Abstract
Human epidermal growth factor receptor 2 (HER2) is an effective therapeutic target in breast cancer. However, not all patients benefit from trastuzumab-based therapy. We aimed to investigate whether patients with different levels of HER2 amplification would experience different clinical outcomes with trastuzumab-based chemotherapy. We quantified the HER2 gene copy number (GCN) and HER2/centromere chromosome probe 17 (CEP17) ratio in 291 breast cancer patients with HER2 amplification confirmed by immunohistochemistry and fluorescence in situ hybridization. The optimal cutoff points for HER2 GCN and the HER2/CEP17 ratios for distinguishing positive results were determined by receiver operating characteristic (ROC) curve analyses. ROC analysis identified optimal cutoff points for HER2 GCN and HER2/CEP17 ratios as 11.5 and 6.5 (P = 0.039 and P = 0.012), respectively. The DFS in patients with HER2 GCN <11.5 was significantly longer than in HER2 GCN ≥11.5 patients (P = 0.015) according to Kaplan–Meier survival curves analysis. Similarly, patients with HER2/CEP17 ratios <6.5 had a significantly longer DFS than those with HER2/CEP17 ratios ≥6.5 (P = 0.013). Moreover, patients with HER2 cluster amplification showed a worse survival than those with HER2 non-cluster amplification (P = 0.041). This study demonstrated a significant association between the level of HER2 amplification and survival time in a relatively large cohort of HER2-positive breast cancer patients undergoing trastuzumab-based chemotherapy. Further investigations of more precise quantitative measurements and larger cohorts are required to define this threshold.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer occurring in women, with an average female lifetime risk of developing breast cancer of 1 in 9 [1]. Each year, about 1.4 million new cases of breast cancer are diagnosed worldwide, and more than 4,50,000 deaths from the disease are reported annually [2]. About 50 % of patients with early stage breast cancer ultimately develop metastatic breast cancer [3].
Human epidermal growth factor receptor 2 (HER2) has been identified as a crucial oncogene in breast cancer and is involved in enhancing cancer cell survival, proliferation, invasion, and metastasis via the PI3K/AKT and RAS/MAPK tyrosine kinase pathways [4]. HER2 amplification and HER2 protein overexpression occur in approximately 20–30 % of breast cancer patients and are associated with high recurrence and a poor clinical outcome [5, 6]. As well as being a negative predictive and prognostic marker, HER2 is also an effective therapeutic target through use of the humanized monoclonal antibody trastuzumab and anti-Her2 monoclonal antibodies pertuzumab and ertumaxomab, selective small molecule tyrosine kinase inhibitor, especially in combination with chemotherapeutic agents [7, 8]. Several large, multicenter, randomized trials found that trastuzumab combined with chemotherapy produced significantly more positive results in terms of higher objective response, and the prolongation of progression-free and overall survival in HER2-positive breast cancers compared with [9–11]. However, not all patients benefit from trastuzumab-based therapy, and clinical response rates have been reported to range from 12 to 68 %, indicating that there is a high correlation between response to trastuzumab-based treatment and HER2 status [12, 13]. It is therefore crucial to accurately determine the HER2 status in breast cancer patients to ensure that they receive appropriate anti-HER2 targeted therapies.
According to current guidelines proposed by the American Society of Clinical Oncology/College of American Pathologists (ASCO/CAP), fluorescence in situ hybridization (FISH) and immunohistochemistry (IHC) are approved techniques to assess the status of HER2 amplification and HER2 expression [14]. The IHC scoring system classifies the HER2 expression status into roughly four grades, 0, 1+, 2+, and 3+, which describe HER2 expression in a large dynamic range from 2500 to 2 million receptors per cell. However, when the IHC score is 2+, the status of cancer cases cannot be accurately assessed and so may be ambiguous. In comparison with the qualitative or semiquantitative nature of IHC, FISH quantitatively measures HER2 amplification in breast cancer [14, 15]. However, cancer cases are usually identified as HER2 amplified or non-amplified by the HER2/centromere chromosome probe 17 (CEP17) ratio ≥2.0. Additionally, a wide variation from 2 to over 20 exists in HER2-amplified cases, and it remains unclear whether this variation confers clinical significance [16]. Moreover, different responses to trastuzumab-based treatment and clinical outcome have been observed in breast cancer patients regarded as having an HER2-amplified status [16–19].
Currently, there is insufficient evidence to quantitatively determine the association between the level of HER2 amplification and clinical parameters. In the present study, therefore, we quantified the HER2/CEP17 ratio and HER2 gene copy number (GCN) in 291 breast cancer patients with confirmed HER2 amplification, investigated whether the patients with different levels of HER2 amplification experienced different clinical outcomes following trastuzumab-based chemotherapy and explored the predictive or prognostic role of HER2 amplification quantification in breast cancer.
Materials and methods
Patients
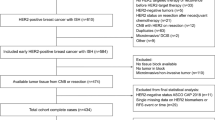
Breast cancer patients were recruited from the Tumor Hospital of Harbin Medical University and the Second Affiliated Hospital of Harbin Medical University between January 1st, 2007 and June 30th, 2009. The inclusion criteria were complete clinical and pathologic data; Eastern Cooperative Oncology Group performance status of 0–1; adequate renal, hepatic, and hematologic function; cardiac ejection fraction within the normal range; no metastatic lesions before surgery; infiltrating ductal carcinoma; verified HER2 amplification; and treated with trastuzumab-based adjuvant standard chemotherapy. Finally, a total of 291 patients were enrolled in the study. Follow-up examinations began from the date of surgery until June 2014. Patients who developed recurrence or metastasis were verified by adequate diagnostic imaging modalities and pathology during the follow-ups. This study was approved by the Local Commission for Medical Ethics and Clinical Studies of Harbin Medical University.
Methods
IHC
All breast cancer tissues were formalin-fixed and paraffin-embedded. Tissue sections were cut into 4-µm-thick sections and mounted on a slide. IHC analysis was performed as previously described [11]. In brief, slides were incubated with an anti-HER2 polyclonal antibody (Dako, Carpinteria, CA), and positive staining of the cell membrane was considered to reflect HER2 protein expression. HER2 expression was scored according to ASCO/CAP guidelines (Table 1) [14]. Sections with strong membrane staining were used as positive controls.
FISH
FISH analysis was performed on paraffinized 5-µm-thick sections using the Vysis LSI HER2 SpectrumOrange and CEP17 SpectrumGreen Dual Color DNA probe kit (VysisPath Vysion, Abbot Laboratories, Des Plaines, IL) in line with the manufacturer’s instructions. In brief, sections were baked, deparaffinized, dehydrated, deproteinized, and refixed. They were then denatured and hybridized in a hybridization oven. Finally, the sections were washed and counterstained with 4′,6-diamidino-2-phenylindole (Invitrogen, Grand Island, NY) for signal calculation. Scoring of HER2 and CEP17 probe signals was performed using a fluorescence microscope (Olympus BX51). FISH results were interpreted depending on two different scoring methods: (1) based on absolute HER2 GCN or (2) based on the HER2/CEP17 ratio. As proposed by the ASCO/CAP guidelines [14], a HER2/CEP17 ratio ≥2.0 or an HER2/CEP17 ratio <2.0 with an average HER2 GCN >6.0 signals/cell was considered HER2 positive.
Statistical methods
Disease-free survival (DFS) was calculated as the time between diagnosis and local recurrence, distant metastasis, or death from breast cancer. To evaluate whether an increased HER2 GCN and/or HER2/CEP17 ratio affected sensitivity to trastuzumab-based adjuvant chemotherapy, we chose patients with recurrence or metastasis during the follow-ups and defined them as the poor survival group. Other patients were named the good survival group. We thought that the patients with good survival time were sensitive to trastuzumab-based adjuvant chemotherapy and vice versa. To further evaluate the prediction performance of HER2 status, receiver operating characteristic (ROC) analysis was performed. Sensitivity and specificity were calculated using the optimal cutoff points on the ROC curves, which determined the maximum value of Youden index [20].
The Chi squared (χ 2) test was used to determine the relationship between clinicopathological parameters and optimal cutoff values. Survival curves were analyzed by the Kaplan–Meier method, and the comparison between curves was evaluated using the log-rank test. All statistical analyses were carried out using IBM SPSS statistics version 20.0 (SPSS Inc., Chicago, IL). Results were considered significant when P values were <0.05.
Results
Patient and tumor characteristics
A total of 291 tumor specimens were included in our study. The characteristics of the enrolled patients are summarized in Table 2. The patient median age was 48 years (range 19–74 years). The median tumor size was 4 cm. Over half of all patients (59.1 %) were premenopausal, and 55 % had no lymphatic metastasis.
HER2 status analysis
Of the 291 cases, two (0.7 %) were IHC level 0, nine (3.1 %) were 1+, 128 (44.0 %) were 2+, and 152 (52.2 %) were 3+. Representative images of HER2 protein overexpression are shown in Fig. 1. Differences in tumor specimen HER2 GCN as shown by FISH can be seen in Fig. 2. HER2/CEP17 ratios ranged from 2.0 to 26 (median 7).
HER2 status identified by FISH. Red signals represent HER2, green signals represent CEP17 (original magnification ×600). a HER2-negative status, b high level of HER2-positive status, HER2/CEP17 ratio ≥6.5, c high level of HER2-positive status, average HER2 GCN ≥11.5, d high level of HER2-positive status, clustered HER2 signals
Optimal cutoff points of HER2 GCN and the HER2/CEP17 ratio
ROC analyses were applied to determine the optimal cutoff point that distinguished between patients with shorter survival and those likely to resist trastuzumab-based adjuvant chemotherapy. Regarding HER2 GCN, 11.5 was identified as the optimal cutoff point for distinguishing refractory patients from sensitive patients (P = 0.039) (Fig. 3a), while 6.5 was identified for the HER2/CEP17 ratio (P = 0.012) (Fig. 3b). The optimal HER2 GCN and HER2/CEP17 ratio cutoff values were related with an IHC 3+ result, as seen in Table 3.
Survival in terms of HER2 amplification
The optimal HER2 GCN cutoff point distinguished those patients with a poor prognosis. Kaplan–Meier survival curves analysis showed that the DFS in patients with a HER2 GCN <11.5 was significantly longer than those with HER2 GCN ≥11.5 (P = 0.015) (Fig. 4a). Similarly, patients with HER2/CEP17 ratios <6.5 had a significantly longer DFS than those with HER2/CEP17 ratios ≥6.5 (P = 0.013) (Fig. 4b).
Patients were divided into two groups according to the status of HER2 cluster amplification in the tissues. Kaplan–Meier survival curves (Fig. 4c) demonstrated that the DFS in patients with HER2 cluster amplification was significantly shorter than in those with HER2 non-cluster amplification (P = 0.041).
Discussion
Compared with hormone receptor-positive subtypes of breast cancer, HER2-positive breast cancer has specific clinicopathological features, including a higher histologic grade, the expression of fewer hormone receptors, increased metastases, and an adverse prognosis [21, 22]. The discovery of HER2-target therapeutic regimes, such as trastuzumab, has revolutionized the treatment for breast cancer. This antibody directly binds the extracellular domain of HER2 and exerts its therapeutic effects by inhibiting proliferation and the survival signaling pathway and initiating antibody-dependent cellular cytotoxicity. To date, trastuzumab-based treatment has become the standard of care for HER2-positive breast cancers [23–25]; however, a series of clinical trials indicated that a high proportion of cases with HER2-positive amplification failed to benefit from such treatment [12, 26, 27].
Recent studies have attempted to explain that differences in clinical outcome after trastuzumab-based treatment could be associated with the level of HER2 amplification [24, 28–30]. However, the results of these studies were controversial. The main purpose of this study was to explore whether patients with varying levels of HER2 amplification present with different clinical outcomes to trastuzumab-based chemotherapy and to identify a more appropriate threshold of HER2 amplification. We applied ROC analysis to 291 HER2-positive patients (determined by FISH) to determine the optimal threshold that discriminated between patients with good and poor outcomes. Although several studies previously suggested that the level of HER2 amplification would predict the response to trastuzumab-based treatment and prognosis, to our knowledge, this is the first time that the threshold of the HER2/CEP17 ratio and HER2 GCN has been used to distinguish treatment response and outcome in HER2-amplified breast cancer patients.
We showed that the low HER2 amplification group (HER2/CEP17 ratio <6.5 or HER2 GCN <11.5) presented with a significantly longer survival time, while the high HER2 amplification group (HER2/CEP17 ratio ≥6.5 or HER2 GCN ≥11.5) had a worse outcome with a significantly shorter survival time. The different prognoses could be explained by different responses to trastuzumab-based treatment or even resistance to treatment. We speculate that a high level of HER2 amplification might cause HER2 crowding on the cell surface, overactivation of the downstream signal, or increased malignant biological behavior that inhibits trastuzumab–HER2 binding, thus abrogating the clinical response. However, the specific molecular mechanisms involved in treatment efficacy remain to be fully validated.
In conclusion, our study demonstrated a significant association between the level of HER2 amplification and survival time in a relatively large cohort of HER2-positive breast cancer patients. Compared with previous reports, our study established the first threshold of the HER2/CEP17 ratio using ROC analysis. This enabled HER2 amplification patients to be classified into those with high or low levels of amplification, which exhibited different clinical outcomes. Our results suggest that another threshold could exist in the level of HER2 amplification besides that for trastuzumab treatment. Future work should investigate more precise quantitative measurements in larger cohorts to better define this threshold.
References
Doss S, Robertson J, Adam J (2012) Lapatinib or trastuzumab in combination with an aromatase inhibitor for first-line treatment of metastatic hormone-receptor-positive breast cancer that overexpresses HER2. Lancet Oncol 13:766–767
Ferlay J, Soerjomataram I, Dikshit R et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359–E386
DeSantis C, Ma J, Bryan L, Jemal A (2014) Breast cancer statistics 2013. CA Cancer J Clin 64:52–62
Krishnamurti U, Silverman JF (2014) HER2 in breast cancer: a review and update. Adv Anat Pathol 21:100–107
Guiu S, Gauthier M, Coudert B et al (2010) Pathological complete response and survival according to the level of HER-2 amplification after trastuzumab-based neoadjuvant therapy for breast cancer. Br J Cancer 103:1335–1342
Aboutorabi A, Hadian M, Ghaderi H et al (2014) Cost-effectiveness analysis of trastuzumab in the adjuvant treatment for early breast cancer. Glob J Health Sci 7:98–106
Kümler I, Tuxen MK, Nielsen DL (2014) A systematic review of dual targeting in HER2-positive breast cancer. Cancer Treat Rev 40:259–270
Gianni L, Pienkowski T, Im YH et al (2012) Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol 13:25–32
Ross JS, Slodkowska EA, Symmans WF et al (2009) The HER-2 receptor and breast cancer: ten years of targeted anti-HER-2 therapy and personalized medicine. Oncologist 14:320–368
Pegram MD, Finn RS, Arzoo K et al (1997) The effect of HER-2/neu overexpression on chemotherapeutic drug sensitivity in human breast and ovarian cancer cells. Oncogene 15:537–547
Di Leo A, Desmedt C, Bartlett JM et al (2011) HER2 and TOP2A as predictive markers for anthracycline-containing chemotherapy regimens as adjuvant treatment of breast cancer: a meta-analysis of individual patient data. Lancet Oncol 12:1134–1142
Bates M, Sperinde J, Köstler WJ et al (2011) Identification of a subpopulation of metastatic breast cancer patients with very high HER2 expression levels and possible resistance to trastuzumab. Ann Oncol 22:2014–2020
Arnould L, Arveux P, Couturier J et al (2007) Pathologic complete response to trastuzumab-based neoadjuvant therapy is related to the level of HER-2 amplification. Clin Cancer Res 13:6404–6409
Wolff AC, Hammond ME, Hicks DG et al (2013) Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American society of clinical oncology/College of American pathologists clinical practice guideline update. J Clin Oncol 31:3997–4013
Sapino A, Goia M, Recupero D, Marchiò C (2013) Current challenges for HER2 testing in diagnostic pathology: state of the art and controversial issues. Front Oncol 3:129
Borley A, Mercer T, Morgan M et al (2014) Impact of HER2 copy number in IHC2+/FISH-amplified breast cancer on outcome of adjuvant trastuzumab treatment in a large UK cancer network. Br J Cancer 110:2139–2143
Wang S, Hossein Saboorian M, Frenkel EP et al (2002) Aneusomy 17 in breast cancer: its role in HER-2/neu protein expression and implication for clinical assessment of HER-2/neu status. Mod Pathol 15:137–145
Yu KD, Liu GY, Zhou XY et al (2012) Association of HER-2 copy number and HER-2/CEP-17 ratio with neoadjuvant taxane-containing chemotherapy sensitivity in locally advanced breast cancer. Oncologist 17:792–800
Giuliani R, Durbecq V, Di Leo A et al (2007) Phosphorylated HER-2 tyrosine kinase and Her-2/neu gene amplification as predictive factors of response to trastuzumab in patients with HER-2 overexpressing metastatic breast cancer (MBC). Eur J Cancer 43:725–735
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35
Rouzier R, Perou CM, Symmans WF et al (2005) Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res 11:5678–5685
Konecny GE, Thomssen C, Lück HJ et al (2004) Her-2/neu gene amplification and response to paclitaxel in patients with metastatic breast cancer. J Natl Cancer Inst 96:1141–1151
Untch M, Konecny GE, Paepke S et al (2014) Current and future role of neoadjuvant therapy for breast cancer. Breast 23:526–537
Fuchs EM, Köstler WJ, Horvat R et al (2014) High-level ERBB2 gene amplification is associated with a particularly short time-to-metastasis, but results in a high rate of complete response once trastuzumab-based therapy is offered in the metastatic setting. Int J Cancer 135:224–231
Hofmann M, Stoss O, Gaiser T et al (2008) Central HER2 IHC and FISH analysis in a trastuzumab (Herceptin) phase II monotherapy study: assessment of test sensitivity and impact of chromosome 17 polysomy. J Clin Pathol 61:89–94
Seol H, Lee HJ, Choi Y et al (2012) Intratumoral heterogeneity of HER2 gene amplification in breast cancer: its clinicopathological significance. Mod Pathol 25:938–948
Lipton A, Köstler WJ, Leitzel K et al (2010) Quantitative HER2 protein levels predict outcome in fluorescence in situ hybridization-positive patients with metastatic breast cancer treated with trastuzumab. Cancer 116:5168–5178
Gomez-Martin C, Plaza JC, Pazo-Cid R et al (2013) Level of HER2 gene amplification predicts response and overall survival in HER2-positive advanced gastric cancer treated with trastuzumab. J Clin Oncol 31:4445–4452
Gullo G, Bettio D, Torri V et al (2009) Level of HER2/neu gene amplification as a predictive factor of response to trastuzumab-based therapy in patients with HER2-positive metastatic breast cancer. Investig New Drugs 27:179–183
Gullo G, Bettio D, Zuradelli M et al (2013) Level of HER2/neu amplification in primary tumours and metastases in HER2-positive breast cancer and survival after trastuzumab therapy. Breast 22:190–193
Acknowledgments
This study was supported by the National Natural Science Foundation of China (Grant No. 81372839).
Conflict of interest
The authors declare that they have no conflicts of interest.
Informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Qijia Xuan and Hongfei Ji contributed equally to the work.
Qijia Xuan and Hongfei Ji should be considered co-first authors.
Rights and permissions
About this article
Cite this article
Xuan, Q., Ji, H., Tao, X. et al. Quantitative assessment of HER2 amplification in HER2-positive breast cancer: its association with clinical outcomes. Breast Cancer Res Treat 150, 581–588 (2015). https://doi.org/10.1007/s10549-015-3334-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-015-3334-2