Abstract
Objectives
To determine the optimal storage solution containing suitable protective agents for the preservation of microencapsulated hepatocytes at 4 °C as well as the optimum incubation time after hypothermic preservation.
Results
L15 was the optimum solution for both maintaining microcapsule integrity and cell viability. Furthermore, 5 %(v/v) PEG (20 or 35 kDa) added to Leibovitz-15 medium was optimal for microencapsulated C3A cells, enhancing cell viability and liver-specific functions, including albumin and urea synthesis as well as CYP1A2 and CYP3A4 activities. The transcription levels of several CYP450-related genes were also dramatically increased in cells incubated in the optimal solution. Pre-incubation for 2 h was the optimal time for restoring favorable levels of CYP1A2 and CYP3A4 activities in microencapsulated C3A cells for short term, 2 day storage.
Conclusions
Leibovitz-15 medium supplemented with 5 % (v/v) PEG is a promising cold solution for microencapsulated hepatocytes at 4 °C, with an incubation of 2 h at 37 °C after hypothermic preservation being the best incubation duration for further cell application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver transplantation is the only effective treatment for many intractable hepatic diseases; however, it is limited by a shortage of donor organs (Aoki et al. 2005). Hepatocyte transplantation may serve as an alternative to whole-liver transplantation (Fox and Roy-Chowdhury 2004). As large numbers of hepatocytes are used in cell transplantation, it is necessary to establish a system capable of storing hepatocytes that are easily accessible on demand (Aoki et al. 2005). Various methods of low-temperature preservation of hepatocytes for multiple purposes have been presented. At present, cell preservation at 2–8 °C for hypothermic cold storage for several days is used widely, which is similar to the conditions used for the storage of organs or bioartificial livers (Janssen et al. 2003).
Compared with the storage of isolated hepatocytes, encapsulated hepatocyte technology is a promising approach to cell transplantation and bioartificial liver systems for clinical use (Khan et al. 2002). This method could preserve a greater quantity of hepatocytes without immunosuppression, and provide a safe and feasible way for the chemically stable immobilization of hepatocytes (Ostrowska et al. 2009). Thus, developing an effective and convenient storage method for the hypothermic preservation of microencapsulated hepatocytes is critical to meeting clinical requirements.
Choosing an appropriate solution is the first step in ensuring appropriate hepatocyte storage. An ideal solution for microencapsulated hepatocytes should maintain both microcapsule stability and cell viability (Hang et al. 2010). This study investigated several reported solutions that have been proven effective for storage methods, including the University of Wisconsin (UW), Celsior (CEL), histidine tryptophan a-ketoglutarate (HTK) (Gramignoli et al. 2014; Serrar et al. 1999), Leibowitz-15 (L15) (Poullain et al. 1992), and selected the optimal medium to store microencapsulated hepatocytes at 4 °C in terms of microcapsule integrity and the viability of microencapsulated cells.
Protective agents added to cold solutions arebeneficial for enhancing preservation efficiency by preventing cell damage caused by hypothermia (Hang et al. 2010). High molecular weight PEG (such as 20 k and 35 k Da; PEG20 and PEG35, respectively) can exert protective effects against cold-induced injury during cell transplantation (Dutheil et al. 2006; Valuckaite et al. 2009). Trehalose is also frequently added to preservation medium (Katenz et al. 2007). This study was evaluated the protective effect of PEG20, PEG35 and trehalose on microencapsulated cells by determining cell viability and related functions Moreover, pre-incubation in culture medium for several hours at 37 °C is another method to protect cells from hypothermic damage and to restore cell functions (Terry et al. 2006), the optimum duration of incubation at 37 °C of microencapsulated hepatocytes after removal from hypothermic preservation was determined. To our knowledge, this study is the first to assess the optimal incubation time of microencapsulated hepatocytes for purposes of preserving liver-specific functions.
Materials and methods
Cell culture
C3A cells (CRL-10741, ATCC) were cultured in Dulbecco’s modified eagle medium (DMEM) supplemented with 10 % (v/v) fetal bovine serum and 1 % penicillin/streptomycin. For collection, cells were removed from culture plates by enzymatic digestion with 0.05 % trypsin EDTA. Cells were counted and diluted to 3 × 106/ml with 2 % (v/v) alginate.
Cell-microcapsule production
Alginate/chitosan (AC) microcapsules were produced: a mixture of 3 × 106 C3A cells/mL with 2 % sodium alginate(154 mM NaCl, 10 mM HEPES, pH 7.4) was sprayed at 9.5 ml/min through an electrostatic microencapsulator unit (NiscoEngineering, Zurich, Switzerland). The alginate droplets fell into 0.7 % chitosan solution (DAC 85.6 %), dissolved in deionized water containing 0.1 M CaCl2, 15.6 M HEPES, pH 6.0), which was allowed to gel for 30 min, and was washed with normal saline three times. AC microcapsules containing C3A cells with diameters of 800 mm were produced.
Groups
To determine microcapsule integrity and cell viability, four experimental groups and one control group were used. Five ml of AC microcapsules per well was stored separately in six-well plates containing 10 ml UW (Bristol Myers Squibb B.V., Woerden, Netherlands), CEL (Genzyme Polyclonals S.A.S., Limoges, France), histidine tryptophana-ketoglutarate (Dr. Franz Koehler Chemie Gmbh, Alsbach-Haehnlein, Germany), Leibovitz 15 (Gibco, Auckland, NZ). The control group consisted of 5 ml of AC microcapsules stored in 10 ml DMEM supplemented with 10 % (v/v) fetal bovine serum and 1 % penicillin/streptomycin.
In the second test, various protective agents; i.e., 5 % (v/v) PEG20 (Sigma), 5 % (v/v) PEG35 (Sigma) and 0.4 M trehalose (Campbell and Brockbank 2012), were added to storage solutions separately. The control solution was as described above. The solutions were stored at 4 °C for 3 days for both tests.
To determine the optimal incubation time, solutions containing the protective agents were used as the experimental groups. The control solution was as described above (DMEM group). The solutions were stored at 4 °C for 3 days. On each day, the solutions were exchanged for culture medium and then incubated at 37 °C for 0 h, 2 h, 6 h, 12 h, and 24 h.
Microcapsule integrity in cold-preservation solutions
Microcapsule integrity was employed to enhance the effectiveness of microcapsule storage. C3A microcapsules were preserved in the five different solutions at 4 °C for 3 days. Every 24 h, 500 microcapsules were selected from each group and placed into a 15 ml centrifuge tube with 5 ml normal saline and shaken at 180 rpm for 24 h on a horizontal shaker. After 24 h, the microcapsules were assessed under a microscope, and the deformed and broken microcapsules were counted.
Cell viability test
To demonstrate the viability of cells in different cold solutions with and without protective agents, microcapsules containing C3A cells in four experimental solutions and the control group were assessed using the cell proliferation (MTT) assay.
Cell staining and imaging by fluorescence microscopy were used to estimate cell viability. Cells were labeled using the rhodamine 123 and 5- (and 6-) carboxy-4′,5′-dimethylfluorescein diacetate (CMFDA). Dead cells were labeled with propidium iodide (PI).
Cytochrome P450 1A2 and 3A4 activity assay
Cytochrome P450 (CYP450) 1A2 and 3A4 activities were determined in the recovered cells using 24-well plates by directly testing luciferase activity with the P450-Glo CYP1A2 assay (V8422; Promega, Madison, WI) and the CYP3A4 assay (V9002; Promega, Madison, WI), respectively.
Urea and albumin synthesis tests
Urea concentration was determined using a urea assay kit (DIUR-500, Biotechnology BioAssay Systems, Hayward, CA). Albumin concentration was determined using the human albumin ELISA quantitation set (E80–129; Bethyl Laboratories, Montgomery, TX). The results were analyzed using CurveExpert 1.3 software and fitted with the logistic model with R2 > 0.99.
Real-time PCR
After hypothermic preservation and incubation for 3 days, microencapsulated C3A cells were suspended in 55 mM sodium citrate (pH 8.0), centrifuged at 1000 rpm for 5 min, and washed twice with phosphate-buffered saline. RNA was extracted with TRIzol. cDNA was synthesized using an oligo primer and reverse transcription kit (Qiagen). Real-time quantitative PCR analyses were processed on a Bio-Rad Cycler using customized PCR arrays with various sequences. (Supplementary Table 1).
Statistical analysis
Measurements are presented as means ±SDs. Statistical analyses were performed using the Student’s t test and one-way analysis of variance (ANOVA) using SPSS for Windows version 16.0 (Chicago, IL, United States). Results were considered statistically significant at a p value < 0.05.
Results
Microcapsule integrity
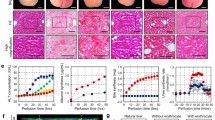
The rates at which microcapsules were damaged after shaking in the five different cold mediums are presented in Fig. 1. Microcapsules in UW and CEL solutions had significantly higher breaking rates per day (p < 0.05) compared with the other three groups.
Cell viability
C3A cell viability determined by MTT (Fig. 2a) and CMFDA and PI staining (Fig. 2b) was measured. In general, cell viability in the five solutions decreased with increasing time over the 3 days. The viability of cells in DMEM and HTK solutions significantly decreased compared with those in the other three solutions on days 2 and 3 (p < 0.05). The cell viability in the L15 solution was higher than that of cells in the UW and CEL solutions on day 2 (p < 0.05). The results of the MTT assay were consistent with the staining results.
C3A cell viability in the five cold solutions. a Cell viability according to MTT assay results. b Images of live (CMFDA stained) and dead (propidium iodide stained) C3A cells in microcapsules. Scale bar, 500 µm. CMFDA, fluorophores rhodamine 123 (R123), 5- (and 6-) carboxy-4′,5′-dimethylfluorescein diacetate
The results indicated marked damage to microcapsules in UW and CEL solutions and low cell viability in HTK solution (Figs. 1, 2). Due to the unfavorable performance in terms of maintaining microcapsule integrity and cell viability, the three solutions were deemed unsuitable for the hypothermic preservation of microencapsulated hepatocytes. Therefore, L15 was employed in the subsequent experiments.
L15 was supplemented with 5 % PEG20 (L15+5%PEG20), 5 % PEG35 (L15+5%PEG35), or 0.4 M trehalose (L15+7.6%trehalose). C3A cell viability rates in the three protective agent groups and the control (DMEM) group were determined using the MTT assay (Fig. 3a) and FDA and PI staining (Fig. 3b). For 3 days, the cell viability in the four groups had gradually declined. Cell viability in L15+5%PEG35 was higher than that in other groups (p < 0.05) during the previous 2 days. Cell viability in L15+5%PEG20 and L15+5%PEG35 was significantly increased compared with that in the other two groups on the last day (p < 0.05), while there was no significant difference between PEG of different molecular weights. The results from the staining experiments were in agreement with the MTT findings.
C3A cell viability in solutions with protective agents. a Cell viability in DMEM and L15 with different protective agents according to MTT assay results. b Images of live (CMFDA stained) and dead (propidium iodide stained) C3A cells in microspheres. Scale bar, 500 µm. CMFDA, fluorophores rhodamine 123 (R123), 5- (and 6-) carboxy-4′,5′-dimethylfluorescein diacetate
Cell metabolic functions
The activities of P450 CYP3A4 and CYP1A2 were estimated to evaluate the biotransformation ability of C3A cells in L15 cold solutions with different protective agents (Fig. 4a, b). The CYP3A4 and CYP1A2 activity of cells in L15 supplemented with PEG was significantly increased compared with that of the control and L15+ trehalose groups for 3 days (p < 0.05).
Hepatocyte-related functions of C3A cells in solutions supplemented with protective agents. a, b Activities of phase I enzymes CYP 1A2 (a) and CYP3A4 (b) measured via fluorometric substrates in DMEM and L15 with different protective agents. c, d Rates of albumin secretion (c) and urea synthesis (d) of C3A cells in DMEM and L15 supplemented with different protective agents. Columns labeled with the same letter indicate statistically insignificant results; for all other comparisons, p < 0.05
Albumin (Fig. 4c) and urea (Fig. 4d) levels in C3A cells were quantitatively measured for the encapsulated cells in L15 with different protective agents. The albumin concentrations of cells in L15 with PEG were significantly higher than those in L15 with trehalose for 3 days (p < 0.05). Urea synthesis by the encapsulated C3A cells in L15 with PEG was greater than that of the other groups on day 1 (p < 0.05). On the last day, urea synthesis in cells in L15 supplemented with protective agents was higher compared with that of the control group (p < 0.05). Thus, L15 with PEG significantly improved albumin and urea synthesis; however, there were no differences in levels between the two different molecular weights of PEG.
Regarding the evaluation of protective agents, L15 supplemented with 5 % PEG significantly increased the functions of CYP450 enzymes. As a result, L15+5%PEG20 and L15+5%PEG35 were used to explore the optimal incubation time for recovery of special functions (Fig. 5a, b, c). With regard to various incubation times, the highest CYP1A2 and CYP3A4 activities were present in the cells that were incubated for 2 h during the first 2 days. However, the highest CYP450 activity was seen after an incubation of 6 h on the last day.
Gene expression
Several classes of CYP450 phase I and II enzymes and specific proteins were selected to determine the transcription levels of metabolism-related genes in hepatocytes by real-time PCR (Fig. 6). The normalized transcription levels of several CYP450-related genes and albumin-related genes (1A2, 3A4, ALB) were significantly greater in cells in L15 with different protective agents compared with in cells of the control group (p < 0.05). Regarding expression of the three genes, the improvements in L15 supplemented with PEG were significantly greater than those in L15 supplemented with trehalose (p < 0.05). Furthermore, enhanced expression levels of 3A5 were found in cells in L15+5%PEG35 (p < 0.05).
Normalized gene expression of CYP450 enzymes in C3A cells after 72 h of culture. a Normalized gene expression of CYP450 enzymes in C3A cells in DMEM and solutions with protective agents. b Normalized gene expression of CYP450 enzymes in C3A cells in solutions with different incubation times. All data were normalized to the activity of C3A cells cultured under static conditions
Discussion
This study investigated the short-term hypothermic preservation of microencapsulated hepatocytes at 4 °C and aimed to determine the optimum preservation solution by assessing the effects of various protective agents on cell functions. Furthermore, the optimal cell incubation duration after hypothermic preservation was determined.
In the first part of this study, several solutions that were used in previous studies were evaluated. The majority of microcapsules maintained their original shapes in all solutions but UW and CEL. Previous studies demonstrated that lactobionate is an important component of the UW and CEL solution, where it acts to decrease cell swelling to preserve viability (Uhlmann et al. 2002). However, as a calcium chelator, lactobionate would disrupt the spherical structure of the microcapsule, as calcium compounds are crucial components of microcapsules, resulting in the deformation and damage seen under microscopy. Our comparison of microcapsule integrity and cell viability determined that L15 was the ideal solution for the hypothermic storage of microencapsulated hepatocytes.
Previously, unfavorable cell viability appeared during hypothermic preservation in which a medium was used without a protective agent (Meng 2003). In this study, two molecular weights of PEG and trehalose were added to L15 individually The results demonstrated that microencapsulated hepatocytes stored in L15 with 5 % PEG had significant improvements in cell viability and functioning as well as increases in the expression levels of most of the selected genes. The presence of PEG was previously reported to reduce cell swelling (Poullain et al. 1992) and suppress lipid peroxidation (Mack et al. 1991), resulting in the prevention of cell damage caused by hypothermia. Therefore, it could have increased viability and improved the liver functioning in the PEG groups. However, although trehalose is beneficial in the process of cryopreservation (Katenz et al. 2007), it showed no positive effects on hypothermic storage in this study.
The functions of microencapsulated hepatocytes undergoing hypothermic preservation were enhanced by the use of suitable solutions, protective agents, and pre-incubation durations (Terry et al. 2006). With regards to pre-incubation, hepatocytes were not revived rapidly or effectively when they were immediately transferred from cold solutions to culture medium (Terry et al. 2006). Thus, incubation time was necessary to restore hepatocyte function. To assess whether various incubation times could influence hepatocyte activity, their functional capabilities should be compared with that of hepatocytes with no incubation time. To date, such comparisons have been rare. In this study, we explored different incubation times of microencapsulated hepatocytes at 37 °C after storage at 4 °C. The results showed that incubation for 2 h after hypothermic preservation was the most efficient in maintaining and elevating CYP450 function and related-gene expressions. However, CYP450 activity had not yet reached an optimal level at an incubation time of 2 h on day 3. This may be due to translational modifications or environmental stimuli (Meng 2003), Nevertheless, the mechanisms underlying the functional improvements in microencapsulated hepatocytes with varying incubation times remain to be determined by future studies.
Conclusion
The L15 solution could be appropriate for hypothermic preservation of microencapsulated C3A cells in terms of maintaining microcapsule integrity and cell viability. Furthermore, cell viability and specific functions were well preserved in L15 supplemented with 5 % PEG, indicating that the addition of suitable protective agents could be beneficial. Moreover, this study was the first to explore the effect of pre-incubation time on reviving microencapsulated hepatocytes and demonstrated that incubation for 2 h at 37 °C was the most beneficial incubation time for recovery of specific liver functions. These results provide a solid foundation for the future clinical use of microencapsulated hepatocytes. Overall, L15 supplemented with 5 % PEG appears to be a promising cold solution for storing microencapsulated hepatocytes on a short-term basis at 4 °C. Moreover, incubation at 37 °C for 2 h prior to 2 days of hypothermic preservation could be the optimal incubation time for further hepatocyte use.
Abbreviations
- UW:
-
University of Wisconsin solution
- CEL:
-
Celsior solution
- HTK:
-
Histidine tryptophana-ketoglutarate solution
- L15:
-
Leibovitz 15
- L15+5%PEG20:
-
Leibovitz 15 supplemented with 5 % (v/v) polyethylene glycol (20 k Da; 5 g PEG mixed into 100 ml Leibovitz 15)
- L15+5%PEG35:
-
Leibovitz 15 supplemented with 5 % (v/v) polyethylene glycol (35 k Da; 5 g PEG mixed into 100 ml Leibovitz 15)
- L15+7.6% trehalose:
-
Leibovitz 15 supplemented with 7.6 % (v/v) trehalose
References
Aoki T, Koizumi T, Kobayashi Y, Yasuda D, Izumida Y, Jin Z et al (2005) A novel method of cryopreservation of rat and human hepatocytes using an encapsulation technique and possible use for cell transplantation. Cell Transplant 14:609–620
Campbell LH, Brockbank KG (2012) Culturing with trehalose produces viable endothelial cells after cryopreservation. Cryobiology 64:240–244
Dutheil D, Rioja-Pastor I, Tallineau C, Goujon JM, Hauet T, Mauco G, Petit-Paris I (2006) Protective effect of PEG 35,000 Da on renal cells: paradoxical activation of the JNK signaling pathway during cold storage American Journal of Transplantation: official journal of the American Society of Transplantation and the American Society of Transplant Surgeons 6:1529–1540
Fox IJ, Roy-Chowdhury J (2004) Hepatocyte transplantation. J Hepatol 40:878–886
Gramignoli R, Dorko K, Tahan, Skvorak KJ, Ellis E, Jorns C et al (2014) Hypothermic storage of human hepatocytes for transplantation. Cell Transplant 23:1143–1151
Hang H, Shi X, Gu G, Wu Y, Gu J, Ding Y (2010) In vitro analysis of cryopreserved alginate-poly-l-lysine-alginate-microencapsulated human hepatocytes. Liver Int Off J Int Assoc Study Liver 30:611–622
Inuo H, Eguchi S, Yanaga K, Hamada T, Yamanouchi K, Okudaira S, Kanematsu T (2007) Protective effects of a hibernation-inducer on hepatocyte injury induced by hypothermic preservation. J Hepato-biliary-Pancreat Surg 14:509–513
Janssen H, Janssen PH, Broelsch CE (2003) Celsior solution compared with University of Wisconsin solution (UW) and histidine-tryptophan-ketoglutarate solution (HTK) in the protection of human hepatocytes against ischemia-reperfusion injury transplant international. Off J Eur Soc Organ Transplant 16:515–522
Katenz E, Vondran FW, Schwartlander R, Pless G, Gong X, Cheng X et al (2007) Cryopreservation of primary human hepatocytes: the benefit of trehalose as an additional cryoprotective agent liver transplantation. Off Publ Am Assoc Study Liver Dis Int Liver Transplant Soc 13:38–45
Khan AA, Capoor AK, Parveen N, Naseem S, Venkatesan VT, Habibullah CM (2002) In vitro studies on a bioreactor module containing encapsulated goat hepatocytes for the development of bioartificial liver Indian Journal of gastroenterology. Off J Indian Soc Gastroenterol 21:55–58
Mack JE, Kerr JA, Vreugdenhil PK, Belzer FO, Southard JH (1991) Effect of polyethylene glycol on lipid peroxidation in cold-stored rat hepatocytes. Cryobiology 28:1–7
Meng Q (2003) Hypothermic preservation of hepatocytes. Biotechnol Prog 19:1118–1127
Ostrowska A, Gu K, Bode DC, Van Buskirk RG (2009) Hypothermic storage of isolated human hepatocytes: a comparison between University of Wisconsin solution and a hypothermosol platform. Arch Toxicol 83:493–502
Poullain MG, Fautrel A, Guyomard C, Chesne C, Grislain L, Guillouzo A (1992) Viability and primary culture of rat hepatocytes after hypothermic preservation: the superiority of the Leibovitz medium over the University of Wisconsin solution for cold storage. Hepatology 15:97–106
Serrar H, El-Kadi A, Du Souich P, Haddad P (1999) Cytochrome P-450 content and activity after cold storage of rat hepatocytes in University of Wisconsin and sodium-lactobionate-sucrose solutions Liver Transplantation and Surgery: Official Publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society 5:119–125
Terry C, Dhawan A, Mitry RR, Lehec SC, Hughes RD (2006) Preincubation of rat and human hepatocytes with cytoprotectants prior to cryopreservation can improve viability and function upon thawing liver transplantation. Off Publ Am Assoc Study Liver Dis Int Liver Transplant Soc 12:165–177
Uhlmann D, Armann B, Ludwig S, Escher E, Pietsch UC, Tannapfel A, Teupser D et al (2002) Comparison of Celsior and UW solution in experimental pancreas preservation. J Surg Res 105:173–180
Valuckaite V, Zaborina O, Long J, Hauer-Jensen M, Wang J, Holbrook C, Zaborin A, Drabik K et al (2009) Oral PEG 15-20 protects the intestine against radiation: role of lipid rafts. Am J Physiol Gastrointest Liver Physiol 297:G1041–1052
Supporting information
Supplementary Table—Primers used in the real-time quantitative PCR analyses.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors Juan Lu and Yanhong Zhang have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lu, J., Zhang, Y., Zhu, D. et al. Improvement of short-term hypothermic preservation of microencapsulated hepatocytes. Biotechnol Lett 38, 909–917 (2016). https://doi.org/10.1007/s10529-016-2063-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10529-016-2063-x