Abstract
Among the different neuromodulation techniques, neurofeedback (NF) is gaining increasing interest in the treatment of children with attention-deficit/hyperactivity disorder (ADHD). In this article, a methodological framework is summarised considering the training as a neuro-behavioural treatment. Randomised controlled trials are selectively reviewed. Results from two smaller-scale studies are presented with the first study comprising a tomographic analysis over the course of a slow cortical potential (SCP) training and a correlational analysis of regulation skills and clinical outcome in children with ADHD. In the second study, ADHD-related behaviour was studied in children with tic disorder who either conducted a SCP training or a theta/low-beta (12–15 Hz) training (single-blind, randomised design). Both studies provide further evidence for the specificity of NF effects in ADHD. Based on these findings, a refined model of the mechanisms contributing to the efficacy of SCP training is developed. Despite a number of open questions concerning core mechanisms, moderators and mediators, NF (theta/beta and SCP) training seems to be on its way to become a valuable and ethically acceptable module in the treatment of children with ADHD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neuromodulation techniques are increasingly studied as potential therapeutics in neurology and psychiatry. For example, repetitive transcranial magnetic stimulation and deep brain stimulation appear to be promising treatments for various disorders (e.g., depression, obsessive–compulsive disorder, Parkinson’s disease, see other articles in this issue). In contrast to these ‘exogeneous’ neuromodulation techniques neurofeedback (NF) training leads to neuronal changes caused by the patient’s activity. In NF training, participants learn to modulate specific aspects of neural activity. It is an operant learning procedure: feedback of neural activity (based on EEG but also fMRI measures) is provided via visual and/or acoustic information and changes in the required direction are positively reinforced (Heinrich et al. 2007; Birbaumer, submitted, this issue).
EEG-based NF has gained increasing interest as a potential treatment option for children with attention-deficit/hyperactivity disorder (ADHD). As there are no external devices necessary to trigger neuroplastic changes and the therapeutic aim is a functional modification of brain activity in order to better cope with daily life situations, NF training in ADHD children seems to be justified from an ethical point of view. NF treatment has the potential to enhance the patient’s autonomic agency, defined as “the capacity to form and execute plans of action” (Glannon 2013). Additionally, as agency alone is not sufficient for behaviour control, the child must be able to “identify with or endorse the neural and mental health states that produce action” (Glannon 2013). Accordingly, the patient who is able to perform NF training should be seen as an autonomous agent.
Concerning safety aspects, in pediatric research it is suggested to categorize the EEG procedure itself as minimal risk (Radenbach and Wiesemann 2010). Up to now, we are not aware of any severe adverse events in NF feedback training, although safety aspects are not sufficiently documented (Lofthouse et al. 2010).
NF training seems to be attractive to children since it is commonly realised as a kind of computer game. Small drop-out rates were reported in previous studies (e.g. <10 % in Gevensleben et al. 2009a). Thus, acceptance (as a relevant ethical issue) may be considered high.
What is ADHD?
ADHD is one of the most prevalent child psychiatric disorders (prevalence of about 5 %; Polanczyk et al. 2007) characterised by developmentally inappropriate levels of hyperactivity, impulsivity and/or inattention. It is considered a clinically and pathophysiologically heterogeneous condition with different neurodevelopmental pathways accounting for this disorder (Banaschewski et al. 2005). Clinical guidelines recommend a multimodal treatment approach, tailored to the particular needs of a child (Taylor et al. 2004; Graham et al. 2011). Psychopharmacological treatments, mainly methylphenidate, behaviour therapy and parent counselling have proven to be effective (Faraone and Buitelaar 2010; Pelham and Fabiano 2008). However, there is still a need for effective treatment strategies in improving attentional as well as self-regulation capabilities in children with ADHD. Increasing evidence suggests neurofeedback to be such a treatment option within the framework of a multimodal treatment program (Gevensleben et al. 2012).
Methodological Framework and Empirical Evidence
Neurofeedback Protocols and Neuro-Behavioural Model
In a theta/beta training, the participant has to learn to decrease activity in the theta band (4–7.5 Hz) and to increase activity in the beta band (13–20 Hz) of the EEG (with feedback calculated e.g. from electrode Cz). Behaviourally, this is thought to correspond to an alert and focused but relaxed state. Earlier studies suggested that ADHD is characterised by increased theta and/or reduced beta activity at rest as well as during task processing (Barry et al. 2003; El-Sayed et al. 2002). However, recent studies question this notion or conclude that only a subgroup may be characterised by this deviant EEG pattern (Arns and Kenemans 2012; Liechti et al. 2013). Nevertheless, NF can be seen as a tool for enhancing specific cognitive or attentional states.
A sensorimotor rhythm (SMR, 12–15 Hz) training, which aims at increasing SMR activity can also be conducted. Recently, Arns and Kenemans (2012) presented a model for the mechanisms of SMR training related to ADHD. They hypothesize that, in a subgroup of ADHD patients (with sleeping problems), SMR training targets the sleep spindle circuitry resulting in vigilance stabilization. Secondary to sleep improvements, behavioural improvements follow.
A neurofeedback training of slow cortical potentials Footnote 1 (SCPs) is related to phasic regulation of cortical excitability. Surface-negative SCPs (reflecting increased cortical excitability; allocation of attentional resources) and surface-positive SCPs (reflecting reduced excitability/inhibition; a relaxed state) have to be generated over the sensorimotor cortex. The contingent negative variation (CNV), a SCP associated with cognitive preparation, was found to be reduced in children with ADHD in several event-related potential (ERP) studies suggesting a dysfunctional regulation of energetical resources in ADHD (Banaschewski and Brandeis 2007; Sergeant 2005). In this respect, NF training of slow cortical potentials could help to address this dysfunctional regulation of energetical resources.
There are different ways to realise a NF training depending on different assumptions related to the mechanisms of action. In a recent paper (Gevensleben et al. 2012), we proposed a hypothetical model of the active ingredients of NF training in ADHD considering NF a neuro-behavioural treatment, emphasising cognitive and motivational variables underlying the treatment. Nevertheless, improvements in neurophysiological self-regulation and thus, strengthened neuronal networks are regarded as a central mechanism.
Attention management including for example transfer trials during the training and implementation of the strategies into daily life are also considered to play a central role. These core components interact with personality variables such as self-efficacy and achievement motivation, with the neurophysiological profile of a subject as well as social reinforcement processes. So, these variables could also contribute to the success of NF training and—vice versa—may be modulated by the training (Gevensleben et al. 2012).
Information about the realisation of NF training as well as some technical details can be found in the Supplementary Material.
Design Issues
Earlier studies reported positive effects for the NF protocols mentioned above in reducing ADHD symptomatology. However, due to methodological shortcomings (e.g. small sample size, non-randomised design and inadequate control condition) firm conclusions are not possible. Randomised controlled trials (RCTs) are needed to further elucidate efficacy and specificity of NF.
There is an ongoing discussion about adequate control conditions in NF research. Some suggest using a placebo approach (e.g. Loo and Barkley 2005) as in medication trials where double-blind placebo-controlled randomised trials are considered the gold standard.
Is a placebo controlled NF-RCT in children with ADHD ethically acceptable?
On the one hand, it would be ethically unwise to principally deny placebo NF-RCTs if they are considered to provide great scientific value. Moreover, releasing a treatment to the market without sufficient understanding of their properties and knowledge about risks appears to be more problematic (Roberts et al. 2001). If trials with placebo groups (and any other control condition expected to provide no benefit) are run, designs summarised in Box 1 should be considered.
On the other hand, it has to be asked if it is ethically legitimate to work with sham feedback parameters and discuss the course of these parameters over a trial (interpreting it as reflecting the child’s mental state) in so many training units (usually about 30–40 over a period of several weeks to months). Concerning potential risks and benefits, patients and their families have at least to be well informed about and to consent to the possibility to be randomized into a sham feedback trial arm.
Methodological aspects argue against the use of a placebo control condition (Herbert and Gaudiano 2005; Omer and London 1989). Neurofeedback relies on learning (i.e. psychological mechanisms). In contrast to pharmacological treatments, the success of psychotherapeutic interventions is based on internal and external attributions (e.g. responsibility, self-control, treatment credibility, Goldstein and Shipman 1961; Plotkin 1980). These basic (“non-specific”) variables must be controlled, but should not be affected adversely by the control condition. Expecting to be part of the placebo group may seriously change attributions concerning locus of control and treatment credibility and thereby distract potential moderators of NF, particularly concerning self-efficacy and effort (Gevensleben et al. 2012).
Therefore, our group favours alternative (active) control conditions and to control for attributional effects e.g. via appropriate evaluation scales.
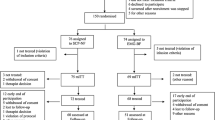
Empirical Evidence from Randomised Controlled Trials
In the (up to now) largest randomised controlled NF trial in ADHD (about 100 children with ADHD) we used a computerised attention skills training as a control condition, which was designed as similarly as possible concerning the setting (e.g., transfer into daily life) and the demands placed upon the participants. Positive results at the behavioural and neurophysiological level could be obtained (Gevensleben et al. 2009a, 2009b, 2010; Wangler et al. 2011).
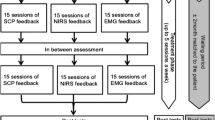
The NF training consisted of one block of theta/beta training and one block of SCP training allowing comparison of both protocols at the intraindividual level. Each training block consisted of 18 training units (duration: 50 min) only, i.e. the number of training units per protocol was relatively low.
According to parent and teacher ratings, reductions in the total score of the German ADHD rating scale (primary outcome measure) was greater for the NF training compared to the control condition (medium effect size of ca. 0.6) with comparable improvements for theta/beta training and SCP training. Superiority of NF was confirmed at 6-month follow-up. Parents of both groups did not differ on evaluation scales (e.g., expectations/satisfaction with the training). These clinical results provide clear evidence for the specificity of effects. Further evidence for specificity was obtained at the neurophysiological level (EEG and ERP analysis). For theta/beta training, theta activity over centro-parietal midline electrodes in the resting EEG (pre-training level, change from pre- to post-training) was associated with clinical improvements. For SCP training, alpha activity (pre-training level, change from pre- to post-training) predicted the clinical success.
A CNV increase, which had already been reported in Heinrich et al. (2004), may be interpreted as a neuroplastic change specific for SCP training. A higher pre-training CNV was a positive predictor of clinical outcome: being initially able to recruit more resources may facilitate transfer into daily life. Otherwise, these resources need to build up first.
In another RCT, Bakhshayesh et al. (2011) compared clinical and neuropsychological effects of theta/beta training to those of an EMG biofeedback training (reinforcer-controlled design). A large effect size for inattention and small to medium effect sizes for hyperactivity and impulsivity, respectively, also argue for the specificity of the effects of theta/beta training in ADHD.Footnote 2 At the neuropsychological level (attention tests), NF was also superior to the control condition though it has to be noted that sample size (total sample: n = 35) did not allow to detect medium effect sizes of about 0.5 with sufficient statistical power.
In placebo-controlled trials run so far, NF did not turn out to be superior to the placebo (sham) condition (Lansbergen et al. 2011; Arnold et al. 2012). Feasibility of blinding (providing sham feedback, not recognised by the participants), but not fidelity of the treatment under placebo-conditions could be shown in these studies (it is even unclear whether neuro-regulation has taken place during sessions). Furthermore, due to serious methodical limitations concerning the quality of the NF treatment (e.g., non-standard NF protocols were used, NF training did not follow operant learning principles, Sherlin et al. 2011), it is not possible to draw any firm conclusions based on these studies.
Further RCTs are on their way, e.g., a large multicentre study comparing SCP training to an EMG biofeedback training is about to be finished (Holtmann et al. http://www.controlled-trials.com/ISRCTN76187185), indicating the increasing scientific interest in NF as a treatment approach for children with ADHD. In the following, two smaller-scale studies are presented which may basically provide further evidence for the specificity of SCP training effects in ADHD and enhance our understanding of underlying mechanisms.
Study I: Specific Aspects of SCP Training in Children with ADHD
Background/Objective
As outlined above, children with ADHD benefit from SCP training. In addition, there is evidence for an association between the CNV measured in an attention task at pre-training and the success of a (18 unit) SCP training. Learning curves have been presented in two studies (Strehl et al. 2006; Drechsler et al. 2007) demonstrating that children with ADHD can actually learn self-regulation of SCPs. Strehl et al. (2006) reported that the ability to produce negative SCPs in transfer trials at the end of the training was associated with the clinical success of the training (indicating specificity).
Tomographic analysis (fMRI) indiciated that, in (healthy) adults who had learnt SCP self-regulation (feedback electrode Cz), generation of negativity was accompanied by widespread fMRI activation in central, dorsolateral prefrontal, and parietal brain regions as well as in the basal ganglia after the end of the training. Positivity was associated with widespread fMRI deactivations at several cortical sites (e.g. central areas) as well as some activation, primarily in frontal and parietal structures, and in the insula and putamen (Hinterberger et al. 2003). However, it has not yet been investigated which brain areas are involved during learning of SCP self-regulation. Tomographic analysis can also be done based on multichannel EEG using e.g. sLORETA (standardised low resolution brain electromagnetic tomography, Pascual-Marqui 2002) though with the constraints of limited spatial resolution and problems in the presence of noise.
We addressed these two issues (relation between regulation skill and clinical outcome; EEG-based tomographic analysis over the course of a SCP training) in a smaller SCP training study in boys with ADHD.
Methods
Subjects
10 boys (aged 10–13 years) were included in the study which was conducted at the Dept. of Child and Adolescent Mental Health, University Hospital of Erlangen. They were recruited from a NF waiting list, i.e., the families had applied for a NF training by themselves. Sample characteristics are summarised in Table 1.
ADHD diagnosis was based on a clinical interview by an experienced clinical psychologist and confirmed with the German ADHD rating scale (FBB-HKS, Döpfner and Lehmkuhl 2000). The diagnostic procedure was supervised by a board-certified child and adolescent psychiatrist.
In the clinical interview, it was also assured that the child is aware of his problems and sufficiently motivated. In this respect, the sample of this study may be considered more homogeneous compared to other studies (concerning motivational aspects).
Neurologic or comorbid psychiatric disorders other than conduct disorder, emotional disorder and dyslexia were considered as exclusionary criteria. IQ was required to be larger than 80 (HAWIK-IV). Children on medication (methylphenidate) were allowed to participate but had to keep medication constant during study participation.
Parents and children gave informed written consent. The study was approved by the Ethics Committee of the University Hospital of Erlangen and conducted according to the declaration of Helsinki.
Neurofeedback Training/Procedure
NF training consisted of 13 double-lesson sessions [duration of a session: ca. 105 (60 + 45) min]. The number of sessions per week varied between one and three depending on the family’s schedule.
Children should acquire appropriate strategies for producing negative and positive SCP shifts. Typically four blocks of 36–48 trials were conducted within a session. In one of these blocks, trials (without contingent feedback) were combined with an attention (S1–S2) task with S1 representing a cue stimulus and S2 a go or nogo stimulus. Interpreting SCP training as a neuro-behavioural treatment, transfer into daily life was practised in the training including integration of a real life situation (e.g. homework from school, contact to peers) starting at the sixth training session.
Comparable to our previous study, children had to do NF homework (e.g. ‘dry runs’, recognise situations where strategies could be useful) and a token system was applied: Successful regulation was rewarded in order to keep the children motivated. To support the children regarding transfer into daily life, parents attended one NF session in the first half as well as another in the second half.
Every fourth session (1st, 5th, 9th and 13th session), a 32-channel recording was done for an EEG-based tomographic analysis. In all other sessions, EEG activity was recorded from Cz vs. the right earlobe and vertical EOG was used to control and correct for eye movements/blinks (for details of EEG recording and analysis see Supplementary Material).
Behavioural (Clinical) Measures
In order to assess training effects at the behavioural level, parents were asked to fill out questionnaires before the beginning of the training and after the end of the complete training.
The German ADHD rating scale (FBB-HKS; Döpfner and Lehmkuhl 2000), a 20-item questionnaire related to DSM-IV and ICD-10 criteria for ADHD and hyperkinetic disorders, provides a total score and subscores for inattention and hyperactivity/impulsivity.
In addition, the German rating scale for oppositional defiant/conduct disorders (FBB-SSV; Döpfner and Lehmkuhl 2000) and the homework problem checklist (HPC, German version, Döpfner et al. 2002) were used to study effects in associated domains.
Data and Statistical Analysis
For pre- to post-training comparisons of clinical data, paired t tests were applied.
NF regulation/EEG data of every fourth session were analysed offline using the Vision Analyzer software (Brainproducts; Gilching, Germany). After preprocessing steps (incl. EOG correction and artefact control), averages for negativity and positivity trials were built. Mean amplitudes for the interval 4–8 s of the feedback phase were calculated.
To study if neuroregulation at the feedback electrode Cz in trials with contingent feedback was learnt successfully, a repeated-measure ANOVA with within-subject factors Session (1st, 5th, 9th, 13th) and Polarity (negativity, positivity) was computed.
Correlational analysis between neuroregulation measures (negativity and positivity in the 1st, 5th, 9th and 13th session as well as differences to the first session) and clinical outcome (FBB-HKS total score and subscales) was done in an exploratory manner (i.e. without correction for multiple comparisons).
To get a visual impression of the contributing cerebral sources, sLORETA solutions were computed for the grand average signals (negativity and positivity trials) of the 1st, 5th, 9th and 13th training session.
Results
All boys completed their training. Though post-training ratings may have been biased in two boys towards higher scores (escalating situation due to problems at school that came out; separation of the parents during study participation), we decided to include all children in the analysis which challenged particularly the correlational analysis.
Behavioural (Clinical) Level
ADHD symptomatology (FBB-HKS total score) was significantly reduced after the training (t(9) = 3.03, p = 0.014). Effects were slightly larger for the inattention subscale (ca. 25 % improvement) than for the hyperactivity/impulsivity subscale (about 20 % improvement; see also Table 1). In 7 of 10 boys, parent ratings showed a reduction of 40 % (responder criterion) and more in the FBB-HKS total score from pre- to post-training.
In associated domains, comparable effects were observed. For oppositional behaviour (t(9) = 2.41, p = 0.04), delinquent and physical aggression (t(9) = 3.77, p = 0.004) and homework problems (t(9) = 2.48, p = 0.035), large effect sizes were obtained.
Neuroregulation
The repeated-measure ANOVA revealed no main effects but a significant session × polarity interaction (F(3,27) = 4.36, p = 0.013) indicating that regulation improved over the course of the training. Children achieved negative mean amplitudes in negativity trials but were unable to reach positive mean amplitudes in positivity trials (see Figs. 1a, 2, left column).
a Mean amplitudes (and standard error) of negativity (red) and positivity trials (blue) over the course of a SCP training (1st, 5th, 9th, 13th session) in boys with ADHD. b Change of negativity (related to the 1st session) versus change of FBB-HKS inattention score for the 5th, 9th and 13th session. Linear regression lines are also depicted (Color figure online)
Left column grand average signals (at Cz) for negativity (red) and positivity trials (blue) at the 1st, 5th, 9th and 13th session of a SCP training in boys with ADHD. Please note that negative amplitudes are plotted upwards. Middle column sLORETA solutions for positivity trials. Right column sLORETA solutions for negativity trials (Color figure online)
The change of the FBB-HKS inattention score correlated with the change of negativity from the first to the fifth session (r = 0.65, p = 0.04) and from the first to the ninth session (r = 0.63, p = 0.05) but not with the change from the first to the last session (r = −0.05, n.s.) as illustrated in Fig. 1b. A comparable pattern was obtained when considering the negativities of the sessions absolutely, i.e., not related to the first session (5th session: r = 0.61, p = 0.06; 9th session: r = 0.61, p = 0.06; 13th session: r = −0.08, n.s.). Thus, a more negative mean amplitude in the fifth and ninth session was associated with a larger reduction of the inattention score.
For other neuro-regulation data, no significant correlations with clinical outcome measures were obtained.
Tomographic (sLORETA) Analysis
In the first session, main activations were found in prefrontal regions. As the training proceeded, activations involved mostly fronto-parietal areas as medial and superior frontal gyri, supplementary motor area, pre- and postcentral gyri as well as paracentral lobule. Note that these areas are located rather close to Cz (feedback electrode). Although activation patterns for positivity and negativity trials generally looked similar, there was a tendency for negativity trials to activate deeper structures, in particular the cingulate gyrus whereas activation for positivity trials rather remained at the cortical surface.
Discussion
Positive effects of SCP training on ADHD symptomatology and associated domains were obtained. The high responder rate of 70 % (despite a strict criterion) seems quite remarkable. Associations between the ability to produce negative SCP shifts and clinical improvements were obtained. Interestingly, negativity achieved in the fifth training session (corresponding to the 9th and 10th lesson) already predicted reductions of inattention at post-testing whereas no corresponding correlation was found for the negativity of the last training session. This finding will be discussed in more detail later when refining our neurobehavioural model of SCP training in ADHD.
Tomographic (sLORETA) analysis over the course of the training supports the notion that fronto-parietal networks contribute to the generation of SCPs. The finding of missing activation in the target region (motor cortex) in the first session but activation of prefrontal areas may be due to cognitive evaluation processes that are dominating when starting the training.
Whereas sLORETA solutions for the grand average ERPs were plausible, estimations for single subjects were rather inconsistent probably due to a low signal-to-noise ratio (for details see Kleemeyer 2010). This might at least partly explain why children with ADHD did not learn to self-regulate activity in the anterior cingulate cortex reliably in a sLORETA-based NF training (Liechti et al. 2012).
Study II: NF Effects on ADHD-Related Behaviour in Children with Tic Disorder
Background/Objective
Tics are involuntary, abrupt, mostly sudden, short non-rhythmic movements usually in circumscribed functional muscle groups (motor tics) and vocal utterances (vocal tics) that serve no obvious purpose. Inhibitory deficits and impaired neural synchronisation within the sensorimotor loops are assumed to underlie tic disorders. Particularly, striatal and thalamo-cortical networks are thought to be involved. Though tics are involuntary, patients often have some (conscious and unconscious) self-control to suppress/reduce their tics for a certain period of time (Leckman et al. 2006; Rothenberger and Roessner 2013).
ADHD is a common co-existing disorder in children with tic disorders (50–60 %) and the main factor in relation to psychosocial problems (Rothenberger and Roessner 2013). Within the motor system, distinct inhibitory deficits are described for tic disorders and ADHD supporting an additive model of comorbidity (Moll et al. 2001). When in co-existing TD plus ADHD cognitive aspects come into play, things are getting more complex and some interaction may take place (Banaschewski et al. 2007; Rothenberger and Roessner 2013).
To reduce tics, drugs (e.g., benzamides) are considered as therapy of first choice, habit reversal is the most important behavioural approach used (Roessner et al. 2012). In order to reduce accompanying ADHD problems stimulants may be given in parallel (Graham et al. 2011). It may be hypothesized that patients with TD + ADHD as well as with TD-only also benefit from NF training by ‘strengthening’ inhibitory and/or synchronisation capabilities within the sensorimotor system.
So far, only case reports on NF in tic disorders are available. Protocols aiming to increase SMR activity were typically applied and positive effects reported (e.g., Tansey 1986; Messerotti Benvenuti et al. 2011) but more research is necessary. Hence, we started to run a randomised trial to investigate the effects of SCP training and theta/low-beta (12–15 Hz) training.Footnote 3 With respect to tic symptomatology, comparable improvements for both NF protocols were expected. At the neurophysiological level (brain electrical activity, transcranial magnetic stimulation) distinct patterns may occur comparable to our NF study in ADHD (e.g., Gevensleben et al. 2009b). Here we report the results of an interim analysis with a focus on the effects on ADHD behaviour co-existing with tics.
Methods
Subjects
41 children (aged 9–16 years) with Tourette syndrome or chronic motor tic disorder (according to DSM-IV-R), IQ > 80 and without neurological disorders were randomly assigned (using a randomised list) to conduct either a SCP training (n = 20) or a theta/low-beta training (n = 21).
Interim analysis is based on 16 children of the SCP group and 14 children of the theta/low-beta group for whom ADHD pre- and post-training assessments were available. Sample characteristics are summarised in Table 2.
All participants were outpatients of the Department of Child and Adolescent Psychiatry, University Medicine Göttingen visiting the clinic for secondary opinion on tic/Tourette diagnosis. The clinic is a nationwide center for tic/Tourette diagnosis and treatment. Patients were assessed for tic disorder/Tourette syndrome and associated conditions by clinical interview, standardised inventories (e.g., Yale Global Tic Severity Scale, Leckman et al. 1989) and special interviews (e.g., C-Y-Bocs if screening for obsessive–compulsive behaviour was positive). The diagnostic procedure was supervised by a senior board-certified child and adolescent psychiatrist with special expertise in diagnosis and treatment of tic disorder/Tourette syndrome.
Patients with a confirmed diagnosis of chronic motoric tic disorder or Tourette syndrome and need for behavioural treatment were informed of the study. If wished by the patient and his family, a separate appointment was arranged and the patients were introduced to the treatment and passed a trial session.
The study follows the CONSORT guidelines for randomised trials (Boutron et al. 2008). A corresponding flow-chart can be found in the Supplementary Material. The study was approved by the ethics committee of the University Medicine Goettingen and conducted according to the declaration of Helsinki. Assent was obtained from the children and written informed consent from their parents.
Neurofeedback Training
The training was run as a two-week holiday course. A course comprised 6–8 training days with three training units of 50 min each scheduled in the morning. So, children conducted 18–24 training units. A training day consisted of about 80 min of neuroregulation, reflection about the regulation performance and associated strategies as well as exercises regarding the implementation of regulation strategies in daily life. Transfer trials, i.e. trials without contingent feedback (30 %, from the beginning of the training) as well as ‘dry runs’ from the second week on were intended to support the transfer into daily life.
In a SCP training session, typically 7–8 blocks of 30–40 trials of 8 s length each (2 s baseline, 6 s feedback phase) were run. Children were instructed that positivity corresponds to a relaxed state whereas negativity is associated with directing attention.
For theta/low-beta training, a 3 min baseline was recorded in the beginning of a training. For theta, threshold was set to 5 % above the baseline value; for low-beta, it was 5 % below the baseline value. If theta activity was lower and beta activity higher than these thresholds, the child received positive feedback. Typically, a theta/low-beta training session comprised 7–8 trials lasting 10 min each. Children were instructed to follow the feedback information and to regulate EEG parameters in the desired direction. Further instructions were provided according to individual concerns. Usually, the participants were told that it would help to get into/keep a relaxed but attentive state.
For both NF protocols, the program SAM (Self-regulation and Attention Monitoring) was used. EEG activity was recorded from Cz versus the left earlobe, vertical EOG was used to control and correct for eye movements/blinks (for details see Supplementary Material).
Parametrisation
Before the beginning of the training course, parents filled out questionnaires related to tic frequency and ADHD behaviour (pre-training assessment). About one to 5 weeks after the end of the training (not before the end of the vacation), these questionnaires were assessed again (post-training assessment).
Tic frequency was assessed using the Yale Tourette Symptom Scale (YTSS). ADHD behaviour was measured via the FBB-HKS. The FBB-HKS total score as well as subscores for inattention and hyperactivity/impulsivity were considered.
Statistical Analysis
For pre- and post-training comparisons (YTSS and FBB-HKS scores), group (SCP training, theta/low-beta training) × time (pre, post) ANOVAs were computed. For all statistical procedures, significance was assumed if p < 0.05. Effect sizes (part. η2) were computed with part. η2 > 0.01 indicating small, part. η2 > 0.06 medium, and part. η2 > 0.14 large effects (Cohen 1988).
Results
Both treatment groups did not differ significantly concerning tic frequency or ADHD behaviour at pre-training.
Tic frequency was reduced after the training (factor time: (F(1,24) = 7.81, p = 0.01, part. η2 = 0.246). The effect was comparable for both NF protocols as indicated by a non-significant group × time interaction (F(1,24) = 0.14, p = 0.72, part. η2 = 0.006).
For the FBB-HKS total score, the ANOVA revealed a significant time effect (F(1,28) = 5.55, p = 0.026, part. η2 = 0.165) as well as a significant group × time interaction (F(1,28) = 4.69, p = 0.039, part. η2 = 0.144): Training effects on comorbid ADHD behaviour were larger for SCP training compared to theta/low-beta training (see Table 3). This was mainly due to the symptom domain hyperactivity/impulsivity, where significant effects for the factor time (F(1,28) = 6.77, p = 0.015, part. η2 = 0.195) and the group × time interaction (F(1,28) = 4.85, p = 0.036, part. η2 = 0.148) were also obtained. Whereas reduction of hyperactive/impulsive behaviour was 26 % in the SCP group, nearly no improvement (reduction of 3 %) was observed in the theta/low-beta group. No significant effects were found for the inattention subscale—neither for the factor time: F(1,28) = 1.40, p = 0.246, part. η2 = 0.048) nor for the group × time interaction (F(1,28) = 1.67, p = 0.207, part. η2 = 0.056).
The same pattern of results (i.e., significant group × time interactions concerning the FBB-HKS total score and hyperactivity/impulsivity subscale) was obtained when only those children were included in the analysis, who had a diagnosis of comorbid ADHD.
Discussion
Reduction of tic frequency (large effect size) was comparable for SCP training and theta/low-beta training. The study design does not allow any conclusion about the specificity of this effect. However, it can be argued that it reflects a clinically relevant improvement. Relating the clinical outcome to neuroregulation skills and neurophysiological measures, respectively, may help to answer the question of specificity. This will be done after finishing the complete study.
NF protocol-specific effects on ADHD-related behaviour were obtained. SCP training was superior to theta/low-beta training in reducing ADHD behaviour primarily due to a reduction of hyperactive/impulsive behaviour. Why were the effects of SCP training larger concerning this symptom domain? In first line, the training was conducted as a treatment for tic disorders. So, the focus of transfer into daily life was related to inhibition of behaviour (i.e. tic suppression). With respect to ADHD, this rather concerns hyperactivity/impulsivity but not inattention. This would also explain why training effects on inattention were smaller compared to previous SCP training studies. And even more relevant, it underlines the necessity of implementing appropriate transfer into daily life in a SCP training.
Whereas theta/beta training led to comparable improvements as SCP training in our previous study in children with ADHD (Gevensleben et al. 2009a) as well as in Leins et al. (2007), theta/low-beta training did not actually affect ADHD behaviour in children with tic disorder. Different beta frequency bands (12–15 vs 13–20 Hz) and different threshold strategies may account for these diverging findings. On the other hand, no differences between SCP and theta/low-beta training were found with respect to tic frequency. We would prefer the notion that the aspect of comorbidity is the relevant factor, i.e., those children with ‘pure’ ADHD and those comorbid for tic disorder may reflect different subtypes responding differentially to theta/beta training.
In summary, both NF protocols turned out to be similarly effective concerning tic disorder, while the interim analysis provided further clear evidence for the specificity of NF effects on ADHD behaviour (advantage for SCP training). Findings related to generalisation allow to refine our model of SCP training in ADHD.
Refined Model of SCP Training in ADHD
In all SCP training studies in ADHD, SCP training was realised as a neuro-behavioural treatment: Self-control of SCPs was extensively practiced (with an active role for the participant) and transfer into daily life was explicitly addressed to support generalisation of effects. Accordingly, improved neuroregulation related to ‘strengthened’ neural networks and attention/self-management are considered to play a central role in our hypothetical model of ‘active ingredients’ (Gevensleben et al. 2012).
In the first study reported in this article, SCP-negativities achieved relatively early in the course of the training (at the 5th double-lesson) predicted reductions of inattention though this finding may have to be interpreted with caution due to the small sample size. We would not expect massive cortical reorganisation to happen within this small number of training sessions but rather suggest that children learn/become aware of how to access a specific mechanism and get into a specific state—related to negativities: how to recruit neural resources reflecting preparation.
In Wangler et al. (2011), children with a higher pre-training CNV in an attention task (i.e., initially being able to allocate more resources) took more benefit from the SCP training (see also “Empirical evidence“ section above). In the attention task, allocation of resources appears to be externally guided by the task demands. As a next step, it seems to be important that these resources can be recruited voluntarily. If neural resources are available and can be accessed voluntarily then transfer of goal oriented behaviour into daily life seems to be more successful.
What should transfer aim at? In the second study of this article investigating NF effects on ADHD behaviour in children with tic disorders, SCP training primarily reduced hyperactivity/impulsivity. This contrast to pure ADHD studies derives probably from the fact that transfer of tic control focused on behavioural inhibition and not (as in ADHD studies) on attention; i.e., SCP-NF may be directed to a specific goal depending on the problem to be solved. This finding underlines the importance of focused/generalized transfer to directly apply the newly acquired self-regulatory skills in concrete everyday life situations, socially reinforced by significant others. We assume that this initially controlled cognitive processing (self-regulation in distinct situations, e.g. homework) will progressively become automatic and leave higher-order self-regulatory resources to guide further behaviour.
In Wangler et al. (2011), we already argued that the CNV at pre-training should be regarded as an indicator for the number of SCP training units rather than a general predictor for success. In study I, negativity of the last session was not correlated with reduction of inattention (in contrast to the 5th and 9th session) due to an increase in negativity (compared to previous sessions) in children with poor outcome. It may be hypothesized that these children needed more time to acquire appropriate strategies/to build up adequate resources. If training was prolonged, at least part of them would supposedly benefit more from the training.
On the other hand, considerably longer trainings may induce motivational problems even if the children started the training with sufficient motivation. Thus, potential moderating factors come into play which could affect training outcome. Besides personality factors, the neurophysiological profile of a child as well as psychosocial factors (e.g., parental support, Drechsler et al. 2007) may reflect potential moderators that are also expected to be—vice versa—modulated by the training (Gevensleben et al. 2012). Potential moderators and interactions will have to be investigated systematically in future studies in order to refine the model further and to ‘feed’ it with empirical evidence.
Conclusions and Future Directions
There is clear evidence for specific effects of NF (primarily SCP training and theta/beta training) in ADHD based on randomised trials, comparison of different NF protocols and associations between neurophysiological measures/neuroregulation and clinical outcome. However, medium effect sizes (in adequately controlled trials) indicate that NF should not be seen as a stand-alone intervention but rather as a module within a multimodal treatment tailored to the particular needs of a child.
The findings of the two smaller-scale studies presented in this article allowed refining our neuro-behavioural model of SCP training in ADHD concerning core mechanisms and transfer into daily life. Nevertheless, a number of open questions remain as to mechanisms of action, moderators and mediators of the training. There are different models and ways of application so that only one or a few specific aspects can be considered by a single study (Gevensleben et al., submitted).
As NF trials are rather time-consuming, Ros et al. (2010, 2013) documented neuroplastic effects directly after a single session of NF training. Though such short-term designs do not supplant evaluation studies, they may facilitate knowledge about the functional significance of a certain NF protocol. In the field of ADHD, this seems to be relevant for theta/beta training where a clear rationale is currently missing.
Tomographic NF may allow a more specific training leading to larger clinical improvements. In this respect, faster learning is reported for fMRI-based NF (Birbaumer, submitted). However, the diverging solutions of the sLORETA analyses for single subjects as obtained in our SCP study indicate that some methodical adaptions may be necessary to make sLORETA-based NF more robust.
We reflected ethical and methodological aspects concerning study design which are discussed controversially in the scientific community. Concerning placebo-controlled trials, feasibility has not yet been documented sufficiently. We stated to favour alternative research strategies to ensure efficacy and specificity of treatments, well-documented in the psychotherapy research literature and guidelines for evidence-based medicine (Chambless and Ollendick 2001).
We may conclude that neurofeedback seems to be on its way to become a valuable and ethically acceptable treatment module for children with ADHD with room for further improvements (optimisation and individualisation of training, methodical advancements).
Notes
A comprehensive review about SCPs is provided in Birbaumer et al. (1990).
Originally, a SMR training was intended to be run. However, as a SMR training is recommended to reinforce a specific SMR spindle with duration of 0.25 s (Sherlin et al. 2011), which has not been done in our study, we decided to name the protocol 'theta/low-beta'.
References
Arnold LE, Lofthouse N, Hersch S, Pan X, Hurt E, Bates B, Kassouf K, Moone S, Grantier C (2012) EEG neurofeedback for ADHD: double-blind sham-controlled randomized pilot feasibility trial. J Atten Disord. doi:10.1177/1087054712446173
Arns M, Kenemans JL (2012) Neurofeedback in ADHD and insomnia: vigilance stabilization through sleep spindles and circadian networks. Neurosci Biobehav Rev. doi:10.1016/j.neubiorev.2012.10.006
Arns M, de Ridder S, Strehl U, Breteler M, Coenen A (2009) Efficacy of neurofeedback treatment in ADHD: the effects on inattention, impulsivity and hyperactivity: a meta-analysis. Clin EEG Neurosci 40:180–189
Bakhshayesh AR, Hänsch S, Wyschkon A, Rezai MJ, Esser G (2011) Neurofeedback in ADHD: a single-blind randomized controlled trial. Eur Child Adolesc Psychiatry 20(9):481–491
Banaschewski T, Brandeis D (2007) Annotation: what electrical brain activity tells us about brain function that other techniques cannot tell us: a child psychiatric perspective. J Child Psychol Psychiatry 48:415–435
Banaschewski T, Hollis C, Oosterlaan J, Roeyers H, Rubia K, Willcutt E, Taylor E (2005) Towards an understanding of unique and shared pathways in the psychopathophysiology of ADHD. Dev Sci 8(2):132–140
Banaschewski T, Neale BM, Rothenberger A, Roessner V (2007) Comorbidity of tic disorders & ADHD: conceptual and methodological considerations. Eur Child Adolesc Psychiatry 16(Suppl 1):5–14
Barry RJ, Clarke AR, Johnstone SJ (2003) A review of electrophysiology in attention deficit/hyperactivity disorder: I. Qualitative and quantitative electroencephalography. Clin Neurophysiol 114:171–183
Birbaumer N, Elbert T, Canavan AG, Rockstroh B (1990) Slow potentials of the cerebral cortex and behavior. Physiol Rev 70(1):1–41
Boutron I, Moher D, Douglas G, Altman G, Schulz F, Ravaud P (2008) Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med 148:295–310
Chambless DL, Ollendick TH (2001) Empirically supported psychological interventions: controversies and evidence. Annu Rev Psychol 52:685–716
Cohen JD (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Erlbaum, Hillsdale
Döpfner M, Lehmkuhl G (2000) DISYPS-KJ: Diagnostik-System für psychische Störungen im Kindes- und Hugendalter. Hans Huber, Bern
Döpfner M, Schürmann S, Frölich J (2002) Therapieprogramm für kinder mit hyperkinetischem und oppositionellem problemverhalten (THOP). Beltz, Weinheim
Drechsler R, Straub M, Doehnert M, Heinrich H, Steinhausen HC, Brandeis D (2007) Controlled evaluation of a neurofeedback training of slow cortical potentials in children with attention deficit/hyperactivity disorder (ADHD). Behav Brain Funct 3:35
El-Sayed E, Larsson JO, Persson HE, Rydelius PA (2002) Altered cortical activity in children with attention-deficit/hyperactivity disorder during attentional load task. J Am Acad Child Adolesc Psychiatry 41:811–819
Faraone SV, Buitelaar J (2010) Comparing the efficacy of stimulants for ADHD in children and adolescents using meta-analysis. Eur Child Adolesc Psychiatry 19(4):353–364
Freedman B (1987) Equipoise and the ethics of clinical research. N Engl J Med 317:141–145
Gevensleben H, Holl B, Albrecht B, Vogel C, Schlamp D, Kratz O, Studer P, Rothenberger A, Moll GH, Heinrich H (2009a) Is neurofeedback an efficacious treatment for ADHD? A randomised controlled clinical trial. J Child Psychol Psychiatry 50:780–789
Gevensleben H, Holl B, Albrecht B, Schlamp D, Kratz O, Studer P, Wangler S, Rothenberger A, Moll GH, Heinrich H (2009b) Distinct EEG effects related to neurofeedback training in children with ADHD: a randomized controlled trial. Int J Psychophysiol 74:149–157
Gevensleben H, Holl B, Albrecht B, Schlamp D, Kratz O, Studer P, Rothenberger A, Moll GH, Heinrich H (2010) Neurofeedback training in children with ADHD: 6-month follow-up of a randomised controlled trial. Eur Child Adolesc Psychiatry 19(9):715–724
Gevensleben H, Moll GH, Rothenberger A, Heinrich H (2012) Neurofeedback in children with ADHD: validation and challenges. Expert Rev Neurother 12(4):447–460
Gevensleben H, Moll GH, Rothenberger A, Heinrich H (submitted) Neurofeedback in attention-deficit/hyperactivity disorder: different models and ways of application
Glannon W (2013) Neuromodulation, agency and autonomy. Brain Topogr. doi:10.1007/s10548-012-0269-3
Goldstein AP, Shipman WG (1961) Patient expectancies, symptom reduction and aspects of the initial psychotherapeutic interview. J Clin Psychol 17:129–133
Graham J, Banaschewski T, Buitelaar J, Coghill D, Danckaerts M, Dittmann RW, Döpfner M, Hamilton R, Hollis C, Holtmann M, Hulpke-Wette M, Lecendreux M, Rosenthal E, Rothenberger A, Santosh P, Sergeant J, Simonoff E, Sonuga-Barke E, Wong IC, Zuddas A, Steinhausen HC, Taylor E, For the European Guidelines Group (2011) European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry 20:17–37
Heinrich H, Gevensleben H, Freisleder FJ, Moll GH, Rothenberger A (2004) Training of slow cortical potentials in ADHD: evidence for positive behavioral and neurophysiological effects. Biol Psychiatry 55(7):772–775
Heinrich H, Gevensleben H, Strehl U (2007) Annotation: neurofeedback: train your brain to train behaviour. J Child Psychol Psychiatry 48(1):3–16
Herbert JD, Gaudiano BA (2005) Moving from empirically supported treatment lists to practice guidelines in psychotherapy: the role of the placebo concept. J Clin Psychol 61(7):893–908
Hinterberger T, Veit R, Strehl U, Trevorrow T, Erb M, Kotchoubey B, Flor H, Birbaumer N (2003) Brain areas activated in fMRI during self-regulation of slow cortical potentials (SCPs). Exp Brain Res 152(1):113–122
Kleemeyer M (2010) Self-regulation of slow cortical potentials in children with attention-deficit/hyperactivity disorder: a tomographic analysis over the course of a neurofeedback-training. Master Thesis, University of Bremen
Lansbergen MM, van Dongen-Boomsma M, Buitelaar JK, Slaats-Willemse D (2011) ADHD and EEG-neurofeedback: a double-blind randomized placebo-controlled feasibility study. J Neural Transm 118(2):275–284
Leckman JF, Riddle MA, Hardin MT, Ort SI, Swartz KL, Stevenson J, Cohen DJ (1989) The Yale Global Tic Severity Scale: initial testing of a clinician-rated scale of tic severity. J Am Acad Child Adolesc Psychiatry 28(4):566–573
Leckman JF, Vaccarino FM, Kalanithi PS, Rothenberger A (2006) Annotation: tourette syndrome: a relentless drumbeat–driven by misguided brain oscillations. J Child Psychol Psychiatry 47(6):537–550
Leins U, Goth G, Hinterberger T, Klinger C, Rumpf N, Strehl U (2007) Neurofeedback for children with ADHD: a comparison of SCP and theta/beta protocols. Appl Psychophysiol Biofeedback 32(2):73–88
Liechti M, Maurizio S, Heinrich H, Jäncke L, Meier L, Steinhausen HC, Walitza S, Drechsler R, Brandeis D (2012) First clinical trial of tomographic neurofeedback in attention-deficit/hyperactivity disorder: evaluation of voluntary cortical control. Clin Neurophysiol 123(10):1989–2005
Liechti MD, Valko L, Müller UC, Döhnert M, Drechsler R, Steinhausen HC, Brandeis D (2013) Diagnostic value of resting electroencephalogram in attention-deficit/hyperactivity disorder across the lifespan. Brain Topogr 26(1):135–151
Lofthouse N, Arnold L, Hurt E (2010) A comment on Sherlin, Arns, Lubar, and Sokhadze. J Neutother 14(4):301–306
Loo SK, Barkley RA (2005) Clinical utility of EEG in attention deficit hyperactivity disorder. Appl Neuropsychol 12(2):64–76
Messerotti Benvenuti S, Buodo G, Leone V, Palomba D (2011) Neurofeedback training for tourette syndrome: an uncontrolled single case study. Appl Psychophysiol Biofeedback 36(4):281–288
Moll GH, Heinrich H, Trott GE, Wirth S, Bock N, Rothenberger A (2001) Children with comorbid attention-deficit-hyperactivity disorder and tic disorder: evidence for additive inhibitory deficits within the motor system. Ann Neurol 49(3):393–396
Omer H, London P (1989) Signal and noise in psychotherapy. The role and control of non-specific factors. Br J Psychiatry 155:239–245
Pascual-Marqui RD (2002) Standardized low-resolution brain electromagnetic tomography (sLORETA): technical details. Methods Find Exp Clin Pharmacol 24(Suppl D):5–12
Pelham WE Jr, Fabiano GA (2008) Evidence-based psychosocial treatments for attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol 37(1):184–214
Plotkin WB (1980) The role of attributions of responsibility in the facilitation of unusual experiential states during alpha training: an analysis of the biofeedback placebo effect. J Abnorm Psychol 89(1):67–78
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007) The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 164(6):942–948
Radenbach K, Wiesemann C (2010) Risiko und Belastung als Kriterien der Zulässigkeit von Forschung mit Kindern und Jugendlichen. In: Marckmann G, Niethammer D (eds) Ethische Aspekte pädiatrischer Forschung. Deutscher Ärzte-Verlag, Köln, pp 37–49
Roberts LW, Lauriello J, Geppert C, Keith SJ (2001) Placebos and paradoxes in psychiatric research: an ethics perspective. Biol Psychiatry 49:887–893
Roessner V, Schoenefeld K, Buse J, Wanderer S, Rothenberger A (2012) Therapy of tic disorders. Z Kinder Jugendpsychiatr Psychother 40(4):217–236
Ros T, Munneke MA, Ruge D, Gruzelier JH, Rothwell JC (2010) Endogenous control of waking brain rhythms induces neuroplasticity in humans. Eur J Neurosci 31(4):770–778
Ros T, Théberge J, Frewen PA, Kluetsch R, Densmore M, Calhoun VD, Lanius RA (2013) Mind over chatter: plastic up-regulation of the fMRI salience network directly after EEG neurofeedback. Neuroimage 65:324–335
Rothenberger A, Roessner V (2013) The phenomenology of attention-deficit/hyperactivity disorder in Tourette syndrome. In: Martino D, Leckman JF (eds) Tourette syndrome. Oxford Press, New York
Sergeant JA (2005) Modeling attention-deficit/hyperactivity disorder: a critical appraisal of the cognitive-energetic model. Biol Psychiatry 57:1248–1255
Sherlin LH, Arns M, Lubar J, Heinrich H, Kerson C, Strehl U, Sterman MB (2011) Neurofeedback and basic learning theory: implications for research and practice. Journal of Neurotherapy 15:292–304
Strehl U, Leins U, Goth G, Klinger C, Hinterberger T, Birbaumer N (2006) Self-regulation of slow cortical potentials: a new treatment for children with attention-deficit/hyperactivity disorder. Pediatrics 118(5):e1530–e1540
Tansey MA (1986) A simple and a complex tic (Gilles de la Tourette’s syndrome): their response to EEG sensorimotor rhythm biofeedback training. Int J Psychophysiol 4(2):91–97
Taylor E, Döpfner M, Sergeant J, Asherson P, Banaschewski T, Buitelaar J, Coghill D, Danckaerts M, Rothenberger A, Sonuga-Barke E, Steinhausen HC, Zuddas A (2004) European clinical guidelines for hyperkinetic disorder: first upgrade. Eur Child Adolesc Psychiatry 13(Suppl 1):I7–I30
Wangler S, Gevensleben H, Albrecht B, Studer P, Rothenberger A, Moll GH, Heinrich H (2011) Neurofeedback in children with ADHD: specific event-related potential findings of a randomized controlled trial. Clin Neurophysiol 122(5):942–950
Acknowledgments
The studies included in this paper were supported by the German Research Foundation (study I, HE 4536/2, MO 726/2) and the Tourette Gesellschaft Deutschland (study II). The authors thank the participating families (particularly the children) and all colleagues and students contributing to these studies.
Author information
Authors and Affiliations
Corresponding author
Additional information
This is one of several papers published together in Brain Topography on the “Special Topic: Clinical and Ethical Implications of Neuromodulation Techniques”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gevensleben, H., Kleemeyer, M., Rothenberger, L.G. et al. Neurofeedback in ADHD: Further Pieces of the Puzzle. Brain Topogr 27, 20–32 (2014). https://doi.org/10.1007/s10548-013-0285-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10548-013-0285-y