Abstract
Diabetes mellitus is a metabolic disease characterized by, among others, elevated blood glucose levels. Hyperglycaemia as well as enhanced levels of glucose-derived reactive metabolites contribute to the development of diabetic complications partly via increased generation of reactive oxygen species (ROS). ROS are not only part of signaling pathways themselves but also lead to carbonylation of particular amino acid side chains by direct metal-catalyzed oxidation. In addition, carbonyl groups can be introduced into proteins indirectly by non-oxidative covalent adduction of reactive carbonyl species generated by the oxidation of lipids or carbohydrates. Both direct and indirect carbonylation mechanisms may affect protein conformation, activity, and function. Herein we introduce the different mechanisms of the carbonylation reaction, discuss degradation mechanisms, and the fate of proteins modified this way and how the overall degree of carbonylation affects protein homeostasis and function differently. The role of protein carbonylation in metabolic control systems and cell signaling are also summarized. Finally, current diagnostic and antioxidant therapeutic options in diabetes are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is a metabolic disorder of glucose metabolism characterized by an increased level of reactive oxygen species (ROS) in combination with hyperglycaemia, which lead to the formation of reactive carbonyl-containing intermediates such as glyoxal and methylglyoxal (MG) derived from the oxidation of glucose. Excessive cellular ROS formation arises as a result of an imbalance between the more or less continuous generation of these reactive intermediates and the cellular capacity for their detoxification (Zatalia and Sanusi 2013). Typically, hyperglycaemia causes an increase in oxidative chemical modification of lipids and DNA but also leads to non-enzymatic MG–thiol adduction or metal-catalyzed carbonylation of proteinogenic amino acids (Maisonneuve et al 2009; Giacco and Brownlee 2010; Higdon et al 2012).
Protein carbonylation represents the most common type of non-enzymatic post-translational modification (PTM). Carbonyl groups are introduced into proteins by an oxidative (direct) or non-oxidative (indirect) mechanism and it appears that the “choice” is not at random.
Firstly, direct iron-catalyzed oxidation involves the reaction of certain ROS (e.g., hydrogen peroxide, lipid hydroperoxides, etc.) with specific amino acids (Cattaruzza and Hecker 2008). It selectively occurs at the protein surface within hot spots of carbonylation enriched for the susceptible amino acids arginine, lysine, proline or threonine, and it seems to be self-enhancing since carbonylation increases the reactivity of neighboring carbonylatable sites (Maisonneuve et al 2009). ROS production results from either radical-induced modification of molecular oxygen or incomplete consumption of molecular oxygen resulting in superoxide anion formation (Curtis et al 2010). Normally, these superoxide anions are efficiently converted by superoxide dismutases to hydrogen peroxide that in turn is transformed into water by catalase, glutathione peroxidase or peroxiredoxin/thioredoxins (Curtis et al 2010). In the presence of free iron (II), hydrogen peroxide can be readily converted via the Fenton reaction to hydroxyl radicals (Fig. 1) which in turn reacts directly with the mentioned amino acids.
Carbonylation biochemistry. Formation of protein carbonyls by direct metal ion-dependent oxidation or reaction with carbonyl compounds derived from autoxidation of carbohydrates and lipoxidation products. 4-HNE, 4-hydroxy trans-2,3-nonenal; 4-ONE, 4-oxo trans-2,3-nonenal; GPx, glutathione peroxidase; PRDX, peroxyredoxin; SOD, superoxide dismutase
Secondly, carbonyl groups are indirectly introduced into proteins by non-oxidative covalent adduction of reactive carbonyl species (RCS) to side chains of the nucleophilic amino acids arginine, lysine, and cysteine. These RCS are derived from hydroxyl radical-mediated oxidation of lipids (e.g., 4-hydroxy trans-2,3-nonenal (4-HNE), malondialdehyde (MDA), acrolein) and autoxidation of carbohydrates (e.g., glyoxal, MG) (Adams et al 2001) (Fig. 1). Reactive lipid aldehydes and their derivatives are normally detoxified by a variety of phase I and phase II systems (Curtis et al 2010). Phase I metabolism decreases the reactivity of these reactive lipid aldehydes via oxidation and reduction reactions by aldehyde dehydrogenases, aldo-keto reductases, and alkenal/one oxidoreductase (Frohnert and Bernlohr 2013). Phase II metabolism of reactive aldehydes is carried out primarily by enzymatic glutathionylation. In the case of 4-HNE, this occurs chiefly via the action of glutathione S-transferases, such as glutathione S-transferase A4 (GSTA4), as well as nonenzymatically (Frohnert and Bernlohr 2013). The resulting glutathionylated molecule (e.g., GS-HNE) can undergo further metabolic modification by aldo-keto reductases and aldehyde dehydrogenases (Curtis et al 2010).
MG, a common intermediate in the Maillard reaction of glucose (Oya et al 1999), is known to trigger formation of advanced glycation end products (AGEs) through protein glycation, which disrupts the secondary protein structure of an enzyme. Changes in protein structure such as this one might explain an alteration in function as compared to unmodified proteins (Suravajjala et al 2013). Moreover, misfolding of a protein may not only lead to a loss of function but may also mark it for proteolytic degradation (Diaz-Villanueva et al 2015). Normally, MG is detoxified by the glyoxalase system into D-lactate, with glyoxalase I (GLO1) as the key enzyme in anti-glycation defense (Maessen et al 2015).
Role of carbonylation in protein degradation
Cumulative protein carbonylation has been proven valuable as a biomarker for protein oxidation in aging and disease. On a functional level, it has been shown to impair protein structure and function (Fedorova et al 2014). Recently, a study profiled carbonylated proteins in plasma samples obtained from lean individuals and obese patients with or without type 2 diabetes (T2D) (Bollineni et al 2014). Among the identified 158 unique carbonylated proteins were 36 carbonylated proteins detected only in obese patients with T2D. Functionally, these proteins are implicated in cell adhesion, cytoskeletal remodeling, intracellular signaling and angiogenesis, cellular processes frequently associated with diabetes, obesity, and metabolic diseases.
Highly oxidized proteins appear to be relatively poor substrates for ubiquitination. Therefore, the ubiquitin-proteasome-system does not seem to be involved in the recognition or targeting of oxidized proteins. Highly carbonylated proteins have been reported to be dysfunctional and to accumulate as protein aggregates, cross-linked covalently, making them highly resistant to proteolysis (Nystrom 2005). The inability to degrade these extensively oxidized proteins seems to adversely affect the general functional integrity of cells during diseases and the aging process (Nystrom 2005).
In contrast, mild oxidization of proteins results in their increased susceptibility to proteasomal degradation largely due to unfolding of the targeted protein domains and exposure of hydrophobic amino acids. These hydrophobic surface patches seem to represent a major recognition motif by the 20S ‘core’ proteasome and the ATP-dependent serine-protease Lon (La) (Jung and Grune 2008; Lee and Suzuki 2008). Interestingly, recent studies have shown that the 19S and 20S proteasome subunits themselves are susceptible to oxidative modifications, including carbonylation and HNE modification suppressing their proteolytic activities (Aiken et al 2011). In the case of T1D, hyperglycaemia-induced formation of MG has been shown to covalently modify the 20S proteasome, decreasing its activity in the diabetic kidney of hyperglycaemic Ins2 Akita and streptozotocin-diabetic mice and reducing the polyubiquitin receptor 19S–S5a (Queisser et al 2010). Also, in non-insulin-dependent T2D patients, proteasomal dysfunction may exacerbate metabolic disorders in the skeletal muscle (Al-Khalili et al 2014) by imparting an insulin-resistant gene expression signature (Konstantopoulos et al 2011).
Metabolic control systems and protein carbonylation in diabetes
Conditions of increased oxidative stress compromise antioxidant defense systems. As a consequence, the overall cellular load with protein carbonyls is increased (Nystrom 2005). These PTMs have been implicated as causative in a variety of pathological metabolic states including neurodegeneration, muscle wasting, insulin resistance, and aging (Curtis et al 2012). Although such modifications usually result in loss of protein function, protein carbonylation may also be beneficial by regulating and activating signaling pathways involved in antioxidant defense and cellular homeostasis (Curtis et al 2012), as described in the following sections.
As outlined above protein carbonylation is chemically and not enzymatically driven. Thus, this post-translational modification depends on the cellular redox environment, the abundance of ROS and their proximity to the protein. Mitochondria play a central role in cellular energy metabolism. Since the mitochondrial respiratory chain constitutes a major source of superoxide anions with the mitochondrial manganese superoxide dismutase (SOD2) converting them to hydrogen peroxide, it is not surprising that a large proportion of carbonylated proteins is found within this organelle (Curtis et al 2012). Substantial evidence of mitochondrial dysfunction in diabetic hearts was already gathered 30 years ago when reduced state 3 respiration of mitochondria isolated from hearts of obese and type 2 diabetic db/db mice was first demonstrated (for a recent review refer to (Bugger and Abel 2014). Mechanisms underlying an impaired oxidative capacity of mitochondria, and concomitantly an altered morphology, include oxidative damage, transcriptional and translational alterations in oxidative phosphorylation (OXPHOS) subunit expression, impaired mitochondrial calcium handling and changes in cardiac insulin signaling (Bugger and Abel 2008; Konig et al 2012). However, reactive oxygen intermediates like H2O2 or O2 •− can diffuse through aquaporin or anion channels across cell membranes (Fisher 2009), so location of the carbonylated proteins does not necessarily define the source of such ROS (Curtis et al 2012).
Chronic hyperglycaemia and subsequent ROS formation can affect the regulation of metabolic pathways and provoke aberrant signaling pathways involving diverse signaling molecules or enzyme activities. As an example, thioredoxin-interacting protein (TxNIP) has been found to be up-regulated by high glucose and associated with oxidative stress (Shah et al 2013). TxNIP is a critical component of the high glucose-ROS signaling pathway required for the induction of mitochondrial and total cellular hydrogen peroxide production through the NADPH oxidase isoform (Nox4) in mesangial cells (Shah et al 2013) and thus may represent a potential target to combat diabetic nephropathy. Moreover, in patients with newly diagnosed type 2 diabetes increased MG plasma levels due to high cellular glucose metabolism have been reported (Kong et al 2014) linking increased MG levels and its metabolism by glyoxalase 1 (Glo1) to clinical microvascular complications like nephropathy, retinopathy, and neuropathy (Rabbani and Thornalley 2014). Excess glucose is metabolized through the polyol pathway that converts glucose into sorbitol, which then depletes a large amount of antioxidants like glutathione (GSH) and increases the level of oxidative stress (Chung et al 2003). Subsequently, Glo1 activity is decreased thereby preventing detoxification of glyoxal and methylglyoxal hence increasing the associated glycation reactions (Thornalley 2008). There is also strong and consistent evidence that progression from prediabetes to T2D can be delayed by obesity management (American Diabetes Association 2016). Obesity can be regarded as a state of mild inflammation correlated with increased oxidative stress. Pro-oxidative conditions such as these also lead to the production of reactive aldehydes, such as 4-HNE and 4-ONE (Ruskovska and Bernlohr 2013). These reactive aldehydes are implicated in the development of insulin-resistant obesity and a variety of other metabolic diseases (Grimsrud et al 2007), such as rheumatoid, neurodegenerative or gastrointestinal diseases as well as atherosclerosis (Castro et al 2017). Using proteomics technologies, protein modification by 4-HNE as a consequence of obesity, and its potential relationship to the development of insulin resistance, were investigated with lean insulin-sensitive and obese insulin-resistant C57Bl/6 J mice (Grimsrud et al 2007). High carbohydrate, high fat feeding of mice resulted in a 2–3-fold increase in total adipose tissue protein carbonylation. Consistent with an increase in oxidative stress in obesity, the abundance of glutathione S-transferase A4 (GSTA4), a key enzyme responsible for metabolizing 4-HNE, decreased 3–4-fold in the adipose tissue of the obese mice (Grimsrud et al 2007). Moreover, loss of adipose tissue GSTA4 in GST A4-knockout mice led to increased protein carbonylation, ROS production and mitochondrial dysfunction, and contributed to the development of insulin resistance and T2D (Curtis et al 2010). In line with these results, reactive glucose metabolites have been shown to upregulate carnosinase-1 (CN1) activity by carbonylation. CN1 contributes to diabetic nephropathy by cleaving, e.g., inactivating histidine dipeptides, which scavenge reactive oxygen and carbonyl species and increase nitric oxide bioavailability (Peters et al 2015). Carnosine, the substrate of CN1, is considered nephroprotective and could possibly be used to treat diabetic nephropathy as it restored the glomerular ultrastructure in BTBR (Black and Tan, BRachyuric) ob/ob mice, a T2D diabetes model phenotypically resembling advanced diabetic nephropathy in humans (Albrecht et al 2017).
In addition, specific carbonylated proteins involved in cellular stress responses, lipotoxicity, and insulin signaling were analyzed in adipose tissue using mass spectrometry methods (Grimsrud et al 2007). In particular, redox enzymes such as GST M1, glutathione peroxidase 1 (GPx1), and peroxiredoxin (PRDX) 1 were identified, providing a mechanistic link between increased oxidative stress and the development of insulin resistance.
Recently, it has been proposed that GST activity may play a role in diabetic nephropathy since it is highly active in patients with nephropathy as compared to healthy individuals (Sharma et al 2016). The GST isoform responsible for this finding has to be determined, but there is evidence for the existence of multiple GST isoforms that possess both transferase and selenium-independent peroxidase activity (Singhal et al 2015). Nonetheless, further studies are necessary to validate the introduction of GST as an accurate marker of early diabetic nephropathy (Tesauro et al 2015).
GPX1, the most abundant selenoprotein, is one of the major antioxidant enzymes targeting oxidative stress. Strikingly, overexpression of GPX1 in mice induces a T2D-like phenotype and obesity, whereas knockout of Gpx1 leads to metabolic disorders similar to T1D (Lei and Vatamaniuk 2016). Moreover, it has been reported that carbonylation renders GPx1 enzymatically inactive, which might play a role in the activation of transcription factors like NF-κB and subsequent cellular stress responses contributing to insulin resistance (Ruskovska and Bernlohr 2013).
Peroxiredoxins (PRDXs) represent a ubiquitous family of antioxidant cysteine-dependent peroxidases that play dominant roles in regulating peroxide levels and are suitable markers of oxidative stress (Poynton and Hampton 2014). Plasma PRDX1, PRDX2, PRDX4, and PRDX6 levels are reported to be higher in diabetic patients than in healthy control subjects (El Eter and Al-Masri 2015). Moreover, the population-based Prevention of Renal and Vascular Endstage Disease (PREVEND) cohort study demonstrated that elevated circulating PRDX4 levels are associated with an increased risk of T2D, even after adjusting for common risk factors of diabetes (Abbasi et al 2014). Finally, it has been demonstrated that PRDX6 is a key mediator of hyperglycaemia in T2D-associated glucose metabolism (Pacifici et al 2014). PRDX6 knockout mice develop a phenotype similar to early-stage T2D caused by both reduced glucose-dependent insulin secretion and increased insulin resistance, leading to a reduction in muscle glucose uptake (Pacifici et al 2014). Interestingly, PRDX6 itself was found to be carbonylated in human pulmonary artery smooth muscle cells in response to short-time treatment with cell proliferation-inducing platelet-derived growth factor (Wong et al 2013) or endothelin-1 (ET-1) (Wong et al 2008). In the latter case, ET-1 induced in parallel a fast and efficient decarbonylation of PRDX6 through activation of the thioredoxin pathway (Wong et al 2013), whereas other proteins such as annexin A1 remained carbonylated and were subject to rapid proteasomal degradation. So far, the exact ET-1-driven mechanism of carbonylation and decarbonylation it is not known. However, the finding that siRNA knockdown of glutaredoxin, which catalyzes the reversible reduction of glutathione-protein mixed disulfides, inhibits decarbonylation of peroxiredoxin, strengthens the concept that thiol-dependent decarbonylation defines the kinetics of protein carbonylation-dependent signaling (Wong et al 2013).
Relevance of protein carbonylation in other diseases
As free radical formation is a hallmark of mitochondrial dysfunction, oxidative stress has also been demonstrated to be an underlying pathophysiologic process in various inborn errors of metabolism (Ristoff and Larsson 2002; Mc Guire et al 2009).
3-hydroxy-3-methylglutaric aciduria (HMGA) is a rare autosomal recessive disorder, caused by the deficiency of 3-hydroxy-3-methylglutaryl-CoA lyase, which results in accumulation of 3-hydroxy-3-methylglutaric (HMG) and 3-methylglutaric (MGA) acids in tissues and biological fluids of affected individuals. HMG and MGA are known to decrease cellular levels of reduced glutathione, the activities of superoxide dismutase and glutathione reductase but to increase glutathione peroxidase and catalase activities (Fernandes et al 2013). In addition, HMG also provoked an inhibition of glucose-6-phosphate dehydrogenase activity (Fernandes et al 2013) which plays an essential role in the control of oxidative stress by primarily regulating the main intracellular reductant, NADPH, leading to increased ROS levels and oxidative DNA damage in the cell (Stanton 2012). The disturbed cellular redox homeostasis may contribute to neurological manifestations observed in these patients (Dos Santos Mello et al 2015). Oxidative protein damage remained high even in HMGA patients under treatment with a low-protein diet and L-carnitine supplementation for antioxidant capacity correction, as demonstrated by increased formation of protein carbonyls and di-tyrosine concentrations in the urine (Dos Santos Mello et al 2015). In line with this, it has been proposed recently that quantification of carbonylated proteins in human cerebrospinal fluid might serve as a biomarker of oxidative injury within the central nervous system (Irani 2017). As carbonylation mechanisms are known to affect protein conformation, activity and function, one can speculate that oxidative stress-induced protein carbonylation of the mentioned redox enzymes may also play a role in the development of HMGA.
Oxidative stress might also play, at least in part, an important role in the pathogenesis of homocystinuria, another inherited disorder biochemically characterized by a cystathionine-β-synthase (CBS) deficiency, high urinary excretion of homocystine (Hcy), and increased levels of Hcy and methionine in biological fluids (Vanzin et al 2011). In CBS-deficient patients, a significant positive correlation between interleukin-6 levels and plasma carbonyl group content has been proven, indicating a possible association between inflammation and oxidative protein damage (Vanzin et al 2015). Human CBS has a heme cofactor with cysteine and histidine as ligands (Carballal et al 2013). Interestingly, cell culture and tissue studies suggest that in the presence of carbon monoxide (CO) a reductive carbonylation of CBS must occur in vivo, since an increase in CO concentration was found to inhibit CBS enzymatic activity (Carballal et al 2013). CO binds to ferrous CBS by displacing the axial cysteine ligand giving rise to formation of Fe(II)CO-CBS. Modifications on activation loop residues such as cysteine or histidine by reactive aldehydes are also able to regulate cellular signaling attributed to pro-inflammatory processes and apoptosis (Grimsrud et al 2008).
Epidemiological studies provided evidence that the risk of cardiovascular diseases like atherosclerosis is increased in patients with diabetes and related to the extent of glycaemic control without providing insight into causality (Chait and Bornfeldt 2009). Mechanisms for vascular disease in diabetes include the pathologic effects of AGE accumulation, impaired vasodilatory response attributable to nitric oxide inhibition, smooth muscle cell dysfunction, overproduction of endothelial growth factors, chronic inflammation, hemodynamic dysregulation, impaired fibrinolytic ability, and enhanced platelet aggregation (Cade 2008).
Monocytes are the primary pro-inflammatory cell type that infiltrate early atherosclerotic lesions (Randolph 2009). Interestingly, monocytes derived from T2D patients produce increased levels of ROS and show an increased ability to carbonylate and attach to laminin in an alpha2 integrin subunit (CD49b)-dependent manner (Kostidou et al 2007). In addition, endothelial cells also attach to oxidized laminin at a higher degree in a CD49b-dependent manner and the interaction results in an increased adhesion molecule expression (intercellular adhesion molecule 1, ICAM-1) and consequently increased monocyte recruitment capacity (Kostidou et al 2009). Incubation of endothelial cells with low doses of carbonylated albumin also caused a significant increase in ICAM-1 and vascular cell adhesion molecule-1 (VCAM-1) abundance (Pavone et al 2011). Thus, carbonylated albumin displayed biological effects that may be relevant to uremic atherosclerosis (Pavone et al 2011).
In patients with T2D and cardiovascular disease, the expression of tissue inhibitor of metalloproteinase 3 (TIMP3) is reduced in carotid atherosclerotic plaques, particularly in regions enriched with monocyte/macrophage-like cells (Cardellini et al 2009). TIMP3 overexpression in macrophages isolated from transgenic mice (MacT3) resulted in reduced oxidative stress signals, as evidenced by lower lipid peroxidation, protein carbonylation, and nitration in atheromas (Casagrande et al 2012) thus providing another link between diabetes, oxidative carbonylation in vascular cells, and atherosclerosis.
Diabetes is not only associated with the development of macrovascular diseases like coronary artery disease and atherosclerotic plaque formation, it also induces changes in the microvasculature, causing extracellular matrix protein synthesis and capillary basement membrane thickening, which are the pathognomic features of diabetic microangiopathy (Chawla et al 2016). Diabetic retinopathy may be the most common microvascular complication of diabetes and has a complex pathogenesis characterized by a plethora of tissue-specific alterations occurring in response to the diabetic milieu (Chen et al 2013). Although there are many reports about the importance of advanced glycation end product accumulation during the initiation and progression of retinal damage in diabetic patients (Chen et al 2013), there are few reports describing a relationship between oxidative stress, membrane protein carbonyls, and the clinical severity of diabetic retinopathy, such as that described for the increased protein carbonylation of red blood cell membrane in T2D patients (Margetis et al 2009). This finding was confirmed recently by Loukovaara et al (2014), who found that protein carbonyl and transcription factor hypoxia inducible factor (HIF)-1α levels were significantly increased in the vitreous fluid of surgically treated eyes of patients with diabetic retinopathy.
Role of protein carbonylation in cell signaling
Regulatory mechanisms in signal transduction require that amino acid side chains can be modified or removed by enzymes that specifically target them, presumably changing protein function. Wong and co-workers proposed that primary direct protein carbonylation, in the past considered to be irreversible, mediates cell signaling, and that this modification is reversible (Wong et al 2012). Transient protein carbonylation kinetics spanning 30 min, as observed in ET-1-stimulated smooth muscle cells, are typical for other signal transduction processes such as protein phosphorylation/dephosphorylation (Wong et al 2008). Cysteine and glutathione were found to be efficient substrates for decarbonylation (Wong et al 2013). Moreover, thiols decreased the protein carbonyl content, as detected by 2,4-dinitrophenylhydrazine, but not the levels of malondialdehyde or 4-hydroxynonenal protein adducts. Thus, the decarbonylation process may involve the reduction of primary protein carbonyls, in which carbonyls are formed through direct oxidation of amino acid side chains (Wong et al 2013).
Indeed there is published evidence that thioredoxins might play a role in such a mechanism of protein decarbonylation (Cattaruzza and Hecker 2008). Thioredoxins act as antioxidants by facilitating the reduction of other proteins by cysteine thiol-disulfide exchange. These enzymes are found in nearly all known organisms and are absolutely vital in mammals (Lu and Holmgren 2014). Thus, decarbonylation may occur with the aid of two thiol-dependent enzymes, thioredoxin reductase and glutaredoxin. This assumption was confirmed by the fact that blockage of thioredoxin reductase promotes protein carbonylation and that siRNA-mediated knockdown of glutaredoxin inhibits peroxiredoxin decarbonylation (Wong et al 2013).
Besides post-translational modifications and subsequent changes in protein conformation, protein carbonylation may also result in the activation of transcription factors inducing up- or down-regulation of gene expression (Grimsrud et al 2008). One well-documented example is Kelch-like ECH-associated protein 1 (KEAP1), which acts as a substrate adapter protein for an E3 ubiquitin ligase complex targeting the transcription factor NFE2L2/Nrf2 for ubiquitination and degradation (Curtis et al 2012). KEAP1 modification by 4-HNE at critical cysteine residues leads to its degradation, thereby releasing Nrf2, a master transcription factor regulator of the antioxidant response. Activated Nrf2 heterodimerizes with other factors and activates the transcription of a variety of antioxidant gene targets (Curtis et al 2012). NADPH quinone oxidoreductase, glutathione S-transferase, HO-1, and γ-glutamylcysteine synthetase are particularly well-studied targets of Nrf2 that are upregulated through the antioxidant response element found in the promoters of these genes. Therefore, it is not surprising that attention has focused on identifying small molecule activators of the Nrf2/KEAP1 pathway, as inflammation and oxidative stress are known to be enhanced by the diabetic milieu (de Haan 2011). On the other hand, the recent discovery of KEAP1 somatic mutations in cancer cell lines and human cancer samples suggests that the aberrant activation of Nrf2 signaling may be detrimental (Sykiotis and Bohmann 2008). Many tumors are characterized by high-level expression of Nrf2-dependent genes (HO-1, GST, membrane transport proteins, etc.) and enhanced levels of glutathione (Turpaev 2013). The high level of expression of protective genes in tumors is associated with hypoxia and enhanced ROS production (Turpaev 2013). In line with these findings, general GPx-1 overexpression leads to insulin resistance, hyperglycaemia, and obesity (McClung et al 2004), which might be due to the fact that insulin signaling is influenced by ROS and thus insulin sensitizing is diminished by excess antioxidant capacity (McClung et al 2004). Another example is the c-Jun N-terminal kinase (JNK) upstream kinase ASK1, which is activated by 4-HNE. This modification stimulates the ASK1-stress signaling kinase (SEK1)-JNK pathway, linking oxidative stress to inflammation (Grimsrud et al 2008). Activation/phosphorylation of JNK by SEK1 leads to phosphorylation of IκBα, translocation to the nucleus/activation of the transcription factor NF-κB, and ultimately induction of pro-inflammatory target gene expression (Curtis et al 2012).
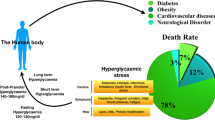
Finally, oxidative protein carbonylation presumably has a biphasic effect as demonstrated for the carbonylation of renal proximal tubule Na/K-ATPase α1 subunit. Physiological low α1 subunit carbonylation stimulates Na/K-ATPase signaling and sodium excretion, conferring salt resistance (Shah et al 2016). In contrast, prolonged exposure to enhanced oxidant stress leads to an increase in α1 subunit carbonylation and desensitized Na/K-ATPase signaling, resulting in salt sensitivity. It appears that a redox status balanced within a physiological range may be critical to maintain beneficial ROS signaling or carbonylation. Due to the distinct carbonylation of amino acid residues, a partial local structural rearrangement is likely to occur, thus leading to solvent exposure of further possible, previously buried, carbonylatable sites. The subsequently induced conformational changes may lead to a loss of function or enzymatic activity of a highly carbonylated protein. It may therefore be concluded that physiological oxidative carbonylation, possibly regulated by decarbonylation, can lead to dynamic activation of protein function. In contrast, any abnormal increase in oxidative stress may promote protein inactivation followed by proteasomal degradation or aggregate formation and accumulation, after modification has reached a critical level (cf. Fig. 2). The balance between protective and detrimental effects of protein carbonylation has to be determined, but is presumably difficult to define. This threshold may be dependent on the overall intracellular redox status, the intracellular localization of the protein and its individual amino acid sequence-dependent susceptibility to carbonylation.
Balance of the redox status within a physiological range may be critical in maintaining beneficial ROS signaling or carbonylation. Reactive intermediates such as methylglyoxal (MG) or ROS (hydroxyl radical, •OH) formed by glucose metabolism mediate site-specific post-translational modifications of transcription factors (TF) or functional proteins. Normal blood glucose or mild oxidative stress is likely to be cell-protective due to cellular and signaling responses associated with increased TF-initiated redox enzyme expression or elevated activity of antioxidant defense mechanisms. In contrast, severe oxidative stress as a result of hyperglycaemia may lead to cell damage because of excessive protein carbonylation leading to proteasomal degradation that if exceeded causes accumulation and aggregation of the carbonylated proteins. The possible regulatory role of the decarbonylation process in cell signaling at physiological conditions is indicated by dotted arrows
Current diagnostic and antioxidant therapeutic options in diabetes
Screening for T2D in high-risk patients and subsequent lowering of high blood glucose levels were not associated with a reduction in all-cause, cardiovascular or diabetes-related 10-year mortality (Simmons et al 2012). Other clinical studies clearly demonstrated that the long-used diagnostic markers blood glucose and glycated hemoglobin (HbA1c) are insufficient to predict the development of diabetic complications (van ‘t Riet et al 2010). As an alternative, glyoxalate (Nikiforova et al 2014) or post-translational protein modifications by MG derived from glucose metabolism could be a better diagnostic marker to predict the development of diabetic complications (Gajjala et al 2015). As discussed herein, increased post-translational protein modifications can lead to conformational changes associated with an altered protein function or activation of signaling cascades, which may result in a functional impairment of an entire organ. Therefore, the balance between formation and detoxification of glucose-derived reactive metabolites and the related post-translational modifications may provide a new concept for understanding how diabetic complications can develop independently of an abnormally high glucose level. In line with this, metformin has recently been shown to reduce plasma MG levels in patients with T2D not due to its scavenging properties, but because it restores activity of glyoxalase-1, the glutathione-dependent enzyme for MG detoxification (Kender et al 2014).
High blood glucose levels can initiate the formation of superoxide anions and hydrogen peroxide, which are able to stimulate the decline of antioxidant systems, directly damage biomolecules, and increase lipid peroxidation in diabetes. Since ROS production and lipid peroxidation are increased in patients with diabetes, several attempts have been made to pharmaceutically target the cellular redox balance. So far, pharmacologically reinforcing antioxidant defense mechanisms hardly produced any beneficial effects, in fact it sometimes even deteriorated diabetes and its sequelae (Hasanain and Mooradian 2002). Some experimental studies suggest that natural antioxidants, such as α-tocopherol (vitamin E), ascorbate (vitamin C), coenzyme Q (CoQ) or α-lipoic acid, attenuate diabetic complications. However, results from large, long-term clinical trials using vitamin E supplementation were disappointing (Nishikawa and Araki 2013). Therefore, the efficacy of antioxidant-based therapies in preventing diabetic complications in clinical practice is still uncertain. Given the paramount importance of the cellular redox system, one could speculate that any interference with its sensitive balance and conditionally dependent signaling pathways could be one reason for this disappointing outcome.
Nevertheless, recent findings obtained from patients with inherited neurometabolic diseases like HMGA (cf. Relevance of protein carbonylation in other diseases) demonstrated that L-carnitin supplementation may be a useful treatment strategy for this disorder. L-carnitine was shown to be involved in the reduction of oxidative damage observed in these disorders (Ribas et al 2014); besides its important role in lipid metabolism, L-carnitine is also a potent free radical scavenger and antioxidant. Considering the ability of L-carnitine to easily cross the blood–brain barrier, supplementation may thus be beneficial in preventing neurological damage derived from oxidative injury (Ribas et al 2014).
Conclusion
Carbonyl groups represent the most common type of non-enzymatic post-translational modification introduced into proteins by an oxidative (direct) or non-oxidative (indirect) mechanism. Whereas a high degree of protein carbonylation is a sign of severe oxidative damage and disease-derived protein dysfunction, moderate carbonylation may directly activate or inhibit the activities of target proteins as well as their selective proteasomal degradation. Further research is needed to assess the described decarbonylation process of primary protein carbonyls which offers the opportunity of dynamic regulation of protein conformation, activity and function. An altered redox balance may play a crucial role in the pathogenesis of oxidative stress-related diseases like diabetes mellitus.
Abbreviations
- 4-HNE:
-
4-hydroxy trans-2,3-nonenal
- 4-ONE:
-
4-oxo trans-2,3-nonenal
- ASK1:
-
apoptosis signal-regulating kinase 1
- ET-1:
-
endothelin-1
- Glc:
-
glucose
- GPx1:
-
glutathione peroxidase 1
- GST:
-
glutathione S-transferase
- HO-1:
-
heme oxygenase-1
- IκBα:
-
NF-κB inhibitor, alpha
- MG:
-
methylglyoxal
- NADPH:
-
nicotinamide adenine dinucleotide phosphate
- NF-κB:
-
nuclear factor ‘kappa-light-chain-enhancer’ of activated B-cells
- NFE2L2:
-
Nuclear factor erythroid-derived 2-like 2 (also referred to as Nrf2)
- Nrf2:
-
nuclear factor-erythroid 2-related factor 2
- PRDX:
-
peroxiredoxin
- PTM:
-
post-translational modification
- RCS:
-
reactive carbonyl species
- ROS:
-
reactive oxygen species
- T1D:
-
type 1 diabetes mellitus
- T2D:
-
type 2 diabetes mellitus
References
Abbasi A, Corpeleijn E, Gansevoort RT et al (2014) Circulating peroxiredoxin 4 and type 2 diabetes risk: the prevention of renal and vascular endstage disease (PREVEND) study. Diabetologia 57:1842–1849
Adams S, Green P, Claxton R et al (2001) Reactive carbonyl formation by oxidative and non-oxidative pathways. Front Biosci 6:A17–A24
Aiken CT, Kaake RM, Wang X, Huang L (2011) Oxidative stress-mediated regulation of proteasome complexes. Mol Cell Proteomics 10:R110 006924
Al-Khalili L, de Castro Barbosa T, Ostling J et al (2014) Proteasome inhibition in skeletal muscle cells unmasks metabolic derangements in type 2 diabetes. Am J Physiol Cell Physiol 307: C774-C787
Albrecht T, Schilperoort M, Zhang S et al (2017) Carnosine attenuates the development of both type 2 diabetes and diabetic nephropathy in BTBR ob/ob mice. Sci Rep 7:44492
American Diabetes Association (2016) 6. Obesity management for the treatment of type 2 diabetes. Diabetes Care 39(Suppl 1):S47–S51
Bollineni RC, Fedorova M, Bluher M, Hoffmann R (2014) Carbonylated plasma proteins as potential biomarkers of obesity induced type 2 diabetes mellitus. J Proteome Res 13:5081–5093
Bugger H, Abel ED (2008) Molecular mechanisms for myocardial mitochondrial dysfunction in the metabolic syndrome. Clin Sci (Lond) 114:195–210
Bugger H, Abel ED (2014) Molecular mechanisms of diabetic cardiomyopathy. Diabetologia 57:660–671
Cade WT (2008) Diabetes-related microvascular and macrovascular diseases in the physical therapy setting. Phys Ther 88:1322–1335
Carballal S, Cuevasanta E, Marmisolle I et al (2013) Kinetics of reversible reductive carbonylation of heme in human cystathionine beta-synthase. Biochemistry 52:4553–4562
Cardellini M, Menghini R, Martelli E et al (2009) TIMP3 is reduced in atherosclerotic plaques from subjects with type 2 diabetes and increased by SirT1. Diabetes 58:2396–2401
Casagrande V, Menghini R, Menini S et al (2012) Overexpression of tissue inhibitor of metalloproteinase 3 in macrophages reduces atherosclerosis in low-density lipoprotein receptor knockout mice. Arterioscler Thromb Vasc Biol 32:74–81
Castro JP, Jung T, Grune T, Siems W (2017) 4-Hydroxynonenal (HNE) modified proteins in metabolic diseases. Free Radic Biol Med 111:309–315
Cattaruzza M, Hecker M (2008) Protein carbonylation and decarboylation: a new twist to the complex response of vascular cells to oxidative stress. Circ Res 102:273–274
Chait A, Bornfeldt KE (2009) Diabetes and atherosclerosis: is there a role for hyperglycemia? J Lipid Res 50(Suppl):S335–S339
Chawla A, Chawla R, Jaggi S (2016) Microvasular and macrovascular complications in diabetes mellitus: distinct or continuum? Indian J Endocrinol Metab 20:546–551
Chen M, Curtis TM, Stitt AW (2013) Advanced glycation end products and diabetic retinopathy. Curr Med Chem 20:3234–3240
Chung SS, Ho EC, Lam KS, Chung SK (2003) Contribution of polyol pathway to diabetes-induced oxidative stress. J Am Soc Nephrol 14:S233–S236
Curtis JM, Grimsrud PA, Wright WS et al (2010) Downregulation of adipose glutathione S-transferase A4 leads to increased protein carbonylation, oxidative stress, and mitochondrial dysfunction. Diabetes 59:1132–1142
Curtis JM, Hahn WS, Long EK, Burrill JS, Arriaga EA, Bernlohr DA (2012) Protein carbonylation and metabolic control systems. Trends Endocrinol Metab 23:399–406
de Haan JB (2011) Nrf2 activators as attractive therapeutics for diabetic nephropathy. Diabetes 60:2683–2684
Diaz-Villanueva JF, Diaz-Molina R, Garcia-Gonzalez V (2015) Protein folding and mechanisms of proteostasis. Int J Mol Sci 16:17193–17230
Dos Santos Mello M, Ribas GS, Wayhs CA et al (2015) Increased oxidative stress in patients with 3-hydroxy-3-methylglutaric aciduria. Mol Cell Biochem 402:149–155
El Eter E, Al-Masri AA (2015) Peroxiredoxin isoforms are associated with cardiovascular risk factors in type 2 diabetes mellitus. Braz J Med Biol Res 48:465–469
Fedorova M, Bollineni RC, Hoffmann R (2014) Protein carbonylation as a major hallmark of oxidative damage: update of analytical strategies. Mass Spectrom Rev 33:79–97
Fernandes CG, da Rosa MS, Seminotti B et al (2013) In vivo experimental evidence that the major metabolites accumulating in 3-hydroxy-3-methylglutaryl-CoA lyase deficiency induce oxidative stress in striatum of developing rats: a potential pathophysiological mechanism of striatal damage in this disorder. Mol Genet Metab 109: 144-153
Fisher AB (2009) Redox signaling across cell membranes. Antioxid Redox Signal 11:1349–1356
Frohnert BI, Bernlohr DA (2013) Protein carbonylation, mitochondrial dysfunction, and insulin resistance. Adv Nutr 4:157–163
Gajjala PR, Fliser D, Speer T, Jankowski V, Jankowski J (2015) Emerging role of post-translational modifications in chronic kidney disease and cardiovascular disease. Nephrol Dial Transplant 30:1814–1824
Giacco F, Brownlee M (2010) Oxidative stress and diabetic complications. Circ Res 107:1058–1070
Grimsrud PA, Picklo MJ Sr, Griffin TJ, Bernlohr DA (2007) Carbonylation of adipose proteins in obesity and insulin resistance: identification of adipocyte fatty acid-binding protein as a cellular target of 4-hydroxynonenal. Mol Cell Proteomics 6:624–637
Grimsrud PA, Xie H, Griffin TJ, Bernlohr DA (2008) Oxidative stress and covalent modification of protein with bioactive aldehydes. J Biol Chem 283:21837–21841
Hasanain B, Mooradian AD (2002) Antioxidant vitamins and their influence in diabetes mellitus. Curr Diab Rep 2:448–456
Higdon A, Diers AR, Oh JY, Landar A, Darley-Usmar VM (2012) Cell signalling by reactive lipid species: new concepts and molecular mechanisms. Biochem J 442:453–464
Irani DN (2017) Cerebrospinal fluid protein carbonylation identifies oxidative damage in autoimmune demyelination. Ann Clin Transl Neurol 4:145–150
Jung T, Grune T (2008) The proteasome and its role in the degradation of oxidized proteins. IUBMB Life 60:743–752
Kender Z, Fleming T, Kopf S et al (2014) Effect of metformin on methylglyoxal metabolism in patients with type 2 diabetes. Exp Clin Endocrinol Diabetes 122:316–319
Kong X, Ma MZ, Huang K et al (2014) Increased plasma levels of the methylglyoxal in patients with newly diagnosed type 2 diabetes 2. J Diabetes 6:535–540
Konig A, Bode C, Bugger H (2012) Diabetes mellitus and myocardial mitochondrial dysfunction: bench to bedside. Heart Fail Clin 8:551–561
Konstantopoulos N, Foletta VC, Segal DH et al (2011) A gene expression signature for insulin resistance. Physiol Genomics 43:110–120
Kostidou E, Koliakos G, Alamdari DH, Paletas K, Tsapas A, Kaloyianni M (2007) Enhanced laminin carbonylation by monocytes in diabetes mellitus. Clin Biochem 40:671–679
Kostidou E, Topouridou K, Daniilidis A, Kaloyianni M, Koliakos G (2009) Oxidized laminin-1 induces increased monocyte attachment and expression of ICAM-1 in endothelial cells. Int J Exp Pathol 90:630–637
Lee I, Suzuki CK (2008) Functional mechanics of the ATP-dependent Lon protease- lessons from endogenous protein and synthetic peptide substrates. Biochim Biophys Acta 1784:727–735
Lei XG, Vatamaniuk M (2016) Glutathione Peroxidase 1: models for diabetes and obesity. In Hatfield DL, Schweizer U, Tsuji PA, Gladyshev VN eds. Selenium: Its Molecular Biology and Role in Human Health. Cham: Springer, pp 587-594
Loukovaara S, Koivunen P, Ingles M, Escobar J, Vento M, Andersson S (2014) Elevated protein carbonyl and HIF-1alpha levels in eyes with proliferative diabetic retinopathy. Acta Ophthalmol 92:323–327
Lu J, Holmgren A (2014) The thioredoxin antioxidant system. Free Radic Biol Med 66:75–87
Maessen DE, Stehouwer CD, Schalkwijk CG (2015) The role of methylglyoxal and the glyoxalase system in diabetes and other age-related diseases. Clin Sci (Lond) 128:839–861
Maisonneuve E, Ducret A, Khoueiry P et al (2009) Rules governing selective protein carbonylation. PLoS One 4:e7269
Margetis PI, Antonelou MH, Petropoulos IK, Margaritis LH, Papassideri IS (2009) Increased protein carbonylation of red blood cell membrane in diabetic retinopathy. Exp Mol Pathol 87:76–82
Mc Guire PJ, Parikh A, Diaz GA (2009) Profiling of oxidative stress in patients with inborn errors of metabolism. Mol Genet Metab 98:173–180
McClung JP, Roneker CA, Mu W et al (2004) Development of insulin resistance and obesity in mice overexpressing cellular glutathione peroxidase. Proc Natl Acad Sci U S A 101:8852–8857
Nikiforova VJ, Giesbertz P, Wiemer J et al (2014) Glyoxylate, a new marker metabolite of type 2 diabetes. J Diabetes Res 2014:685204
Nishikawa T, Araki E (2013) Mechanism-based antioxidant therapies promise to prevent diabetic complications? J Diabetes Investig 4:105–107
Nystrom T (2005) Role of oxidative carbonylation in protein quality control and senescence. EMBO J 24:1311–1317
Oya T, Hattori N, Mizuno Y et al (1999) Methylglyoxal modification of protein. Chemical and immunochemical characterization of methylglyoxal-arginine adducts. J Biol Chem 274:18492–18502
Pacifici F, Arriga R, Sorice GP et al (2014) Peroxiredoxin 6, a novel player in the pathogenesis of diabetes. Diabetes 63:3210–3220
Pavone B, Sirolli V, Giardinelli A et al (2011) Plasma protein carbonylation in chronic uremia. J Nephrol 24:453–464
Peters V, Lanthaler B, Amberger A et al (2015) Carnosine metabolism in diabetes is altered by reactive metabolites. Amino Acids 47:2367–2376
Poynton RA, Hampton MB (2014) Peroxiredoxins as biomarkers of oxidative stress. Biochim Biophys Acta 1840:906–912
Queisser MA, Yao D, Geisler S et al (2010) Hyperglycemia impairs proteasome function by methylglyoxal. Diabetes 59:670–678
Rabbani N, Thornalley PJ (2014) The critical role of methylglyoxal and glyoxalase 1 in diabetic nephropathy. Diabetes 63:50–52
Randolph GJ (2009) The fate of monocytes in atherosclerosis. J Thromb Haemost 7(Suppl 1):28–30
Ribas GS, Vargas CR, Wajner M (2014) L-carnitine supplementation as a potential antioxidant therapy for inherited neurometabolic disorders. Gene 533:469–476
Ristoff E, Larsson A (2002) Oxidative stress in inborn errors of metabolism: lessons from glutathione deficiency. J Inherit Metab Dis 25:223–226
Ruskovska T, Bernlohr DA (2013) Oxidative stress and protein carbonylation in adipose tissue—implications for insulin resistance and diabetes mellitus. J Proteome 92:323–334
Shah A, Xia L, Goldberg H, Lee KW, Quaggin SE, Fantus IG (2013) Thioredoxin-interacting protein mediates high glucose-induced reactive oxygen species generation by mitochondria and the NADPH oxidase, Nox4, in mesangial cells. J Biol Chem 288:6835–6848
Shah PT, Martin R, Yan Y, Shapiro JI, Liu J (2016) Carbonylation modification regulates Na/K-ATPase Signaling and salt sensitivity: a review and a hypothesis. Front Physiol 7:256
Sharma M, Gupta S, Singh K et al (2016) Association of glutathione-S-transferase with patients of type 2 diabetes mellitus with and without nephropathy. Diabetes Metab Syndr 10:194–197
Simmons RK, Echouffo-Tcheugui JB, Sharp SJ et al (2012) Screening for type 2 diabetes and population mortality over 10 years (ADDITION-Cambridge): a cluster-randomised controlled trial. Lancet 380:1741–1748
Singhal SS, Singh SP, Singhal P, Horne D, Singhal J, Awasthi S (2015) Antioxidant role of glutathione S-transferases: 4-Hydroxynonenal, a key molecule in stress-mediated signaling. Toxicol Appl Pharmacol 289:361–370
Stanton RC (2012) Glucose-6-phosphate dehydrogenase, NADPH, and cell survival. IUBMB Life 64:362–369
Suravajjala S, Cohenford M, Frost LR, Pampati PK, Dain JA (2013) Glycation of human erythrocyte glutathione peroxidase: effect on the physical and kinetic properties. Clin Chim Acta 421:170–176
Sykiotis GP, Bohmann D (2008) Keap1/Nrf2 signaling regulates oxidative stress tolerance and lifespan in drosophila. Dev Cell 14:76–85
Tesauro M, Nistico S, Noce A et al (2015) The possible role of glutathione-S-transferase activity in diabetic nephropathy. Int J Immunopathol Pharmacol 28:129–133
Thornalley PJ (2008) Protein and nucleotide damage by glyoxal and methylglyoxal in physiological systems—role in ageing and disease. Drug Metabol Drug Interact 23:125–150
Turpaev KT (2013) Keap1-Nrf2 signaling pathway: mechanisms of regulation and role in protection of cells against toxicity caused by xenobiotics and electrophiles. Biochemistry (Mosc) 78:111–126
Van’t Riet E, Alssema M, Rijkelijkhuizen JM, Kostense PJ, Nijpels G, Dekker JM (2010) Relationship between A1C and glucose levels in the general Dutch population: the new Hoorn study. Diabetes Care 33:61–66
Vanzin CS, Biancini GB, Sitta A et al (2011) Experimental evidence of oxidative stress in plasma of homocystinuric patients: a possible role for homocysteine. Mol Genet Metab 104:112–117
Vanzin CS, Mescka CP, Donida B et al (2015) Lipid, oxidative and inflammatory profile and alterations in the enzymes paraoxonase and butyrylcholinesterase in plasma of patients with homocystinuria due CBS deficiency: the vitamin B12 and folic acid importance. Cell Mol Neurobiol 35:899–911
Wong CM, Bansal G, Marcocci L, Suzuki YJ (2012) Proposed role of primary protein carbonylation in cell signaling. Redox Rep 17:90–94
Wong CM, Cheema AK, Zhang L, Suzuki YJ (2008) Protein carbonylation as a novel mechanism in redox signaling. Circ Res 102:310–318
Wong CM, Marcocci L, Das D et al (2013) Mechanism of protein decarbonylation. Free Radic Biol Med 65:1126–1133
Zatalia SR, Sanusi H (2013) The role of antioxidants in the pathophysiology, complications, and management of diabetes mellitus. Acta Med Indones 45:141–147
Acknowledgements
The authors are indebted to Dr. Gerd König for providing Fig. 2 and for critically reading the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. H. Wagner and M. Hecker declare that they have no conflict of interest.
Informed consent
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Additional information
Responsible Editor: Verena Peters
Rights and permissions
About this article
Cite this article
Hecker, M., Wagner, A.H. Role of protein carbonylation in diabetes. J Inherit Metab Dis 41, 29–38 (2018). https://doi.org/10.1007/s10545-017-0104-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-017-0104-9