Abstract
Micro total analysis systems (-TAS) or labs-on-a-chip, have been spreading rapidly due to their desirable characteristics, including reductions in reagent consumption, space requirements and analysis time. This work aimed at establishing an integrated microfluidic system which can supply the cells with fresh medium of oxygen and nutrition continuously at a control flow rate mimicking the microenvironment in vivo. Human non-small cell lung cancer cell line SPCA1 was seeded in a microchip supplied with fresh medium at a constant rate of 15 mm/24 h controlled by a pump. The expression of P-gp for verapamil-pretreated or non-pretreated cells was assayed with immunofluorescence. Both groups cells were exposed to anticancer drug VP-16 at 30 μM for 6 h before the apoptosis analysis online. The results indicated that the cells could grow and spread well for 4 days in the microfluidic system successively furnished with fresh medium. Immunofluorescence assay showed that the intensity of the fluorescence for the verapamil-pretreated cells was obvious weak compared with that of non-pretreated cells. Apoptosis analysis demonstrated that the percentage of apoptotic cells for verapamil-pretreated group increased around twofold compared with that of non-verapamil pretreated group (26.5 ± 2.5% versus 10.9 ± 0.85%, p < 0.05), showing a similar results as by flow cytometry analysis. All these indicate that P-gp plays an important role in the resistance to VP-16 in SPCA1, the microfluidic system provides a suitable environment for cells survival and is valuable in long time cell culture and bioassays mimicking the microenvironment in vivo and deserved to be studied further.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The integration of various chemical devices and complex operations onto a microchip, also known as micro total analysis systems (-TAS) or labs-on-a-chip (Reyes et al. 2002; Tudos et al. 2001; Verpoorte 2002), have been spreading rapidly due to their desirable characteristics, including reductions in reagent consumption, space requirements and analysis time. Furthermore, as the scale of the fluidic microvolume is roughly proportional to living cell sizes and processing capabilities, combinations of cells and microchemical systems are useful to achieve practical prototypical micro-devices, such as tools for investigating cellular functions, biochemical reactors, and bio-microreactors (Andersson and Van Den Berg 2003; Yi et al. 2006; El-Ali et al. 2006; Khademhosseini et al. 2006). In recent years, many reports are related to the cell culture with the micro-devices, however, most of them are still performed with static medium, environments that are far from representative for the cells in vivo and rare involved in long term cell culture. Therefore, it is essential to establish a microfluidic platform supplied with fresh medium of oxygen and nutrition at a control flow rate continuously for mimicking cellular microenvironments to achieve cell culture and biomedical assay in an environment closer to the in vivo situation.
Lung cancer is currently the leading cause of cancer deaths worldwide no matter in men or women. Chemotherapy is an important means of the treatment for patients with lung cancer. However, the drug resistance as developed during the treatment really limits the efficacy of chemotherapy. Multiple pathways are suggested to be involved in the complexity of chemotherapy resistance in lung cancer. P-glycoprotein (P-gp), a kind of protein product of the MDR-1 gene, which expressed as a transmembranal protein (Mr 170 000), is capable of decreasing the intracellular concentration of a broad range of cytotoxic agents in an energy-dependent mediated efflux (Hrycyna 2001; Sauna et al. 2001). It is reported that the development of multiple drug resistance (MDR) characterized by intrinsic P-gp expression, is a general phenomenon occurring in several tumors, including hepatocellular carcinoma. But little is known on the drug resistance mediated by P-gp in human lung cancer cell lines.
In this work, an integrated microfluidic system was developed which can supply the cells with continuously fresh medium of oxygen and nutrition at a control flow rate around 15 mm/24 h mimicking the microenvironment in vivo. With this system, the expression of P-gp for human lung cancer cell line SPCA1 with or without the pretreatment of verapamil—a known P-gp inhibitor, was assayed by Immunofluorescence, and the relationship between the expression of P-gp and resistance to anticancer drug VP-16 was analyzed as well.
2 Materials and methods
2.1 Fabrication of microfluidic system
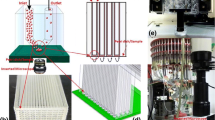
The microfluidic system was composed of a MS26 injection pump and a single channel microchip (Fig. 1). The microchip was fabricated in PDMS (Sylgard 184, Dow Corning, Midland, MI, USA) by standard soft lithography methods (Dertinger et al. 2001; Tilles et al. 2001). The PDMS microchip was fabricated by replica molding PDMS against the masters. Inlets and outlets were drilled with a blunted and beveled syringe needle, and the resulting PDMS microchip was irreversibly bonded to a glass slide assisted by oxygen plasma surface treatment (150 mTorr, 50 W, 20 s). The length, width and depth of the channel are 24 mm, 240 μm and 150 μm, respectively (Fig. 2). The MS26 injection pump is a power driven device for pushing the plunger of a syringe forward at an accurately controlled rate. The motor turns every (168÷rate set) minutes. Because the volume of the syringe fixed on the pump was 1 ml, 2 μl will be driven by one pulse of the motor. In addition, since the total volume of the microchannel is less than 1 μl, the medium can be refreshed completely after one pulse.
2.2 Cell culture
The human non-small cell lung cancer cell line SPCA1 was obtained from ATCC (Manassas, VA, USA). Prior to cell injection, the microfluidic system was sterilized by UV irradiation, after that, the PDMS microchip was treated as follows: First, the channel was washed with dehydrated alcohol and water, successively, for 1 h each in an ultrasonic bath. Next, the chip was autoclaved at 120°C for 15 min. The channel was filled with 0.01% poly-L-lysine solution (Sigma-Aldrich Co., St. Louis, MO) for 1 h in order to coat its inner surface. The SPCA1 cells dissociated from the culture flask were injected into the microchip via the cell inlet at the density of around 1 × 106 cells per milliliter, the total injected volume was 10 μl. Then the chip was put into a 10 cm culture dish and set for 2 h before the connection of the MS26 injection pump. The fresh medium of PRMI 1640 medium supplemented with 10% FBS, 100 U/ml penicillin and 100 U/ml streptomycin was injected through the pump at a constant rate of 1 mm/24 h, 5 mm/24 h, 10 mm/24 h and 15 mm/24 h, respectively. Then, the cells were incubated at 37°C in a humidified atmosphere with 5% CO2. The morphology of cells was observed by a microscope successively at the time points of 24 h, 48 h, 72 h, and 96 h, the viability of the cells was measured by trypan staining as before (Choi et al. 2008).
2.3 Cells treatment
After 4 days’ cell culture in the microfluidic system, the cells were divided into verapamil pretreatment group and control group (non-verapamil pretreatment group). For the former, verapamil (Invitrogen Co. USA) at concentration of 10 μM was added to the medium and fed the cells for another 24 h; for the later, the free medium was used. The medium was injected into the microchannels through the pump as above. The expression of P-gp for the two groups cells were assayed by immunofluorescence.
In order to elucidate the correlation between the expression of P-gp and anti-cancer drug VP-16, the cells of the both groups were treated with VP-16 at 30 μM continuously for 6 h, after that, apoptosis was detected by PI and Hochest staining in the microfluidic system as well as by flow cytometry in parallel.
2.4 Immunofluorescence assay of Pg-p expression
P-gp expression for the cells of the two groups was determined by immunofluorescence. Briefly, after two times wash with PBS, the cells were fixed with 4% paraformaldehyde in PBS for 25 min, permeablized in PBS containing 0.1% Triton X-100 and 5% bovine serum albumin for 30 min before the detection of P-gp with immunofluorescence. The media with anti- P-gp goat polyclonal antibody (Santa Cruz Biotechnology, Inc., Santa Cruz, CA) at a dilution of 1:500 were introduced into the channel and the cells were incubated over night at 4°C. After being washed with PBS for three times, the cells were stained with anti-goat FITC green-conjugated secondary antibody (Santa Cruz Biotechnology, Inc) at a dilution of 1:200 at 37°C for 1 h. Cell images were subsequently captured with fluorescence microscope (IX-71; Olympus Optical Co., Tokyo, Japan).
2.5 Analysis of apoptosis after VP-16 treatment
The viabilities of the cells either non-pretreated or verapamil-pretreated were assayed after the treatment by anti-cancer drug VP-16 at concentration of 30 μM. The drug medium with VP-16 was introduced into the culture chambers respectively. After 6 h incubation, the cells were then washed with PBS. Hochest at a concentration of 5 μg/ml was injected into the channels and incubated for 30 min. After being washed with PBS twice, propidium iodide (PI) at a concentration of 10 μg/ml was injected into the channel. Stained nuclei were visualized and photographed using a Zeiss fluorescence microscope (IX-71; Olympus Optical Co., Tokyo, Japan). Alive cells were stained blue whereas apoptotic cells were stained red.
In order to verify the results with the new system, analysis of apoptosis on the cells cultured in the flask were also done with flow cytometry parallelly. The both groups cells were exposed to VP-16 at concentration of 30 μM as well. Annexin V and PI fluorescein isothiocyanate (PharMingen) were used to stain the cells as usual (Wang et al. 2008), the percentage of apoptotic cells were assayed by flow cytometry (FAC star; BD Biosciences).
2.6 Statistical analysis
The statistical analysis was carried out with SPSS 12.0 for Windows software and student’s t test was used to compare the results of analysis of apoptosis. A value of p < 0.05 was regarded as statistically significant.
3 Results
3.1 Fabrication of the microfluidic system and cell culture
3.1.1 Flow rate adjustment in the system
We successfully built the microfluidic system (Fig. 1) and carried out cell culture with it. The flow rate of medium was set at 1 mm/24 h, 5 mm/24 h, 10 mm/24 and 15 mm/24 h respectively followed the injection of cells into the microchip at the density of 4 × 106. The morphology of cells was observed after 24 h culture. As shown in Fig. 3, the cells grew and spread well when the flow rate was below 15 mm/24 h. However, if the flow rate was faster than 15 mm/24 h, shape of cells turned round and cells were flowed away because of the strong shearing force. Therefore, the flow rate should be set below 15 mm/24 h.
3.1.2 Successive SPCA1 cell culture in the system
After injected into the microchip at the density of 1 × 106 cells/ml, the SPCA1 cells were cultured in the system with the supply of fresh medium at the rate below 15 mm/24 h. As it is shown in Fig. 4, the cells grew and propagated well and the number of cells in the system increased gradually after 24 h. Till the third day, cells became confluent, and after being cultured for 4 days successively, the cells spread fully and took up almost all the parts of the microchannel. Trypan blue exclusion assay showed less than 1% of cells died. The viability and the morphology of the cells suggested that the microfluidic system provides a suitable environment for cells growth and the cells could be used in other assays further (Fig. 5).
3.2 Expression of Pg-p
To examine the effect of verapamil on Pg-p expression in SPCA1 cell line, we carried out an immunofluorescence assay on the cells pretreated with or without verapamil at concentration of 10 μM for 24 h. As it is shown in Fig. 6, Pg-p displayed a membrane presented pattern of green fluorescence (excitation at 488 nm) distributed in the cells. Compared with the non-pretreated cells, the intensity of the fluorescence for the verapamil-pretreated cells was clearly weak which meant verapamil could inhibit the expression of Pg-p effectively in SPCA1 cell line.
3.3 Correlation between expression of Pg-p and drug-resistance to VP-16
In order to know whether down-regulation of Pg-p inhibited by verapamil could lead to the decrease of drug resistance to VP-16 in SPCA1 cell line, the cells of either verapamil-pretreated or non-verapamil pretreated were exposed to VP-16 for 6 h, specific features of apoptosis were detected by PI and Hochest staining for the cells in the microfluidic system online and by Annexin V and PI staining for the cells cultured in the flask with conventional flow cytometry in parallel. With the new system, the percentage of apoptotic cells for verapamil-pretreated group increased around twofold compared with that of the non-verapamil pretreated group (26.5 ± 2.5% versus 10.9 ± 0.85%, p < 0.05, Fig. 7); while with the flow cytometry, analysis also showed the similar results (18.94 ± 2.11% versus 9.63 ± 1.23%, p < 0.05, Fig. 8). All these suggest that Pg-p inhibition could enhance VP-16 induced apoptosis in SPCA1 cell line, which meant Pg-p had the correlation to the resistance to VP-16 in human non-small cell lung cancer as well. It also suggests that the microfluidic system is proper for the functional assay on cells.
(a) Fluorescent microscopic analysis of apoptotic cells stained with PI and Hochest staining after treatment with VP-16. a verapamil-pretreated group; b non-verapamil pretreated group; Stained with red were apoptotic cell while blue cells were alive (×100). (b) The statistic analysis of percentage of apoptotic cells with PI and Hochest staining in verapamil-pretreated and non-verapamil pretreated groups. All the experiments were repeated three times
(a) Measurement of apoptotic cells under VP-16 (30 μM) treatment for 6 h determined by flow cytometry analysis. a verapamil-pretreated group; b non-verapamil pretreated group; The cells were labeled with annexin V and PI. Viable cells were those with low annexin or no annexin and PI staining (lower left panel). Early stage apoptotic cells were represented by high annexin and low PI staining (lower right panel), later stage apoptotic cells were represented by high annexin and high PI staining (upper right panel), and necrosis cells were represented by high PI and low annexin staining (upper left panel). (b) The statistic analysis of percentage of apoptotic cells in verapamil-pretreated and non-verapamil pretreated groups. All the experiments were repeated three times
4 Discussion
We were to build an integrated microfluidic system which can supply the cells with fresh medium continuously for mimicking the microenvironment in vivo. The flow rate of medium was controlled through a MS26 injection pump, a connection between the pump and microchip was successfully conducted and the cells culture was carried out within the system for as long as 4 days. The viability and the morphology assay showed that SPCA1 cells grew and propagated well in the system which suggested that the microfluidic system could provide a suitable environment conducive for cell growth and proliferation. In the investigation, the control of the medium flow rate was critical in this system. With high flow rate, cells were washed away because of the strong shearing force, whereas with low flow rate, cells lost their viability because of a shortage of nutrients and oxygen. We found that to maintain the flow rate at lower than 15 mm/24 h (about 24 mm/pulse /11mins) is better for the SPCA1 cells culture and further assay. Although the flow rate in the system is much lower than that of human capillary vessel (0.5–1 mm/s) physiologically, the system can successively refresh the medium in the microchannel and a successive supply of oxygen and nutrient flow to the cells in the channel could keep them grow and propagate well in the system. As a contrast, our parallel experiment with static medium revealed that the cells only can survive for 2 days (data not shown). All these suggest that the microfluidic system could be used for cell culture and related research mimicking the microenvironment in vivo and has the potential to be further studied.
In this study, the PDMS chip was used for the cell culture and vital analysis. In contrast to glass and silicon, polymers are inexpensive and less fragile. Having the characteristic of optically transparent and biocompatible with high gas and oxygen permeability, PDMS chips were often used in cell culture (Tomida and Tsuruo 1999; Torisawa et al. 2007). Cultured in the PDMS chip, the expression of P-gp and the apoptosis analysis induced by VP-16 for the human lung cancer SPCA1 cell line were also done in the work. The whole processes from cell culture to the detection of P-gp with immunofluorescence and apoptosis analysis online were fulfilled which involved simple liquid-handling procedures and low consumption of reagents (especially for the expensive antibody) and short time analysis. Furthermore, there is no handing intervention during the process of cell culture, since the microfluidic control device would refresh the medium successively and automatically. Thus, our system may be ideal for cell-based biological studies.
In addition, the investigation with the new system revealed two novel observations: First, the expression of P-gp at protein level was decreased significantly with the inhibition of verapamil in the human lung cancer SPCA1 cell line. Second, the apoptosis percentage VP-16 induced in the cells pretreated with verapamil was significantly higher than that of the cells non-pretreated (Fig. 4) Interestingly, the apoptosis results were consistent with that by the conventional methods of flow cytometry. To our best knowledge, this is the first report on the down-regulation of P-gp by verapamil, including the function of the suppression in the resistance to VP-16 in human lung cancer SPCA cells assay with the microfluidic system.
Nowadays, only few reports are involved in P-gp associated chemotherapy resistance to VP-16. VP-16 is the topoisomerase inhibitor and can interact with the enzyme to stabilize topoisomerase-DNA complex, blocking strand-passing activity, thereby resulting in DNA breakage (Froelich-Ammon and Osheroff 1995). P-gp encoded by the MDR1 gene is an important member of the ATP-binding cassette transporters which acts as an ATP-driven efflux pump for a wide variety of structurally and functionally unrelated anti-cancer agents, including the vinca alkaloids, anthracyclines, epipodophyllotoxins (VP-16) and taxanes, as well as other cytotoxic agents (Che et al. 2002). Overexpression of P-gp is the best understood mechanism of multidrug resistance (MDR) associated factor (Ponce de León and Barrera-Rodríguez 2005), whereas Verapamil can inhibit the function of P-gp through the inhibition of MDR-1or the increase of drug concentration in the cancer cells by competitively combining P-gp. Therefore, down-regulation of P-gp may become a new focal point for the cancer therapy.
5 Conclusions
We developed an integrated microfluidic system which can supply fresh medium continuously to the cells mimicking the microenvironment in vivo. The human lung cancer cell line SPCA1 can be cultured and grow well in the system. The assay of the expression of multidrug resistance related protein P-gp and the correlation between the expression of P-gp and resistance to VP-16 were fulfilled in the system with many advantages such as lower quantity of chemical reagents, simple handling course, and high degree of integration. All these indicate that the system was valuable in long time cell culture and bioassays mimicking the microenvironment in vivo and deserved to be studied further.
References
H. Andersson, A. Van Den Berg, Sens. Actuators 92, 315–325 (2003)
X.F. Che, Y. Nakajima, T. Sumizawa, R. Ikeda, X.Q. Ren, C.L. Zheng, M. Mukai, T. Furukawa, M. Haraguchi, H. Gao, Y. Sugimoto, S. Akiyama, Cancer Lett. 187, 111–119 (2002)
S.H. Choi, S.E. Jin, M.K. Lee, S.J. Lim, J.S. Park, B.G. Kim, W.S. Ahn, C.K. Kim, Eur. J. Pharm. Biopharm. 68, 545–554 (2008)
S.K.W. Dertinger, D.T. Chiu, N.L. Jeon, G.M. Whitesides, Anal. Chem. 73, 1240–1246 (2001)
J. El-Ali, P.K. Sorger, K.F. Jensen, Nature 442, 403–411 (2006)
S.J. Froelich-Ammon, N. Osheroff, J. Biol. Chem. 270, 21429–21432 (1995)
C. Hrycyna, Cell Dev. Biol. 12, 247–256 (2001)
A. Khademhosseini, R. Langer, J. Borenstein, J.P. Vacanti, Proc. Natl. Acad. Sci. 103, 2480–2487 (2006)
V. Ponce de León, R. Barrera-Rodríguez, Cancer Cell Int. 5(1), 20 (2005)
D. Reyes, D. Iossifidis, P. Auroux, A. Manz, Anal. Chem. 74, 2623–2636 (2002)
Z.E. Sauna, M.M. Smith, M. Müller, K.M. Kerr, Ambudkar SV. J. Bioenerg. Biomembr. 33, 481–491 (2001)
A.W. Tilles, H. Baskaran, P. Roy, M.L. Yarmush, M. Toner, Biotechnol. Bioeng. 73, 379–389 (2001)
A. Tomida, T. Tsuruo, Anticancer Drug Des. 14, 169–177 (1999)
Y.S. Torisawa, A. Takagi, Y. Nashimoto, T. Yasukawa, H. Shiku, T. Matsue, Biomaterials 28, 559–566 (2007)
A. Tudos, G. Besselink, R. Schasfoort, Lab Chip 1, 83–95 (2001)
E. Verpoorte, Electrophoresis 23, 677–712 (2002)
Y. Wang, W. Wang, S. Wang, BMC Cancer 8, 372–381 (2008)
C.Q. Yi, C.W. Li, S.L. Ji, M.S. Yang, Anal. Chim. Acta 560, 1–23 (2006)
Acknowledgement
This work was supported by National Nature Science Foundation of China.
Author information
Authors and Affiliations
Corresponding author
Additional information
Zhao Long and Wang Zhenshan both contributed equally.
Rights and permissions
About this article
Cite this article
Zhao, L., Wang, Z., Fan, S. et al. Chemotherapy resistance research of lung cancer based on micro-fluidic chip system with flow medium. Biomed Microdevices 12, 325–332 (2010). https://doi.org/10.1007/s10544-009-9388-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10544-009-9388-3