Abstract
We investigated the associations between two CYP1A1 polymorphisms (Ile462Val and Thr461Asn) and one CYP1B1 polymorphism (Leu432Val) and breast cancer risk. The study population consisted of 483 breast cancer patients and 482 healthy population controls, all of homogenous Finnish origin. No statistically significant overall associations were found between the CYP1A1 and CYP1B1 genotypes and breast cancer risk. However, a significant increase in the breast cancer risk was seen for women who had smoked 1–9 cigarettes/day and carried the CYP1B1 432Val allele; the OR was 2.6 (95% CI 1.07–6.46) for women carrying the Leu/Val genotype and 5.1 (95% CI 1.30–19.89, P for trend 0.005) for women with the Val/Val genotype compared to similarly smoking women homozygous for the 432Leu allele. Furthermore, when CYP1B1 genotypes were combined with the previously analyzed N-acetyl transferase (NAT2) genotypes, a significant increase in breast cancer risk was found among women who had at least one CYP1B1 432Val allele together with the NAT2 slow acetylator genotype (OR 1.52; 95% CI 1.03–2.24) compared to women carrying a combination of CYP1B1 Leu/Leu and NAT2 rapid acetylator genotypes. This risk was seen to be confined to ever smokers; the OR was 2.46 (95% CI 1.11–5.45) for ever smokers carrying at least one CYP1B1 432Val allele together with the NAT2 slow acetylator genotype compared to ever smokers with the CYP1B1 Leu/Leu and NAT2 rapid acetylator genotype combination. Our results suggest that the CYP1B1 polymorphism may be an important modifier of breast cancer risk in Finnish Caucasian women who have been exposed to tobacco smoke and/or carry the NAT2 slow acetylator genotype.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most of the established risk factors for breast cancer are linked to prolonged estrogen exposure, like early age at menarche, late age at menopause, nulliparity and obesity in postmenopausal women [1]. Also some life style factors, such as the use of hormone replacement therapy (HRT) and alcohol are known to contribute to the increased risk, while the studies on the association between smoking and breast cancer risk have given discrepant results [2, 3]. Tobacco smoke contains a wide variety of known carcinogens including polycyclic aromatic hydrocarbons (PAHs) and nitrosoamines. However, in some studies tobacco smoking has been suggested to have protective effect against breast cancer, possibly due to earlier menopause and thus shorter exposure to estrogen [4]. Increased level of 2-hydroxyestradiol induced by smoking has also been suggested as one potential anti-estrogenic mechanism of tobacco smoke [5].
Cytochrome P450 (CYP) 1A1 and 1B1 enzymes are involved in the metabolism of both estradiol and PAHs to mutagenic intermediates capable of causing DNA damage [6–8]. CYP1A1 mediates hydroxylation of 17-β-estradiol (E2) mainly to 2-hydroxyestradiol and CYP1B1 preferably to 4-hydroxyestradiol [6, 7]; the latter metabolite has been shown to be carcinogenic [9, 10]. The expression of CYP1A1 and CYP1B1 is induced by PAHs and recently CYP1B1 was also demonstrated to be induced by E2 in estrogen receptor positive cells [11, 12]. Different expression levels of these enzymes as well as inter-individual differences due to genetic variations may thus further contribute to variations in individual susceptibility to breast cancer.
To date, several genetic polymorphisms have been identified in the CYP1A1 and CYP1B1 genes [13, 14]. In CYP1A1, in addition to a T3801C polymorphism detectable by MspI restriction enzyme [15], two polymorphisms leading to an amino acid change exist in exon 7 (Thr461Asn and Ile462Val) [16, 17]. A strict linkage disequilibrium have been reported between the CYP1A1 3801C and CYP1A1 462Val alleles in Caucasian population [16, 18, 19]. Among African–Americans, an additional polymorphic site exists in the 3′ non-coding region of CYP1A1; a T3205C creating a novel MspI restriction site [20]. Functional significance of the different CYP1A1 genotypes in human lymphocytes has been studied with somewhat inconclusive results [21–24]. One study showed that subjects with the variant CYP1A1 462Val allele had an increased inducibility of CYP1A1 mRNA and threefold increase in enzymatic activity, whereas T3801C polymorphism had no effect on the induction of CYP1A1 [22]. Similarly, lymphocyte CYP1A1 enzyme activity was significantly increased among subjects with the variant CYP1A1 462Val allele according to two other studies [21, 24]. The variant CYP1A1 3801C allele has also been reported to be more readily inducible or having higher activity than the wild type in human lymphocytes [23, 24].
In CYP1B1, two polymorphisms, Leu432Val and Asn453Ser are located in a catalytically important heme binding domain in exon 3 [25, 26]. Two linked amino acid substitutions in exon 2 (Arg48Gly and Ala119Ser) constitute an additional allele [25, 27]. Functional assays of CYP1B1 Leu432Val polymorphisms in bacterial expression systems have shown that the CYP1B1 432Val allele encodes an enzyme with higher activity towards E2 than the 432Leu variants [28, 29]. However, one study performed in bacterial expression system suggested that all variant enzymes (with amino acid substitutions at codon 48, 119, 432 or 453) were associated with increased catalytic efficiency for the 4-hydroxylation of E2 [30]. Instead, the CYP1B1*2 (48Gly and 119Ser) variant has not been shown to alter the catalytic activity towards E2 [27, 31]. One study using (−)-trans-(7R,8R)-benzo[a]pyrene 7,8-dihydrodiol as a substrate in a bacterial system found no major differences in catalytical properties for studied CYP1B1 variants [28].
In earlier studies a significant overall association has been found between the CYP1A1 polymorphisms and breast cancer risk [32–39]. However, only three out of eight studies reported positive association among Caucasian population [32, 37, 38]. Moreover, in all other Caucasian studies as well as in two Asian studies no significant overall association was seen [40–49]. When exposure to tobacco smoke or polychlorinated biphenyls (PCBs) has been taken into account, stronger evidence for the association between CYP1A1 genotypes has been found [38, 44–46, 49–51].
Two earlier studies have found an overall association between CYP1B1 Leu432Val polymorphism and breast cancer risk [52, 53]. Moreover, the 432Val allele has been associated with estrogen and/or progesterone receptor positive tumors [26, 54], breast cancer risk among HRT users [55] and current smokers in a case-only study [56]. In contrast, at least five case-control studies have not found any significant association between the 432Val allele and breast cancer risk [57–61].
In this study, the potential modifying role of the CYP1A1 and CYP1B1 genotypes was studied in a homogenous Finnish study population consisting of 483 incident breast cancer patients and 482 healthy population controls. We also evaluated the potential interaction between the CYP1B1 genotypes and the previously [62] analyzed N-acetyl transferase (NAT2) genotypes.
Materials and methods
Subjects
This case-control study is an extension of the Kuopio Breast Cancer Study [63, 64]. This study was approved by the Joint Committee of the University of Kuopio and Kuopio University Hospital. Participation was based on written consent. Women with a suspect breast lump, mammographic abnormality or a breast symptom necessitating further examinations were invited to Kuopio University Hospital (Finland) between 1990 and 1995 for diagnostic procedures. Detailed data were collected from all study subjects by a trained study nurse before any diagnostic procedures were initiated. Among other things, the questionnaires outlined socio-economic background, family history of breast cancer, history of benign breast disease, reproductive and medical history, smoking habits, current alcohol intake and body size indicators. Smoking inquiries included the data about the amount of daily smoking (cigarettes/day), the duration of smoking (in years), and the time since cessation of smoking (in years). Exposure to passive smoking at work and/or at home was also resolved (in years).
A total of 516 women were eventually diagnosed with histologically confirmed breast cancer. Because all interviewed women agreed to donate a blood sample and only 12 women who were later diagnosed with breast malignancy refused to participate, the co-operation rate for the cases was 98%. The recruitment protocol missed 51 women within the hospital, all being private patients not entering the hospital through the standard referral system. Additional 11 cases were lost due to nurses’ one-month strike in spring 1995. Only 26 breast cancer patients from the hospital catchment area were treated elsewhere according to the files of the Finnish Cancer Registry. The contact rate for the cases, calculated as described in Slattery et al. [65], was therefore 86% and the overall response rate 84%.
Healthy population controls with no previous breast problems or symptoms were drawn from the Finnish National Population Register covering the catchment area of cases. They were initially contacted by a letter explaining the study protocol and later called up by a study nurse. The exact contact rate is not available for controls. Overall, 514 controls were interviewed in parallel with the breast cancer cases, all of whom agreed to donate blood. The co-operation rate among controls was 72%. The main reason for non-participation was refusal.
Lymphocyte DNA was available for 483 breast cancer patients and for 488 controls. Six subjects among controls were excluded because they had an earlier breast cancer diagnosis (n = 4) or they were of non-Finnish origin (n = 2). Consequently, the final case group included 483 patients (44.3–91.6 years, mean 58.9 years) and the final control population consisted of 482 subjects (37.5–77.2 years, mean 53.5 years).
Genotyping analyses
Lymphocyte DNA was extracted by standard techniques. The CYP1A1 genotypes were determined using 100 ng of DNA as template in a PCR-based restriction fragment length polymorphism (RFLP) method previously described by Cascorbi et al. [16]. Briefly, a 204 bp PCR amplification product was digested with BseM I (Fermentas, Amherst, NY, USA) or Bsa I (New England Biolabs, Inc., Beverly, MA, USA) restriction enzymes for determination of the polymorphisms CYP1A1 Ile462Val and CYP1A1 Thr461Asn genotypes, respectively.
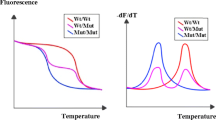
For CYP1B1 genotyping, 50 ng of DNA was amplified by AmpliTaq Gold DNA polymerase which is included in TaqMan Universal Master mix (Applied Biosystems, Foster city, CA, USA). The detection of alleles was based on fluorogenic TaqMan MGB probes using the ABI PRISM 7000 Sequence Detection Systems (Applied Biosystems, Foster City, CA, USA). Primer Express™ Version 2.0 software (Applied Biosystems, Foster city, CA, USA) was used for designing short amplicons for detecting the CYP1B1 432Val allele. A 108 bp PCR product was amplified using specific forward (5′-ACC TCT GTC TTG GGC TAC CAC AT-3′) and reverse (5′-TGG ATC AAA GTT CTC CGG GTT A-3′) primers. Allele specific TaqMan MGB-probes (Applied Biosystems, Cheshire, UK) 5′-VIC-AT CAT GAC CCA CTG AA-3′ and 5′-FAM-AAT CAT GAC CCA GTG AA-3′ were used for detecting the CYP1B1 432Leu allele and the 432Val allele, respectively. The PCR reaction was performed in a total volume of 20 μl containing 1× TaqMan Universal Master mix, 900 nM of each primer and 200 nM of each probe. Two initial hold steps of 2 min at 50°C and 10 min at 94°C were followed by 40 cycles of two-step PCR with denaturation at 94°C for 15 s and annealing and extension at 60°C for 1 min. For quality control purposes 144 of the TaqMan genotyping results were confirmed by a PCR–RFLP method published earlier [26].
All obscure results as well as a random repertoire of 10% of all samples, were re-examined for the quality assurance of the laboratory work. All the results were interpreted by two independent investigators. No discrepancies were found in the replicate analyses.
The NAT2 was genotyped by a TaqMan method as previously described in [62].
Statistical methods
The observed CYP1A1 and CYP1B1 genotype frequencies were compared to the expected genotype frequencies to determine whether they are in Hardy–Weinberg equilibrium (HWE).
Associations between CYP1A1 or CYP1B1 genotypes and breast cancer risk were analysed by unconditional logistic regression to estimate adjusted odds ratios (ORs) and 95% confidence intervals (CIs) using the SPSS 9.0 statistical package (SPSS Inc, Chicago, IL, USA). Known or suspected risk factors for breast cancer were used as adjusting variables in the multivariate logistic models. These covariates included age (<45, 45–53, 53–61, >61 years), age at menarche (≤12, 13–14, ≥ 15 years), age at first full-term pregnancy (nulliparous, <25, 25–30, >30 years), number of full-term pregnancies (continuous), history of benign breast disease (no/yes), first-degree (mother, sister, daughter) family history of breast cancer (no/yes), smoking (never/ever), use of alcohol (never/ever) and body mass index (BMI) (<25.4 kg/m2, ≥25.4 kg/m2). Subjects were excluded from the logistic regression if any of the adjusting variables were missing.
Women who had ever smoked daily for at least 3 months were classified as smokers and those who reported smoking at reference date were considered current smokers. Women who reported ever being exposed to passive smoking at work or at home were classified as passive smokers. Adjusted estimates for active and passive smoking and breast cancer risk were calculated in order to evaluate the potential association between smoking habits and breast cancer risk. The factors of interest were smoking status (never active/passive, only passive, former and current smokers), duration of smoking (1–14 and ≥15 years), number of cigarettes smoked per day (1–9 and ≥10) and pack-years of cigarettes (<5 and ≥5). Pack-years were calculated as number of packs (20 cigarettes per pack) smoked per day multiplied by the number of smoking years.
Women were considered postmenopausal if they had reported natural menopause, or had gone through bilateral oophorectomy. Women who were hysterectomized with intact ovaries (ovary) (40 cases and 41 controls) or for whom details of the operations were unknown (6 cases and 2 controls) were classified postmenopausal if they were no longer menstruating and were older than 51 years (median for menopause among Finnish women). All the rest were classified premenopausal.
Possible associations between the CYP1A1 and CYP1B1 genotypes and smoking, use of oral contraceptives (OCs) (never/ever) or HRT (never/ever), were examined by stratified analyses. The interactive effects were assessed by the likelihood ratio tests to compare the goodness of fit of the models with and without the interaction term taking into account other adjusting variables. The association between CYP1A1 or CYP1B1 genotypes and the expression of estrogen or progesterone receptors in the tumour was also evaluated.
Based on the data from previous studies, homozygous for the CYP1A1 461Thr and 462Ile alleles and CYP1B1 432Leu alleles were chosen to serve as the referent category in all separate analyses for these locuses, respectively [35, 41, 51, 55, 57]. In order to increase statistical power the heterozygous and homozygous variant genotypes were combined as the risk genotype group.
For the combined analyses the rapid NAT2 acetylator genotypes were grouped with the CYP1B1 Leu/Leu genotypes to act as a reference group.
Results
Our previous studies have shown a high (>0.91) waist-to-hip ratio, first-degree family history of breast cancer, and history of benign breast disease to be associated with increased risk of breast cancer in this study population, whereas parity and use of OCs were associated with decreased risk [64]. Cases (mean age 58.9 years, SD 14.3 years) were somewhat older compared to controls (mean age 53.5 years, SD 10.9 years) (P < 0.001) [63, 64]. In contrast, there was no difference in the daily consumption of cigarettes, duration of smoking, pack-years of smoking, BMI or the use of OCs (duration in months) between cases and controls (data not shown).
Table 1 shows the distribution of CYP1A1 and CYP1B1 genotypes among cases and controls. All genotype frequencies were in Hardy–Weinberg equilibrium in the controls. Since the CYP1A1 T3801C and CYP1A1 Ile462Val polymorphisms are closely linked in Caucasian populations [16, 18, 19], only the Ile462Val and Thr461Asn polymorphisms were studied for CYP1A1 gene.
Overall, the CYP1A1 and CYP1B1 genotype frequencies did not vary significantly between cases and controls (Table 1). When stratified by menopausal status, a tendency of protective effect was seen among premenopausal women carrying the CYP1A1 462Val allele (OR 0.51, 95% CI 0.25–1.05) compared to women without the allele. No effect was seen in this context for the CYP1A1 Thr461Asn and CYP1B1 Leu432Val polymorphisms (data not shown).
No significant association was found between the CYP1A1 and CYP1B1 genotypes and breast cancer risk in subgroups defined by estrogen or progesterone receptor status or use of OCs or HRT (never/ever) (data not shown). However, a tendency of increased risk of breast cancer was seen among ever users of OCs with at least one CYP1B1 432Val allele (OR 1.50, 95% CI 0.98–2.30) compared to women without this allele. Smoking (never/ever) did not have interaction with CYP1A1 genotypes (data not shown). In contrast, the CYP1B1 genotypes appeared to interact with smoking in modifying the individual breast cancer risk; ever smokers with one copy of the CYP1B1 432Val allele were at borderline increased risk of breast cancer (OR 1.86, 95% CI 1.01–3.42) compared to ever smokers with the Leu/Leu genotype (Table 2). Moreover, when ever smokers were further stratified by daily consumption of cigarettes a statistically significant increase in breast cancer risk was seen for women who had smoked 1–9 cigarettes daily and carried either one (OR 2.63; 95% CI 1.07–6.46) or two (OR 5.09; 95% CI 1.30–19.9) CYP1B1 432Val alleles compared to women who had smoked the same amount but carried the Leu/Leu genotype (P for interaction 0.009) (Table 2.). Similarly, women with at least one CYP1B1 432Val allele were at increased risk if they had smoked less than 15 years (OR 2.62, 95% CI 1.06–6.49) compared to women who had smoked the same time but lacked the allele. Similarly, women with at least one CYP1B1 432Val allele were at increased risk if they had smoked less than five pack-years (OR 2.73, 95% CI 1.09–6.83) compared to women who had smoked the same amount but carried the Leu/Leu genotype.
Although no significant interaction was found between CYP1B1 and NAT2 genes (P = 0.385) when CYP1B1 genotypes were combined with the previously analyzed NAT2 genotypes, women who had at least one CYP1B1 432Val allele together with the NAT2 slow acetylator genotype were found to be at 1.52-fold (95% CI 1.03–2.24) increased risk of breast cancer compared to women simultaneously carrying the Leu/Leu and NAT2 rapid acetylator genotypes. This risk was confined to premenopausal women (OR 1.90; 95% CI 1.02–3.56). Moreover, the risk increased with the number of at risk genotypes (P for trend 0.04) (Table 3.). When stratified by smoking habits, this risk was seen to be confined to ever smokers; a 2.46-fold (95% CI 1.11–5.45) risk for breast cancer was seen among women who carried at least one CYP1B1 432Val allele (P for trend 0.03) together with the NAT2 slow acetylator genotype compared to ever smokers who carried the Leu/Leu genotype together with the NAT2 rapid acetylator genotype (Table 4.). A further increase in the risk was seen for women who had smoked daily 1–9 cigarettes and carried the high-risk genotype combination; they were at over fourfold (OR 4.41; 95% CI 1.29–15.1) risk of breast cancer compared to women who smoked the same amount daily and were carriers of the CYP1B1 Leu/Leu and NAT2 rapid acetylator genotype combination. Similar association was found among women who had smoked under 15 years (data not shown).
Discussion
The frequency of the CYP1A1 462Val allele found in this study (7.1%) is well in accordance with the frequencies found in other Caucasian populations (4–9%) [19, 41]. Instead, the frequency of the CYP1A1 461Asn allele was lower in our study population (0.5%), compared to previous studies among other Caucasian population (2.0–5.7%) [66]. Historical and demographic reasons could partly explain this difference [67, 68]. Consequently, the power of the study was far too low for any reliable interpretations of the CYP1A1 Thr461Asn and breast cancer risk.
The lack of significant overall association between the studied CYP1A1 polymorphisms and breast cancer risk is in good agreement with most of the previous studies among Caucasian population [40–46]. Although contradictory results also exist [32–37], only three of them are from Caucasian studies; an increased breast cancer risk was observed among French–Canadian women with at least one variant CYP1A1 461Asn allele (OR 3.3, 95% CI 1.1–9.7) [32] and with Caucasian women (in Connecticut) with the CYP1A1 462Val allele (OR 2.1, 95% CI 1.1–3.9) [38] whereas a decreased risk was seen among Caucasian women (central European origin) with at least one CYP1A1 3801C allele (OR 0.55, 95%CI 0.36–0.82) [37].
A tendency of decreased breast cancer risk was seen in our study among premenopausal women with at least one CYP1A1 462Val allele (OR 0.51, 95% CI 0.25–1.05). Similar, statistically significant decrease in the risk has been seen among Japanese women (OR 0.66, 95% CI 0.45–0.96) [33] in whom the frequency of the CYP1A1 462Val allele is almost fourfold compared to our population (25.4% vs. 7.1%). A recent meta-analysis found no significant associations between CYP1A1 T3801C, Ile462Val or Thr461Asn polymorphisms and breast cancer risk [69].
In many of the studies that failed to find any overall associations between the CYP1A1 genotypes and breast cancer, significant associations between the CYP1A1 polymorphisms and smoking habits or higher levels of serum PCBs in relation to risk of breast cancer have been observed [38, 44–46, 49–51]. However, in accordance with our studies no association between the smoking habits and the CYP1A1 Ile462Val or CYP1A1 Thr461Asn polymorphisms and breast cancer risk have been found in white Caucasians [32, 41, 42, 46]. The role of PCBs in relation to breast cancer risk could not be evaluated in our study, as the data on the exposure to PCBs was not available.
The frequency of the CYP1B1 432Val allele (34%) in the present study was well in accordance with earlier findings in Caucasians (27–45%) [25, 26, 53, 55]. In agreement with most of the previous studies [26, 54, 55, 57–61, 70], no overall association with breast cancer risk was seen for the CYP1B1 genotypes. However, ever smokers with one CYP1B1 432Val allele were at increased risk of breast cancer compared to ever smokers with the Leu/Leu genotype. Furthermore, a significant interaction was seen with daily use of cigarettes; the increase was confined to those women who were smoking less than ten cigarettes a day with a significant trend of increasing risk with increasing number of variant alleles.
In a recent case-only study among French women, a similar borderline significant increase in breast cancer risk was found for current smokers carrying two CYP1B1 432Val alleles compared to never smokers with at least one 432Leu allele (OR 2.32, 95% CI 1.00–5.38) [56]. The finding reached statistical significance among heavier smokers (i.e. >5 cigarettes/day, >20 years or >10 pack-years). In our study no increase in the risk was seen among women smoking more than ten cigarettes/day. However, since the French study was a case only study, the results are not fully comparable. Furthermore, at least two studies have reported no association between breast cancer risk and the CYP1B1 genotypes in relation to smoking [53, 55].
As NAT2 is also involved in the metabolism of tobacco carcinogens and as we have earlier found a significant association between the slow acetylator status and breast cancer risk in smoking women [62], we also examined the potential combined effects of the NAT2 and CYP1B1 genotypes; the study did not have sufficient power to evaluate the CYP1A1 and NAT2 genotype combinations in this context.
The concurrent presence of at least one CYP1B1 432Val allele and the NAT2 slow acetylator genotype appeared to pose a statistically significant increase in the risk of breast cancer compared to women with the CYP1B1 Leu/Leu genotype together with the NAT2 rapid acetylator genotype. However, no interaction was found between these two genes. When stratified by smoking, the increased risk seemed to be confined to ever smokers, especially to light smokers (1–9 cigarettes/day) or to those who had smoked less than 15 years. Our finding agrees with the suggestions that the importance of genetic susceptibility might be more significant at lower levels of exposure to carcinogens [71]; the xenobiotic metabolizing enzymes may saturate at higher concentrations of the substrates. Accordingly, NAT2, which is known to be involved in the metabolism of tobacco carcinogens, has been suggested to be associated with increased risk of cancer especially at low doses of tobacco carcinogens in studies by us [62, 72] and others [73, 74].
One shortage in our study is that even though our study size is relatively large, the number of smokers is fairly low. Moreover, the number of pack-years is fairly low. These results should, therefore, be considered preliminary before confirmed in larger studies with adequate number of smokers. Furthermore, due to the multiple comparisons performed, the possibility of a chance finding should also be considered.
In our study, a tendency of increasing risk was seen among ever users of OCs carrying at least one copy of the CYP1B1 432Val allele (OR 1.50, 95% CI 0.98–2.31) compared to those with the CYP1B1 Leu/Leu genotype. This issue has previously been studied only in a Turkish population where no association between breast cancer and CYP1B1 genotypes in relation to use of OCs was found [53]. One possible mechanistic explanation for our finding is that increased CYP1B1 activity may result in producing higher levels of genotoxic 4-OHE2.
Finally, the CYP1B1 Val/Val genotype has been shown to be more prevalent in the tumors expressing the ER and/or PR [26, 54] or among patients who have used HRT for more than 4 years [55]. However, in agreement with two previous studies [55, 75], no association between ER and/or PR status and CYP1B1 Val was seen in our study. Neither were no associations found when stratified by the use of postmenopausal hormones.
In summary, we found no significant overall associations between the CYP1A1 and CYP1B1 genotypes and breast cancer risk. However, the CYP1B1 432Val allele was associated with increased risk of breast cancer among light smokers. Moreover, as a novel finding, a significant trend of increasing risk with increasing number of the putative at-risk genotypes of CYP1B1 and NAT2 was seen. This association was confined to light smokers.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CYP:
-
Cytochrome P450
- E2 :
-
17-β-estradiol
- HRT:
-
Hormone replacement therapy
- NAT2:
-
N-acetyl transferase
- OC:
-
Oral contraceptive
- OR:
-
Odds ratio
- PAH:
-
Polycyclic aromatic hydrocarbon
- PCB:
-
Polychlorinated biphenyl
- PCR:
-
Polymerase chain reaction
- RFLP:
-
Restriction fragment length polymorphism
References
Key TJ, Verkasalo PK, Banks E (2001) Epidemiology of breast cancer. Lancet Oncol 2:133–140
Terry PD, Rohan TE (2002) Cigarette smoking and the risk of breast cancer in women: a review of the literature. Cancer Epidemiol Biomarkers Prev 11:953–971
Collaborative group on hormonal factors in breast cancer (2002) Alcohol, tobacco and breast cancer—collaborative reanalysis of individual data from 53 epidemiological studies, including 58,515 women with breast cancer and 95,067 women without the disease. Br J Cancer 87:1234–1245
Baron JA, La Vecchia C, Levi F (1990) The antiestrogenic effect of cigarette smoking in women. Am J Obstet Gynecol 162:502–514
Michnovicz JJ, Hershcopf RJ, Naganuma H, Bradlow HL, Fishman J (1986) Increased 2-hydroxylation of estradiol as a possible mechanism for the anti-estrogenic effect of cigarette smoking. N Engl J Med 315:1305–1309
Hayes CL, Spink DC, Spink BC, Cao JQ, Walker NJ, Sutter TR (1996) 17 beta-estradiol hydroxylation catalyzed by human cytochrome P450 1B1. Proc Natl Acad Sci USA 93:9776–9781
Spink DC, Eugster HP, Lincoln DW 2nd, Schuetz JD, Schuetz EG, Johnson JA, Kaminsky LS, Gierthy JF (1992) 17 beta-estradiol hydroxylation catalyzed by human cytochrome P450 1A1: a comparison of the activities induced by 2,3,7,8-tetrachlorodibenzo-p- dioxin in MCF-7 cells with those from heterologous expression of the cDNA. Arch Biochem Biophys 293:342–348
Shimada T, Hayes CL, Yamazaki H, Amin S, Hecht SS, Guengerich FP, Sutter TR (1996) Activation of chemically diverse procarcinogens by human cytochrome P-450 1B1. Cancer Res 56:2979–2984
Liehr JG, Fang WF, Sirbasku DA, Ari-Ulubelen A (1986) Carcinogenicity of catechol estrogens in Syrian hamsters. J Steroid Biochem 24:353–356
Liehr JG, Ricci MJ (1996) 4-Hydroxylation of estrogens as marker of human mammary tumors. Proc Natl Acad Sci USA 93:3294–3296
Tsuchiya Y, Nakajima M, Kyo S, Kanaya T, Inoue M, Yokoi T (2004) Human CYP1B1 is regulated by estradiol via estrogen receptor. Cancer Res 64:3119–3125
Iwanari M, Nakajima M, Kizu R, Hayakawa K, Yokoi T (2002) Induction of CYP1A1, CYP1A2, and CYP1B1 mRNAs by nitropolycyclic aromatic hydrocarbons in various human tissue-derived cells: chemical-, cytochrome P450 isoform-, and cell-specific differences. Arch Toxicol 76:287–298
http://www.imm.ki.se/CYPalleles/cyp1a1.htm
http://www.imm.ki.se/CYPalleles/cyp1b1.htm
Spurr NK, Gough AC, Stevenson K, Wolf CR (1987) Msp-1 polymorphism detected with a cDNA probe for the P-450 I family on chromosome 15. Nucleic Acids Res 15:5901
Cascorbi I, Brockmoller J, Roots I (1996) A C4887A polymorphism in exon 7 of human CYP1A1: Population frequency, mutation linkages, and impact on lung cancer susceptibility. Cancer Res 56:4965–4969
Hayashi S, Watanabe J, Nakachi K, Kawajiri K (1991) Genetic linkage of lung cancer-associated MspI polymorphisms with amino acid replacement in the heme binding region of the human cytochrome P450IA1 gene. J Biochem (Tokyo) 110:407–411
Fontana X, Peyrottes I, Rossi C, Leblanc-Talent P, Ettore F, Namer M, Bussiere F (1998) Study of the frequencies of CYP1A1 gene polymorphisms and glutathione S- transferase mu1 gene in primary breast cancers: an update with an additional 114 cases. Mutat Res 403:45–53
Hirvonen A, Husgafvel-Pursiainen K, Karjalainen A, Anttila S, Vainio H (1992) Point-mutational MspI and Ile-Val polymorphisms closely linked in the CYP1A1 gene: lack of association with susceptibility to lung cancer in a Finnish study population. Cancer Epidemiol Biomarkers Prev 1:485–489
Crofts F, Cosma GN, Currie D, Taioli E, Toniolo P, Garte SJ (1993) A novel CYP1A1 gene polymorphism in African–Americans. Carcinogenesis 14:1729–1731
Cosma G, Crofts F, Taioli E, Toniolo P, Garte S (1993) Relationship between genotype and function of the human CYP1A1 gene. J Toxicol Environ Health 40:309–316
Crofts F, Taioli E, Trachman J, Cosma GN, Currie D, Toniolo P, Garte SJ (1994) Functional significance of different human CYP1A1 genotypes. Carcinogenesis 15:2961–2963
Landi MT, Bertazzi PA, Shields PG, Clark G, Lucier GW, Garte SJ, Cosma G, Caporaso NE (1994) Association between CYP1A1 genotype, mRNA expression and enzymatic activity in humans. Pharmacogenetics 4:242–246
Kiyohara C, Hirohata T, Inutsuka S (1996) The relationship between aryl hydrocarbon hydroxylase and polymorphisms of the CYP1A1 gene. Jpn J Cancer Res 87:18–24
Stoilov I, Akarsu AN, Alozie I, Child A, Barsoum-Homsy M, Turacli ME, Or M, Lewis RA, Ozdemir N, Brice G, Aktan SG, Chevrette L, Coca-Prados M, Sarfarazi M (1998) Sequence analysis and homology modeling suggest that primary congenital glaucoma on 2p21 results from mutations disrupting either the hinge region or the conserved core structures of cytochrome P4501B1. Am J Hum Genet 62:573–584
Bailey LR, Roodi N, Dupont WD, Parl FF (1998) Association of cytochrome P450 1B1 (CYP1B1) polymorphism with steroid receptor status in breast cancer. Cancer Res 58:5038–5041
McLellan RA, Oscarson M, Hidestrand M, Leidvik B, Jonsson E, Otter C, Ingelman-Sundberg M (2000) Characterization and functional analysis of two common human cytochrome P450 1B1 variants. Arch Biochem Biophys 378:175–181
Li DN, Seidel A, Pritchard MP, Wolf CR, Friedberg T (2000) Polymorphisms in P450 CYP1B1 affect the conversion of estradiol to the potentially carcinogenic metabolite 4-hydroxyestradiol. Pharmacogenetics 10:343–353
Shimada T, Watanabe J, Kawajiri K, Sutter TR, Guengerich FP, Gillam EM, Inoue K (1999) Catalytic properties of polymorphic human cytochrome P450 1B1 variants. Carcinogenesis 20:1607–1613
Hanna IH, Dawling S, Roodi N, Guengerich FP, Parl FF (2000) Cytochrome P450 1B1 (CYP1B1) pharmacogenetics: association of polymorphisms with functional differences in estrogen hydroxylation activity. Cancer Res 60:3440–3444
Aklillu E, Oscarson M, Hidestrand M, Leidvik B, Otter C, Ingelman-Sundberg M (2002) Functional analysis of six different polymorphic CYP1B1 enzyme variants found in an Ethiopian population. Mol Pharmacol 61:586–594
Krajinovic M, Ghadirian P, Richer C, Sinnett H, Gandini S, Perret C, Lacroix A, Labuda D, Sinnett D (2001) Genetic susceptibility to breast cancer in French–Canadians: role of carcinogen-metabolizing enzymes and gene-environment interactions. Int J Cancer 92:220–225
Miyoshi Y, Takahashi Y, Egawa C, Noguchi S (2002) Breast cancer risk associated with CYP1A1 genetic polymorphisms in Japanese women. Breast J 8:209–215
da Fonte de Amorim L, Rossini A, Mendonca G, Lotsch P, de Almeida Simao T, de Moura Gallo C, Pinto L (2002) CYP1A1, GSTM1, and GSTT1 polymorphisms and breast cancer risk in Brazilian women. Cancer Lett 181:179–186
Huang CS, Shen CY, Chang KJ, Hsu SM, Chern HD (1999) Cytochrome P4501A1 polymorphism as a susceptibility factor for breast cancer in postmenopausal Chinese women in Taiwan. Br J Cancer 80:1838–1843
Taioli E, Bradlow HL, Garbers SV, Sepkovic DW, Osborne MP, Trachman J, Ganguly S, Garte SJ (1999) Role of estradiol metabolism and CYP1A1 polymorphisms in breast cancer risk. Cancer Detect Prev 23:232–237
Hefler LA, Tempfer CB, Grimm C, Lebrecht A, Ulbrich E, Heinze G, Leodolter S, Schneeberger C, Mueller MW, Muendlein A, Koelbl H (2004) Estrogen-metabolizing gene polymorphisms in the assessment of breast carcinoma risk and fibroadenoma risk in Caucasian women. Cancer 101:264–249
Zhang Y, Wise JP, Holford TR, Xie H, Boyle P, Zahm SH, Rusiecki J, Zou K, Zhang B, Zhu Y, Owens PH, Zheng T (2004) Serum polychlorinated biphenyls, cytochrome P-450 1A1 polymorphisms, and risk of breast cancer in Connecticut women. Am J Epidemiol 160:1177–1183
Chacko P, Joseph T, Mathew BS, Rajan B, Pillai MR (2005) Role of xenobiotic metabolizing gene polymorphisms in breast cancer susceptibility and treatment outcome. Mutat Res 581:153–163
Dialyna IA, Arvanitis DA, Spandidos DA (2001) Genetic polymorphisms and transcriptional pattern analysis of CYP1A1, AhR, GSTM1, GSTP1 and GSTT1 genes in breast cancer. Int J Mol Med 8:79–87
Basham VM, Pharoah PD, Healey CS, Luben RN, Day NE, Easton DF, Ponder BA, Dunning AM (2001) Polymorphisms in CYP1A1 and smoking: no association with breast cancer risk. Carcinogenesis 22:1797–1800
Bailey LR, Roodi N, Verrier CS, Yee CJ, Dupont WD, Parl FF (1998) Breast cancer and CYPIA1, GSTM1, and GSTT1 polymorphisms: evidence of a lack of association in Caucasians and African Americans. Cancer Res 58:65–70
Rebbeck TR, Rosvold EA, Duggan DJ, Zhang J, Buetow KH (1994) Genetics of CYP1A1: coamplification of specific alleles by polymerase chain reaction and association with breast cancer. Cancer Epidemiol Biomarkers Prev 3:511–514
Ishibe N, Hankinson SE, Colditz GA, Spiegelman D, Willett WC, Speizer FE, Kelsey KT, Hunter DJ (1998) Cigarette smoking, cytochrome P450 1A1 polymorphisms, and breast cancer risk in the nurses’ health study. Cancer Res 58:667–671
Laden F, Ishibe N, Hankinson SE, Wolff MS, Gertig DM, Hunter DJ, Kelsey KT (2002) Polychlorinated biphenyls, cytochrome P450 1A1, and breast cancer risk in the nurses’ health study. Cancer Epidemiol Biomarkers Prev 11:1560–1565
Li Y, Millikan RC, Bell DA, Cui L, Tse CK, Newman B, Conway K (2004) Cigarette smoking, cytochrome P4501A1 polymorphisms, and breast cancer among African–American and white women. Breast Cancer Res 6:R460–R473
Miyoshi Y, Ando A, Hasegawa S, Ishitobi M, Yamamura J, Irahara N, Tanji Y, Taguchi T, Tamaki Y, Noguchi S (2003) Association of genetic polymorphisms in CYP19 and CYP1A1 with the oestrogen receptor-positive breast cancer risk. Eur J Cancer 39:2531–2537
Boyapati SM, Shu XO, Gao YT, Cai Q, Jin F, Zheng W (2005) Polymorphisms in CYP1A1 and breast carcinoma risk in a population-based case-control study of Chinese women. Cancer 103:2228–2235
Li Y, Millikan RC, Bell DA, Cui L, Tse CK, Newman B, Conway K (2005) Polychlorinated biphenyls, cytochrome P450 1A1 (CYP1A1) polymorphisms, and breast cancer risk among African American women and white women in North Carolina: a population-based case-control study. Breast Cancer Res 7:R12–R18
Ambrosone CB, Freudenheim JL, Graham S, Marshall JR, Vena JE, Brasure JR, Laughlin R, Nemoto T, Michalek AM, Harrington A et al (1995) Cytochrome P4501A1 and glutathione S-transferase (M1) genetic polymorphisms and postmenopausal breast cancer risk. Cancer Res 55:3483–3485
Moysich KB, Shields PG, Freudenheim JL, Schisterman EF, Vena JE, Kostyniak P, Greizerstein H, Marshall JR, Graham S, Ambrosone CB (1999) Polychlorinated biphenyls, cytochrome P4501A1 polymorphism, and postmenopausal breast cancer risk. Cancer Epidemiol Biomarkers Prev 8:41–44
Zheng W, Xie DW, Jin F, Cheng JR, Dai Q, Wen WQ, Shu XO, Gao YT (2000) Genetic polymorphism of cytochrome P450-1B1 and risk of breast cancer. Cancer Epidemiol Biomarkers Prev 9:147–150
Kocabas NA, Sardas S, Cholerton S, Daly AK, Karakaya AE (2002) Cytochrome P450 CYP1B1 and catechol O-methyltransferase (COMT) genetic polymorphisms and breast cancer susceptibility in a Turkish population. Arch Toxicol 76:643–649
De Vivo I, Hankinson SE, Li L, Colditz GA, Hunter DJ (2002) Association of CYP1B1 polymorphisms and breast cancer risk. Cancer Epidemiol Biomarkers Prev 11:489–492
Rylander-Rudqvist T, Wedren S, Granath F, Humphreys K, Ahlberg S, Weiderpass E, Oscarson M, Ingelman-Sundberg M, Persson I (2003) Cytochrome P450 1B1 gene polymorphisms and postmenopausal breast cancer risk. Carcinogenesis 24:1533–1539
Saintot M, Malaveille C, Hautefeuille A, Gerber M (2003) Interactions between genetic polymorphism of cytochrome P450–1B1, sulfotransferase 1A1, catechol-o-methyltransferase and tobacco exposure in breast cancer risk. Int J Cancer 107:652–657
Lee KM, Abel J, Ko Y, Harth V, Park WY, Seo JS, Yoo KY, Choi JY, Shin A, Ahn SH, Noh DY, Hirvonen A, Kang D (2003) Genetic polymorphisms of cytochrome P450 19 and 1B1, alcohol use, and breast cancer risk in Korean women. Br J Cancer 88:675–678
Thyagarajan B, Brott M, Mink P, Folsom AR, Anderson KE, Oetting WS, Gross M (2004) CYP1B1 and CYP19 gene polymorphisms and breast cancer incidence: no association in the ARIC study. Cancer Lett 207:183–189
Watanabe J, Shimada T, Gillam EM, Ikuta T, Suemasu K, Higashi Y, Gotoh O, Kawajiri K (2000) Association of CYP1B1 genetic polymorphism with incidence to breast and lung cancer. Pharmacogenetics 10:25–33
Dunning AM, Dowsett M, Healey CS, Tee L, Luben RN, Folkerd E, Novik KL, Kelemen L, Ogata S, Pharoah PD, Easton DF, Day NE, Ponder BA (2004) Polymorphisms associated with circulating sex hormone levels in postmenopausal women. J Natl Cancer Inst 96:936–945
Wen W, Cai Q, Shu XO, Cheng JR, Parl F, Pierce L, Gao YT, Zheng W (2005) Cytochrome P450 1B1 and catechol-O-methyltransferase genetic polymorphisms and breast cancer risk in Chinese women: results from the shanghai breast cancer study and a meta-analysis. Cancer Epidemiol Biomarkers Prev 14:329–335
Sillanpaa P, Hirvonen A, Kataja V, Eskelinen M, Kosma VM, Uusitupa M, Vainio H, Mitrunen K (2005) NAT2 slow acetylator genotype as an important modifier of breast cancer risk. Int J Cancer 114:579–584
Männistö S, Pietinen P, Pyy M, Palmgren J, Eskelinen M, Uusitupa M (1996) Body-size indicators and risk of breast cancer according to menopause and estrogen-receptor status. Int J Cancer 68:8–13
Mitrunen K, Jourenkova N, Kataja V, Eskelinen M, Kosma VM, Benhamou S, Vainio H, Uusitupa M, Hirvonen A (2000) Steroid metabolism gene CYP17 polymorphism and the development of breast cancer. Cancer Epidemiol Biomarkers Prev 9:1343–1348
Slattery ML, Edwards SL, Caan BJ, Kerber RA, Potter JD (1995) Response rates among control subjects in case-control studies. Ann Epidemiol 5:245–249
Mrozikiewicz PM, Cascorbi I, Brockmoller J, Roots I (1997) CYP1A1 mutations 4887A, 4889G, 5639C and 6235C in the Polish population and their allelic linkage, determined by peptide nucleic acid-mediated PCR clamping. Pharmacogenetics 7:303–307
Peltonen L, Jalanko A, Varilo T (1999) Molecular genetics of the Finnish disease heritage. Hum Mol Genet 8:1913–1923
de la Chapelle A (1993) Disease gene mapping in isolated human populations: the example of Finland. J Med Genet 30:857–865
Masson LF, Sharp L, Cotton SC, Little J (2005) Cytochrome P-450 1A1 gene polymorphisms and risk of breast cancer: a HuGE review. Am J Epidemiol 161:901–915
Ahsan H, Chen Y, Whittemore AS, Kibriya MG, Gurvich I, Senie RT, Santella RM (2004) A family-based genetic association study of variants in estrogen-metabolism genes COMT and CYP1B1 and breast cancer risk. Breast Cancer Res Treat 85:121–131
Vineis P (1997) Molecular epidemiology: low-dose carcinogens and genetic susceptibility. Int J Cancer 71:1–3
Jourenkova-Mironova N, Wikman H, Bouchardy C, Mitrunen K, Dayer P, Benhamou S, Hirvonen A (1999) Role of arylamine N-acetyltransferase 1 and 2 (NAT1 and NAT2) genotypes in susceptibility to oral/pharyngeal and laryngeal cancers. Pharmacogenetics 9:533–537
Hou SM, Ryberg D, Falt S, Deverill A, Tefre T, Borresen AL, Haugen A, Lambert B (2000) GSTM1 and NAT2 polymorphisms in operable and non-operable lung cancer patients. Carcinogenesis 21:49–54
Hou SM, Falt S, Yang K, Nyberg F, Pershagen G, Hemminki K, Lambert B (2001) Differential interactions between GSTM1 and NAT2 genotypes on aromatic DNA adduct level and HPRT mutant frequency in lung cancer patients and population controls. Cancer Epidemiol Biomarkers Prev 10:133–140
Han W, Kang D, Park IA, Kim SW, Bae JY, Chung KW, Noh DY (2004) Associations between breast cancer susceptibility gene polymorphisms and clinicopathological features. Clin Cancer Res 10:124–130
Acknowledgments
We thank our colleagues at the Kuopio Cancer Research Center and A.K. Lyytinen, R.,N., for data collection. This work was partly supported by ECNIS (Environmental Cancer Risk, Nutrition and Individual Susceptibility), a network of excellence operating within the European Union 6th Framework Program, Priority 5: ’’Food Quality and Safety” (Contract No 513943).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sillanpää, P., Heikinheimo, L., Kataja, V. et al. CYP1A1 and CYP1B1 genetic polymorphisms, smoking and breast cancer risk in a Finnish Caucasian population . Breast Cancer Res Treat 104, 287–297 (2007). https://doi.org/10.1007/s10549-006-9414-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-006-9414-6