Abstract
We investigated the association between the risk of locoregional recurrence (LRR) and biological subtypes defined by hormonal receptors (HR) and HER-2 status in women with invasive breast cancer (BC). A total of 618 newly diagnosed BC patients were identified from a cancer registry within a single institution with standardized methods of tumor assessment for estrogen receptor (ER), progesterone receptor (PR), and HER-2. Patients were stratified based on surgical treatment, breast-conserving therapy (BCT) versus modified radical mastectomy (MRM), as well as biological subtypes: HR+/HER-2− (ER-positive or PR-positive, HER-2-negative), HR+/HER-2+ (ER-positive or PR-positive, HER-2-positive), HR−/HER-2+ (ER-negative and PR-negative, HER-2-positive) and TN (ER-negative, PR-negative and HER-2-negative). The association between clinicopathological factors, biological subtype and LRR was evaluated with univariate and multivariate Cox analysis. With a median follow-up of 4.8 years, the rate of LRR was 7.5%. On multivariate analysis, TN, tumor size ≥2 cm and lymph node (LN) positivity were associated with increased risk of LRR (P = 0.023, P = 0.048, and P = 0.0034, respectively). In BCT group, HR−/HER-2+ and LN positivity were associated with increased risk of LRR (HR 11.13; 95% CI 2.78–44.53; P = 0.0007 and HR 5.40; 95% CI 1.67–17.43; P = 0.0048, respectively). In MRM group, TN subtype and LN positivity were associated with increased risk of LRR (HR 4.72; 95% CI 1.53–14.52; P = 0.0069 and HR 3.23; 95% CI 1.44–7.29; P = 0.0047, respectively). Compared to HR+/HER-2−, HR−/HER-2+ treated by BCT and TN treated by MRM showed a significant decrease of 5-year LRR free survival (P = 0.0002 and P = 0.002, respectively). Tumor profiling using ER, PR, and HER-2 biomarkers is a promising tool to identify patients at high risk of LRR based on surgical treatment. Our findings suggest a different follow-up and locoregional treatment for patients with HR−/HER-2+ and TN subtypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Invasive carcinoma of the breast is a heterogeneous group of neoplasms with regards to their molecular alterations, cellular composition, and response to treatment. Conventional clinicopathologic factors, such as, histological grade and type, tumor size, lymph node (LN) involvement, surgical margins, and lymphovascular invasion (LVI) provide prognostic information and are routinely used in decisions regarding locoregional treatment of breast cancer (BC). The clinical heterogeneity of BC creates a challenge in developing tumor classifications based on these variables that are useful with respect to prognosis and prediction of locoregional risk of relapse. As controversies still persist in the locoregional management of BC, the expectation that molecular profiling could further personalize the risk of relapse, improve the locoregional treatment and predict the response to therapy was raised [1–4].
During the last decade, genome-wide analyses using microarrays have revolutionized cancer research. Such studies of invasive breast carcinoma have led to the identification of five so-called “molecular subtypes” characterized by differential gene expression signatures [1, 2], as well as differences in patient survival and response to therapy [3, 5, 6]. As the feasibility of molecular profiling to guide treatment remains unrealistic, recent studies have focused on developing classification based on three biological biomarkers: estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor-2 (HER-2). These readily available biomarkers determined by immunohistochemistry have been used to approximate the molecular subtypes. Among the ER-positive tumors (luminal subtypes), the two major subtypes are luminal A (ER-positive or PR-positive, HER-2-negative) and luminal B (ER-positive or PR-positive, HER-2-positive). They are biologically distinct in that luminal A have higher expression of ER-related genes and a lower expression of proliferative genes than luminal B, such as Ki-67 [7]. The ER-negative tumors (basal subtypes) are subdivided into HER-2 (ER-negative and PR-negative, HER-2-positive) and triple negative (TN)/basal-like carcinomas (ER-negative, PR-negative, and HER-2-negative) [8, 9]. These distinct subtypes have been validated in different patient cohorts and were associated with different outcomes [7, 8, 10]. For instance, HER-2 and TN subtypes, which are more likely grade 3 tumors, appear to be significantly associated with poor outcome compared to luminal A subtype [2].
The potential of integration of BC molecular subtypes into clinical decision making may contribute to tailoring locoregional as well as systemic treatment. The current locoregional treatment decisions are based on clinicopathologic factors and the application of molecular profiling of BC to assess the risk of locoregional recurrence (LRR) is not well developed among women newly diagnosed with BC. There is an urgent need to investigate the risk of LRR associated with each of these BC biological subtypes with the prospect of tailoring the locoregional treatment.
The primary purpose of this study was to determine the impact of BC biological subtypes defined by hormonal receptors (HR; ER and PR) and HER-2 status on risk of LRR in newly diagnosed women with BC treated with either breast-conserving therapy (BCT) or modified radical mastectomy (MRM). Our study highlights the increased risk of LRR associated with HR−/HER-2+ and TN biological subtypes.
Patients and methods
This population-based study included a cohort of HER-2 positive and -negative BC patients treated between January 1998 and December 2003 in a single, comprehensive cancer center where HER-2 testing is performed at initial presentation. Ethics approval was obtained from Alberta Cancer Ethics Review Board. Patients were identified from the provincial cancer registry and the pathology laboratory. The goal of our selection process was to identify a population of newly diagnosed BC patients with HER-2 overexpression, and to investigate their increased risk of LRR [11]. Patients were considered HER-2 positive if they were 3+ on immunohistochemistry or 2+ on immunohistochemistry with gene amplification identified by chromogenic in situ hybridization (CISH) testing. A total of 460 patients were identified with HER-2 overexpression. After chart review, 187 patients were excluded because of a recurrent cancer (BC diagnosis preceding 01/1998), ductal carcinoma in situ, or an associated cancer of non-breast type. A total of 273 patients with HER-2-positive BC were included for analysis. For the HER-2-negative population, a random sample of 500 patients from the same time period with HER-2-negative disease was identified. After chart review, 155 patients were excluded for the previous criteria and 345 HER-2-negative patients were eligible for analysis. Data collected included standard prognostic factors including tumor size, LN, ER, PR status, modified Scarff–Bloom–Richardson tumor grade, LVI, date of surgery, treatment received and treatment response, LRR, time and site of first recurrence and subsequent metastatic progression, last follow-up, and death.
Patients were classified into four biological subtypes using HR and HER-2 status: HR+/HER-2− (ER-positive or PR-positive, HER-2-negative), HR+/HER-2+ (ER-positive or PR-positive, HER-2-positive), HR−/HER-2+ (ER-negative and PR-negative, HER-2-positive), HR−/HER-2− (ER-negative, PR-negative and HER-2-negative) referred to as TN for the remainder of this article.
Patient management and follow-up
All patients treated were reviewed by a multidisciplinary group and were offered a guideline-based staging, surgery (segmental resection vs. mastectomy with axillary staging, including sentinel node dissection or complete axillary LN dissection), adjuvant chemotherapy, hormonal and radiation treatments as per published Canadian recommendations [12–15]. The Cross Cancer Institute is the only tertiary cancer center, the only facility for delivery of radiotherapy (RT), and the only testing center for hormone receptor status and HER-2 status in Northern Alberta. BC diagnoses within this population are pathologically reviewed and referred to this center. The variety of treatments given (see Table 1) reflects the population-based nature of this study. Adjuvant chemotherapy was offered to all LN-positive and high-risk LN-negative patients. Adjuvant hormonal therapy used tamoxifen, with anastrozole used in post-menopausal patients with tamoxifen contraindications. RT to the breast (42.5–50 Gy in 16–25 fractions) was offered to all patients after segmental resection, with regional LN irradiation being offered to patients with ≥4 LN-positive. Post-mastectomy patients were offered chest wall and regional LN irradiation (45–50 Gy in 20–25 fractions) if they had LN-positive disease (≥1 LN-positive) or locally advanced disease (i.e., greater than T3 tumor). Follow-up was provided as per Canadian guidelines [12–15]. LRR was defined as recurrence within the chest wall, breast, supraclavicular fossa, axilla, or internal mammary LNs. All patients with evidence of LRR were assessed for systemic disease.
Primary endpoints and statistical analysis
The primary endpoint of this study was the time to LRR as a first event. The secondary endpoint was the overall survival. LRR was considered as a binary response variable. Chi-square test was used to compare the distribution of baseline characteristics among the biological subtypes. Univariate Cox regression analysis was performed for each prognostic variable. Factors identified on univariate analysis with a P ≤ 0.05 were included in multivariate model. Multivariate Cox regression analysis was performed, using the stepwise backward elimination method with model removal set at P ≤ 0.05, to identify predictive factors for LRR. All reported P values are two-sided and differences were considered statistically significant when P < 0.05. The SAS program (Version 9.1, SAS Institute Inc., Cary, NC, USA) was used for the statistical analysis.
Results
Patients and treatment characteristics
The characteristics of 618 newly diagnosed BC patients stratified by biological subtypes are listed in Table 1. Forty-four percent of patients had HR+/HER-2− tumors (N = 271), 29% had HR+/HER-2+ (N = 181), 15% had HR−/HER-2+ (N = 92), and 12% had TN (N = 74). The four biological subgroups had similar rates of LN positivity. Compared to the HR+/HER-2− subtype, HR+/HER-2+ (P < 0.0001), HR−/HER-2+ (P = 0.0006), and TN (P < 0.0001) subtypes were more likely to have tumors with significantly greater size (≥2 cm) and higher grade (≥2). HR+/HER-2+ and HR−/HER-2+ subtypes were more likely to have LVI-positive tumors (P = 0.004 and P = 0.002, respectively).
Baseline treatment characteristics are summarized in Table 1. The rate of BCT (segmental resection and adjuvant breast RT) and MRM were not significantly different between the different biological subtypes compared to the HR+/HER-2− subtype. Although equal numbers of patients in all four groups had RT, HR+/HER-2+ (P < 0.0001), HR−/HER-2+ (P < 0.0001), and TN (P < 0.0001) patient groups were more likely to receive chemotherapy than HR+/HER-2− patients. Although trastuzumab was not used in the adjuvant setting between January 1998 and December 2003, 30 patients were enrolled in BCIRG B006 (Breast Cancer International Research Group B006) and received adjuvant trastuzumab.
Patterns of LRR by biological subtypes
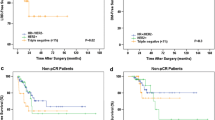
Table 2 summarizes the pattern of LRR in the biological subtypes based on the initial surgical management (i.e., BCT vs. MRM). Patients who had biopsies followed by neo-adjuvant chemotherapy were excluded from the analysis of LRR (N = 16). Over a median follow-up of 4.8 years, 45 out of 602 patients (7.5%) developed LRR as a first event including 7 (15.5%) patients with simultaneously distant metastasis. Out of the 40 patients with LRR as their only site of initial recurrence, 27 patients (68%) subsequently developed systemic relapse. Thirteen patients in the HR−/HER-2+ subtype developed LRR (14.7%), with 7/27 (26%) in the group treated by BCT versus 6/61 (9.8%) in the group treated by MRM (P = 0.007) (Table 2). In addition, 10 of these HR−/HER-2+ patients who had LLR received adjuvant RT at their initial management. In the TN subtype, eight patients developed LRR with 1/31 (3%) occurring in BCT group versus 7/41 (17%) in the MRM group (P = 0.007) (Table 2). In this subtype, out of the eight patients who had LRR, four received adjuvant RT as their initial management. The 5-year LRR free survival in the HR−/HER-2+ subtype treated by BCT was 74% compared to 98% in the luminal A (P = 0.0002, Fig. 1). The 5-year LRR free survival in the TN group treated by MRM was 82% compared to 97% in the HR+/HER-2− (P = 0.002, Fig. 2).
Factors associated with LRR
Next, we investigated the potential association between biological subtypes and increased risk of LRR as compared with conventional prognostic factors (tumor size, LN status, grade, and LVI) in the entire population. In univariate analysis, HR+/HER-2+, HR−/HER-2+, and TN subtypes (compared to HR+/HER-2− subtype) were associated with increased risk of LRR. In multivariate analysis, TN (P = 0.023), tumor size ≥2 cm (P = 0.048), and ≥1 LN-positive (P = 0.0034) were associated with increased risk of LRR (Table 3). The margins were not included as a variable in this analysis as all our patients have clear margins (guidelines >3 mm for in situ and invasive component) before starting their adjuvant treatment.
The relationship between type of breast surgery (BCT vs. MRM) and risk of LRR has been reported [16, 17]. To eliminate this confounding factor in examining the risk of LRR based on biological subtypes, we have stratified our population based on their initial surgery—BCT vs. MRM (Table 4). The association between biological subtypes (HR+/HER-2− as a control) and risk of LRR was assessed in the BC groups who received BCT and MRM. In patients treated by BCT, HR−/HER-2+ subtype and ≥1 LN-positive were found as independent prognostic factors with increased risk of LRR on multivariate analysis (HR = 11.13; 95% CI 2.78–24.53; P = 0.0007 and HR = 5.40; 95% CI 1.67–17.43; P = 0.0048, respectively) (Table 4, Fig. 1). In patients treated by MRM, TN subtype and ≥1 LN-positive were associated with increased risk of LRR on multivariate analysis (HR = 4.72; 95% CI 1.53–14.52; P = 0.0069 and HR = 3.23 95% CI 1.44–7.29; P = 0.0047, respectively) (Table 4, Fig. 2).
On multivariate analysis, HR−/HER-2+ (HR = 3.27; 95% CI 1.78–6.04; P = 0.0001), TN subtype (HR = 3.11; 95% CI 1.65–5.90; P = 0.0005), tumor size ≥2 cm (HR = 3.52; 95% CI 2.12–5.83; P = 0.0001), and ≥1 LN-positive (HR = 2.04; 95% CI 1.26–3.30; P = 0.0036) were associated with decreased overall survival (Table 5).
Discussion
BC molecular subtypes have phenotypic diversity with regards to their tumor aggressiveness [2, 7] and response to systemic therapy [18]. Although these molecular subtypes correlate with patient outcome, their impact on risk of LRR, compared to conventional prognostic factors has not been fully investigated. Recent studies suggested that HER-2 and TN subtypes exhibited a poor prognosis with increased risk of local recurrence [19, 20]. However, the risk of LRR associated with these molecular subtypes was not determined based on the initial surgical management (i.e., BCT vs. MRM). In our population-based study, we characterized the frequencies of LRR among women with BC based on biological subtype, using HR and HER-2 status as surrogates for the biological subtype. We found that HR−/HER-2+ and TN subtypes are independent prognostic factors associated with higher rate of LRR (14.7 and 11%, respectively) compared with HR+/HER-2− (3.4%) subtype.
In accordance with our data supporting the effect of these biological subtypes on LRR, Nguyen et al. [21] reported in a limited cohort of HER-2 subtype (32 patients) treated with BCT a significant increase in 5-year LRR (8.4%) in HER-2 subtype compared with the luminal A and B subgroups (0.8 and 1.5%, respectively). In addition, we further investigated the relationship between these biological subtypes and risk of LRR based on surgical management (i.e., BCT vs. MRM). For the patients treated by BCT, HR−/HER-2+ subtype and LN positivity were the only independent prognostic factors associated with increased risk of LRR (P = 0.0007, and P = 0.0048, respectively). In contrast, the association between HR−/HER-2+ subtype and increased risk of LRR was lost in the group treated with MRM (P = 0.33). Furthermore, Gonzalez-Angulo [20] have reported that HER-2 subtype T1abN0M0 have a significant risk of distant relapse without information about their risk of LRR. Whether this increased risk of LRR and distant metastasis is an intrinsic property of the HER-2 subtype and/or is a subsequent effect related to the type of surgery warrants further investigation in a larger cohort of HER-2 subtype. Our study as well as others was conducted in the era preceding the use of trastuzumab in adjuvant setting. Furthermore, the early data from NSABP B31/N9831 trial indicated that the use of adjuvant trastuzumab reduced the risk of LRR [22]. So far, this reduction of LRR has not been confirmed by the HERA trial [23]. Our follow-up was limited to 5 years, and longer follow-up may be required to assess the impact of HER-2 subtype on the increased risk of LRR. This is especially true for patients with HR+/HER-2− tumors, as their risk of LRR is extended well beyond 5 years [24].
In patients treated by MRM, we found that TN subtype and LN positivity were associated with an increased risk of LRR (4.7- and 3.2-fold, respectively). In our study, the use of a panel of three biomarkers as surrogates to estimate molecular subtype did not allow the distinction between basal-like and non basal-like TN tumor subtypes [25] for the assessment of their risk of LLR. There is growing evidence that TN subtype predicts lower incidence of axillary LN involvement and exhibits an independent poor prognostic factor compared to tumor size and LVI [26]. Furthermore, Foulkes et al. [27] found that tumor size was an unreliable predictor of prognosis of basal-like BC (~70–80% of TN) and did not correlate closely with LN status. In current practice, axillary LN involvement and tumor size have conventionally been considered as critical determinant of clinical outcome and locoregional RT after MRM. However, the tendency of TN subtype to behave aggressively, despite their small size (≤1 cm in diameter) and the absence of nodal involvement raise questions whether these factors should be considered exclusively as the unique determinant of locoregional treatment decisions. Furthermore, patients with TN tumors treated with MRM in Danish BC studies [28] showed a significant increased risk of LRR independent of adjuvant post-mastectomy RT. These data suggest that the disconnection between tumor size/lymph-node status and prognosis in these TN tumors reflects an inconsistent relationship between tumor size (i.e., size of cancer cell population) and metastatic potential in this subset of BC [27]. Altogether, along with the association between TN and the high risk of LRR, these observations should have direct implications for locoregional radiation after MRM, particularly for women with T1/2N0 and TN subtype.
Using simplified triple biomarker assessment differs from gene expression testing and implies that some patients could be misclassified [29]. In contrast, compared to these available clinical biomarkers, the genotyping approach may not be a cost effective method and is relatively underdeveloped in clinical practice. The first generation of genomic assays developed to predict which BC patients with ER-positive may benefit from adjuvant chemotherapy based upon predicted risk of recurrence has entered clinical practice [6, 30]. In a similar manner, there is also evidence that molecular profiling using additional immunohistochemical markers including Ki-67, CK5/6, and EGFR-1 also predicts the risk of LRR [25, 31–33]. All these studies evaluating molecular subtypes should be viewed as exploratory and their impact on locoregional management requires further validation from other confirmatory studies.
While the added value of biological subtype as compared with conventional factors is still evolving, this new classification paradigm presents a huge clinical potential. It provides the opportunity to investigate biological and clinical questions in a homogeneous subgroup of patients. There is a need to integrate these defined subtypes with clinically available biomarkers into treatment decision making. Potential applications include examining in future studies the effect of more aggressive locoregional treatment in groups identified at increased risk of LRR, for example, the use of RT boost for HR−/HER-2+ subtype and post-MRM RT in LN-negative patients with TN subtype. This approach will improve the prognostic and predictive information of classical prognostic features to better tailor the locoregional treatment based on the risk of LRR.
References
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA et al (2000) Molecular portraits of human breast tumours. Nature 406(6797):747–752
Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, Hastie T, Eisen MB, van de Rijn M, Jeffrey SS et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98(19):10869–10874
van de Vijver MJ, He YD, van’t Veer LJ, Dai H, Hart AA, Voskuil DW, Schreiber GJ, Peterse JL, Roberts C, Marton MJ et al (2002) A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med 347(25):1999–2009
Chang HY, Nuyten DS, Sneddon JB, Hastie T, Tibshirani R, Sorlie T, Dai H, He YD, van’t Veer LJ, Bartelink H et al (2005) Robustness, scalability, and integration of a wound-response gene expression signature in predicting breast cancer survival. Proc Natl Acad Sci USA 102(10):3738–3743
Wang Y, Klijn JG, Zhang Y, Sieuwerts AM, Look MP, Yang F, Talantov D, Timmermans M, Meijer-van Gelder ME, Yu J et al (2005) Gene-expression profiles to predict distant metastasis of lymph-node-negative primary breast cancer. Lancet 365(9460):671–679
Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, Baehner FL, Walker MG, Watson D, Park T et al (2004) A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 351(27):2817–2826
Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, Deng S, Johnsen H, Pesich R, Geisler S et al (2003) Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA 100(14):8418–8423
Sotiriou C, Neo SY, McShane LM, Korn EL, Long PM, Jazaeri A, Martiat P, Fox SB, Harris AL, Liu ET (2003) Breast cancer classification and prognosis based on gene expression profiles from a population-based study. Proc Natl Acad Sci USA 100(18):10393–10398
Kreike B, van Kouwenhove M, Horlings H, Weigelt B, Peterse H, Bartelink H, van de Vijver MJ (2007) Gene expression profiling and histopathological characterization of triple-negative/basal-like breast carcinomas. Breast Cancer Res 9(5):R65
Bertucci F, Finetti P, Rougemont J, Charafe-Jauffret E, Cervera N, Tarpin C, Nguyen C, Xerri L, Houlgatte R, Jacquemier J et al (2005) Gene expression profiling identifies molecular subtypes of inflammatory breast cancer. Cancer Res 65(6):2170–2178
Gabos Z, Sinha R, Hanson J, Chauhan N, Hugh J, Mackey JR, Abdulkarim B (2006) Prognostic significance of human epidermal growth factor receptor positivity for the development of brain metastasis after newly diagnosed breast cancer. J Clin Oncol 24(36):5658–5663
Levine M (2001) Clinical practice guidelines for the care and treatment of breast cancer: adjuvant systemic therapy for node-negative breast cancer (summary of the 2001 update). CMAJ 164(2):213
Truong PT, Olivotto IA, Whelan TJ, Levine M (2004) Clinical practice guidelines for the care and treatment of breast cancer: 16. Locoregional post-mastectomy radiotherapy. CMAJ 170(8):1263–1273
Whelan T, Olivotto I, Levine M (2003) Clinical practice guidelines for the care and treatment of breast cancer: breast radiotherapy after breast-conserving surgery (summary of the 2003 update). CMAJ 168(4):437–439
Shenkier T, Weir L, Levine M, Olivotto I, Whelan T, Reyno L (2004) Clinical practice guidelines for the care and treatment of breast cancer: 15. Treatment for women with stage III or locally advanced breast cancer. CMAJ 170(6):983–994
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, Jeong JH, Wolmark N (2002) Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 347(16):1233–1241
Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, Aguilar M, Marubini E (2002) Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 347(16):1227–1232
Rouzier R, Perou CM, Symmans WF, Ibrahim N, Cristofanilli M, Anderson K, Hess KR, Stec J, Ayers M, Wagner P et al (2005) Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res 11(16):5678–5685
Millar EK, Graham PH, O’Toole SA, McNeil CM, Browne L, Morey AL, Eggleton S, Beretov J, Theocharous C, Capp A et al (2009) Prediction of local recurrence, distant metastases, and death after breast-conserving therapy in early-stage invasive breast cancer using a five-biomarker panel. J Clin Oncol 27(28):4701–4708
Gonzalez-Angulo AM, Litton JK, Broglio KR, Meric-Bernstam F, Rakkhit R, Cardoso F, Peintinger F, Hanrahan EO, Sahin A, Guray M et al (2009) High risk of recurrence for patients with breast cancer who have human epidermal growth factor receptor 2-positive, node-negative tumors 1 cm or smaller. J Clin Oncol 27(34):5700–5706
Nguyen PL, Taghian AG, Katz MS, Niemierko A, Abi Raad RF, Boon WL, Bellon JR, Wong JS, Smith BL, Harris JR (2008) Breast cancer subtype approximated by estrogen receptor, progesterone receptor, and HER-2 is associated with local and distant recurrence after breast-conserving therapy. J Clin Oncol 26(14):2373–2378
Romond EH, Perez EA, Bryant J, Suman VJ, Geyer CE Jr, Davidson NE, Tan-Chiu E, Martino S, Paik S, Kaufman PA et al (2005) Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med 353(16):1673–1684
Piccart-Gebhart MJ, Procter M, Leyland-Jones B, Goldhirsch A, Untch M, Smith I, Gianni L, Baselga J, Bell R, Jackisch C et al (2005) Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med 353(16):1659–1672
Blows FM, Driver KE, Schmidt MK, Broeks A, van Leeuwen FE, Wesseling J, Cheang MC, Gelmon K, Nielsen TO, Blomqvist C et al (2010) Subtyping of breast cancer by immunohistochemistry to investigate a relationship between subtype and short and long term survival: a collaborative analysis of data for 10, 159 cases from 12 studies. PLoS Med 7(5):e1000279
Voduc KD, Cheang MC, Tyldesley S, Gelmon K, Nielsen TO, Kennecke H (2010) Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol 28(10):1684–1691
Crabb SJ, Cheang MC, Leung S, Immonen T, Nielsen TO, Huntsman DD, Bajdik CD, Chia SK (2008) Basal breast cancer molecular subtype predicts for lower incidence of axillary lymph node metastases in primary breast cancer. Clin Breast Cancer 8(3):249–256
Foulkes WD, Reis-Filho JS, Narod SA (2010) Tumor size and survival in breast cancer—a reappraisal. Nat Rev 7:348–353
Kyndi M, Sorensen FB, Knudsen H, Overgaard M, Nielsen HM, Overgaard J (2008) Estrogen receptor, progesterone receptor, HER-2, and response to postmastectomy radiotherapy in high-risk breast cancer: the Danish Breast Cancer Cooperative Group. J Clin Oncol 26(9):1419–1426
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, Karaca G, Troester MA, Tse CK, Edmiston S et al (2006) Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295(21):2492–2502
Albain KS, Barlow WE, Shak S, Hortobagyi GN, Livingston RB, Yeh IT, Ravdin P, Bugarini R, Baehner FL, Davidson NE et al (2010) Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol 11(1):55–65
Mamounas EP (2005) Continuing evolution in breast cancer surgical management. J Clin Oncol 23(8):1603–1606
Mamounas EP, Tang G, Fisher B, Paik S, Shak S, Costantino JP, Watson D, Geyer CE Jr, Wickerham DL, Wolmark N (2010) Association between the 21-gene recurrence score assay and risk of locoregional recurrence in node-negative, estrogen receptor-positive breast cancer: results from NSABP B-14 and NSABP B-20. J Clin Oncol 28(10):1677–1683
Musgrove EA, Sergio CM, Loi S, Inman CK, Anderson LR, Alles MC, Pinese M, Caldon CE, Schutte J, Gardiner-Garden M et al (2008) Identification of functional networks of estrogen- and c-Myc-responsive genes and their relationship to response to tamoxifen therapy in breast cancer. PloS one 3(8):e2987
Acknowledgments
We thank the members of Alberta Cancer Registry for the identification of this population of breast cancer and the technicians from Department of Laboratory Medicine and Pathology for their support in immunohistochemistry.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gabos, Z., Thoms, J., Ghosh, S. et al. The association between biological subtype and locoregional recurrence in newly diagnosed breast cancer. Breast Cancer Res Treat 124, 187–194 (2010). https://doi.org/10.1007/s10549-010-1135-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-010-1135-1