Abstract
The optimal method for locoregional staging in patients treated with neoadjuvant chemotherapy (NAC), usually ultrasound (US) and pre- or post-chemotherapy sentinel lymph node biopsy (SLNB), remains subject of debate. The aim of this study was to assess the value of 18F-FDG PET/CT for detecting locoregional lymph node metastases in primary breast cancer patients scheduled for NAC. 311 breast cancer patients, scheduled for NAC, underwent PET/CT of the thorax in prone position with hanging breasts. A panel of four experienced reviewers examined PET/CT images, blinded for other diagnostic procedures. FDG uptake in locoregional nodes was determined qualitatively using a 4-point scale (0 = negative, 1 = questionable, 2 = moderately intense, and 3 = very intense). Results were compared with pathology obtained by US-guided fine needle aspiration or SLNB prior to NAC. All FDG-avid extra-axillary nodes were considered metastatic, based on the previously reported high positive predictive value of the technique. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of FDG-avid nodes for the detection of axillary metastases (score 2 or 3) were 82, 92, 98, 53, and 84 %, respectively. Of 28 patients with questionable axillary FDG uptake (score 1), 23 (82 %) were node-positive. Occult lymph node metastases in the internal mammary chain and periclavicular area were detected in 26 (8 %) and 32 (10 %) patients, respectively, resulting in changed regional radiotherapy planning in 50 (16 %) patients. In breast cancer patients scheduled for NAC, PET/CT renders pre-chemotherapy SLNB unnecessary in case of an FDG-avid axillary node, enables axillary response monitoring during or after NAC, and leads to changes in radiotherapy for a substantial number of patients because of detection of occult N3-disease. Based on these results, we recommend a PET/CT as a standard staging procedure in breast cancer patients scheduled for NAC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The TNM staging system is generally used for classification, prognostication, and treatment planning in breast cancer patients [1]. The 5-year relative survival rate decreases according to stage at presentation from 99 % in node-negative disease to 84 % in node-positive disease, and 23 % in distant disease [2]. An increase in the number of tumor-positive axillary nodes is related to a worsened prognosis irrespective of primary tumor size [3]; the presence of a tumor-positive internal mammary node (IMN) or periclavicular node results in a further decrease in survival [4–6]. Although IMN involvement is of prognostic significance, IMN biopsy and irradiation are still controversial because of lack of established survival benefit and increased morbidity [6–10].
Neoadjuvant chemotherapy (NAC) is standard of care in locally advanced breast cancer (LABC) and is increasingly used in larger operable breast cancer [11–13]. Because of the administration of chemotherapy before surgical treatment, a different strategy for locoregional nodal staging is required as compared with treatment without NAC. Ultrasound (US) with fine needle aspiration (FNA) of axillary and periclavicular nodes is routinely performed prior to NAC, but its accuracy in the detection of metastases is suboptimal [14–16]. Sentinel lymph node biopsy (SLNB) before NAC can accurately stage axillary and internal mammary nodes and enables determination of axillary response following NAC, but it requires an additional surgical procedure [17–19]. Furthermore, if a tumor-positive pre-chemotherapy SLNB is routinely followed by post-chemotherapy axillary lymph node dissection (ALND), overtreatment occurs in patients with a complete axillary response to NAC [20]. SLNB can be performed after NAC as well, determining final axillary status and resulting in less invasive axillary treatment in patients with complete axillary response. It should be noted that the identification rate is suboptimal (81–94 %) and the false negative rate is relatively high (14–20 %), especially in (clinically) node-positive patients [21, 22]. Also, uncertainty remains for the other axillary nodes as they receive no further treatment in case of a negative post-chemotherapy sentinel node, although they might have been tumor-positive before start of NAC [20].
Positron emission tomography (PET), with or without computed tomography (CT), using 18F-fluorodeoxyglucose (FDG) is useful for the detection of axillary metastases in early breast cancer [23], but knowledge of its value for locoregional staging in large or node-positive breast cancer prior to NAC is limited [16, 19, 24–28]. The aim of this study was to assess the accuracy of FDG PET/CT to visualize axillary and extra-axillary lymph node metastases in breast cancer patients scheduled for NAC. Second, we aimed to determine how often TNM-stage and treatment had to be changed because of PET/CT findings.
Patients and methods
Patients
Women who presented with primary invasive breast cancer >3 cm and/or at least one tumor-positive node were offered to receive NAC in the context of one of several trials of NAC [29]. In case of eligibility for NAC, an FDG PET/CT was performed [24]. Patients without accurate pathological staging of the axilla prior to NAC (i.e., SLNB in case of negative FNA) were excluded from this analysis. The institutional review board approved this study and informed consent was obtained from all patients.
Conventional staging
Primary tumor characteristics were determined by histological biopsies. The size of the primary tumor was determined with contrast-enhanced magnetic resonance imaging (CE-MRI). The axillary lymph node status was primarily assessed with US and concomitant FNA of suspect nodes (cortex thickening ≥2.3 mm) within 2 weeks before PET/CT. When FNA cytology showed absence of tumor cells, a pre-chemotherapy SLNB was performed, preferably after PET/CT, but always within 2 weeks of PET/CT. Cytology or histology of IMNs was obtained in case of a suspect (enlarged) IMN on CE-MRI or in case of drainage to the internal mammary chain on lymphoscintigraphy. The periclavicular region was examined using US and FNA. Bone scintigraphy, US of the liver, and chest radiography were used to exclude the presence of distant metastases.
Nodes harvested by SLNB were fixed in formalin, bisected, embedded in paraffin, and cut at a minimum of six levels at intervals of 50–150 μm. Deferred pathological evaluation included hematoxylin–eosin and immunohistochemical staining (CAM5.2). Analysis of conventional imaging and pathology was performed without PET/CT information.
Treatment
NAC regimens were employed as previously described [29]. Briefly, most HER2-negative tumors received six courses of cyclophosphamide and doxorubicin, administered in a dose-dense schedule (every 2 weeks). All human epidermal growth factor receptor 2 (HER2)-positive tumors were treated with a trastuzumab-based regimen, mainly consisting of three 8-week courses of weekly paclitaxel, trastuzumab, and carboplatin. Following NAC, breast-conserving or ablative surgery was performed. An ALND was performed in initially node-positive patients.
18F-FDG PET/CT
The PET/CT was performed after a fasting period of 6 h with a blood glucose level <10 mmol/l. An FDG dose of 180–240 MBq was given intravenously, depending on body mass index. Ten minutes before FDG injection, 10 mg diazepam was administered orally to prevent FDG uptake in brown fat and muscle. The PET/CT was acquired after a resting period of 60 ± 10 min. Using a whole-body PET/CT scanner (Gemini TF, Philips, Cleveland, USA), a PET scan (3.00 min per bed position) of the thorax was performed for locoregional assessment with the patient in prone position, with hanging breasts and the arms above the head, with image reconstruction to 2 × 2 × 2 mm voxels. This approach provides high-resolution images of the breasts and regional lymph node areas without tissue compression or breathing motion [30]. PET acquisition was preceded by a low-dose CT (40 mAs) with 2.0-mm slices. Subsequently, a standard whole-body PET/CT (1.30 min per bed position and 5.0 mm CT slices) was performed from the base of the skull to the upper half of both femora in supine position for staging purposes.
Image reading
A panel of experienced readers evaluated the images using orthogonal multiplanar reconstruction and simultaneous display of PET, CT, and fused PET/CT images. Reviewers were blinded for other diagnostic procedures. First, FDG uptake in locoregional nodes was qualitatively assessed using a 4-degree scoring system [16]: (0) similar to surrounding tissue or lymph nodes, (1) slightly more than surrounding structures, (2) moderately intense, and (3) very intense. In addition, the FDG-avid lesion was measured using maximum standardized uptake values (SUVmax). The diameter of FDG-avid IMNs and periclavicular nodes were determined on low-dose CT images, based on corresponding PET/CT images.
Data analysis
Qualitative and quantitative axillary FDG uptake was compared with pathology. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of PET/CT in the detection of axillary metastases were calculated. To compare the proportion of missed axillary metastases between subgroups, Fisher’s exact (two variables), Pearson chi-square (three or more nominal variables), and linear-by-linear association tests (three or more ordered variables) were used. Because of previously reported high specificity and positive predictive value of the technique and the difficulty of pathological verification in the majority of extra-axillary nodes, all FDG-avid nodes in this region were considered metastatic [23]. The Mann–Whitney test was used to test the difference in size of US-detected periclavicular nodes and those exclusively detected by PET/CT. To compare in which subgroups of patients PET/CT detected occult N3-disease, Fisher’s exact (two variables), Pearson chi-square (three or more nominal variables), and linear-by-linear association tests (three or more ordered variables) were used.
Results
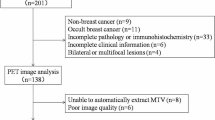
311 patients who underwent a PET/CT between September 2007 and October 2011 were included in this analysis. PET/CT images of locoregional nodes are demonstrated in Fig. 1.
Fused PET/CT (left column) and corresponding low-dose CT (right column) images of locoregional lymph node involvement. a, b Intense FDG uptake in right axillary node; c, d faint FDG uptake in left axillary node; e, f intense FDG uptake in right internal mammary node; g, h intense FDG uptake in left infraclavicular node
Baseline characteristics are presented in Table 1. In 32 patients with metastatic disease (stage IV), PET/CT and conventional staging (bone scintigraphy, chest radiography, and US of the liver) were in accordance in five patients; PET/CT detected additional lesions in four metastatic patients, and PET/CT was the only modality detecting metastases in 23 patients. Twelve (38 %) of 32 patients did not undergo surgery, whereas 18 patients (56 %) received additional or changed treatment (adjusted chemotherapeutic regimens, additional radiotherapy). In 2 patients, treatment was not changed (mediastinal metastases within the planned radiation field).
Axilla
Assessment of axillary nodes with PET/CT was impossible in 21 patients (SLNB before PET/CT—7 macrometastases, 2 micrometastases, 12 tumor-negative). No increased FDG uptake (score 0) was seen in 62 (21 %) of 290 patients. Slightly increased FDG uptake (score 1) was seen in 28 (10 %) patients and corresponded with SUVmax values ranging from 1.6 to 3.0. Intense FDG uptake (score 2–3) was seen in 200 (69 %) patients, corresponding with SUVmax of 2.1–24.4. The comparison between PET/CT (score 2–3) and histopathology is shown in Fig. 2 and Table 2. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of FDG-avid axillary nodes in the detection of lymph node metastases were 82, 92, 98, 53, and 84 %, respectively. In 23 (82 %) of 28 patients with score 1 FDG uptake, pathology showed axillary metastases. Of 62 axillae without increased FDG uptake (score 0), 19 (31 %) were tumor-positive. All patients having an axillary node with SUVmax ≥ 3.8 were node-positive.
The proportion of missed axillary metastases with PET/CT was significantly lower in patients with N2- or N3-disease, invasive ductal carcinomas, Ki67 > 10 %, and grade 3 tumors. Triple negative and HER2-positive tumors were less often associated with missed axillary metastases (p = 0.011). A larger false negative rate was seen in tumors with no or slightly increased primary tumor FDG uptake (p = 0.006). Table 3 presents the number of correctly classified and missed axillary metastases with PET/CT of different subgroups.
Internal mammary nodes
The internal mammary chain was evaluable with PET/CT in 310 patients (IMN SLNB prior to PET/CT in one patient). US/FNA, based on enlarged nodes on CE-MRI, found an IMN metastasis in 3 patients. Of these, two revealed intense FDG uptake. In the remaining 307 patients, PET/CT visualized intense FDG uptake in at least one IMN in 27 patients. The median size of FDG-avid IMNs was 7 mm (interquartile range [IQR] 4 mm). An SLNB in the internal mammary chain was performed in one of 27 patients, which was tumor-negative. In one patient without FDG uptake in IMNs, SLNB after PET/CT revealed a metastasis. Based on intense FDG uptake, new IMN involvement was detected in 26 (8 %) of 311 patients. A flowchart of IMN involvement is presented in Fig. 3.
Periclavicular lymph nodes
US/FNA in the periclavicular region was tumor-positive in 31 (10 %) patients, of which 30 (97 %) showed intense FDG uptake. In the remaining 280 patients, PET/CT visualized intense FDG-avid periclavicular nodes in 32 (10 %) patients. Targeted US with FNA of FDG-avid nodes following PET/CT was performed in four patients, all revealing tumor-positive nodes. The median size of periclavicular nodes discovered by US and PET/CT and by PET/CT only was 10 mm (IQR 6.5 mm) and 9 mm (IQR 4 mm), respectively (p = 0.246). Figure 4 presents a flowchart of periclavicular node involvement.
Change in TNM-stage and treatment
A total of 58 new suspect N3-nodes (26 IMNs, 32 periclavicular nodes) were detected by PET/CT in 56 (18 %) patients (new suspect nodes in both the internal mammary chain and in the periclavicular region in 2 patients). New N3-nodes were significantly more often detected in patients with a larger primary tumor and a higher stage. No difference in detection of occult N3-disease was found for different histologic types, clinical subtypes, P53, Ki-67, or grade. The N-stage was altered in 48 of 56 patients, since PET/CT discovered IMN involvement in 8 patients who were already classified as N3 because of US-detected periclavicular metastases. The TNM-stage was changed by PET/CT in 38 (12 %) patients because of newly discovered N3-disease; 10 patients were already classified as stage IV because of distant metastatic disease. Radiotherapy treatment was changed in 50 (16 %) patients because of involvement of internal mammary or periclavicular nodes, including four patients with oligometastatic disease (1 patient with a single bone metastasis, 3 patients with a single mediastinal metastasis), who were treated with curative intent as well. The detection of occult N3-disease and changed stage and radiotherapy treatment for different subgroups are presented in Table 4.
Discussion
Accurate evaluation of locoregional and distant spread of breast cancer remains essential because of its implications for treatment and prognosis. Staging of axillary lymph nodes can be done relatively reliably [17], but the assessment of lymph nodes in the internal mammary chain and periclavicular region remains a challenge [9, 15]. Particularly if NAC is applied, a different strategy for lymph node staging may be required: detection of axillary and extra-axillary nodes using US is suboptimal and controversy remains regarding timing of SLNB (either pre- or post-chemotherapy). The results from this study show that PET/CT could significantly contribute to fill these gaps by reliably assessing the presence of axillary lymph node metastases prior to NAC, enabling axillary response monitoring during or after therapy, and accurately visualizing periclavicular and internal mammary nodes, thereby upstaging a substantial proportion of patients.
Axillary staging of early breast cancer patients with PET and PET/CT has been investigated earlier [23]. While sensitivity was suboptimal (37–95 %), specificity is consistently reported high (84–100 %). Although an FDG-avid axillary node could provide an indication for ALND instead of SLNB, standard use of PET/CT in early breast cancer is not recommended [31]. Evidence on the accuracy of PET/CT in the detection of axillary metastases in large or locally advanced tumors is limited [19, 25, 27, 28]. This study shows that both specificity (92 %) and positive predictive value (98 %) of PET/CT for the detection of axillary metastases in patients with primary breast cancer scheduled for NAC are high. Replacement of pre-chemotherapy SLNB by PET/CT enables non-invasive, accurate axillary staging and allows axillary response determination, which is an important prognosticator [32]. If an SLNB is omitted in case of axillary FDG-uptake, the node is left in situ and axillary response monitoring during or after NAC could be performed [19, 20, 32, 33].
Axillary nodes with faint FDG uptake (score 1) were found to be metastatic in 82 %. In our opinion, this is too low to recommend omission of an SLNB, since 18 % of patients with a tumor-negative axilla will undergo ALND. Therefore, combined with the relatively high false negative rate of post-chemotherapy SLNB, we recommend to perform an SLNB prior to NAC in case of an axillary node with no or slightly increased FDG uptake.
From research on FDG uptake in primary tumors it is known that tumors with aggressive characteristics show a higher degree of FDG uptake [34, 35]. As NAC is given to advanced, often highly proliferative tumors, we hypothesized that axillary metastases might be more aggressive as well, enhancing its detectability with PET/CT. Although we did find an association of visualization of axillary node metastases with FDG uptake of the primary tumor and prognostic characteristics (Table 3), sensitivity in the whole population was suboptimal. However, the lower false negative rate in tumors with prognostically unfavorable characteristics increases the value of PET/CT for the detection of axillary metastases in this particular subgroup.
The involvement of IMNs has been shown to be prognostically significant [6], but up to now no clear benefit form surgical or radiotherapeutic treatment has been found [9]. Furthermore, irradiation of IMNs results in increased cardiac morbidity [36]. The introduction of internal mammary SLNB has helped to personalize decisions regarding adjuvant therapy. In our population, SLNB detected only two IMN metastases, as compared with 28 with PET/CT (2 metastases confirmed with FNA prior to PET/CT, 26 new suspect nodes). Based on our results PET/CT could help selecting patients for post-operative internal mammary chain radiotherapy.
Several studies have reported on the benefit of radiotherapeutic treatment of periclavicular lymph node metastases [5, 37]. Investigation of the periclavicular region is normally done with US and FNA, which is inaccurate [15]. Use of PET/CT for the detection of extra-axillary lymph node metastases has been investigated previously, but patient groups have been relatively small and the majority of studies used PET alone, lacking anatomical information of the concomitant low-dose CT [16, 25, 38, 39]. Our study, which comprises a large population of patients, shows that PET/CT detects occult periclavicular node involvement in a substantial proportion of patients, changing stage and treatment in the majority of them.
In this study, PET/CT detected new N3-disease in 18 % of patients. Its yield was somewhat lower in stage IIA disease, but this was mainly due to the low yield in T1N1 tumors: new N3-disease was detected in 0 of 21 T1N1 patients and in 5 (11 %) of 47 T2N0 patients. This is in accordance with previous literature on PET/CT and detection of distant metastases [24, 26].
A shortcoming of this study is that most FDG-avid nodes in the internal mammary chain or periclavicular region have not been confirmed to harbor tumor by pathology. Main reasons were the presence of nodes in anatomical sites that were difficult to access by US/FNA, reluctance to plan a further surgical intervention, or the small size of the FDG-avid node. However, previous publications have shown a very high positive predictive value of FDG-avid axillary nodes [23]. The results from this study confirm the high positive predictive value for axillary lymph node evaluation with PET/CT. Since an FDG-avid axillary node is highly predictive for lymph node metastasis, this finding can be extrapolated for IMNs and periclavicular nodes. Furthermore, of 31 periclavicular lymph nodes detected with US/FNA in this study, 30 (97 %) was FDG-avid, indicating a high accuracy in detecting N3-disease as well.
We used straightforward visual interpretation to identify lymph node metastases on PET/CT. In addition, basic quantification was performed using SUVmax. While a threshold SUVmax of 2.5 roughly correlated with visual evaluation, this could not provide a more accurate identification of tumor-positive nodes. Furthermore, a fixed SUV threshold tends to have a dependency on variations in FDG biodistribution and image quantification (e.g., renal function, software versions, lesion delineation, scanner brand, and calibration procedures). Although SUVmax is generally used, we have shown that visual interpretation is accurate, providing the easiest implementation in clinical practice.
Conclusion
This study shows that an FDG-avid axillary node on PET/CT in breast cancer patients scheduled for NAC is highly predictive for metastasis, which provides a rationale for omission of pre-chemotherapy SLNB in these patients. Sensitivity and negative predictive value were suboptimal and an SLNB in case of absence of FDG-avid axillary nodes remains important, either before or after NAC. A substantial proportion of patients was upstaged because of the detection of occult lymph node metastases in the internal mammary chain and periclavicular region, changing radiotherapy treatment in the majority of them. Based on these results and prior research on the additional value of PET/CT in the detection of distant metastases, we recommend performing a PET/CT as a standard diagnostic procedure in breast cancer patients scheduled for NAC.
References
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A (eds) (2010) AJCC cancer staging manual, 7th edn. Springer, New York
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62:10–29
Carter CL, Allen C, Henson DE (1989) Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer 63:181–187
Newman LA, Kuerer HM, Fornage B, Mirza N, Hunt KK, Ross MI et al (2001) Adverse prognostic significance of infraclavicular lymph nodes detected by ultrasonography in patients with locally advanced breast cancer. Am J Surg 181:313–318
Brito RA, Valero V, Buzdar AU, Booser DJ, Ames F, Strom E et al (2001) Long-term results of combined-modality therapy for locally advanced breast cancer with ipsilateral supraclavicular metastases: The University of Texas M.D. Anderson Cancer Center experience. J Clin Oncol 19:628–633
Sugg SL, Ferguson DJ, Posner MC, Heimann R (2000) Should internal mammary nodes be sampled in the sentinel lymph node era? Ann Surg Oncol 7:188–192
Veronesi U, Marubini E, Mariani L, Valagussa P, Zucali R (1999) The dissection of internal mammary nodes does not improve the survival of breast cancer patients. 30-year results of a randomised trial. Eur J Cancer 35:1320–1325
Stemmer SM, Rizel S, Hardan I, Adamo A, Neumann A, Goffman J et al (2003) The role of irradiation of the internal mammary lymph nodes in high-risk stage II to IIIA breast cancer patients after high-dose chemotherapy: a prospective sequential nonrandomized study. J Clin Oncol 21:2713–2718
Chen RC, Lin NU, Golshan M, Harris JR, Bellon JR (2008) Internal mammary nodes in breast cancer: diagnosis and implications for patient management—a systematic review. J Clin Oncol 26:4981–4989
Veronesi U, Arnone P, Veronesi P, Galimberti V, Luini A, Rotmensz N et al (2008) The value of radiotherapy on metastatic internal mammary nodes in breast cancer. Results on a large series. Ann Oncol 19:1553–1560
Kaufmann M, von Minckwitz G, Mamounas EP, Cameron D, Carey LA, Cristofanilli M et al (2012) Recommendations from an international consensus conference on the current status and future of neoadjuvant systemic therapy in primary breast cancer. Ann Surg Oncol 19:1508–1516
Mieog JSD, van der Hage JA, van de Velde CJH (2007) Neoadjuvant chemotherapy for operable breast cancer. Br J Surg 94:1189–1200
Fisher B, Bryant J, Wolmark N, Mamounas E, Brown A, Fisher ER et al (1998) Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol 16:2672–2685
Deurloo EE, Tanis PJ, Gilhuijs KGA, Muller SH, Kröger R, Peterse JL et al (2003) Reduction in the number of sentinel lymph node procedures by preoperative ultrasonography of the axilla in breast cancer. Eur J Cancer 39:1068–1073
Altinyollar H, Dingil G, Berberoglu U (2005) Detection of infraclavicular lymph node metastases using ultrasonography in breast cancer. J Surg Oncol 92:299–303
Aukema TS, Straver ME, Peeters MJTFDV, Russell NS, Gilhuijs KGA, Vogel WV et al (2010) Detection of extra-axillary lymph node involvement with FDG PET/CT in patients with stage II–III breast cancer. Eur J Cancer 46:3205–3210
Giuliano AE, Kirgan DM, Guenther JM, Morton DL (1994) Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg 220:391–401
Estourgie SH, Tanis PJ, Nieweg OE, Valdés Olmos RA, Rutgers EJT, Kroon BBR (2003) Should the hunt for internal mammary chain sentinel nodes begin? An evaluation of 150 breast cancer patients. Ann Surg Oncol 10:935–941
Straver ME, Aukema TS, Olmos RAV, Rutgers EJT, Gilhuijs KGA, Schot ME et al (2010) Feasibility of FDG PET/CT to monitor the response of axillary lymph node metastases to neoadjuvant chemotherapy in breast cancer patients. Eur J Nucl Med Mol Imaging 37:1069–1076
Straver ME, Rutgers EJT, Russell NS, Oldenburg HSA, Rodenhuis S, Wesseling J et al (2009) Towards rational axillary treatment in relation to neoadjuvant therapy in breast cancer. Eur J Cancer 45:2284–2292
Gimbergues P, Abrial C, Durando X, Le Bouedec G, Cachin F, Penault-Llorca F et al (2008) Sentinel lymph node biopsy after neoadjuvant chemotherapy is accurate in breast cancer patients with a clinically negative axillary nodal status at presentation. Ann Surg Oncol 15:1316–1321
Pecha V, Kolarik D, Kozevnikova R, Hovorkova K, Hrabetova P, Halaska M, et al. (2011) Sentinel lymph node biopsy in breast cancer patients treated with neoadjuvant chemotherapy. Cancer. doi:10.1002/cncr.26102
Peare R, Staff RT, Heys SD (2010) The use of FDG-PET in assessing axillary lymph node status in breast cancer: a systematic review and meta-analysis of the literature. Breast Cancer Res Treat 123:281–290
Koolen BB, Vrancken Peeters MJTFDV, Aukema TS, Vogel WV, Oldenburg HSA, van der Hage JA et al (2012) 18F-FDG PET/CT as a staging procedure in primary stage II and III breast cancer: comparison with conventional imaging techniques. Breast Cancer Res Treat 131:117–126
Fuster D, Duch J, Paredes P, Velasco M, Muñoz M, Santamaría G et al (2008) Preoperative staging of large primary breast cancer with [18F]fluorodeoxyglucose positron emission tomography/computed tomography compared with conventional imaging procedures. J Clin Oncol 26:4746–4751
Groheux D, Giacchetti S, Espié M, Vercellino L, Hamy A-S, Delord M et al (2011) The yield of 18F-FDG PET/CT in patients with clinical stage IIA, IIB, or IIIA breast cancer: a prospective study. J Nucl Med 52:1526–1534
Ueda S, Tsuda H, Asakawa H, Omata J, Fukatsu K, Kondo N et al (2008) Utility of 18F-fluoro-deoxyglucose emission tomography/computed tomography fusion imaging (18F-FDG PET/CT) in combination with ultrasonography for axillary staging in primary breast cancer. BMC Cancer 8:165
Veronesi U, De Cicco C, Galimberti VE, Fernandez JR, Rotmensz N, Viale G et al (2007) A comparative study on the value of FDG-PET and sentinel node biopsy to identify occult axillary metastases. Ann Oncol 18:473–478
Loo CE, Straver ME, Rodenhuis S, Muller SH, Wesseling J, Vrancken Peeters M-JTFD et al (2011) Magnetic resonance imaging response monitoring of breast cancer during neoadjuvant chemotherapy: relevance of breast cancer subtype. J Clin Oncol 29:660–666
Vidal-Sicart S, Aukema TS, Vogel WV, Hoefnagel CA, Valdes Olmos RA (2010) Added value of prone position technique for PET-TAC in breast cancer patients. Rev Esp Med Nucl 29:230–235
Hodgson NC, Gulenchyn KY (2008) Is there a role for positron emission tomography in breast cancer staging? J Clin Oncol 26:712–720
Rouzier R, Extra J-M, Klijanienko J, Falcou M-C, Asselain B, Vincent-Salomon A et al (2002) Incidence and prognostic significance of complete axillary downstaging after primary chemotherapy in breast cancer patients with T1 to T3 tumors and cytologically proven axillary metastatic lymph nodes. J Clin Oncol 20:1304–1310
Straver ME, Loo CE, Alderliesten T, Rutgers EJT, Vrancken Peeters MTFD (2010) Marking the axilla with radioactive iodine seeds (MARI procedure) may reduce the need for axillary dissection after neoadjuvant chemotherapy for breast cancer. Br J Surg 97:1226–1231
Groheux D, Giacchetti S, Moretti J-L, Porcher R, Espié M, Lehmann-Che J et al (2011) Correlation of high 18F-FDG uptake to clinical, pathological and biological prognostic factors in breast cancer. Eur J Nucl Med Mol Imaging 38:426–435
Gil-Rendo A, Martínez-Regueira F, Zornoza G, García-Velloso MJ, Beorlegui C, Rodriguez-Spiteri N (2009) Association between [18F]fluorodeoxyglucose uptake and prognostic parameters in breast cancer. Br J Surg 96:166–170
Giordano SH, Kuo Y-F, Freeman JL, Buchholz TA, Hortobagyi GN, Goodwin JS (2005) Risk of cardiac death after adjuvant radiotherapy for breast cancer. J Natl Cancer Inst 97:419–424
Olivotto IA, Chua B, Allan SJ, Speers CH, Chia S, Ragaz J (2003) Long-term survival of patients with supraclavicular metastases at diagnosis of breast cancer. J Clin Oncol 21:851–854
Bellon JR, Livingston RB, Eubank WB, Gralow JR, Ellis GK, Dunnwald LK et al (2004) Evaluation of the internal mammary lymph nodes by FDG-PET in locally advanced breast cancer (LABC). Am J Clin Oncol 27:407–410
Çermik TF, Mavi A, Basu S, Alavi A (2008) Impact of FDG PET on the preoperative staging of newly diagnosed breast cancer. Eur J Nucl Med Mol Imaging 35:475–483
Acknowledgments
This study was performed within the framework of CTMM, the Center for Translational and Molecular Medicine (www.ctmm.nl), project Breast Care (Grant 03O-104).
Conflict of interest
The authors have declared no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koolen, B.B., Valdés Olmos, R.A., Elkhuizen, P.H.M. et al. Locoregional lymph node involvement on 18F-FDG PET/CT in breast cancer patients scheduled for neoadjuvant chemotherapy. Breast Cancer Res Treat 135, 231–240 (2012). https://doi.org/10.1007/s10549-012-2179-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2179-1