Abstract
The objectives of this phase I/II study (NCT00140738) were to evaluate the safety and clinical activity of a cancer immunotherapeutic agent (recombinant HER2 protein (dHER2) and the immunostimulant AS15) in patients with HER2-overexpressing metastatic breast cancer (MBC). Forty HER2-positive MBC patients received up to 18 doses (12q2w, 6q3w) of dHER2 immunotherapeutic, as first- or second-line therapy following response to trastuzumab-based treatment as maintenance. Toxicity was graded by the Common Terminology Criteria for Adverse Events (CTCAE) and clinical activity was evaluated by target lesion assessment according to the Response Evaluation Criteria in Solid Tumors (RECIST). Immunogenicity was assessed. The dHER2 immunotherapeutic was well tolerated: grade 1/2 adverse events (AEs) were most common. No cardiac events were observed and one patient experienced an asymptomatic decrease of left ventricular ejection fraction below the normal range (47 %). Both humoral and cellular immunogenicity to the dHER2 antigen was observed. No patient discontinued the immunizations because of AEs but 35/40 withdrew prematurely, 34 because of disease progression (24/34 before or at the tumor assessment after dose 6). One patient achieved a complete response lasting 11 months and one patient had a partial response lasting 3.5 months. Ten patients experienced stable disease ≥26 weeks with 4/10 still in stable disease at the last tumor assessment after 47 weeks. Immunization of MBC patients with the dHER2 immunotherapeutic was associated with minimal toxicity and no cardiac events. Clinical activity was observed with two objective responses and prolonged stable disease for 10/40 patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately, 15–20 % of patients with breast cancer (BC) have tumors that overexpress the human epidermal growth factor receptor 2 gene (HER2). This subtype exhibits both aggressive biological behavior and poor clinical outcome [1]. For HER2-overexpressing BC patients, the humanized monoclonal antibody trastuzumab has become the mainstay of treatment in the adjuvant setting [1, 2]. However, metastatic breast cancer (MBC) is incurable and about 50 % of patients have disease progression within 1 year of starting treatment for advanced disease [3]. There is a need for a way to better control the disease in the metastatic setting and to prevent resistance to anti-HER2 agents [4, 5].
The HER2 protein has been shown to be immunogenic [6, 7]. Antigen-specific immunotherapy that mobilizes the patient’s own immune system to elicit a potent immune response against the HER2-overexpressing tumor cells may represent a promising therapeutic option. A strong, persistent, and functional immune response would also reduce the risk of relapse. As cancer immunotherapy has generally been shown to be less toxic than chemotherapy or targeted molecular inhibitors [8], this new therapeutic approach might also have a less negative impact on the patients’ quality of life than these other treatment options. Furthermore, if a persistent immune response can be elicited, HER2-targeted immunotherapy could be useful as adjuvant therapy after local–regional treatment of in situ cancer, and as second- or higher-line therapy in combination with monoclonal antibodies. This combination therapy could be used for treatment of metastatic patients with minimal residual disease after optimal standard care with trastuzumab/pertuzumab plus chemotherapy and other HER2-targeting agents like trastuzumab emtansine or lapatinib [9–11].
The objectives of this phase I/II clinical study were to assess the safety, clinical activity, and immunogenicity of immunization of HER2-overexpressing MBC patients with the dHER2 immunotherapeutic: an antigen-specific immunotherapeutic based on recombinant HER2 protein (dHER2) combined with AS15 immunostimulant AS15.
Patients and methods
Patient population
The study was conducted in 14 centers in Belgium, Colombia, France, Italy, and Peru.
The study protocol and its amendments were approved by the ethics committee of each participating study site and all enrolled patients gave written informed consent before any study procedure was performed (ClinicalTrials.gov: NCT00140738).
Eligibility requirements were: age 18 or older; a diagnosis of MBC with minimal tumor burden (defined in online-only); documented tumor overexpression of HER2 on metastatic disease (Table S1, online-only); Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1; adequate organ function (bone marrow reserve, renal and hepatic function); and left ventricular ejection fraction (LVEF) in the normal range (>50 %).
The patients could receive the dHER2 immunotherapeutic either as first-line therapy for metastatic disease or as second-line therapy after a first-line treatment based on maintenance trastuzumab treatment, either as monotherapy or in combination with chemotherapy. For the patients in the second-line cohort, the last dose of trastuzumab should not have been given less than 3 weeks before the first administration of the dHER2 immunotherapeutic. During the immunization period, the patients received no other anti-cancer treatment. After disease progression or completion of the immunizations, subsequent treatment was at the investigator’s discretion.
Treatment and monitoring
Each dose of dHER2 immunotherapeutic contains 500 µg of dHER2, a fusion protein including the complete extracellular domain (ECD) and a truncated part of the intracellular domain (ICD) of the HER2 protein plus a fixed dose of AS15 (see online-only). The complete immunization schedule consisted of 18 intramuscular injections administered in three cycles of six doses each, with an interval of 2 weeks for the first two cycles and 3 weeks for the third one. Immunizations were stopped at the first documented disease progression.
Cardiac monitoring was performed as sequential multi-gated acquisition evaluations of LVEF at baseline, midway and at the end of each of the two first treatment cycles, and midway during the last cycle. Blood samples for assessment of safety and immunogenicity were drawn at pre-specified time points. The severity of adverse events (AEs) was graded according to the Common Terminology Criteria for Adverse Events (CTCAE, version 3.0).
The clinical activity of the dHER2 immunotherapeutic was assessed by applying the Response Evaluation Criteria in Solid Tumors (RECIST, Version 1 [12]) at pre-specified time points. Time to disease progression was defined as the time from the first immunization until the time of documented progression or death, and censored at the last date of contact for non-progressing patients.
The anti-HER2 humoral immune response was assessed by separate antigen-specific enzyme-linked immunosorbent assays (ELISAs) measuring the antibody (Ab) concentration against the full recombinant protein (dHER2), and against each of the domains (HER2-ECD and HER2-ICD) separately. The HER2-specific cell-mediated immune (CMI) response was assessed by performing in vitro T-cell assays on peripheral blood mononuclear cells (PBMCs) collected at several pre-specified time points. Cellular immunogenicity was evaluated for CD4+ and CD8+ T-cell responses to HER2-ECD and HER2-ICD. Further details about the immunological monitoring are presented online only.
Results
Patients and treatment exposure
Between March 2005 and September 2009, 40 patients were enrolled and received at least one immunization: 17 as first-line and 23 as second-line therapy. Demographics and baseline disease characteristics are summarized in Table 1 (and Table S1 of online material). Five patients completed the 18-dose immunization schedule, one patient withdrew her consent after two immunizations (not AE-related) and 34 were withdrawn because of disease progression (Fig. 1). Of these 34 patients, 24 (71 %) were withdrawn during the first cycle of immunizations or at the tumor assessment 2 weeks after dose 6.
Safety
Table 2 summarizes the reported AEs, with the worst grade experienced at any time per patient reported. Most frequently reported AEs were grade 1–2 constitutional symptoms such as back pain, myalgia, diarrhea, chest pain, pain in extremities, and arthralgia. Three patients experienced grade 3 AEs possibly related to study treatment. In the first-line cohort, one patient had asthenia while in the second-line cohort, one patient had diarrhea and one patient had fatigue that was also reported as a serious adverse event (SAE). Four other treatment-unrelated SAEs were experienced, one in the first-line cohort (grade 1 bronchitis) and three in the second-line cohort (one grade 3 diarrhea, one grade 3 secondary BC, and one fatal pulmonary embolism). Three patients died of BC progression during the study.
No cardiac event was reported but five patients experienced an asymptomatic decrease of LVEF during the treatment period, with an absolute decrease from 9 to 19 %-points. One first-line patient experienced a temporary LVEF decrease of >20 % relative to baseline and with an absolute value of 47 %. Of these five patients, three in the first-line cohort had received epirubicin for the primary disease, and of the two in the second-line cohort, one had received doxorubicin and trastuzumab while the other had received trastuzumab only.
Clinical activity
One first-line patient achieved a complete response (CR), recorded at the first follow-up visit after the last scheduled immunization. This CR lasted 11 months after the patient had been in stable disease (SD) for 47 weeks. One second-line patient achieved a partial response (PR), recorded after the first treatment cycle (dose 6). This PR lasted 3 months, whereupon the patient progressed and discontinued the treatment.
Twelve patients (five in first-line, seven in second-line) achieved SD as best response, lasting 18 weeks for two patients, 26 weeks for four, 37 weeks for two, and 47 weeks or more for four patients who were still in SD at the last tumor assessment. With the definition of a clinical benefit rate (CBR, [13]) as CR + PR + SD (≥26 weeks), the overall CBR was 30 % (12/40 patients): 35 % (6/17 patients) in the first-line and 26 % (6/23 patients) in the second-line cohort.
The median time to disease progression was 2.8 months for the first-line and 3.4 months for the second-line cohort (Fig. 2).
Immunogenicity
The number of patients with available Ab data at each time point is variable (Fig. 3a). All first-line patients developed an Ab response to the whole dHER2 protein and to both the HER2-ECD and HER2-ICD after four to five immunizations (Fig. 3a). All patients remained responders to dHER2 and HER2-ICD during the entire immunization period and 3/5 patients were still responders to dHER2 after one year of follow-up. After the full response observed at the end of the first immunization cycle, the rate of humoral response to HER2-ECD was variable but always exceeding 50 % until the end of the follow-up. At baseline, no first-line patient had detectable anti-dHER2 or anti-HER2-ECD Abs, while anti-HER2-ICD Abs above the assay antigen immunogenicity cut-off value were observed for one patient (data not shown).
Percentage of responders (a) and antibody geometric mean concentrations (GMCs) (b) for first-line and second-line patients. a. Histograms indicate the percentage of responders (or no. of responders/no. assessed). On the X-axis, PDx indicates post Dose x. The relation between the assessment time points (PDx) and weeks (W) after treatment start is PD1 at W2, PD2 at W4, PD3 at W6, PD4 at W8, PD5 at W10, PD6 at W12, PD9 at W20, PD12 at W26, and PD15 at W37. Follow-up visits were as follows: FU1 1 month after the last administration of the study product (W47), FU2 3 months after (W55), FU3 6 months after (W69), and FU4 52 weeks after (W95). b. Cohort 1 first-line cohort, Cohort 2 second-line cohort, GMC geometric mean concentration, Weeks weeks after the start of the study treatment. The vertical bars around each observation point indicate 95 % CIs. On the X-axis, the small ticks represent the doses received in both cohorts; the long ticks represent the booster doses received in cohort 3. The horizontal dotted lines correspond to the assay cut-off (90 EU/mL for anti-dHER2, 44 EU/mL for anti-HER2-ECD, 104 EU/mL for anti-HER2-ICD)
In the second-line cohort, the rate of response during the immunization period peaked at 50 % for dHER2 and at 25 % for HER2-ECD (Fig. 3a). These low response rates are partly explained by the presence of anti-dHER2 or anti-HER2-ECD Abs due to the prior treatment with trastuzumab (knowing that the ECD of the HER2 protein comprises the epitope targeted by trastuzumab) and the protocol definition of responders involving the baseline Ab concentration. During the follow-up, the rate of responders to dHER2 and HER2-ECD increased to above 70 %. All the patients became responders to HER2-ICD after dose 5 and after 1 year of follow-up, the rate of responders was still 50 %. As expected, 13/17 patients (76.5 %) in the second-line cohort had detectable anti-dHER2 and anti-HER2-ECD Abs at baseline and one had anti-HER2-ICD Abs.
The kinetics of the Abs geometric mean concentrations (GMCs) for the first- and second-line cohorts are shown in Fig. 3b.
For technical reasons, data are limited for the CMI response to the dHER2 immunotherapeutic, with a maximum of four patients in either cohort with data recorded at any single time point. Suggestive CD4+ and CD8+ T-cell responses to both HER2-ECD and HER2-ICD were detectable 1 year after the last treatment administration (Table 3), but a conclusive assessment of the cellular immunogenicity is not possible due to the small sample size. Of note, however, each of the two patients with an objective tumor response showed detectable cellular responses including both CD4+ and CD8+ T-cells.
Discussion
The recombinant dHER2 is a fusion protein combining the entire ECD of the human HER2 protein and a part of its ICD [14]. In constructing this compound, the intent was to generate a therapeutic level of anti-HER2 Abs similar to those passively transferred by injections of trastuzumab and to emulate the various supposed mechanisms of action of trastuzumab, including HER2 degradation, inhibition of HER2 activation, and antibody-dependent cellular cytotoxicity [15–18]. The HER2-ICD-specific Abs were not expected to play any functional role in the immune response except to boost pre-existing cellular immunogenicity when released from lysed tumor cells and possibly by antigen epitope spreading [14–19]. Activating the host immune system by immunization with the dHER2 immunotherapeutic would have the advantage over monoclonal Ab treatment of eliciting a more effective immune response comprising both T-cells and polyclonal Abs with multiple mechanisms of action. In addition, active immunization would be expected to induce a sustained immune memory which would reduce or eliminate the need for repeated immunizations over the long-term to avoid tumor relapse.
Contrary to what was expected following the preclinical research program (unpublished data), the Ab data obtained after the dHER2 immunizations of the first-line patients showed a strong immune response against the HER2-ICD while the Ab response against the HER2-ECD was less prevalent, not sustained and with lower GMC values overall. This suggests a higher level of immune tolerance to this domain. In the first-line trastuzumab-naïve cohort, the anti-HER2-ECD Ab GMC peaked at 660 EU/mL after dose 6, while the pre-immunization anti-HER2-ECD Ab GMC in the second-line cohort was 2185 EU/mL, carrying over from the prior trastuzumab treatment after a wash-out period varying in length from patient to patient. It should be noted, however, that such a comparison involves comparing a presupposed polyclonal Ab response to an undefined number of epitopes [14] with the Ab response to a single epitope elicited by monoclonal Ab treatment.
The notable difference in the development of the anti-HER2-ECD Abs during the follow-up (Fig. 3b) is complicated to interpret, because further anti-cancer treatment post-immunization was at the discretion of the investigator and not recorded. The anti-HER2-ECD Abs observed may therefore have been impacted by post-immunization treatment with trastuzumab.
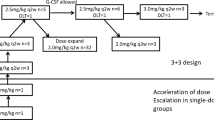
A stronger Ab response against HER2-ICD compared to HER2-ECD was also seen in previous trials with the dHER2 immunotherapeutic. In the first of these, the compound was investigated as single-agent adjuvant therapy for early stage BC patients with HER2-positive tumors at high risk of relapse [20]. This was a dose-escalation study to determine the optimal dose of dHER2 to be combined with AS15 in the immunotherapeutic agent. The focus was on safety and immunogenicity and the patients were followed-up for 5 years for these endpoints. In the second study, the dHER2 immunotherapeutic was tested in combination with lapatinib in heavily pretreated MBC patients [5] using the same dose of dHER2 and the same immunization schedule as in the present study.
Remarkably, the first-line patient achieving a CR showed an Ab response much more in line with the preclinical study results than the response of the other first-line patients. This patient did not present any detectable HER2-specific Abs at baseline and the level of her anti-ECD Abs increased after each successive immunization and peaked after dose 16. By contrast, the other first-line patients’ anti-ECD Ab levels plateaued or decreased after three or four immunizations (Figure S1A, online-only). Suggestive CD4+ T-cell activity specific for both ECD and ICD was also observed in this patient (Figure S1B, online-only).
It is notable in our study that 71 % of the patients who discontinued treatment because of disease progression did so during the first treatment cycle of six immunizations or at the tumor assessment at the end of the cycle. More than a third (12/34) of the progressing patients were already withdrawn at the visit for dose 4 administration or earlier. Arguably, the patients discontinuing the immunizations at an early stage of the study may not have had the necessary time to build up a comprehensive immune response capable of impacting tumor growth [21]. This may lead to speculation that the immunizations have been discontinued prematurely for a number of these patients, as was also noted in the study of the dHER2 immunotherapeutic combined with lapatinib [5]. A reassessment of the CBR leaving out the very early withdrawals of the analysis resulted in a CBR of 28.6 %, similar to the CBR of 30 % when including all the patients (online-only). However, this reassessment does not take into account the possibility that patients with early disease progression might have eventually shown an objective tumor response if they had been allowed to continue the immunizations [21].
Of particular note is the number of immunizations administered before an objective response was recorded. The PR was measured after the first cycle of six immunizations and the CR only after the last of the scheduled 18 immunizations. This underscores that prolonged time and many immunizations may be required to elicit effective immune responses (either antigen-specific or subsequent to antigen epitope spreading) [22] with a measurable impact on tumor lesions. Therefore, identification of predictive biomarkers that could reliably single out the patients who eventually would develop a potent and durable immune response should be given a high priority. Thus far, no clinical study has identified any definitive predictive biomarker other than HER2 expression itself to guide decision making concerning HER2 blockade [1, 23].
With a CR achieved as late as 10 months after the initiation of the immunizations, it may be questioned whether the response was mediated by a HER2-specific T-cell response or caused by something else. One possibility is the notion of epitope spreading, i.e., that the antigen-specific immune response is restricted to the initial phase of the anti-tumor response. Subsequent to this may follow immune responses to other, non-monitored antigens expressed by the tumor cells, which may determine the eventual tumor response [7, 8]. Another possible mechanism is immunogenic cell death, whereby tumor cells succumbing to previous chemotherapy or another modality are effectively converted into an immunotherapeutic agent, which in itself may elicit an adaptive immune response [24].
Few cancer immunotherapy agents have demonstrated a direct link between the predicted mechanism of action of the compound and clinical benefit for the patient [25, 26]. Some recent studies have, however, reported that patients showing high Ab response had longer survival [26–29]. Based on this hypothesis, post hoc analyses were performed on the possible association between the clinical response and the level of anti-HER2-ECD Abs for the first-line patients; the second-line patients could not be assessed because of their prior trastuzumab treatment. The analyses focused on the anti-HER2-ECD Abs because of their presupposed potential impact on clinical outcomes, whereas the anti-HER2-ICD Abs were not expected to have any direct functional role.
These exploratory analyses suggest that a longer progression-free-survival time was observed for patients with high anti-HER2-ECD Ab concentrations compared to low (above versus below the median), and for patients with an early HER2-ECD response (no later than after dose 3 vs. after dose 4 or later). It is possible that the time of the anti-HER2-ECD response is more important than the level of anti-HER2-ECD Abs concentration as the timing of the response segregates the survival curves more clearly than the level of the anti-HER2-ECD Abs (Figures S2 and S3, online-only). Considering the small number of patients in these analyses, these observations should be taken as indicative.
In conclusion, in patients with HER2-overexpressing MBC with minimal tumor burden, the dHER2 immunotherapeutic showed an acceptable safety profile and immunogenicity in patients receiving it either in the first-line setting or as maintenance therapy following standard-of-care therapy. The immunizations elicited a humoral immune response to each specific antigen domain in all trastuzumab-naïve patients. Many patients in both first- and second-line therapy displayed evidence of clinical benefit in terms of achieving CR, PR or prolonged SD. Some patients also presented signs of cell-mediated immunogenicity.
The dHER2 immunotherapeutic could potentially be tested as maintenance therapy for patients with optimal response after standard care [30, 31], although without a prospective randomized trial no definitive conclusion can be drawn. Arguably, the suboptimal HER2-ECD response induced by the dHER2 immunotherapeutic as currently designed could be countered by concomitant administration of trastuzumab until an adequate level of anti-HER2-ECD Abs has been achieved [5]. HER2 overexpression predicts an increased risk of isBCR in ductal in situ carcinoma (DCIS) of the breast [32]. To determine the clinical effect of anti-HER2 blockade, the National Surgical Adjuvant Breast Project (NSABP) B-43 phase III randomized trial is currently ongoing to test the efficacy of adding trastuzumab to conventional surgical and radiation therapy treatment of patients with HER2-overexpressing DCIS. The ideal trial with dHER2 can be performed in the preventive setting including patients with DCIS HER2 positive and defining as endpoint in situ and invasive recurrence.
Abbreviations
- Ab:
-
Antibody
- AE:
-
Adverse events
- BC:
-
Breast cancer
- CBR:
-
Clinical benefit rate
- CMI:
-
Cell-mediated immunogenicity
- CR:
-
Complete response
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- ECD:
-
Extracellular domain
- ECOG:
-
Eastern Cooperative Oncology Group
- ELISA:
-
Enzyme-linked immunosorbent assays
- GMC:
-
Geometric mean concentrations
- HER2:
-
Human epidermal growth factor receptor 2
- ICD:
-
Intracellular domain
- LVEF:
-
Left ventricular ejection fraction
- MBC:
-
Metastatic breast cancer
- PBMC:
-
Peripheral blood mononuclear cells
- PR:
-
Partial response
- RECIST:
-
Response evaluation criteria in solid tumors
- SAE:
-
Serious adverse event
- SD:
-
Stable disease
References
Zardavas D, Cameron D, Krop I et al (2013) Beyond trastuzumab and lapatinib: New options for HER2-positive breast cancer. Am Soc Clin Oncol Educ Book e2-e11
Goldhirsch A, Gelber RD, Piccart-Gebhart MJ et al (2013) 2 years versus 1 year of adjuvant trastuzumab for HER2-positive breast cancer (HERA): an open-label randomised controlled trial. Lancet 382:1021–1028
Andersson M, Lidbrink E, Bjerre K et al (2011) Phase III randomized study comparing docetaxel plus trastuzumab with vinorelbine plus trastuzumab as first-line therapy of metastatic or locally advanced human epidermal growth factor receptor 2-positive breast cancer: the HERNATA study. J Clin Oncol 29:264–271
Higgins MJ, Baselga J (2011) Targeted therapies for breast cancer. J Clin Invest 121:3797–3803
Hamilton E, Blackwell K, Hobeika AC et al (2012) Phase I clinical trial of HER2-specific immunotherapy with concomitant HER2 kinase inhibition. J Transl Med. doi:10.1186/1479-5876-10-28
Disis ML, Pupa SM, Gralow JR et al (1997) High-titer HER2/neu protein-specific antibody can be detected in patients with early-stage breast cancer. J Clin Oncol 15:3363–3367
Emens LA, Reilly RT, Jaffee EM (2005) Breast cancer vaccines: maximizing cancer treatment by tapping into host immunity. Endocr Relat Cancer 12:1–17
Bilusic M, Madan RA (2012) Therapeutic cancer vaccines: the latest advancement in targeted therapy. Am J Ther 19:e172–e181
Swain SM, Kim SB, Cortés J et al (2013) Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA study): overall survival results from a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol. 14:461–471
Verma S, Miles D, Gianni L et al (2012) Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med 367:1783–1791
Krop IE, Kim SB, Gonzalez-Martin A et al (2014) Trastuzumab emtansine versus treatment of physician’s choice for pretreated HER2-positive advanced breast cancer (TH3RESA): a randomised open-label, phase 3 trial. Lancet Oncol 15:689–699
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst 92:205–216
Krop IE, Beeram M, Modi S et al (2010) Phase I study of trastuzumab-DM1, an HER2 antibody-drug conjugate, given every 3 weeks to patients with HER2-positive metastatic breast cancer. J Clin Oncol 28:2698–2704
Foy TM, Fanger GR, Hand S et al (2002) Designing HER2 vaccines. Semin Oncol 29(Suppl 11):53–61
Valabrega G, Montemurro F, Aglietta M (2007) Trastuzumab: mechanism of action, resistance and future perspectives in HER2-overexpressing breast cancer. Ann Oncol 18:977–984
Stagg J, Loi S, Divisekera U et al (2011) Anti-ErbB-2 mAb therapy requires type I and II interferons and synergizes with anti-PD-1 or anti-CD137 mAb therapy. Proc Natl Acad Sci USA 108:7142–7147
Vu T, Claret FX (2012) Trastuzumab: updated mechanisms of action and resistance in breast cancer. Front Oncol 2:62
Shi Y, Fan X, Meng W et al (2014) Engagement of immune effector cells by trastuzumab induces HER2/ERBB2 downregulation in cancer cells through STAT1 activation. Breast Cancer Res 16:R33
Disis ML, Wallace DR, Gooley TA et al (2009) Concurrent trastuzumab and HER2/neu-specific vaccination in patients with metastatic breast cancer. J Clin Oncol 27:4685–4692
Limentani SA, Campone M, Dorval T, et al: A non-randomized dose-escalation Phase I trial of a protein-based immunotherapeutic for the treatment of breast cancer patients with HER2-overexpressing tumors. Breast Cancer Res Treat, manuscript submitted in parallel
Schlom J (2012) Therapeutic cancer vaccines: current status and moving forward. J Natl Cancer Inst 104:599–613
Kruit WH, Suciu S, Dreno B et al (2013) Selection of immunostimulant AS15 for active immunization with MAGE-A3 protein: results of a randomized phase II study of the European Organization for Research and Treatment of Cancer Melanoma Group in metastatic melanoma. J Clin Oncol 31:2413–2420
Curigliano G, Perez EA (2014) Immunoscoring breast cancer: TILs remember what they target. Ann Oncol 25:1455–1456
Zitvogel L, Kepp O, Kroemer G (2011) Immune parameters affecting the efficacy of chemotherapeutic regimens. Nat Rev Clin Oncol 8:151–160
Sharma P, Wagner K, Wolchok JD et al (2011) Novel cancer immunotherapy agents with survival benefit: recent successes and next steps. Nat Rev Cancer 11:805–812
Campbell CT, Gulley JL, Oyelaran O et al (2014) Humoral response to a viral glycan correlates with survival on PROSTVAC-VF. Proc Natl Acad Sci USA 111:E1749–E1758
Garcia B, Neninger E, de la Torre A et al (2008) Effective inhibition of the epidermal growth factor/epidermal growth factor receptor binding by anti-epidermal growth factor antibodies is related to better survival in advanced non-small-cell lung cancer patients treated with the epidermal growth factor cancer vaccine. Clin Cancer Res 14:840–846
Harrop R, Shingler W, Kelleher M et al (2010) Cross-trial analysis of immunologic and clinical data resulting from phase I and II trials of MVA-5T4 (TroVax) in colorectal, renal, and prostate cancer patients. J Immunother 33:999–1005
Harrop R, Shingler WH, McDonald M et al (2011) MVA-5T4-induced immune responses are an early marker of efficacy in renal cancer patients. Cancer Immunol Immunother 60:829–837
Miles D, Roche H, Martin M et al (2011) Phase III multicenter trial of the sialyl-TN (STn)-keyhole limpet hemocyanin (KLH) vaccine for metastatic breast cancer. Oncologist 16:1092–1100
Ibrahim NK, Murray JL, Zhou D et al (2013) Survival advantage in patients with metastatic breast cancer receiving endocrine therapy plus sialyl Tn-KLH vaccine: Post hoc analysis of a large randomized trial. J Cancer 4:577–584
Curigliano G, Disalvatore D, Esposito A et al (2015) Risk of subsequent in situ and invasive breast cancer in human epidermal growth factor receptor 2-positive ductal carcinoma in situ. Ann Oncol 26(4):682–687
Acknowledgments
The authors thank the patients who participated in this study and their families. They also acknowledge the investigators and their clinical teams for their contribution to the study and their support and care of patients, in particular Thomas Bachelot, Henri Roche and Jaak Janssens. The authors thank the global and regional clinical operations and safety teams of GSK for their contribution to the study, the scientific writer for clinical protocol and clinical report writing and the team of statisticians at GSK for the statistical analysis. The authors thank Françoise Cormont, Valentine Wascotte and Anne-Laure Puaux for critical reading of the paper and helpful suggestions. The authors thank Niels Neymark (medical writer on behalf of GSK) for assistance in the manuscript writing, and Sophie Timmery (XPE Pharma & Science) for coordination and editorial assistance.
Author contributions
Study conception and design Vincent Brichard, Frédéric F. Lehmann, Jamila Louahed, Andrea Callegaro. Collection and assembly of data Giuseppe Curigliano, Gilles Romieu, Lionel Duck, Célia Roemer-Becuwe, Mario Roselli, Silvia Neciosup, Jean-Luc Canon. Data analysis and interpretation Vincent Brichard, Frédéric F. Lehmann, Jamila Louahed, Wivine Burny, Giuseppe Curigliano, Pedro Miguel de Sousa Alves, Andrea Callegaro, Lionel Duck, Mario Campone. Provision of study materials or patients Giuseppe Curigliano, Gilles Romieu, Silvia Neciosup, Mario Campone.
Disclosures
Employment Pedro Miguel De Sousa Alves (GSK group of companies); Frédéric F. Lehmann (GSK group of companies); Jamila Louahed (GSK group of companies); Vincent G. Brichard (GSK group of companies); Wivine Burny (GSK group of companies); Andrea Callegaro (GSK group of companies). Stock ownership Frédéric F. Lehmann (GSK group of companies); Jamila Louahed (GSK group of companies); Vincent G. Brichard (GSK group of companies); Pedro Miguel De Sousa Alves (GSK group of companies). Honoraria Mario Campone (Novartis, Servier, Menar). Consultant or advisory role Mario Campone (Novartis, Servier, Menar), Jean-Luc Canon (GSK). Speakers’ bureau Gilles Romieu (GSK, Roche), Mario Campone (Novartis). Research funding Mario Campone’s institution (Novartis). Expert testimony: Gilles Romieu (Roche). Travel, accommodations, expenses Gilles Romieu (Amgen), Mario Campone (Novartis).
Funding
This work was supported by GlaxoSmithKline Biologicals SA that was involved in all stages of the study conduct and analysis. GlaxoSmithKline Biologicals SA also funded all costs associated with the development and the publishing of the present manuscript. All authors had full access to the data and the corresponding author was responsible for submission of the publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Giuseppe Curigliano, Lionel Duck, Célia Roemer-Becuwe, Mario Roselli, Silvia Neciosup, Thierry Dorval declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Curigliano, G., Romieu, G., Campone, M. et al. A phase I/II trial of the safety and clinical activity of a HER2-protein based immunotherapeutic for treating women with HER2-positive metastatic breast cancer. Breast Cancer Res Treat 156, 301–310 (2016). https://doi.org/10.1007/s10549-016-3750-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-016-3750-y