Abstract
We examined the factors associated with screening mammography adherence behaviors and influencing factors on women’s attitudes toward mammography in non-adherent women. Design-based logistic regression models were developed to characterize the influencing factors, including socio-demographic, health related, behavioral characteristics, and knowledge of breast cancer/mammography, on women’s compliance with and attitudes toward mammography using the 2003 Health Information National Trends Survey data. Findings indicate significant associations among adherence to mammography and marital status, income, health coverage, being advised by a doctor to have a mammogram, having had Pap smear before, perception of chance of getting breast cancer, and knowledge of mammography (frequency of doing mammogram) in both women younger than 65 and women aged 65 and older. However, number of visits to a healthcare provider per year and lifetime number of smoked cigarettes are only significant for women younger than 65. Factors significantly associated with attitudes toward mammography in non-adherent women are age, being advised by a doctor to have a mammogram, and seeking cancer information. To enhance adherence to mammography programs, physicians need to continue to advise their patients to obtain mammograms. In addition, increasing women’s knowledge about the frequency and starting age for screening mammography may improve women’s adherence. Financially related factors such as income and insurance are also shown to be significant factors. Hence, healthcare policies aimed at providing breast cancer screening services to underserved women will likely enhance mammography participation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer among women in the United States, aside from non-melanoma skin cancer. In 2013, approximately 232,340 new cases of invasive and 64,640 new cases of ductal carcinoma in situ breast cancer will be diagnosed, and about 39,620 women will die from breast cancer [1]. Screening mammography is currently the most common method of breast cancer early detection and has been shown to reduce breast cancer mortality risk by 15 % [2]. On average, screening mammography can detect breast cancer 1.7 years before a woman is able to feel a lump in her breast [3].
There are varying recommendations from different agencies for screening mammography in the U.S. The two most referred guidelines are from the American Cancer Society (ACS) and the U.S. Preventive Services Task Force (USPTF). The ACS recommends starting annual mammography at age 40 but recommends no ending age [4]. In November 2009, the USPSTF issued new breast cancer screening guidelines, which recommend biennial screening for women ages from 50 to 74. The USPSTF also recommended that women ages from 40 to 49 should not undergo screening mammography unless they are in a high-risk group [5].
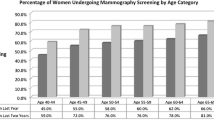
The impact of mammography on women’s outcomes is strongly associated with women’s compliance with the mammography recommendations. Examination of a clinic-based group of 216 women with a strong family history of breast or ovarian cancer showed that 50, 83, 69, and 53 % of the women at age groups of 30–39, 40–49, 50–64, and 65 years and older, respectively, had only one mammogram between 1995 and 1999 [6]. More recently, a study by the Centers for Disease Control and Prevention (CDC) revealed that, in 2010, about 67.1 % of women aged 40 and older had one mammogram between 2008 and 2010 [7].
In this study, we aim to (1) identify significant factors (socio-demographic, health related, behavioral attributes, and knowledge mammography) associated with women’s adherence to mammography screening and (2) study the attitudes toward mammography in non-adherent women. We assume that women’s compliance with screening mammography is strongly correlated with their intentions to get a mammogram (i.e. their expectations about their next mammogram or their thoughts about getting a mammogram [8]). Based on this assumption, if a woman has a positive attitude toward screening mammograms and her plan for the next mammogram is within the next one or two years, then she is considered to be adherent.
Methods
Data source
We used the 2003 Health Information National Trends Survey (HINTS) data for this study [9]. HINTS, developed by the National Cancer Institute (NCI), is a nationally representative telephone survey of 6,369 adults aged 18 and older. The 2003 data are currently the only HINTS data that provide information on women’s attitudes and perceptions toward mammography. HINTS 2005 and 2007 data do not include questions regarding mammography. HINTS 2012 only reports the time of the most recent mammogram and whether a doctor has informed about a mammogram; however, no data are collected on women’s intentions or attitudes toward mammograms, which is the focus of this study.
Study design
There are two stages for this study. In the first stage, we aim to identify significant factors associated with women’s adherence to mammography screenings. To be consistent with current mammography guidelines and practices, we focus on women older than 40. We perform these analyses separately for two age groups: women younger than 65 and women aged 65 and older. In contrast to earlier studies, we measure adherence based on women’s intentions and attitudes toward mammography.
In the second stage, we focus only on women older than 42 with poor mammography history, i.e. women who have never had mammography or their most recent mammography was more than two years ago and they did not say “never heard of it” when asked why they had not had a mammogram. Age 42 is used as the lower boundary for these analyses because an every-other-year interval for mammography requires enough time for women over age 40 to have a mammogram. We do not separate women younger and older than 65 in order to achieve an adequate sample size. We examine the differences between those who think about getting a mammogram and other women in this population.
Predicting factors
We categorized factors that may be associated with women’s adherence to mammography screening into four groups: Socio-demographic characteristics including age, race, marital status, employment, education, income, health coverage, and living area based on Census Division; Health-related characteristics including body mass index (BMI), average number of visits to a healthcare provider a year, family history of cancer, psychological distress composite score, being advised to have a mammogram, and having had a Pap smear; Behavioral characteristics including trusting cancer information from doctors, looking for cancer information, perception of chance of getting breast cancer, eating habits (consumption of fruits and vegetables), having exercised in the last month, and lifetime number of smoked cigarettes; and Knowledge of breast cancer/mammography including knowing the age at which mammography should begin and the frequency of receiving mammograms.
Statistical analysis
HINTS data include a set of 50 replicate weights, which were generated according to jackknife variance estimation [9]. Data were weighted to produce overall and stratified estimates that represent the U.S. population. We incorporate weights in these analyses for the population study.
We first examined bivariate associations between all potential independent variables and response variables to select significant covariates for inclusion in subsequent models and to assess collinearity. We used Rao-Scott corrections to Chi squared tests to incorporate the survey design (50 jackknife weights) of the HINTS data. Design-based multiple logistic regression models incorporating the 50 jackknife weights [10, 11] were then developed to identify significant factors associated with (1) adherence to mammography and (2) thinking about getting a screening mammogram in non-adherent women. For the first response variable, we built separate models and compared results between those less than 65 years and those ages 65 and older. We used the Wald tests [11] to determine the statistical significance of each coefficient in the model.
We defined adherence to mammography (γ) separately for women aged 40 and 41 years versus those aged 42 and older, as a women aged 40 or 41 without any mammography history can still be considered adherent if she plans to get a mammogram in the near future (2 years or 1 year respectively). We defined a woman older than 42 as adherent if the interval between her most recent self-reported mammogram and the next expected mammogram was less than two years. Otherwise, she was considered non-adherent. We categorized those who answered the question “Do you have a plan to get mammography” with “undecided” or “not planned” as non-adherent.
For the outcome measure of thinking about getting a mammogram in non-adherent women (τ), we narrow our attention to women who never had a mammogram or their most recent mammogram was more than 2 years ago. The response variable is one if the answer to the question “Have you thought about getting a mammogram” is yes, or zero otherwise.
To handle missing values for the predicting factors, we use the naive nearest neighbor hot deck method, which takes advantage of the similarity between the observations to impute the missing values. Each missing value is replaced with the observed response from the nearest observation in the dataset [12].
We used classification tables [11] to evaluate the performance of the logistic regression models. We considered a predicted value of 0.5 as the cut off point for our classification analyses. Suppose \( \hat{\gamma }_{1} \) and \( \hat{\gamma }_{2} \) represent the predicted values from the regression models for adherence in women younger than 65 and women aged 65 and older, respectively. We consider a woman younger than 65 (or 65 and older) to be adherent if her probability to be adherent, \( \hat{\gamma }_{1} ({\text or}\, \hat{\gamma }_{2} ), \) is greater than 0.5 and non-adherent otherwise. The same strategy is implemented for the outcome “thinking about getting a mammogram” (τ) in non-adherent women. The observed values for the dependent outcomes and the predicted values are then cross-classified to evaluate the predictive accuracy of the models. All analyses are performed at the significance level of 5 %.
Results
The distributions of all predicting factors for the two response variables are presented in Table 1. There are a total of 2,370 women included for the adherence to mammography response variable and 451 women included for the thinking about getting a mammogram response variable.
Comparing mammography adherence among women in the two age groups
The logistic regression results (Table 2) suggest that in the socio-demographic characteristics category, women who are single, separated, divorced, or widowed are less likely to adhere to screening mammography compared to married women in both age groups (OR = 0.685 and OR = 0.499 for women younger than 65 and women aged 65 and older, respectively). As income increases, adherence to screening mammography also increases. Specifically, among women younger than 65, the difference between women with income more than $75,000 and women whose income is less than $25,000 is significant (OR = 2.526 for income greater than $75,000 versus income less than $25,000). Women younger than 65 who have health insurance are also more likely to adhere to screening mammography (OR = 2.959).
For the health-related characteristics, as the number of visits to a health care provider increases, women are more likely to adhere to screening mammography (OR = 2.358 for women younger than 65 with more than five visits to doctor per year versus women with less than two visits per year). Being advised to have mammogram is the strongest factor in this category (OR = 5.298 and 10.711 for women younger than 65 and women aged 65 and older, respectively compared to women who are not advised). Women who have had a prior Pap smear are more adherent than those who have not (OR = 3.203 and OR = 3.809 for women younger than 65 and women aged 65 and older, respectively).
For the behavioral characteristics, women who trust the cancer information from their doctor “a little,” “some,” and “a lot” are 6.727, 13.194, and 14.824 times more likely to adhere compared to women who do not trust their doctor at all. Women who have an increased risk perception of breast cancer are more adherent. For women younger than 65, the corresponding ORs for women with “moderate” and “high” risk perception are 1.519 and 1.541, respectively. The corresponding values for women older than 65 are 1.645 and 3.036, respectively. Women younger than 65, who have smoked at least 100 cigarettes in their lifetimes are less likely to be adherent (OR = 0.687).
For the knowledge-related class of factors, women whose answer to the appropriate interval between two subsequent mammograms is other than every one or two years are less likely to adhere. The corresponding odds ratios are 0.812 and 0.636 for women younger than 65 and women aged 65 and older, respectively.
Thinking about getting a mammogram in non-adherent women
In the bivariate analysis, age, marital status, income, and insurance are among the variables, which proved to be significant in the socio-demographic class of factors. In the health-related class of factors, being advised to have a mammography and having had Pap smear are statistically significant in bivariate analyses. Looking for cancer information, risk perception of breast cancer, lifetime number of smoked cigarettes, and exercise in the past month are significant factors in the bivariate analyses in the behavioral characteristics class.
However, in the multiple logistic regression analyses (Table 3), the only significant factor is age. As women’s age increased, they reported thinking about getting mammograms less often. Women ages from 60 to 69 years, and older than 70 years are 0.377 and 0.112 times less likely to think about getting a mammogram compared to women aged from 42 to 49 years.
Evaluation of regression models
Tables 4 and 5 present the classification tables for the first response variable and the second response variable, respectively. Sensitivity, specificity, and accuracy of the proposed logistic regression models are presented in the tables. Note that the numbers presented in the tables are weighted according to the replication jackknife weights in the data to be representative of the national population. For example, the number 4,727,850 in Table 4 is the number of non-adherent women younger than 65 who are correctly classified as non-adherent by the design-based logistic regression.
As the results show, for the adherence to mammography response variable, the proposed design-based logistic regression models correctly classify 77.7 % of women younger than 65 and 80.5 % of women aged 65 and older. For the thinking about getting a mammogram response variable, 74.43 % of women are correctly classified.
Discussion
In this study, we evaluated the association between women’s adherence to mammography screening and four classes of factors including various socio-demographic, health related, behavioral characteristics, and knowledge of breast cancer/mammography factors using the 2003 HINTS data.
In the literature, definitions of adherence to mammography screening vary widely across studies. Zapka et al. [13] and Wu et al. [14] defined adherence based on the ACS guideline, “had a mammogram in the last year.” Maxwell et al. [15], Murabito et al. [16], Tejeda et al. [17], Schonberg et al. [18], and Vyas et al. [19], considered “had a mammogram in the past two years” as a measure of adherence, which is consistent with the USPSTF guideline. Wu et al. [14], Maxwell et al. [15], Tejeda et al. [17], and Meissner et al. [20] considered “ever had a mammogram” to measure women’s decisions in mammography participation. However, this measure cannot be interpreted as the adherence to mammography guidelines, since it does not incorporate a specific time interval. Other time intervals are also considered in the literature. For example, Harrison et al. [21] defined “had any mammogram in the preceding 5-year period” as their response variable. Many studies defined adherence based on “ever had” or “the most recent” mammogram rather than considering whether the women returned for repeat mammography or not. To bridge this gap, Carney et al. [22] defined the response variable as “returning for a screening mammogram within 24 months of the initial exam” and identified factors that had significant effect, such as health insurance coverage, first degree relatives with breast cancer, and knowledge about breast cancer. In other studies, Allen et al. [23, 24] explored the relationship between mammography use and social network characteristics, while considering “receipt of at least two mammograms, the most recent of which was within the past 2 years with a maximum interval of 2 years between screenings” as the adherence measure. Rakowski et al. [25] considered “two exams on schedule, based on an every-other-year interval” in their study. A systematic literature review of the studies on the mammography use and the associated factors published from 1988 to 2004 was completed by Schueler et al. [26]. In summary, they found that the strongest predictors of mammography use were past screening behavior (clinical breast examination and Pap test), having access to a physician and having a physician-recommend mammography. These results are in line with our findings as the design-based logistic regression result shows that “having been advised to get mammogram,” “have had Pap test” are the two most important factors. We also found that “perception of chance of getting breast cancer,” “income,” “insurance,” and “knowledge about mammography” are significant factors.
Most of these studies used data at the local, regional, or state level, making the national generalizations difficult. In addition, these studies did not consider if a woman underwent a mammogram because she intended to do so, or for a diagnostic purpose (e.g. after the woman had felt a lump in her breast), or because her doctor prescribed the mammogram. In addition, for the studies that used longitudinal data (sequential mammograms), it is difficult to keep track of women who died, moved, etc. This can potentially cause bias in the data analysis, and as a result, these measures may not truly represent women’s adherence to mammography guidelines.
This study differs from prior studies [13–25] in that adherence is defined based on women’s intention and plans of obtaining mammograms rather than their mammography history behavior. Results from our work will likely help decision makers to differentiate between women who are concerned about mammography and have regular plans for getting mammograms from those who are not concerned. The results of this analysis can help policy makers identify non-adherent populations. We also examine the relationship between aforementioned four classes of factors with women’s attitudes toward getting mammograms for women with poor mammography history. By characterizing the factors associated with attitudes toward mammography in the non-adherent population, policy makers can differentiate between the women who are concerned about receiving a mammogram, but may have some barriers versus those who are not concerned at all.
As for the limitations of our study, it is based on self-reported data and may yield biased results if a woman did not report the exact time of her last mammogram. We also used the 2003 HINTS dataset, since it is the only HINTS data that provide information on women’s intention toward mammography.
Adherence to screening mammography is lower among minorities [27]. Based on the 2010 National Health Interview Survey, 69.4 % of American Indian/Alaska native women and 64.1 % of Asian women had a mammogram between 2008 and 2010, while participation rates among white and black women were about 72.8 and 73.2 %, respectively [28]. Our results also imply that the percent of women intending to have regular screening mammography is lower in races other than white and black. However, we do not have enough evidence to conclude that these differences are statistically significant. The results reveal that for both age groups, married women are more likely to comply with the mammography guidelines. For women younger than 65, financial aspects such as insurance and income are also significant factors the policy makers should consider for improving adherence.
Physicians’ involvement in achieving mammography adherence is important. However, many physicians do not make referrals at the recommended intervals, even though they may endorse the guidelines [29]. Our results show that prior advice to have a mammogram by the woman’ physician is the most significant factor in health-related class of factors. This suggests that to enhance women’s adherence, doctors should recommend that their patients have regular screening mammograms. Mammography referrals are more frequent for women who have access to the health care system (i.e. women with regular physician and health insurance), but less frequent among vulnerable women, (i.e. older women with lower educational attainment, or lower annual family income [30]). It would be worth investigating the factors associated with low mammogram referral rates by physicians. Having history of Pap smear was found to be significant for both age groups. This is in line with a previous study by Augustson et al. [31], in which they characterize the association among clinical breast exam (CBE), Pap smear, fecal occult blood testing (FOBT) adherence, and mammography adherence. Therefore, low compliance with other cancer screenings can help identify women in need of additional interventions to improve mammography adherence. Although the number of visits to a health provider is significant for women younger than 65, this factor is not significant for older women. This is interesting as older women, regardless of being adherent or not, are expected to visit their doctors more frequently than younger women because of aging associated diseases.
In the behavioral characteristics class, “lifetime number of smoked cigarettes” is a significant factor for younger women, but not for older women. Trusting doctor’s information about cancer is proved to be significant for younger women; however, we do not have enough evidence to say that it is also significant for older women. Previous studies differ about whether fear motivated or inhibits precautionary behaviors. McCaul et al. [32] tested different predictors in the context of fear of breast cancer and breast cancer screening and showed that greater fear was related to higher levels of screening intentions and behaviors. Our data analysis confirms this finding and shows that risk perception of breast cancer is a significant predictor on intention of getting regular mammograms for both age groups.
For the last class of covariates, as expected, knowledge about frequency of getting mammograms is significant. Thus, increasing women’s knowledge about breast cancer and mammography recommendations is also likely to significantly influence women’s adherence.
For the second response variable (thinking about getting a mammogram in non-adherent women), we found little difference between women who are and are not concerned about getting mammograms. For this response variable, younger women are more likely to think about obtaining a mammogram. Women who have been advised to get a mammogram before and those who are looking for cancer information may be more concerned about getting mammograms, although these findings are not statistically significant.
This study, considering women’s attitudes and behaviors toward mammography, enables decision makers to identify barriers that women may face to obtain a screening mammogram and also allows for the identification of characteristics of non-adherent women who are not concerned about getting a mammogram. Our findings suggest that the most significant factors influencing women’s compliance are being advised to have a mammogram and insurance. The former has been applied on a systematic level in some European countries (e.g. the UK, Sweden, and Norway), which have organized population-based screening programs, where women are invited through a personal letter for a free mammogram every two or three years [33]. A recent analysis of the European Network for Information on Cancer (EUNICE) data for years 2005, 2006, and/or 2007 (10 national and 16 regional programs for women aged 50–69 in 18 European countries) reported that in 13 of the 26 programs, the participation rate exceeded the European Union benchmark of 70 %, and nine programs achieved a participation level >75 % [34]. According to the CDC, 66.6 and 67.1 % of U.S. women 40 years and over received a mammogram in the past two years based on data from 2005 and 2008, respectively [7]. Although a direct comparison of screening mammography participation rates between European countries and the U.S. is difficult due to difference in recommendations (i.e. age at which to begin screening, interval between mammograms), our results support the benefit of future policies that systematically advise and provide resources to women to receive a mammogram, as it is already done in other countries. Several studies also identified significant factors associated with attendance in population-based mammography programs in European countries (the UK, France, and Sweden) [35–40]. Some of these factors such as income, visiting healthcare providers, having had Pap smear, and perceived risk of breast cancer are also found significant in our analysis. As in most European countries mammography is free, none of these studies reported insurance as an influencing factor for getting a mammogram. However, as our results show, lack of insurance is still a barrier in the U.S. especially for women younger than 65.
In summary, sending reminders and having insurance were shown to be the most influential factors in screening mammography. Other significant factors include marital status, number of visits to health provider a year, having had Pap smear, risk perception of breast cancer, and knowledge of breast cancer/mammography. These findings can help in designing programs aimed at improving screening rates and provide policy makers with data to allow for interventions to remove these barriers and make the targeted population more concerned about getting breast cancer screenings.
References
American Cancer Society, Available at: http://www.cancer.org/Cancer/BreastCancer/OverviewGuide/breast-cancer-overview-key-statistics. Accessed 30 March 2013
Gøtzsche PC, Nielsen M (2009) Screening for breast cancer with mammography. Cochrane Database Syst Rev 4:1
Center for Disease Control and Prevention, The National Breast and Cervical Cancer Early Detection Program, Available at: http://www.cdc.gov/cancer/nbccedp. Accessed March 2013
American Cancer Society web site. Available at: http://www.cancer.org/healthy/findcancerearly/cancerscreeningguidelines/american-cancer-society-guidelines-for-the-early-detection-of-cancer. Accessed 25 May 2013
The US Preventive Services Task Forces. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrca.htm. Accessed 25 May 2013
Isaacs C, Peshkin BN, Schwartz M, DeMarco TA, Main D, Lerman C (2002) Breast and ovarian cancer screening practices in healthy women with a strong family history of breast or ovarian cancer. Breast Cancer Res Treat 71(2):103–112
Center for Disease Control and Prevention. Available at: http://www.cdc.gov/nchs/fastats/mamogram.htm. Accessed 27 June 2013
Becker MH, Maiman LA (1975) Socio-behavioral determinants of compliance with health and medical care recommendations. Med Care 13:10–24
Nelson D, Kreps G, Hesse B, Robert C, Gordon W, Neeraj A, Barbara R, Vishwanath vK, Neil W, Sara A (2004) The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun 9:443–460
Roberts G, Rao JNK, Kumar S (1987) Logistic regression analysis of sample survey data. Biometrika 74(1):1–12
Hosmer DW, Lemeshow S (2000) Applied logistic regression, 2nd edn. Wiley, New York
Andridg RR, Little RJA (2010) A Review of Hot Deck Imputation for Survey Non-response. Int Stat Rev 78(1):40–64
Zapka JG, Hosmer D, Costanza ME (1992) Changes in mammography use: economic, need, and service factors. Am J Public Health 82(10):1345–1351
Wu H, Zhu K, Jatoi I, Shah M, Shriver CD, Potter J (2007) Factors associated with the incompliance with mammogram screening among individuals with a family history of breast cancer or ovarian cancer. Breast Cancer Res Treat 101(3):317–324
Maxwell CJ, Bancej CM, Snider J (2001) Predictors of mammography use among Canadian women aged 50–69: findings from the 1996/97 National Population Health Survey. Can Med Assoc J 164(3):329–334
Murabito JM, Evans JC, Larson MG, Kreger BE, Splansky GL, Freund KM, Mark AM, Wilson PW (2001) Family breast cancer history and mammography Framingham offspring study. Am J Epidemiol 154(10):916–923
Tejeda S, Thompson B, Coronado GD, Martin DP, Heagerty PJ (2009) Predisposing and enabling factors associated with mammography use among hispanic and non-hispanic white women living in a rural area. J Rural Health 25(1):85–92
Schonberg MA, McCarthy EP, York M, Davis RB, Marcantonio ER (2007) Factors influencing elderly women’s mammography screening decisions: implications for counseling. BMC Geriatr 7(1):26
Vyas A, Madhavan S, LeMasters T et al (2011) Factors influencing adherence to mammography screening guidelines in appalachian women participating in a mobile mammography program. J Community Health 37(3):632–646
Meissner HI, Breen N, Taubman ML, Vernon SW, Graubard BI (2007) Which women aren’t getting mammograms and why? (United States). Cancer Causes Control 18(1):61–70
Van Harrison R, Janz NK, Wolfe RA, Tedeschi PJ, Huang X, McMahon LF (2003) 5-Year mammography rates and associated factors for older women. Cancer 97(5):1147–1155
Carney PA, Harwood BG, Weiss JE et al (2002) Factors associated with interval adherence to mammography screening in a population-based sample of new hampshire women. Cancer 95(2):219–227
Allen JD, Stoddard AM, Sorensen G (2008) Do social network characteristics predict mammography screening practices? Health Educ Behav 35(6):763–776
Allen JD, Sorensen G, Stoddard AM (1999) The relationship between social network characteristics and breast cancer screening practices among employed women. Ann Behav Med 21(3):193–200
Rakowski W, Meissner H, Vernon SW et al (2006) Correlates of repeat and recent mammography for women ages 45–75 in the 2002–2003 Health Information National Trends Survey (HINTS 2003). Cancer Epidemiol Biomarkers Prev 15(11):2093–2101
Schueler KM, Chu PW, Smith-Bindman R (2008) Factors associated with mammography utilization: a systematic quantitative review of the literature. J Women’s Health 17(9):1477–1498
Phillips CE, Rothstein JD, Beaver K et al (2011) Patient navigation to increase mammography screening among inner city women. J Gen Intern Med 26(2):123–129
Center for Disease Control and Prevention, National Health Interview Survey, United States, 2010. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6103a1.htm. Accessed 3 July 2013
Blechman EA, Brownell KD (1998) Behavioural medicine and women: a comprehensive handbook. Guilford Press, New York
O’Malley MS, Earp JA, Hawley ST et al (2001) The association of race/ethnicity, socioeconomic status, and physician recommendation for mammography: who gets the message about breast cancer screening? Am J Public Health 91(1):49
Augustson EM, Vadaparampil ST, Paltoo DN et al (2003) Association between CBE, FOBT, and Pap smear adherence and mammography adherence among older low-income women. Prev Med 36(6):734–739
McCaul KD, Reid PA, Rathge RW et al (1996) Does concern about breast cancer inhibit or promote breast cancer screening? Basic Appl Soc Psychol 18(2):183–194
Perry N, Broeders M, deWolf C, et al. (2006) European guidelines for quality assurance in breast cancer screening and diagnosis. [Printed in Belgium]. European Communities 2006. http://ec.europa.eu/health/ph_projects/2002/cancer/fp_cancer_2002_ext_guid_01.pdf. Accessed 6 Dec 2013
Giordano L, von Karsa L, Tomatis M et al (2012) Mammographic screening programmes in Europe: organization, coverage and participation. J Med Screen 19(suppl 1):72–82
Duport N (2012) Characteristics of women using organized or opportunistic breast cancer screening in France. Analysis of the 2006 French Health, Health Care and Insurance Survey. Rev Epidemiol Sante Publique 60(6):421–430
Zackrisson S, Lindström M, Moghaddassi M et al (2007) Social predictors of non-attendance in an urban mammographic screening programme: a multilevel analysis. Scand J Public health 35(5):548–554
Lagerlund M, Maxwell AE, Bastani R (2002) Sociodemographic predictors of non-attendance at invitational mammography screening—a population-based register study (Sweden). Cancer Causes Control 13(1):73–82
Lagerlund M, Widmark C, Lambe M et al (2001) Rationales for attending or not attending mammography screening-a focus group study among women in Sweden. Eur J Cancer Prev 10(5):429–442
Aro AR, de Koning HJ, Absetz P et al (1999) Psychosocial predictors of first attendance for organised mammography screening. J Med Screen 6(2):82–88
Lidbrink E, Frisell J, Brandberg Y, Rosendahl I, Rutqvist LE (1995) Nonattendance in the Stockholm mammography screening trial: relative mortality and reasons for nonattendance. Breast Cancer Res Treat 35(3):267–275
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Madadi, M., Zhang, S., Yeary, K.H.K. et al. Analyzing factors associated with women’s attitudes and behaviors toward screening mammography using design-based logistic regression. Breast Cancer Res Treat 144, 193–204 (2014). https://doi.org/10.1007/s10549-014-2850-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-014-2850-9