Abstract
Thin and flexible polymeric membranes play a critical role in tissue engineering applications for example organs-on-a-chip. These flexible membranes can enable mechanical stretch of the engineered tissue to mimic organ-specific biophysical features, such as breathing. In this work, we report the fabrication of thin (<20 μm), stretchable, and biocompatible polyurethane (PU) membranes. The membranes were fabricated using spin coating technique on silicon substrates and were mounted on a frame for ease of device integration and handling. The membranes were characterized for their optical and elastic properties and compatibility with cell/tissue culture. It was possible to apply up to 10 kilopascal (kPa) pressure to perform cyclic stretch on 4 mm-diameter membranes for a period of 2 weeks at 0.2 hertz (Hz) frequency without mechanical failure. Adenocarcinomic human alveolar basal epithelial (A549) cells were cultured on the apical side of the PU membrane. The morphology and viability of the cells were comparable to those of cells cultured on standard tissue culture plates. Our experiments suggest that the stretchable PU membrane will be broadly useful for various tissue engineering applications in vitro.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Over the last decade, tissue engineering constructs have evolved from simple planar culture to meticulously engineered platforms such as the organs-on-a-chip (Bhatia and Ingber 2014). One of the key features that differentiate organs-on-a-chip devices from conventional tissue-engineered systems is the mechanical stretching of the substrates to simulate critical biophysical features of an organ (Leung et al. 1976; Riehl et al. 2012). This mechanical stretching has been demonstrated to enhance the recapitulation of three dimensional (3D) tissues including cardiac, muscle, vasculature, ligament, tendon, bone, and lung (Esch et al. 2015).
Thin and stretchable membranes are utilized to achieve mechanical stretching in various complex tissue engineering platforms including organs-on-a-chip. In addition, the membranes should be amenable to sterilization techniques, biocompatible for cell/tissue culture, gas-permeable to facilitate long term tissue growth, optically transparent to enable high resolution imaging, and easy to handle for device integration. Polydimethylsiloxane (PDMS) meets many of these requirements and is therefore frequently used as a cell culture substrate in organs-on-a-chip systems (Huh et al. 2010). However, PDMS has been shown to be absorbent of small, hydrophobic molecules (Mukhopadhyay 2007; Wang et al. 2012). Such absorption can lead to several limitations for its application in drug development and toxicity analysis. For example, the absorption of drug molecules can reduce the effective drug concentrations and can impact time-dependent changes in target molecules during the course of a study (Regehr et al. 2009). Therefore, this work focuses on identifying alternate substrates suitable for mechanical stretching.
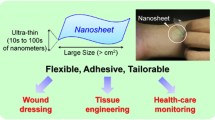
Polyurethane (PU) substrates have been investigated as a substitute for PDMS membranes for use in microfluidics and tissue culture applications (Huh et al. 2010). PU has a number of inherent qualities that are advantageous for cell culture, such as its elasticity, optical transparency, biocompatibility, and partial permeability to gases (Matsunaga et al. 2005; Gu et al. 2014). For these reasons, Ingber et al. developed various microfluidic systems using polyurethane and demonstrated its’ efficacy as a cell culture surface (Domansky et al. 2013). Their work lays the foundation for using PU substrates to fabricate complex 3D tissue engineering platforms. However, systematic development and characterization of ‘thin and flexible’ PU membranes is needed to implement important features such as mechanical and cyclic stretching. There are several commercially available thin, polymeric membranes that are used in medical applications (Zdrahala and Zdrahala 1999), such as wound healing patches (Smiths&Nephew 2016), balloon angioplasty (Mishra and Bahl 2010), and commercially-available culture-plate sealing membranes. However, these membranes are not intended for organs-on-a-chip applications.
In this report, we present the fabrication and characterization of thin and flexible membranes from castable polyurethane polymer suitable for the organs-on-a-chip application. First, we describe the method for fabricating the thin membranes and a handling technique for integrating them into an organs-on-a-chip platform. Second, we characterize the thickness, flexibility, optical properties, and hydrophobic qualities of the membranes. Finally, we demonstrate the ability of the polyurethane membrane-integrated devices to serve as effective cell and tissue culture platforms.
2 Experimental
2.1 Materials
Two-part polyurethane systems were obtained from GS Polymers, Inc. (GSP 1552–2). Silicon wafers were obtained from University Wafer (cat. #452). Adenocarcinomic A549 cells were obtained from ATCC (ATCC, cat. #CCL185). Greiner CELLSTAR Bio-One 24-well culture plates (#662160) were used for cell culture. Additional supplies used include: F-12 K media (ATCC cat. #30–2004); Fetal Bovine serum (FBS) (Thermo Scientific Hyclone, cat. # 10437–028); 0.25% trypsin EDTA (1×) (Gibco, cat. #25200–056); Live/Dead Viability/Cytotoxicity kit for mammalian cells (Molecular Probes, cat. #L3224); Dulbecco’s Phosphate Buffered Saline (DPBS) (Gibco by Life Technologies, cat. #14190–144).
2.2 Fabrication of PU membranes
The two polyurethane components were mixed together at a 1:1 weight ratio using the mixer provided by the company. Approximately 5 g of the polymer mixtures were then poured onto a non-treated 100 mm diameter silicon wafer. Immediately after pouring the polymer, it was spin coated at 500 rpm (rpm) for 60 s, followed by a range from 500 to 6000 rpm for an additional 30 s. The coated silicon wafer was then cured at atmospheric pressure and room temperature overnight, followed by thermal treatment at 80 °C for 4 h. With a sharp knife, the membrane was scored in one cm squares, and the wafer was submerged in water for 24–48 h. After soaking, membranes were ready to be peeled off of the silicon wafer.
2.3 Handling of thin PU membranes
To facilitate release and avoid tearing, tweezers were used carefully to peel the pre-scored membrane (~1 × 1 cm) from the wafer. After removing the membrane from the wafer, we laid the membrane on a flat, glass slide and used microfiber swabs to smooth out any wrinkles. The membranes were then transferred onto a laser-cut polyethylene terephthalate (PET) frame. The PET frames were previously laminated with silicone-based adhesive transfer tape (Nath et al. 2010) on both sides, which serves to bond the membrane to the frame. Once the membrane was transferred onto the frame, a second frame was attached from the opposite side (see supplementary Video 1 (A-D)). Sandwiching the membrane between the adhesive PET frames in this way keeps the membrane flat, taut, and easy to handle for post processing/characterization.
2.4 Membrane characterization
2.4.1 Thickness
After the membranes were integrated into the frame, the membranes became significantly easier to handle for follow-up characterization. The frame and the membranes were then cut using scissors such that the cross-section of the membrane was exposed and its thickness could be measured under a microscope. For more precise thickness characterization, scanning electron microscopy (FEI, Inspect F SEM) was utilized. Imaging was performed with the SEM in secondary electron (SE) mode, at 15 KeV.
2.4.2 Optical characteristics
Gaertner’s L125B single wavelength ellipsometer was used to measure the refractive index. The instrument was calibrated by measuring the refractive index of aluminum. Then, three different samples of PU were measured with the same setting and with a wavelength of 633 nm.
2.4.3 Contact angle measurement
PU membranes were treated with air plasma cleaner for several treatment times and stored in phosphate buffer saline (PBS). To investigate the hydrophilic characteristics the water contact angle of the membrane was measured following the half-angle method utilizing the CAM-PLUS Contact Angle Meter from ChemInstruments (2016).
2.4.4 Characterization of the elastic deformation behavior of the membrane by bulge test
The elastic behavior properties of the thin membrane were determined by a bulge test, described in details by Huang et al. (2007). To perform the bulge test individual membranes were mounted on a test unit using a combination of laser based microfabrication and lamination technique (Nath et al. 2010). The test unit (Fig. 4a) was designed such that a given constant pressure could be applied on the 15 μm thick membrane placed on a 4 mm diameter opening. Each unit was placed in a vertical position (Fig. 4b) so that the bulge can be observed through the microscope (Stereo microscope, AmScope). Constant pressure was applied using the functionality of a pneumatic pump (PneuWave, CorSolutions). The bulge height was observed and captured by image processing software (uEye, IDS Imaging Development Systems GmbH). Each image was analyzed manually to measure the bulge heights (Fig. 4c) against a ruler imaged with the same magnification. The value of the stress (σ), the strain (ε) and the Young’s modulus (Y) of the membrane were determined using the following equations (Wu et al. 2015):
Where R is the radius of circular membrane, P is the applied pressure, t is the thickness of the thin membrane, h is the deformed height at the center of the deflected membrane, ν = Poisson ratio (0.49 was used for calculation (Roussel et al. 2014)), C1 and C2 are constants, where C1 is 4 and C2 is 2.173 for circular opening (Wu et al. 2015). The Young’s modulus (Y) and residual stress (σ 0) was calculated from the experimental result by curve fitting using GNU plot (Kelley 2010).
2.4.5 Absorption of small molecules
To conduct an investigation of the small molecular absorption by PU and PDMS, 6-mm diameter discs mounted on a frame with a 15 μm thickness were fabricated. The membranes were exposed to 200 μL solutions of 1 μM of Rhodamine for one hour. The discs were rinsed up to seven times with PBS and imaged with a Zeiss microscope at 100× magnification with an excitation wavelength of 550 nm.
2.5 Membrane integration into a microfluidic device
Figure 1 (layer model) shows the different layers of the cell culture device. The configurations for each layer were designed using Solid Edge 2D Drafting ST4 software (Siemens PLM Software). The membrane frames and microfluidic channels were all cut with a carbon dioxide laser cutter (M-360, Universal Laser Systems) on PET film (0.25 mm; McMaster-Carr) laminated with adhesive tapes (9122, 3 M Company) on both sides. Our thin PU membranes were fabricated and transferred to PET frames as described in previous sections. This membrane-frame “sandwich” was then integrated into the device.
Schematic representation of different layers of the cell culture device. Parts of Polyethylene Terephthalate (PET) and Acrylic materials were cut with a CO2 laser and stacked on top of each other with the aid of adhesive layers and lamination technique. Fabricated PU was integrated in the device which allows for cell culture and easy access to the membrane using a pipette
2.6 Cell/tissue culture on PU membrane integrated devices
2.6.1 Membrane preparation for cell culture
The PU membranes secured between frames were rinsed using the Branson ultrasonic cleaner for 5 min to remove any dust particles. They were then integrated into devices for cell culture that allowed for easy access to the membrane using a pipette, for applications such as cell seeding and media changing. Prior to cell culture, membrane-integrated devices were sterilized in a solution of 5% hydrogen peroxide diluted in PBS along with UV-sterilization for 30 min. The membranes were then rinsed in sterile PBS and placed into a sterile 100 mm × 25 mm dish. The rinsed membranes were cleaned using the PDC-001-HP Air Plasma Cleaner (high power, maximum RF 30 watt) for two minutes, and submerged under 500 μl of 30 μg/ml rat collagen (Corning collagen I) in PBS at 37 °C for four hours. Any excess collagen was aspirated and the membranes were rinsed once more with sterile PBS.
2.6.2 Cell culture
Human lung adenocarcinoma epithelial cells A549 (ATCC, Manassas, VA) were seeded onto the membranes with a density of 1.6 X 105 in a 400 μl of F-12 K growth medium supplemented with 10% fetal bovine serum (FBS). The cells were added to the top compartment of the device. A549 cells with same density were seeded onto 12-well polystyrene plates and cultured for five days in F-12 k media with 10% FBS as a control. The growth medium for both culture were changed every other day for a period of five days. Cells were observed daily using an EVOS microscope (XL Core).
2.6.3 Cell viability measurements
After 5 days of culture, the membranes were cut from their frames and transferred onto glass slides. The slides were rinsed three times with PBS and incubated for 30 min in 2 μM calcein AM and 4 μM ethidium homodimer-1 using Molecular Probes’ Live/Dead Viability/Cytotoxicity kit. The cells were then imaged using the Carl Zeiss Axio Observer Research Microscope. The excitation wavelength used for calcein was 494 nm and the emission wavelength 514 nm. The excitation wavelength used for ethidium bromide was 350 nm and the emission wavelength was 617 nm. The software ZN 292 (1.1.1.0) Carl Zeiss microscopy GmbH was used to take the images and they were analyzed using ImageJ software (National Institutes of Health).
3 Results and discussion
3.1 Thickness of polyurethane membranes
Membrane thickness is a function of spinning parameters (rpm and spinning time) (Zhao and Marshall 2008). Membranes with various thicknesses were obtained by varying the spinning speed and their thickness was measured (Fig. 2a, b). Figure 2c shows how the thickness of the PU membrane decreases as a function of increasing rpm. Membranes thinner than 15 μm were very delicate and difficult to handle without any damage; as such, we chose to use 15 μm thick membranes for our study, which were fabricated on the spin coater at 3000 rpm.
Fabrication of PU membranes. Immediately after mixing polyurethane components, the mixture was spin coated on silicon (substrate) at different angular speed for 90 s. As the angular velocity increases, the membrane thickness decreases. Membranes were imaged by SEM and thicknesses were measured by ImageJ software. Five measurements for each membranes were taken. (a) And (b) are the SEM images of cross sectional PU fabricated using 500 rpm for 90 s and 6000 rpm for 90 s respectively; (c) Graph showing dependence of PU membrane thicknesses as a function of spin coating speed
3.2 Optical characteristics
Cells and tissues are typically observed through the substrate using high-resolution microscopy during typical culture experiments. Therefore, the substrate’s optical properties, such as its refractive index, are important parameters to consider when choosing a new material for cell and tissue culture applications. Table 1 shows the refractive index of 15 μm thick PU. The refractive index of the PU film was close to that of a glass slide (Corning 2016). Glass is one of the most commonly used material in microscopy because of its excellent optical clarity. The similarity in the refractive index of PU and glass indicate that the PU membrane has a suitable optical clarity for high-resolution microscopy (Daimon and Masumura 2007; Azmayesh-Fard et al. 2013).
3.3 Contact angle measurement
Surface wettability is crucial for typical cell adhesion and growth; it has been shown that cell adhesion drastically improves on hydrophilic surfaces (Dowling et al. 2011). Therefore, it is important to be able to manipulate the surface wettability of a new substrate for cell and tissue culture. We have conducted experiments investigating the change in hydrophobicity of the PU membrane. As shown in Fig. 3a the water contact angle decreases rapidly from 78.66° on untreated PU to 38.4° after the plasma treatment (within minutes). On further evaluation over several days the water contact angle remains low for up to 3 days following which we observe some increase in the hydrophobicity of our membrane (3B). This result is not unexpected since hydrophobic recovery of PU surface has already been reported and explained by air contamination, re-orientation of the polar surface groups and diffusion and reaction of free radicals (Alves et al. 2014). In contrast, un-modified PDMS has shown to recover its hydrophobic characteristics (water contact angle 120°) within 100 h after the plasma treatment (Bodas and Khan-Malek 2007). Which indicates the use of PU membrane for applications that need to be perform on less hydrophobic material than PDMS.
Hydrophilic and hydrophobic recovery of PU. a Duration of plasma treatment: PU membranes were treated with air plasma cleaner for three different treatment times (minutes) and water contact angles were measured by using Contact Angle Meter (n = 3); b Hydrophobic recovery after plasma treatment: PU membranes were stored in PBS after treating them with air plasma for 2 min. Water contact angles were measured on the day of the treatment (Day 0), Day 3 and Day 7 (n = 3)
In our study, PU membranes used for cell culture were treated with plasma for two minutes to facilitate better cell adhesion. The ability to modify the surface properties of PU using plasma treatment gives the user the flexibility to develop membranes tailored to their specific applications.
3.4 Characterization of the elastic deformation behavior of the membrane by bulge test
In order to investigate elastic deformation properties of the membrane we performed bulge test experiments on 3 different samples. Figure 4d shows the deflection of 15 μm thick PU membranes with various applied pressures. The PU membranes underwent deformation with pressures up to 10 kPa without tearing. We calculated that the elastic modulus of the PU membrane was 13.7 megapascal (MPa). Many organ-on-a-chip platforms such as the lung, the heart, and the gut are subjected to linear/cyclic stretching of up to 10% (Janmey and Miller 2011; Benam et al. 2015) to mimic critical biophysical features of the organ. The PU membranes developed in this work were able to maintain their integrity while undergoing cyclic stretching at 10% deflection for a period of 2 weeks at 0.2 Hz frequency. Therefore, the PU membranes developed here should be suitable for long term mechanical stretching in cell and tissue culture applications.
Mechanical properties of PU. a Schematic showing the different layers that were assembled to obtain the bulge test unit; b Photograph showing the bulge test unit placed on the microscope stage: the unit is placed such that it is possible to observe bulging with high precision through the microscope; c Deflected membrane at 10.335 kPa as observed under the microscope. These images were used to calculate the bulge height for a given pressure; d Graph showing the effect of applied pressure on the bulge height of the membrane from the center (n = 3); e The stress-strain curve was calculated from the bulge test
3.5 Qualitative representation of small molecule absorption
The visual comparison of the fluorescent dye absorption of PU and PDMS are shown in Fig. 5. As can be seen that Rhodamine B absorbed noticeably into the PDMS but not into the polyurethane. The qualitative data suggests drastically lesser absorption of small molecules by PU compared to PDMS.
Small molecule absorption into PU and PDMS. Discs of PU and PDMS membranes were immersed in Rhodamine B dye solutions for 1 h, rinsed with phosphate buffer saline, and air-dried. a Rhodamine absorption into PDMS; b Rhodamine absorption into PU. The images are representative of three repeated experiments with exact same conditions
3.6 Handling of thin PU membrane
When released from the substrate, <15 μm thick PU membranes were susceptible to tearing and crumbling. As a result, they were difficult to handle and integrate into microfluidic devices. Consequently, we developed a unique lamination method (see supplementary Video 1 (A-D)), which allowed for ease of handling and integration into multilayer microfluidic devices in a repeatable fashion. Furthermore, it was possible to transport the membranes between facilities to use equipment for characterization without destroying the membranes.
3.7 Sterilization and cell viability measurements
For cell and tissue culture, sterilized substrates are necessary to prevent contamination. PU can be easily sterilized with different techniques such as plasma cleaning, ultraviolet light treatment, ethylene oxide treatment and hydrogen peroxide rinsing. However, the fabrication method used in this work involves different layers of other polymeric substrates such as thin acrylic sheets, which is not suitable for autoclaving or contact with ethanol. Therefore, we used a combination of hydrogen peroxide and UV-light exposure to sterilize the PU-integrated platform. To verify the cytocompatibility of PU membrane after sterilization, A549 cells were seeded on the PU membrane and cultured for 5 days. Figure 6a, b shows A549 cells on tissue culture treated polystyrene plate and on PU membrane. The number of cells observed on the final day of culture were comparable to the number of cells on PU substrate, there was no significant difference in the number of live cells/cm2 between the two substrates (student t test, p < 0.05). It demonstrates PU membrane’s compatibility as a cell and tissue culture substrate (Fig. 6c).
Cell culture compatibility of PU membrane. Live and Dead cell staining of the human adenocarcinomia cells (A549) after 5 days culture on polyurethane (PU) membrane, Red: dead cells; Green: live cells; a Cells cultured on tissue culture polystyrene (PS) plate; b Cells cultured on PU membrane; The tissue culture polystyrene (PS) plate was served as the control, scale bar = 100 μm; c Cell viability on the PU membrane was verified after 5 days of culture (n = 3). No statistical differences in viability were seen between cells cultured on either substrate as calculated by student t test where a value of P < 0.05 was considered statistically significant
4 Conclusions
Here, we have shown how thin, elastic, polyurethane membranes can be successfully fabricated for the integration into cell and tissue culture devices. Various properties of our PU membranes, such as their optical clarity, long-term elasticity, and biocompatibility, further demonstrated the usefulness of these membranes as a suitable substitute for PDMS. Therefore, we conclude that PU membrane can serve as a biocompatible and flexible substrate for a range of cell and tissue culture applications, including the development of complex tissue engineering platforms such as organs-on-a-chip where mechanical stretching of tissue culture is often required.
References
P. Alves, R. Cardoso, T.R. Correia, B.P. Antunes, I.J. Correia, P. Ferreira, Surface modification of polyurethane films by plasma and ultraviolet light to improve haemocompatibility for artificial heart valves. Colloids Surf. B Biointerfaces 113(Supplement C), 25–32 (2014)
S.M. Azmayesh-Fard, L. Lam, A. Melnyk, R.G. DeCorby, Design and fabrication of a planar PDMS transmission grating microspectrometer. Opt. Express 21(10), 11889–11900 (2013)
Regehr, K. J., M. Domenech, J. T. Koepsel, K. C. Carver, S. J. Ellison-Zelski, W. L. Murphy, L. A. Schuler, E. T. Alarid, and D. J. Beebe. 2009. 'Biological implications of polydimethylsiloxane-based microfluidic cell culture', Lab Chip, 9: 2132-9.
K.H. Benam, S. Dauth, B. Hassell, A. Herland, A. Jain, K.-J. Jang, K. Karalis, H.J. Kim, L. MacQueen, R. Mahmoodian, S. Musah, Y.-s. Torisawa, A.D.v.d. Meer, R. Villenave, M. Yadid, K.K. Parker, D.E. Ingber, Engineered in vitro disease models. Annu. Rev. Pathol.: Mech. Dis. 10(1), 195–262 (2015)
S.N. Bhatia, D.E. Ingber, Microfluidic organs-on-chips. Nat. Biotechnol. 32(8), 760–772 (2014)
D. Bodas, C. Khan-Malek, Hydrophilization and hydrophobic recovery of PDMS by oxygen plasma and chemical treatment—An SEM investigation. Sensors Actuators B Chem. 123(1), 368–373 (2007)
ChemInstruments, CAM-PLUS Cntact Angle Meter. from http://cheminstruments.com/contact-angle-meter.html (2016)
Corning, Properties of Code 7800 Pharmaceutical glass. from http://csmedia2.corning.com/LifeSciences/media/pdf/Description_of_%20Code_7800.pdf (2016)
M. Daimon, A. Masumura, Measurement of the refractive index of distilled water from the near-infrared region to the ultraviolet region. Appl. Opt. 46(18), 3811–3820 (2007)
K. Domansky, D.C. Leslie, J. McKinney, J.P. Fraser, J.D. Sliz, T. Hamkins-Indik, G.A. Hamilton, A. Bahinski, D.E. Ingber, Clear castable polyurethane elastomer for fabrication of microfluidic devices. Lab Chip 13(19), 3956–3964 (2013)
D.P. Dowling, I.S. Miller, M. Ardhaoui, W.M. Gallagher, Effect of surface wettability and topography on the adhesion of osteosarcoma cells on plasma-modified polystyrene. J. Biomater. Appl. 26(3), 327–347 (2011)
E.W. Esch, A. Bahinski, D. Huh, Organs-on-chips at the frontiers of drug discovery. Nat. Rev. Drug Discov. 14(4), 248–260 (2015)
P. Gu, T. Nishida, Z.H. Fan, The use of polyurethane as an elastomer in thermoplastic microfluidic devices and the study of its creep properties. Electrophoresis 35(2–3), 289–297 (2014)
C.K. Huang, W.M. Lou, C.J. Tsai, T.-C. Wu, H.-Y. Lin, Mechanical properties of polymer thin film measured by the bulge test. Thin Solid Films 515(18), 7222–7226 (2007)
D. Huh, B.D. Matthews, A. Mammoto, M. Montoya-Zavala, H.Y. Hsin, D.E. Ingber, Reconstituting organ-level lung functions on a chip. Science 328(5986), 1662–1668 (2010)
P.A. Janmey, R.T. Miller, Mechanisms of mechanical signaling in development and disease. J. Cell Sci. 124(1), 9–18 (2011)
T.W.A.C. Kelley, Gnuplot 4.4: an interactive plotting program. from http://gnuplot.sourceforge.net/ (2010)
D.Y. Leung, S. Glagov, M.B. Mathews, Cyclic stretching stimulates synthesis of matrix components by arterial smooth muscle cells in vitro. Science 191(4226), 475–477 (1976)
K. Matsunaga, K. Sato, M. Tajima, Y. Yoshida, Gas permeability of thermoplastic polyurethane elastomers. Polym. J. 37(6), 413–417 (2005)
S. Mishra, V.K. Bahl, Coronary hardware part 3--balloon angioplasty catheters. Indian Heart J. 62(4), 335–341 (2010)
R. Mukhopadhyay, When PDMS isn't the best. What are its weaknesses, and which other polymers can researchers add to their toolboxes? Anal. Chem. 79(9), 3248–3253 (2007)
P. Nath, D. Fung, Y.A. Kunde, A. Zeytun, B. Branch, G. Goddard, Rapid prototyping of robust and versatile microfluidic components using adhesive transfer tapes. Lab Chip 10(17), 2286–2291 (2010)
B.D. Riehl, J.H. Park, I.K. Kwon, J.Y. Lim, Mechanical stretching for tissue engineering: Two-dimensional and three-dimensional constructs. Tissue Eng. Part B Rev. 18(4), 288–300 (2012)
M. Roussel, C. Malhaire, A.-L. Deman, J.-F. Chateaux, L. Petit, L. Seveyrat, J. Galineau, B. Guiffard, C. Seguineau, J.-M. Desmarres, Electromechanical study of polyurethane films with carbon black nanoparticles for MEMS actuators. J. Micromech. Microeng. 24(5), 055011 (2014)
Smiths&Nephew, ALLEVYN Hydrocellular Foam Dressing (2016)
J.D. Wang, N.J. Douville, S. Takayama, M. ElSayed, Quantitative analysis of molecular absorption into PDMS microfluidic channels. Ann. Biomed. Eng. 40(9), 1862–1873 (2012)
Wu CL, Fang W, Yip MC (2015). Measurement of Mechanical Properties of Thin Films Using Bulge Test. Soc. Exp. Mech. Proc.;22:5.
R.J. Zdrahala, I.J. Zdrahala, Biomedical applications of polyurethanes: A review of past promises, present realities, and a vibrant future. J. Biomater. Appl. 14(1), 67–90 (1999)
Y. Zhao, J.S. Marshall, Spin coating of a colloidal suspension. Phys. Fluids 20(4), 15 (2008)
Acknowledgements
We gratefully acknowledge, Aaron Anderson from physical chemistry & applied spectroscopy, LANL, Quinn Mcculloch from MPA-CINT: Center for Integrated Nanotechnologies, LANL, Tito Busani from Center for High Technology Materials, UNM, and Microfabrication support from the P21. This work was supported by DTRA Interagency Agreement (IA) CMBXCEL-XLI-2-0001. This work utilized shared resources at UNM including CHTM research Facility, CINT-LANL, Bioscience LANL.
Public release: J9-16-1398, LA-UR-16-29177.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None.
Electronic supplementary material
Supplementary Video 1
Handling of thin PU membranes. PU membranes with 15 μm in thickness were fabricated on Si wafer. In order to transfer the membranes on cell culture devices, it is necessary to release the membrane from the wafer without any disruption. (A) Shows the difficulty of releasing or peeling the PU membrane from the silicon wafer; (B) Shows the peeling processes of PU from the wafer. The PU membrane was cut into 1 × 1 cm using a knife and the whole wafer was submerged under DI water overnight. Using a tweezer it was possible to peel the membrane from the wafer without any damage; (C) Shows how to flatten the PU membrane on a flat glass surface using a cotton swab; (D) Shows securing the membrane between two PET layers. (MP4 10,847 kb)
ESM 1
(MP4 11,657 kb)
ESM 2
(MP4 5353 kb)
ESM 3
(MP4 8420 kb)
Rights and permissions
About this article
Cite this article
Arefin, A., Huang, JH., Platts, D. et al. Fabrication of flexible thin polyurethane membrane for tissue engineering applications. Biomed Microdevices 19, 98 (2017). https://doi.org/10.1007/s10544-017-0236-6
Published:
DOI: https://doi.org/10.1007/s10544-017-0236-6