were under the age of 50.
Discussion
For this cohort of high risk patients, the screening goals of diagnosis at an early stage and reduction of late stage diagnosis were achieved. Most (62%) breast cancers were diagnosed at stage I (T1bN0), with the highest stage at diagnosis being stage II. This finding is in accordance with results reported from other population based high risk screening programs [10, 11, 15, 17, 18]. These results are even more favorable in terms of early detection when considering that only 42.9% of invasive BC cases are diagnosed at stage I in Ontario, Canada in the general population [21].
While the majority of the participants (60%) enrolled in the high risk screening program due to an ELR ≥ 25%, they had the lowest BC incidence of all the high risk groups. Further analysis of the ELR ≥ 25% subgroup showed that it is a heterogeneous group, including mostly women with familial history of BC but also women with personal history of benign high-risk lesions. Interestingly, a higher estimated lifetime risk (as estimated by the IBIS tool) did not correlate with a higher incidence of BC in this cohort. This was most evident in the group of women with previous high-risk lesions, who had a high estimated lifetime risk but a low BC incidence rate. One possible reason is the nature of the IBIS risk estimation model; when compared with other risk prediction models, IBIS was less likely to underestimate the risk of breast cancer [22]. However this does come at the price of overestimation in women at the high quantiles of familial risk [23, 24] and in women with lobular carcinoma in situ [25]. These findings are further supported by a recent study showing lower than previously reported 10 year incidence of breast cancer after diagnosis of atypical ductal hyperplasia [26].
It has been suggested that defining women as high risk based on their 10-year threshold, rather than lifetime risk, leads to better risk discrimination [27]. This may pose logistical challenges, with possible participants undergoing more frequent risk calculations to remain in the program. However, such an approach may also result in less overestimation and therefore make for better use of the high-risk program resources.
Another possible explanation for the observed low incidence rate of BC in the ELR ≥ 25% group is the relatively short follow-up time and the fact that our cohort included only women up to age 70. Although it is highly possible that the higher incidence of BC in this group manifests at an older age, our finding raises the question whether women with ELR ≥ 25% should have high risk screening starting at the same young age as the other high risk groups.
When stratifying the BC incidence by age, a dramatic effect was seen in the ELR group, while BC incidence remained relatively stable in the PV carriers group. Prior to age 40, the incidence was tenfold higher in the PV group (1.7 vs. 16%). For ages 40–50 the BC incidence in the ELR group more than doubled to 5.8, and starting at age 50 it became statistically similar to the PV carriers group. A similar effect of age on BC incidence was shown in a recent meta-analysis by Phi X.A. et al., which looked at women with strong family history of BC and no known gene mutation, and showed the incidence rate to double with every decade, until reaching rates similar to those reported in PV carriers in women aged 50–60 [17].
In our cohort, median age at BC diagnosis in the ELR ≥ 25% group was 51, 10 years younger than the median age reported for the general population in the SEER database [28]. It is worth noting that median age of 51 at diagnosis would mean that even if not included in a high risk screening program, a big proportion of these women would be screened by at least a mammogram if they participated in the average-risk screening program Ontario Breast Screening program.
Almost half of the patients in the ELR ≥ 25% group were diagnosed with DCIS (43%), in comparison with 23–24% in the other two groups. This raises the concern of potential over-diagnosis, for which the oncological benefit is unknown.
Our study has a number of limitations. First, it is a retrospective study, which by nature is related to at least some degree of selection bias. Another limitation is that the lifetime risk estimation by the IBIS tool was done only once at the time of enrollment, and not updated thereafter.
Since the study cohort was based on the Ontario criteria for high risk screening, the results might not be generalizable to other high risk screening programs. For example, in our program all patients with an ELR ≥ 25% are eligible for participation starting age 30, while NCCN guidelines suggest screening for participants with family history starting 10 years before the age of the youngest affected family member, and not earlier than 30 [8]. MRI follow-up for high risk women with a personal history of breast cancer is also routinely practiced in our program, but is considered of undefined role by the NCCN guidelines [29].
Other limitations include a relatively short follow-up time (maximum of 8 years). The groups were also not equal in size, with the subgroup of women who had a history of chest radiotherapy being especially small in comparison with the others. There is no information about the outcome of women after the age of 70, who are no longer eligible for participation in the screening program. However, these data do provide insight into the outcomes of over 2000 women who underwent high risk screening and suggest that not all patients in these programs have similar risk. As such, personalization of screening may be advantageous in order to decrease the risk of over-investigations while still maximizing the benefits of early detection.
Conclusion
The group of women with an ELR of ≥ 25 without a known PV or history of chest radiotherapy differ from the other subgroups in BC incidence, hazard ratio and age at diagnosis. Key features of high-risk screening—such as age at imaging initiation, optimal imaging modalities and screening intervals- should not be applied to this group based on data from other, better studied, risk groups.
The data presented here shows the yield of high-risk screening in women with ELR ≥ 25% prior to the age of 50 is much lower than the other risk groups, and their calculated risk is highly overestimated. However, it is of value to introduce high risk screening to this group after the age of 50, once their BC risk becomes similar to that of other high-risk groups.
References
Saadatmand S, Bretveld R, Siesling S, Tilanus-Linthorst MM (2015) Influence of tumour stage at breast cancer detection on survival in modern times: population based study in 173 797 patients. BMJ 6(351):h4901
Myers ER, Moorman P, Gierisch JM, Crowley MJ, McCrory DC, Kendrick A et al (2015) Benefits and harms of breast cancer screening: a systematic review. Jama 314(15):1615–34
Paci E (2012) Summary of the evidence of breast cancer service screening outcomes in Europe and first estimate of the benefit and harm balance sheet. J Med Screen 19(1_suppl):5–13
Nyström L, Bjurstam N, Jonsson H, Zackrisson S, Frisell J (2017) Reduced breast cancer mortality after 20+ years of follow-up in the Swedish randomized controlled mammography trials in Malmö, Stockholm, and Göteborg. J Med Screen 24(1):34–42
Monticciolo DL, Newell MS, Moy L, Niell B, Monsees B, Sickles EA (2018) Breast cancer screening in women at higher-than-average risk: recommendations from the ACR. J Am Coll Radiol 15(3):408–414
Mann RM, Balleyguier C, Baltzer PA et al (2015) Breast MRI: EUSOBI recommendations for women’s information. Eur Radiol 25(12):3669–3678
National Collaborating Centre for Cancer (UK) (2013) Familial breast cancer: classification and care of people at risk of familial breast cancer and management of breast cancer and related risks in people with a family history of breast cancer. National Collaborating Centre for Cancer (UK), Cardiff UK
National Comprehensive Cancer Network, Breast Cancer Screening and Diagnosis (version 1.2019) https://www.nccn.org/professionals/physician_gls/pdf/breast-screening.pdf. Accessed 2/7/2019
Cancer Care Ontario, Ontario Breast Screening Program Information for Healthcare Providers; October 2015 https://www.cancercareontario.ca/sites/ccocancercare/files/assets/OBSPHealthcareProviders.pdfAccessed 2/7/2019
Lowry KP, Lee JM, Kong CY et al (2012) Annual screening strategies in BRCA1 and BRCA2 gene mutation carriers: a comparative effectiveness analysis. Cancer 118(8):2021–2030
Passaperuma K, Warner E, Causer PA et al (2012) Long-term results of screening with magnetic resonance imaging in women with BRCA mutations. Br J Cancer 107(1):24
Warner E, Hill K, Causer P et al (2011) Prospective study of breast cancer incidence in women with a BRCA1 or BRCA2 mutation under surveillance with and without magnetic resonance imaging. J Clin Oncol 29(13):1664
Gareth ED, Nisha K, Yit L et al (2014) MRI breast screening in high-risk women: cancer detection and survival analysis. Breast Cancer Res Treat 145(3):663–72
Freitas V, Scaranelo A, Menezes R, Kulkarni S, Hodgson D, Crystal P (2013) Added cancer yield of breast magnetic resonance imaging screening in women with a prior history of chest radiation therapy. Cancer 119(3):495–503
Tieu MT, Cigsar C, Ahmed S et al (2014) Breast cancer detection among young survivors of pediatric Hodgkin lymphoma with screening magnetic resonance imaging. Cancer 120(16):2507–2513
Saadatmand S, Geuzinge HA, Rutgers EJ et al (2019) MRI versus mammography for breast cancer screening in women with familial risk (FaMRIsc): a multicentre, randomised, controlled trial. Lancet Oncol. 20:1136–1147
Phi XA, Houssami N, Hooning MJ et al (2017) Accuracy of screening women at familial risk of breast cancer without a known gene mutation: Individual patient data meta-analysis. Eur J Cancer 1(85):31–38
Bick U, Engel C, Krug B et al (2019) High-risk breast cancer surveillance with MRI: 10-year experience from the German consortium for hereditary breast and ovarian cancer. Breast Cancer Res Treat 175(1):217–228
Kuhl C, Weigel S, Schrading S et al (2010) Prospective multicenter cohort study to refine management recommendations for women at elevated familial risk of breast cancer: the EVA trial. J Clin Oncol 28(9):1450–1457
Gray RJ (1988) A class of K sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16(3):1141–1154
Canadian Cancer Statistics Advisory Committee. Canadian Cancer Statistics 2018. Toronto, ON: Canadian Cancer Society; June 2018. https://www.cancer.ca/Canadian-Cancer-Statistics-2018-EN. Accessed 2/7/2019
Amir E, Freedman OC, Seruga B, Evans DG (2010) Assessing women at high risk of breast cancer: a review of risk assessment models. JNCI 102(10):680–91
Terry MB, Liao Y, Whittemore AS et al (2019) 10-year performance of four models of breast cancer risk: a validation study. Lancet Oncol 20(4):504–517
Brentnall AR, Cuzick J, Buist DS, Bowles EJ (2018) Long-term accuracy of breast cancer risk assessment combining classic risk factors and breast density. JAMA Oncol 4(9):e180174
Lo LL, Milne RL, Liao Y, Cuzick J, Terry MB, Phillips KA (2018) Validation of the IBIS breast cancer risk evaluator for women with lobular carcinoma in-situ. Br J Cancer 119(1):36
Menes TS, Kerlikowske K, Lange J, Jaffer S, Rosenberg R, Miglioretti DL (2017) Subsequent breast cancer risk following diagnosis of atypical ductal hyperplasia on needle biopsy. JAMA Oncol 3(1):36–41
Quante AS, Whittemore AS, Shriver T, Hopper JL, Strauch K, Terry MB (2015) Practical problems with clinical guidelines for breast cancer prevention based on remaining lifetime risk. J Natl Cancer Inst. 107(7):djv124. https://doi.org/10.1093/jnci/djv124
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Table 1.11 Median Age of Cancer Patients at Diagnosis, 2012–2016. https://seer.cancer.gov/csr/1975_2016/results_single/sect_01_table.11_2pgs.pdf#search=median%2520age%2520at%2520diagnosis. Accessed 2/7/2019
National Comprehensive Cancer Network, Breast Cancer (version 3.2020) https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf Accessed 20/3/20
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hermann, N., Klil-Drori, A., Angarita, F.A. et al. Screening women at high risk for breast cancer: one program fits all?. Breast Cancer Res Treat 184, 763–770 (2020). https://doi.org/10.1007/s10549-020-05895-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05895-w