Abstract
Purpose
Previous studies suggest that coffee and caffeine intake may be associated with reduced breast cancer risk. We investigated the association of coffee and caffeine intake with mammographic breast density by woman’s menopausal status and, in postmenopausal women, by hormone therapy (HT).
Methods
This study included 4130 cancer-free women within the Nurses’ Health Study and Nurses’ Health Study II cohorts. Percent breast density (PD) was measured from digitized film mammograms using a computer-assisted thresholding technique and square root-transformed for the analysis. Average cumulative coffee/caffeine consumption was calculated using data from all food frequency questionnaires preceding the mammogram date. Information regarding breast cancer risk factors was obtained from questionnaires closest to the mammogram date. We used generalized linear regression to quantify associations of regular, decaffeinated, and total coffee, and energy-adjusted caffeine intake with percent density.
Results
In multivariable analyses, decaffeinated coffee was positively associated with PD in premenopausal women (2+ cups/day: β = 0.23, p trend = 0.03). In postmenopausal women, decaffeinated and total coffee were inversely associated with PD (decaffeinated 2+ cups/day: β = − 0.24, p trend = 0.04; total 4+ cups/day: β = − 0.16, p trend = 0.02). Interaction of decaffeinated coffee with menopausal status was significant (p-interaction < 0.001). Among current HT users, regular coffee and caffeine were inversely associated with PD (regular coffee 4+ cups/day: β = − 0.29, p trend = 0.01; caffeine 4th vs. 1st quartile: β = − 0.32, p trend = 0.01). Among past users, decaffeinated coffee was inversely associated with PD (2+ cups/day β = − 0.70, p trend = 0.02).
Conclusions
Associations of decaffeinated coffee with percent density differ by woman’s menopausal status. Associations of regular coffee and caffeine with percent density may differ by HT status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mammographic breast density is a well-established and strong predictor of breast cancer risk [1]. Appearance of the breast on the mammogram is a reflection of the amount of fat, connective tissue, and epithelial tissue in the breast [2]. Light (non-radiolucent) areas on the mammogram represent the fibrous and glandular tissues (“mammographically dense”), whereas the dark (radiolucent) areas are primarily fat. Women with breasts of ≥ 75% density (proportion of the total breast area that appears dense on the mammogram) are at fourfold to sixfold greater risk of breast cancer compared to women with more fat tissues in the breasts [1].
A few previous studies have suggested that coffee and caffeine intake may be associated with reduced breast cancer risk [3,4,5,6]. Some of the suggested mechanisms explaining these associations included changes in bioavailable estrogen, antioxidative properties of coffee constituents, and changes in DNA methylation and cellular differentiation [7,8,9,10,11,12,13]. To date, there is limited epidemiologic evidence that diet has a strong influence on mammographic density [14,15,16,17]. The only study that examined the associations between caffeine intake and percent breast density (Minnesota breast cancer family study) found no associations [18]. In addition to the very limited evidence on the association between coffee and caffeine consumption and breast density, it is unknown if there is an interaction between postmenopausal hormone use and caffeine intake in relation to breast density. Postmenopausal hormones have been shown to consistently increase mammographic breast density [19,20,21,22]. As coffee has stimulating effects on variety of enzymes, including those involved in estrogen and xenobiotic metabolism [11], it is possible that the effect of postmenopausal hormones on breast density could potentially be modified by the coffee consumption. To address these knowledge gaps, we examined the associations of coffee and caffeine intake with percent breast density in healthy pre- and postmenopausal women using prospective data from the Nurses’ Health Study and Nurses’ Health Study II cohorts. The associations in postmenopausal women were further examined separately by woman’s hormone therapy (HT) status.
Methods
Study population
Women included in this study were selected from participants of the nested case–control study within Nurses’ Health Study (NHS) and Nurses’ Health Study II (NHSII) cohorts. These prospective cohorts followed registered nurses in the United States who were 30–55 years (NHS) or 25–42 years old (NHSII) at enrollment. After administration of the initial questionnaire, the information on breast cancer risk factors and any diagnoses of cancer or other diseases was updated through biennial questionnaires [2, 23].
A nested case–control approach was originally used to examine the association between selected biomarkers and breast cancer risk within the NHS and NHS II [2, 24]. Using incidence density sampling, women without cancer history (other than non-melanoma skin cancer) at the time of the case’s cancer diagnosis (controls) were matched 1:1 or 1:2 with women diagnosed with in situ or invasive breast cancer (cases) on age at the time of blood collection, menopausal status, and postmenopausal hormone use (current vs. not current) at blood draw, and day/time of blood draw; for NHS II, additional matching included race/ethnicity and day in the luteal phase [25]. Our analysis included controls from this nested case–control study as well as additional women within NHSII cohort without a history of any cancer other than non-melanoma skin who were not included in the original nested breast cancer case–control study. We attempted to obtain mammograms closest to the time of blood collection (or ~ 1997 for those who did not provide blood samples). From all eligible women, 4342 women provided consent and had a usable mammogram for density estimation. Of these women, 4130 (95%) had data on coffee and caffeine intake. This study was approved by the Institutional Review Board at the Brigham and Women’s Hospital. Consent was obtained or implied by return of questionnaires.
Dietary assessment
Usual dietary intake and coffee consumption during the past year were assessed with a semi-quantitative food frequency questionnaire (FFQ) with approximately 130 items which was included in the 1991, 1995, 1999, 2003, and 2007 questionnaires for NHSII [26]. In NHS, information on diet within the preceding 1 year was first collected with 61-item FFQ in 1980 and then expanded to 116 items in 1984, 1986, 1990, 1994, and 1998 [27]. Responses on both NHS and NHSII FFQs were recorded in nine categories of intake frequency ranging from “never or less than once per month” to “six or more per day”. Caffeine intake was derived from self-reported intakes of coffee, soda, tea, and chocolate by multiplying the frequency of consumption of each item by their caffeine content per serving and then summing across all items, as previously described [7].
We separately examined the associations with regular coffee, decaffeinated coffee, total coffee, and caffeine intake. Average cumulative coffee and caffeine intake were calculated using data available from all the questionnaires preceding the mammogram date. Consistent with previous studies in these cohorts [7], coffee consumption categories were defined as ≤ 6 cups/week, 1 cup/day, 2–3 cups/day, and 4+ cups/day. Decaffeinated coffee was categorized as ≤ 1–3 cups/month, 1–6 cups/week, 1 cup/day, and 2+ cups/day. Energy-adjusted caffeine intake was modeled as quartiles based on the distribution among pre- and postmenopausal women (premenopausal: < 94 mg, 94 to < 224 mg, 224 to < 383 mg, and ≥ 383 mg; postmenopausal: < 134 mg, 134 to < 262 mg, 262 to < 400 mg, and ≥ 400 mg). In a secondary analysis, we also explored the associations of recent consumption (preceding and closest to the mammogram date) with percent mammographic density.
Assessment of mammographic breast density
To quantify mammographic density, the craniocaudal views of both breasts for all mammograms in the NHS and for the first two batches of mammograms in the NHSII were digitized at 261 μm per pixel with a Lumisys 85 laser film scanner (Lumisys, Sunnyvale, California). The third batch of NHSII mammograms was digitized using a VIDAR CAD PRO Advantage scanner (VIDAR Systems Corporation; Herndon, VA) and comparable resolution of 150 dots per inch and 12 bit depth). The Cumulus software (University of Toronto, Toronto, Canada) was used for computer-assisted determination of the percent mammographic density on all mammograms [2, 28]. As reported previously, the measure of breast density from NHS mammograms was highly reproducible (within-person intraclass correlation coefficient = 0.93) [2]. All NHSII images were read by a single reader. Although within batch reproducibility was high (intraclass correlation coefficient ≥ 0.90) [29], density measures varied across the NHSII batches. We included a small subset of identical mammograms in all batches to account for batch drift in density measurement readings. The density measures from the second and third batches of NHSII mammograms were adjusted to account for the batch effect (whether due to intra-reader variability or scanner), as previously described [30]. Additionally, to assess the potential variability in percent density by scanner, we conducted a pilot study of 50 mammograms. These mammograms were scanned using both the Lumysis 85 laser scanner and the VIDAR CAD PRO Advantage scanner. The correlation between percent density as measured by the same observer from the two scanners was 0.88.
Percent breast density was measured as percentage of the total area occupied by epithelial/stromal tissue (absolute dense area) divided by the total breast area. Because breast densities of the right and left breast for an individual woman are strongly correlated [28], the average density of both breasts was used in this analysis.
Covariates
Information on breast cancer risk factors was obtained from the biennial questionnaires closest to the date of the mammogram. Women were considered to be postmenopausal if they reported: (1) no menstrual periods within the 12 months before blood collection with natural menopause, (2) bilateral oophorectomy, or (3) hysterectomy with one or both ovaries retained, and were 54 years or older for ever smokers or 56 years or older for never smokers [31, 32].
Statistical analysis
We used generalized linear regression to examine the associations of coffee and caffeine intake with percent density. Because percent mammographic density was non-normally distributed, we used square root transformation to improve normality in all the regression analyses. The lowest intake category for each of the exposures was used as the reference. The regression estimates were adjusted for age (continuous), body mass index (continuous), age at menarche (< 12, 12–13, > 13 years), parity and age at first child’s birth (nulliparous, parous with age at first birth < 25 years, and parous with age at first birth of ≥ 25 years), a confirmed history of benign breast disease (yes, no), a family history of breast cancer (yes, no), alcohol consumption (0, 0 to < 5, ≥ 5 g/day, unknown), study cohort, and in postmenopausal women also for hormone therapy (none, current, past, past with unknown current) and age at menopause (< 46, 46 to < 50, 50 to < 55, ≥ 55, unknown). In a secondary analysis, among current HT users the regression estimates were additionally adjusted for duration of HT.
To assess the overall trend for each of the exposure variables, we used respective medians within each category. For coffee consumption, the intake frequencies were first converted into servings and then the median servings in each quartile were used in the trend analysis. Differences in the associations of exposure variables with breast density by menopausal status were evaluated with two-way interactions and using Wald Chi square test. We used respective medians within each of the exposure categories to model the interaction. The same approach was used to test interactions of exposure variables with HT among postmenopausal women. Statistical significance in all the analyses was assessed at 0.05 level. The analyses were performed using SAS software (version 9.2, SAS Institute, Cary, NC, USA).
Results
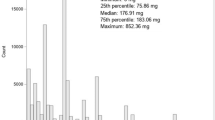
In this study of 4130 cancer-free women, the average age at the mammogram was 53 years (range 30–84). Of these women, 1823 were premenopausal and 2307 were postmenopausal. Pre- and postmenopausal women in the highest caffeine intake quartile had a mean percent density of 37.4 and 25.5%, respectively, as compared with 40.6 and 26.2% in women from the lowest quartile. Distributions of breast cancer risk factors by the quartiles of caffeine intake in pre- and postmenopausal women are presented in Table 1. Women in the highest quartile of caffeine intake as compared with the lowest quartile consumed more alcohol, where less likely to have a history of benign breast disease, and in postmenopausal women, less likely to be currently on HT. Premenopausal women in the highest caffeine quartile had greater BMI as compared with women in the lowest quartile. Distributions of other risk factors were similar across the caffeine intake quartiles.
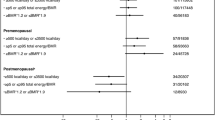
In multivariable analysis, decaffeinated coffee was positively associated with percent density in premenopausal women (β = 0.19 for 1 cup/day and β = 0.23 for 2+ cup/day; p trend = 0.03) (Table 2). In a secondary analysis with untransformed percent density, drinking 2 and more cups of decaffeinated coffee was associated with 2.6% increase in percent density. Regular and total coffee consumption and caffeine intake were not associated with percent breast density. The risk estimates for regular and decaffeinated coffee remained similar after mutually adjusting for these two variables (data not shown).
In postmenopausal women, decaffeinated and total coffee consumption were inversely associated with percent breast density (decaffeinated coffee: β = − 0.12 for 1 cup/day and β = − 0.24 for 2+ cups/day, p trend = 0.04, p-interaction with menopausal status < 0.001; total coffee: β = − 0.17 for 2–3 cups/day and β = − 0.16 for 4+ cups/day, p trend = 0.02) (Table 2). In a secondary analysis with untransformed percent density, drinking 2 and more cups/day of decaffeinated coffee was associated with 2.4% decrease in percent density and intake of 4 and more cups of total coffee per day was associated with 1.2% decrease in percent density. We found a marginal inverse association of caffeine intake with percent density (p = 0.10). The risk estimates for regular and decaffeinated coffee remained similar after mutually adjusting for these two variables (data now shown). We found no interactions of regular and total coffee as well as caffeine intake with menopausal status (p-interaction > 0.05 for all).
In the stratified analysis by woman’s HT status, none of the exposure variables were associated with percent breast density among women with no HT (Table 3). Among current postmenopausal hormone users, regular coffee and caffeine intake were inversely associated with percent density (regular coffee: β = − 0.37 for 2–3 cups/day and β = − 0.29 for 4+ cups/day, p trend = 0.01; caffeine intake: β = − 0.20 for 3rd quartile and β = − 0.32 for 4th quartile, p trend = 0.01). These associations remained similar after additional adjustment for HT duration (data not shown). In a secondary analysis with untransformed percent density among current HT users, drinking 2–3 cups of regular coffee per day was associated with 3.8% decrease in percent density and drinking 4 or more cups per day was associated with 2.9% decrease in percent density. In this analysis, the highest caffeine intake quartile was associated with 3.3% decrease in percent density.
Among past hormone users, decaffeinated coffee was inversely associated with percent density (β = − 0.45 for 1 cup/day and β = − 0.70 for 2+ cups/day, p trend = 0.02). In a secondary analysis with untransformed percent density among past HT users, drinking 1 cup of decaffeinated coffee per day was associated with 4% decrease in percent density and drinking 2 and more cups of decaffeinated coffee was associated with 6% decrease in percent density. We found no interactions of coffee and caffeine intake with the status of HT.
In a secondary analysis examining recent coffee and caffeine intake, the findings were similar (data not shown).
Discussion
In this study of cancer-free women, we investigated the associations of coffee consumption and caffeine intake with mammographic percent density in pre- and postmenopausal women and by the woman’s HT status. Decaffeinated and total coffee intakes were inversely associated with percent density in postmenopausal women and decaffeinated coffee intake was positively associated with percent density in premenopausal women. Inverse associations of regular coffee and caffeine with percent density were limited to current hormone users. Our findings contribute to the very limited evidence on the association of coffee and caffeine intake with breast density.
The only previous study that examined association between caffeine consumption and breast density among 1508 cancer-free women participating in the Minnesota Breast Cancer Family Study (MBCFS), found no statistically significant association overall and when stratified by menopausal status [18]. In contrast, we observed inverse associations of total and decaffeinated coffee intake with percent breast density among postmenopausal women and a positive association of decaffeinated coffee with percent density in premenopausal women. Several aspects of study design and methods could potentially explain inconsistencies in the findings between the two studies. First, our study had considerably larger sample size and included 4130 women (1823 pre- and 2307 postmenopausal) in contrast to 1508 women in MBCFS (81.2% postmenopausal) thus substantially improving our statistical power in both overall and stratified analysis. MBCFS utilized a cross-sectional design with a single measure of caffeine intake while our study was prospective in nature and measured coffee and caffeine intake at multiple time points before the mammogram date thus allowing us to calculate cumulative average exposure measures. Next, two studies differed with respect to breast density estimation. In MBCFS, breast density was estimated visually by a radiologist from the mediolateral oblique view in contrast to computer-assisted density estimation from the craniocaudal views in our study. As the authors of MBCSF noted in their discussion, the study had a smaller proportion of women with dense breasts as compared with other studies as the result of using breast density estimation from mediolateral views which produces systematically lower density estimates as compared with craniocaudal views [18]. Further, the two studies differed with respect to statistical methods, including analytical approach and covariates used for adjustment. As individuals in MBCSF did not represent independent observations, the study implemented bootstrapping procedure to account for the family-based sampling design in which generalized linear models were used for each randomly selected sample followed by the use of standard errors and the pooled parameter estimate for hypothesis testing. In addition, unlike our study, the density measures were not transformed in MBCSF. Finally, multivariate models from MBCSF included smoking. As caffeine has been shown to be positively correlated with smoking [33,34,35], this approach may have resulted in over-adjustment and attenuation of the effects.
In the stratified analysis by hormone therapy status, we noted an inverse association of regular coffee and caffeine intake with percent density and, among past users, an inverse association of decaffeinated coffee with percent density. Previous studies consistently show increase in breast density in HT users [19,20,21,22]. Even though we did not find any statistically significant interactions of regular coffee and caffeine intake with HT, our findings suggest that simultaneous intake of coffee might reduce the effect of HT on breast density which could potentially have implications for breast cancer prevention.
Several biological mechanisms were suggested as a possible explanation for potential effects of coffee and caffeine on breast cancer risk and breast density, including an influence on circulating estrogen levels and bioavailable estrogen [7,8,9], antioxidative potential due to a high content of wide variety of phytochemicals [10], stimulating effects on variety of enzymes, including those involved in estrogen and xenobiotic metabolism [11], and inhibition of DNA methylation [12] all of which eventually can disrupt normal cell proliferation and differentiation.
Our study is the largest study to date that systematically investigated associations of coffee and caffeine intake with mammographic breast density by menopausal status. We examined, for the first time, these associations in postmenopausal women by the status of HT. The analysis used data from the NHS and NHSII cohorts with more than 25 years of follow-up, ascertainment of disease status, and comprehensive information on breast cancer risk factors and breast density.
Our study has a few limitations. The examined associations are based on the density measures from a single mammogram which might not be reflective of the woman’s life-long density pattern; however, studies have suggested that a single measure can predict breast cancer risk for up to 10 years in both pre- and postmenopausal women [36, 37]. Despite the prospective nature of the cohort, potential errors in recall of coffee consumption are possible. However, previous validation studies suggest that reasonable reproducibility and validity of the data from food frequency questionnaires for the use in studies of associations between diet and health outcomes in epidemiologic studies [38, 39].
In conclusion, we investigated the associations of coffee and caffeine intake with percent mammographic density. Our findings suggest that inverse associations of decaffeinated and total coffee intake with mammographic percent density in postmenopausal women and a positive association of decaffeinated coffee with percent density in premenopausal women. Our results also suggest that these associations may differ by woman’s HT status. If these association patterns are confirmed in subsequent studies, then the finding may translate into important public health messages for women using HT.
References
McCormack VA, dos Santos Silva I (2006) Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomark Prev 15(6):1159–1169
Tamimi RM, Byrne C, Colditz GA, Hankinson SE (2007) Endogenous hormone levels, mammographic density, and subsequent risk of breast cancer in postmenopausal women. J Natl Cancer Inst 99(15):1178–1187
Baker JA, Beehler GP, Sawant AC, Jayaprakash V, McCann SE, Moysich KB (2006) Consumption of coffee, but not black tea, is associated with decreased risk of premenopausal breast cancer. J Nutr 136(1):166–171
Lowcock EC, Cotterchio M, Anderson LN, Boucher BA, El-Sohemy A (2013) High coffee intake, but not caffeine, is associated with reduced estrogen receptor negative and postmenopausal breast cancer risk with no effect modification by CYP1A2 genotype. Nutr Cancer 65(3):398–409
Oh JK, Sandin S, Strom P, Lof M, Adami HO, Weiderpass E (2015) Prospective study of breast cancer in relation to coffee, tea and caffeine in Sweden. Int J Cancer 137(8):1979–1989
Bhoo-Pathy N, Peeters PHM, Uiterwaal CSPM, Bueno-de-Mesquita HB, Bulgiba AM, Bech BH, Overvad K, Tjønneland A, Olsen A, Clavel-Chapelon F, Fagherazzi G, Perquier F, Teucher B, Kaaks R, Schütze M, Boeing H, Lagiou P, Orfanos P, Trichopoulou A, Agnoli C, Mattiello A, Palli D, Tumino R, Sacerdote C, van Duijnhoven FJB, Braaten T, Lund E, Skeie G, Redondo M-L, Buckland G, Pérez MJS, Chirlaque M-D, Ardanaz E, Amiano P, Wirfält E, Wallström P, Johansson I, Nilsson LM, Khaw K-T, Wareham N, Allen NE, Key TJ, Rinaldi S, Romieu I, Gallo V, Riboli E, van Gils CH (2015) Coffee and tea consumption and risk of pre- and postmenopausal breast cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort study. Breast Cancer Res 17(1):15
Sisti JS, Hankinson SE, Caporaso NE, Gu F, Tamimi RM, Rosner B, Xu X, Ziegler R, Eliassen AH (2015) Caffeine, coffee, and tea intake and urinary estrogens and estrogen metabolites in premenopausal women. Cancer Epidemiol Biomark Prev 24(8):1174–1183
Kotsopoulos J, Eliassen AH, Missmer SA, Hankinson SE, Tworoger SS (2009) Relationship between caffeine intake and plasma sex hormone concentrations in premenopausal and postmenopausal women. Cancer 115(12):2765–2774
Kotsopoulos J, Eliassen AH, Missmer SA, Hankinson SE, Tworoger SS (2009) Relationship between caffeine intake and plasma sex hormone concentrations in premenopausal and postmenopausal women. Cancer 115(12):2765–2774
Halvorsen BL, Carlsen MH, Phillips KM, Bøhn SK, Holte K, Jacobs DR, Blomhoff R (2006) Content of redox-active compounds (i.e., antioxidants) in foods consumed in the United States. Am J Clin Nutr 84(1):95–135
Rahmioglu N, Heaton J, Clement G, Gill R, Surdulescu G, Zlobecka K, Hodgkiss D, Ma Y, Hider RC, Smith NW, Ahmadi KR (2011) Genetic epidemiology of induced CYP3A4 activity. Pharmacogenet Genomics 21(10):642–651
Lee WJ, Zhu BT (2006) Inhibition of DNA methylation by caffeic acid and chlorogenic acid, two common catechol-containing coffee polyphenols. Carcinogenesis 27(2):269–277
Pozner J, Papatestas AE, Fagerstrom R, Schwartz I, Saevitz J, Feinberg M, Aufses AH Jr (1986) Association of tumor differentiation with caffeine and coffee intake in women with breast cancer. Surgery 100(3):482–488
Boyd NF, Greenberg C, Lockwood G, Little L, Martin L, Byng J, Yaffe M, Tritchler D (1997) Effects at 2 years of a low-fat, high-carbohydrate diet on radiologic features of the breast: results from a randomized trial. Canadian Diet and Breast Cancer Prevention Study Group. J Natl Cancer Inst 89(7):488–496
Vachon CM, Kushi LH, Cerhan JR, Kuni CC, Sellers TA (2000) Association of diet and mammographic breast density in the Minnesota breast cancer family cohort. Cancer Epidemiol Biomark Prev 9(2):151–160
Tseng M, Vierkant RA, Kushi LH, Sellers TA, Vachon CM (2008) Dietary patterns and breast density in the Minnesota breast cancer family study. Cancer Causes Control 19(5):481–489
Takata Y, Maskarinec G, Park SY, Murphy SP, Wilkens LR, Kolonel LN (2007) Mammographic density and dietary patterns: the multiethnic cohort. Eur J Cancer Prev 16(5):409–414
Vachon CM, Kushi LH, Cerhan JR, Kuni CC, Sellers TA (2000) Association of diet and mammographic breast density in the Minnesota breast cancer family cohort. Cancer Epidemiol Biomark 9(2):151–160
Conner P, Svane G, Azavedo E, Soderqvist G, Carlstrom K, Graser T, Walter F, von Schoultz B (2004) Mammographic breast density, hormones, and growth factors during continuous combined hormone therapy. Fertil Steril 81(6):1617–1623
Greendale GA, Palla SL, Ursin G, Laughlin GA, Crandall C, Pike MC, Reboussin BA (2005) The association of endogenous sex steroids and sex steroid binding proteins with mammographic density: results from the postmenopausal estrogen/progestin interventions mammographic density study. Am J Epidemiol 162(9):826–834
Pettersen PC, Raundahl J, Loog M, Nielsen M, Tanko LB, Christiansen C (2008) Parallel assessment of the impact of different hormone replacement therapies on breast density by radiologist- and computer-based analyses of mammograms. Climacteric 11(2):135–143
Vachon CM, Sellers TA, Vierkant RA, Wu FF, Brandt KR (2002) Case-control study of increased mammographic breast density response to hormone replacement therapy. Cancer Epidemiol Biomark Prev 11(11):1382–1388
Colditz GA, Hankinson SE (2005) The nurses’ health study: lifestyle and health among women. Nat Rev Cancer 5(5):388–396
Tworoger SS, Sluss P, Hankinson SE (2006) Association between plasma prolactin concentrations and risk of breast cancer among predominately premenopausal women. Cancer Res 66(4):2476–2482
Bertrand KA, Rosner B, Eliassen AH, Hankinson SE, Rexrode KM, Willett W, Tamimi RM (2015) Premenopausal plasma 25-hydroxyvitamin D, mammographic density, and risk of breast cancer. Breast Cancer Res Treat 149(2):479–487
Farvid MS, Cho E, Chen WY, Eliassen AH, Willett WC (2014) Dietary protein sources in early adulthood and breast cancer incidence: prospective cohort study. BMJ 348:g3437
Oh K, Hu FB, Manson JE, Stampfer MJ, Willett WC (2005) Dietary fat intake and risk of coronary heart disease in women: 20 years of follow-up of the nurses’ health study. Am J Epidemiol 161(7):672–679
Byng JW, Boyd NF, Little L, Lockwood G, Fishell E, Jong RA, Yaffe MJ (1996) Symmetry of projection in the quantitative analysis of mammographic images. Eur J Cancer Prev 5(5):319–327
Pettersson A, Hankinson S, Willett W, Lagiou P, Trichopoulos D, Tamimi R (2011) Nondense mammographic area and risk of breast cancer. Breast Cancer Res 13(5):R100
Bertrand K, Eliassen AH, Hankinson S, Gierach G, Xu X, Rosner B, Ziegler R, Tamimi R (2012) Urinary estrogens and estrogen metabolites and mammographic density in premenopausal women. Breast Cancer Res Treat 136(1):277–287
Willett W, Stampfer MJ, Bain C, Lipnick R, Speizer FE, Rosner B, Cramer D, Hennekens CH (1983) Cigarette smoking, relative weight, and menopause. Am J Epidemiol 117(6):651–658
Stampfer MJ, Willett WC, Colditz GA, Rosner B, Speizer FE, Hennekens CH (1985) A prospective study of postmenopausal estrogen therapy and coronary heart disease. N Engl J Med 313(17):1044–1049
Treur JL, Taylor AE, Ware JJ, McMahon G, Hottenga JJ, Baselmans BML, Willemsen G, Boomsma DI, Munafò MR, Vink JM (2016) Associations between smoking and caffeine consumption in two European cohorts. Addiction 111(6):1059–1068
Klesges RC, Ray JW, Klesges LM (1994) Caffeinated coffee and tea intake and its relationship to cigarette smoking: an analysis of the second national health and nutrition examination survey (NHANES II). J Subst Abuse 6(4):407–418
Treur JL, Taylor AE, Ware JJ, McMahon G, Hottenga JJ, Baselmans BM, Willemsen G, Boomsma DI, Munafo MR, Vink JM (2016) Associations between smoking and caffeine consumption in two European cohorts. Addiction 111(6):1059–1068
Byrne C, Schairer C, Wolfe J, Parekh N, Salane M, Brinton LA, Hoover R, Haile R (1995) Mammographic features and breast cancer risk: effects with time, age, and menopause status. J Natl Cancer Inst 87(21):1622–1629
Yaghjyan L, Colditz GA, Rosner B, Tamimi RM (2013) Mammographic breast density and subsequent risk of breast cancer in postmenopausal women according to the time since the mammogram. Cancer Epidemiol Biomark Prev 22(6):1110–1117
Hu FB, Rimm E, Smith-Warner SA, Feskanich D, Stampfer MJ, Ascherio A, Sampson L, Willett WC (1999) Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr 69(2):243–249
Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, Hennekens CH, Speizer FE (1985) Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol 122(1):51–65
Acknowledgements
This work was supported by the National Cancer Institute at the National Institutes of Health [Grant Numbers CA131332, CA087969, CA175080 to R.M.T., UM1 CA186107 to M.S., UM1 CA176726 to W.W]; Avon Foundation for Women; Susan G. Komen for the Cure®; and Breast Cancer Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
This study was approved by the Institutional Review Board at the Brigham and Women’s Hospital. Consent was obtained or implied by return of questionnaires.
Rights and permissions
About this article
Cite this article
Yaghjyan, L., Colditz, G., Rosner, B. et al. Associations of coffee consumption and caffeine intake with mammographic breast density. Breast Cancer Res Treat 169, 115–123 (2018). https://doi.org/10.1007/s10549-018-4667-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-4667-4