Abstract
MiR-133b is considered to be lowly expressed in osteoporosis patients. This study aimed to probe the role and in-depth mechanism of miR-133b in modulating osteoblast biological behavior and differentiation. The differential expressions of miR-133b and GNB4 in patients with osteoporosis and healthy control were analyzed based on the GEO database. Osteoblastic differentiation of hFOB 1.19 cells was induced in the culture medium containing 10 mM β-glycerophosphate, 50 nm dexamethasone, and 100 μg/ml ascorbic acid. The level of GNB4 was detected using quantitative real-time PCR (qRT-PCR) and Western blot. Cell viability and apoptosis were measured by Cell Counting Kit-8 (CCK-8) and flow cytometry assays, respectively. Western blot was also utilized to measure the levels of osteoblast-related proteins, including ALP, Runx2, Osterix, and OPN. GNB4 was identified and confirmed as a downstream target gene of miR-133b. The expression of miR-133b was declined while the expression of GNB4 was increased in osteoporosis patients. Importantly, up-regulation of miR-133b caused the increase of cell viability and the decrease of apoptosis, which could be blocked by overexpression of GNB4. Also, up-regulation of miR-133b promoted osteoblasts differentiation, as shown by the increase in the expression of ALP, Runx2, Osterix, and OPN. Similarly, this promoting impact resulted from miR-133b overexpression can be reversed via up-regulation of GNB4. These findings revealed that miR-133b can promote the viability and differentiation of osteoblasts by targeting GNB4, hoping to lay a feasible theoretical foundation for the clinical treatment of osteoporosis.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is one of the most common metabolic osteopathy syndromes in clinic, and it is one of the main causes of fracture (Wong et al. 2016; Cauley 2017). The formation, apoptosis rate, and maintenance of osteoblasts and osteoclasts play the key role in bone homeostasis (Chen et al. 2018). If there are problems in the proliferation, differentiation, and apoptosis of osteoblasts and osteoclasts, which destroy the balance between bone formation and bone absorption, it will lead to abnormal bone metabolism and osteoporosis (Sandhu and Hampson 2011; Kiyoi 2018). Therefore, the balance between bone formation and bone resorption may be one of the important targets in the prophylaxis and therapy of osteoporosis (Abdallah and Kassem 2012). Osteoblast differentiation is the key process of bone formation (Wang et al. 2016), so the study of osteoblast differentiation is helpful to clarify the pathogenesis of osteoporosis. Finding effective biomarkers involved in osteoblast differentiation can effectively prevent and reverse the pathological process of osteoporosis.
miRNAs are small non-coding RNAs that act as negative regulators of genes and perform biological functions, such as cell proliferation, apoptosis, viability, and differentiation (Bartel 2004). Recent researches have presented that miRNAs can regulate bone formation at various stages, which is related to osteoporosis and other bone diseases (Chen et al. 2015; Papaioannou et al. 2014). Interestingly, some miRNAs (such as miR-143, miR-378, miR-26a, miR-29b, etc.) have been shown to participate in the process of regulating stem cell adipogenesis or osteoblast differentiation (Wang et al. 2020; Kahai et al. 2009; Luzi et al. 2008; Zeng et al. 2019). MiR-133b, a member of miR-133 family, was increased in differentiated myoblasts and promoted the proliferation of myoblasts (Chen et al. 2006). MiR-133b has been found to be low expressed in osteoporotic patients (Chen et al. 2018) and is related to postmenopausal estrogen deficiency (Lv et al. 2015). Furthermore, miR-133 directly targets Runx2 (a transcription factor essential for bone formation) and regulates its expression (Lv et al. 2015). However, whether miR-133b has biological function in osteoblast phenotype is still unknown.
Herein, we purposed to explore the function of miR-133b in the modulation of osteoblast viability, apoptosis, and differentiation, as well as its possible mechanism, so as to provide a reliable molecular basis for the possibility of miR-133b as a feasible biomarker for the prophylaxis and therapy of osteoporosis.
Materials and Methods
Bioinformatics Analysis
In the present work, we downloaded data from the Gene Expression Omnibus (GEO, www.ncbi.nlm.nih.gov/geo) database (GSE60230) to analyze the differential expression of miR-133b. The dataset included serum samples from 7 patients with femoral neck osteoporotic fracture and 7 age-matched controls. MiRNA differences between the two groups were analyzed using R program limma package with |logFC| > 1 and FDR < 0.05. Consistently, the differential expression of GNB4 was analyzed based on the data of peripheral blood of 105 postmenopausal osteoporosis samples and 7 healthy controls that downloaded from the GEO database (GSE56116 and GSE35958) using R program limma package with |logFC| > 1 and FDR < 0.05.
miRBase (http://www.mirbase.org/), a target gene prediction and analysis website, was used to predict the downstream targets of miR-133b. Herein, I used the prediction algorithms of starBase.
Cell Culture, Differentiation and Transfection
Human osteoblasts hFOB 1.19 was purchased from Shanghai Institute of life sciences, Chinese Academy of Sciences and cultured in Dulbecco's Modified Eagle's medium/Ham's F12 (DMEM/F12) supplement with 10% fetal bovine serum (FBS; Sigma-Aldrich, MO, USA), penicillin (100 U/ml), and streptomycin (100 g/ml) at 37 °C with 5% CO2. Osteoblastic differentiation was induced in the culture medium containing 50 nm dexamethasone, 10 mM β-glycerophosphate, and 100 μg/ml ascorbic acid. The culture medium was changed every 3 days.
MiR-133b mimic/inhibitor and corresponding negative control (NC), as well as si-GNB4 (3′-GTCGAATACAAATGCGAACAA-5′) and si-con (3′-UUCUUCGAAGGUGUCACGUTT-5′) were all synthesized by genepharma Co. (Shanghai, China). Transient transfection of miRNA mimics, inhibitors, or siRNAs (100 nM) was performed in 6-well plates using Lipofectamine 3000 regent (Invitrogen) as directed by manufacturer.
qRT-PCR
Total RNA was exacted from osteoblasts with Trizol kit (Invitrogen), and then RNA purity and concentration were detected with NanoDrop2000 (Thermo). Subsequently, cDNA was synthesized by the Reverse Transcription Kit (TOYOBO, Tokyo, Japan) based on the manufacturer’ manual. qRT-PCR was performed to measure the expression of GNB4 using TB Green Premix Ex Taq (TaKaRa, Japan). GAPDH was utilized as the internal reference gene of GNB4. 2−△△Ct method was performed to quantify the relative level of GNB4. PCR primers (Shanghai Sangon Biotech Co. Ltd) were synthesized and presented as follows (5′–3′):
GNB4: F: CTGGTGCTTGTGATGCCTCTTC; R: AGAGCCAGTGGCGAAGGCATAT
GAPDH: F: GTCTCCTCTGACTTCAACAGCG; R: ACCACCCTGTTGCTGTAGCCAA
Cell Viability
Transfected cells were inoculated into 96-well plates (103 cells/well) and cultured at 37 °C. Cell viability was detected at 0 h, 24 h, 48 h, and 72 h with CCK-8 kit (CT-K; Shanghai Yi Sheng Biotechnology) following the manufacturer's standard. Of note, 10 μl of CCK-8 solution was added into each well at the indicated time points. After incubation for 1.5 h, a microplate reader was utilized to measure the OD value at 450 nm.
Cell Apoptosis
Cell apoptosis was measured by flow cytometry assay kit (Canto, BD Biosciences). Transfected cells were stained with Annexin V conjugated to fluorescein isothiocyanate (FITC) and propidium iodide (PI) as directed by manufacturer. The flow results were analyzed using the Flowjo software.
Western Blotting
Transfected cells were lysed to extract proteins using radio-immunoprecipitation assay (RIPA) lysate (with protease inhibitor). About 20 μg of above proteins was detached by SDS–polyacrylamide gel electrophoresis, followed by transferring onto polyvinylidene difluoride (PVDF) membranes (Merck Millipore Ltd). Hereafter, the PVDF membranes were blocked with skimmed milk powder for 1 h, which then incubated at 4 °C with primary antibodies against the following proteins: GNB4 (1:1000, Abcam), ALP (1:1000, Abcam), RUNX2 (1:1000, Abcam), Osterix (1:1000, Abcam), OPN (1:1000, Abcam), and GAPDH (1:10,000, Abcam). Next day, membranes were incubated with the HRP secondary antibodies (Abcam) for 1.5 h at room temperature. The enhanced chemiluminescence system was exploited to analyze the bands.
Luciferase Reporter Assay
The wild-type and mutant-type miR-133b binding sites in the 3′UTR of GNB4 were synthesized and cloned into a pmirGLO luciferase vector (Shanghai Genechem Co., Ltd., Shanghai, China). Then, cells were co-transfected with GNB4 3′ UTR construct (100 ng) and miR-133b mimics/inhibitors or NC (50 nM) using Lipofectamine 3000 (Invitrogen). After transfection for 48 h, the luciferase activity was assessed with the Dual-Luciferase Reporter Assay System (Promega, USA).
Statistical Analysis
All experiments were repeated three times. Experimental data were analyzed using SPSS 22.0 software (IBM Corp., Armonk, NY, USA) and represented as mean ± SD. Statistical comparison was conducted using the Student's t test (two groups) and one-way analysis of variance with Bonferroni correction post hoc test (multiple groups). P < 0.05 was considered statistically significant.
Results
MiR-133b was Down-Regulated in Osteoporosis Patients and Enhanced the Viability of hFOB 1.19 Cells
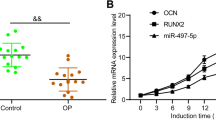
Based on GEO database (GSE60230), the DEGs between the femoral neck osteoporotic fracture and 7 age-matched controls were screened. The results showed that there were significant differences in the three miRNAs between the osteoporosis group and the non-osteoporosis group (P < 0.05), of which 2 were up-regulated and 1 were down-regulated. The down-regulated miR-133b was selected for follow-up study (Fig. 1a, Table 1). Then, we further probed the potential function of miR-133b in osteoblasts phenotype. CCK-8 assay was carried out to evaluate the impact of miR-133b on the viability of osteoblasts. As presented in Fig. 1b, compared with NC group, mimic group and inhibitor group displayed opposite viability trends that the OD value was markedly increased in miR-133b up-regulated cells whereas obviously declined in miR-133b lacked cells. Our data revealed that miR-133b contributed to promoting the viability of osteoblasts.
MiR-133b was expressed at low levels in osteoporosis patients and contributed to promoting osteoblasts hFOB 1.19 viability. a The differential expression of miR-133b in osteoporosis patients (n = 7) and healthy control (n = 7) were analyzed based on the GEO database (GSE60230). P < 0.05. b The impact of miR-133b mimic/inhibitor on osteoblasts hFOB 1.19 viability was detected using CCK-8 assay. **P < 0.01 vs. NC group
GNB4 is a Target Gene of miR-133b
In view of the function of miR-133b in the viability of osteoblasts, we further in depth studied its mechanism. The miR-133b downstream gene was predicted using miRBase website. As presented in Fig. 2a, GNB4 has a potential binding site for miR-133b in the 3′-UTR region, and it may be a direct target of miR-133b (Table 2). Then, this prediction was confirmed using dual-luciferase reporter assay. As expected, miR-133b mimic can markedly decline the luciferase activity of GNB4-WT, but not GNB4-MUT (Fig. 2b). Also, we downloaded the data from GEO database with the accession number GSE56116 and analyzed differential expression of GNB4 in osteoporosis tissues and normal. The results indicated that the level of GNB4 was obviously enhanced in osteoporosis tissues, in comparison with normal tissues (Fig. 2c). Moreover, the impacts of miR-133b on GNB4 expression in hFOB 1.19 cells were measured using qRT-PCR and western blot. The expression of GNB4 in the cells transfected with si-GNB4 was significantly decreased, which indicated that si-GNB4 was successfully transfected (Fig. 2d). It can be seen from Fig. 2e–h that the mRNA and protein levels of GNB4 were clearly elevated by down-regulation of miR-133b while were markedly declined by up-regulation of miR-133b. Our findings in this section indicated that miR-133b directly targets GNB4 and negatively regulates its expression.
GNB4 was a direct target gene of miR-133b. a GNB4 has a potential binding site for miR-133b in the 3′-UTR region, which was predicted by miRBase website. b The luciferase activity of WT-GNB4 and MUT-GNB4 in cells transfected with miR-133b mimic/inhibitor was assessed by Dual-Luciferase Reporter Assay. c The differential expression of GNB4 in osteoporosis patients (n = 10) and healthy control (n = 3) were analyzed based on the GEO database (GSE56116). P < 0.05. qRT-PCR and western blot were carried out to measure the mRNA and protein levels of GNB4 in transfected osteoblasts. Wherein, d, e osteoblasts transfected with miR-133b mimic, pcDNA3.1-GNB4, and miR-133b mimic + pcDNA3.1-GNB4. **P < 0.01 vs. control group. ##P < 0.01 vs. miR-133b mimic group. ^^P < 0.01 vs. pcDNA3.1-GNB4 group. f–g Osteoblasts transfected with miR-133b inhibitor, si-GNB4, and miR-133b inhibitor + si-GNB4. **P < 0.01 vs. control group. ##P < 0.01 vs. miR-133b inhibitor group. ^^P < 0.01 vs.si-GNB4 group
GNB4 may be a Negative Target of miR-133b Participated in the Viability and Apoptosis of Osteoblast
Although miR-133b has been found to regulate GNB4 expression, the function of miR-133b/GNB4 axis in biological behaviors of osteoblast needs further assessment. The impacts of miR-133b/GNB4 axis on viability and apoptosis were assessed using CCK-8 and flow cytometry assays. The results obtained from CCK-8 are presented in Fig. 3a and b. Up-regulation of miR-133b led to a notable increase in viability of osteoblast, while overexpression of GNB4 presented an opposite viability trend. Of note, up-regulation of GNB4 can block the facilitating impact of the miR-133b mimic on osteoblast viability. On the other hand, the osteoblast viability showed a significant reduction when osteoblast treated with miR-133b inhibitor, while the osteoblasts treated with si-GNB4 increased the viability of osteoblasts significantly. Also, after co-transfection of miR-133b inhibitor and si-GNB4, the osteoblast viability was markedly increased than miR-133b inhibitor group.
The impact of miR-133b/GNB4 on phenotype of osteoblasts hFOB 1.19. CCK-8 and flow cytometry assays were performed to measure the impact of miR-133b/GNB4 axis on cell viability and apoptosis. Wherein, a, c osteoblasts transfected with miR-133b mimic, pcDNA3.1-GNB4, and miR-133b mimic + pcDNA3.1-GNB4. **P < 0.01 vs. control group. ##P < 0.01 vs. miR-133b mimic group. ^^P < 0.01 vs.pcDNA3.1-GNB4 group. b, d osteoblasts transfected miR-133b inhibitor, si-GNB4, and miR-133b inhibitor + si-GNB4. **P < 0.01 vs. control group. ##P < 0.01 vs. miR-133b inhibitor group. ^^P < 0.01 vs.si-GNB4 group
Moreover, the flow cytometry assay (Fig. 3c, d) presented an obvious reduction of osteoblast apoptosis in miR-133b up-regulated cells and GNB4 down-regulated cells, respectively. The reverse trend was found in the cells that inhibited miR-133b or overexpressed GNB4. Also, the impact of miR-133b on osteoblast apoptosis was reversed via GNB4. These data illustrated that miR-133b/GNB4 axis contributed to the biological behaviors of osteoblast.
MiR-133b Promoted Osteogenic Differentiation Via Targeting GNB4
The differentiation of osteoblasts is one of the important ways of bone formation (Wang et al. 2016), so we further confirm whether miR-133b/GNB4 axis was involved in osteogenic differentiation. We up-regulated or down-regulated miR-133b and GNB4 in the differentiated hFOB 1.19 cells, and then detected the levels of osteogenic differentiation markers using Western blot, including ALP, Runx2, Osterix, OPN. The protein levels of ALP, Runx2, Osterix, and OPN were enhanced via up-regulating miR-133b while were declined by lacking GNB4. Importantly, when differentiated hFOB 1.19 cells co-transfected with miR-133b mimic and pcDNA3.1-GNB4, the differentiation promoting impact of miR-133b mimic was reversed (Fig. 4a, b). Meanwhile, miR-133b inhibitor can obviously decrease the expression of ALP, Runx2, Osterix, and OPN, but knockdown of GNB4 presented an opposite results. As expected, knockdown of GNB4 can rescue the differentiation inhibition resulted from miR-133b inhibitor (Fig. 4c, d). Hence, our data indicated that miR-133b/GNB4 axis can regulate osteogenic differentiation, which may be a novel target of osteoporosis therapy.
The impact of miR-133b/GNB4 on differentiation of osteoblasts hFOB 1.19. Osteoblastic differentiation was induced in the culture medium containing 50 nm dexamethasone, 10 mM β-glycerophosphate, and 100 μg/ml ascorbic acid. Then, differentiated cells were used to perform subsequent experiments. Western blot was performed to measure the levels of osteogenic markers ALP, Osterix, OPN, and Runx2. Wherein, a, b osteoblasts transfected with miR-133b mimic, pcDNA3.1-GNB4, and miR-133b mimic + pcDNA3.1-GNB4. **P < 0.01 vs. control group. ##P < 0.01 vs. miR-133b mimic group. ^^P < 0.01 vs.pcDNA3.1-GNB4 group. c, d Osteoblasts transfected miR-133b inhibitor, si-GNB4, and miR-133b inhibitor + si-GNB4. **P < 0.01 vs. control group. ##P < 0.01 vs. miR-133b inhibitor group. ^^P < 0.01 vs. si-GNB4 group
Discussion
In this work, we confirmed that the level of miR-133b declined markedly in osteoporosis patients. Importantly, the osteoblast viability was markedly increased in miR-133b up-regulated cells whereas obviously declined in miR-133b lacked cells. Additionally, GNB4 is considered as the downstream target of miR-133b, which eliminates the miR-133b-mediated increase in osteoblast viability and decrease in osteoblast apoptosis, as well as the differentiation promotion impact of miR-133b.
MiR-133 is one of the most studied and most characteristic muscle-specific miRNAs, which is necessary for skeletal muscle development and normal function (Yu et al. 2014). As an important regulator of bone-related genes, miR-133b is also a mediator of vascular calcification (Panizo et al. 2016). Moreover, miR-133b expression was decreased in MC3T3 osteogenic precursor cells of mouse calvaria (Panizo et al. 2016). Li et al. found that miR-133 and miR-135 showed synergistic effect in the bone formation (Li et al. 2008). These reports indicate that miR-133b is a key mechanism for osteoblast differentiation. Furthermore, miR-133b is also down-regulated as a cancer suppressive factor in multiple cancers, e.g., colorectal cancer (Lv et al. 2019), ovarian cancer (Yang et al. 2017), breast cancer (Wang et al. 2018), etc. The multimolecular function of miR-133 makes it a valuable therapeutic gene in miRNA gene therapy (Yu et al. 2014). In this work, the function of miR-133 in the biological behaviors of osteoblasts was studied for the first time. Our results indicated that up-regulation of miR-133b enhanced viability and reduced apoptosis of osteoblasts, whereas the reverse impact occurred in miR-133b lacked cells. Since enhancing the viability of osteoblasts is one of the ways to promote bone formation, these results indicated that miR-133b can promote bone formation, thereby reducing the occurrence of osteoporosis.
GNB4, an important component of heterotrimer G protein, is the key molecule of membrane receptor signaling to intracellular effectors in GPCR pathway (Oldham and Hamm 2008). GPCR signaling pathway has been widely studied, which can regulate cell growth and proliferation through many ways (Wiser and Jan 2010; Exton 1996; Sunahara et al. 1996). To date, the research on GNB4 in Charcot-Marie-Tooth disease is more in depth that GNB4 mutation is a cause of Charcot-Marie-Tooth (Liu and Zhang 2014; Soong et al. 2013). Moreover, GNB4 plays a key role in the insulin signaling pathway, and its activation leads to the decrease of insulin level and the increase of liver glucose output (Saddala et al. 2018; Benjafield et al. 2001). However, the research of GNB4 in osteoporosis is still blank. Our findings revealed that GNB4 can inhibit the viability but promote the apoptosis of osteoblasts at the cellular level. Importantly, miR-133b-mediated impacts on the osteoblasts phenotype can be reversed by GNB4.
To our knowledge, mature osteogenic markers include ALP, Osterix, OPN, and Runx2, which are related to osteogenesis and widely used to indicate osteogenic differentiation (Bandow et al. 2010). Runx2 is a key transcription factor in osteogenic differentiation (Pang et al. 2018), and the peak of ALP activity indicates osteogenic differentiation (Cao et al. 2016). In this present work, we revealed that up-regulation of miR-133b can elevate the expression of ALP, Osterix, OPN, and Runx2, and overexpression of GNB4 presented an opposite trend. This suggested that miR-133b can promote osteogenic differentiation. It is worth noting that the differentiation promoting effect result from overexpression of miR-133b can be blocked by up-regulation of GNB4. These findings indicated that miR-133b/GNB4 axis contributed to the process of osteogenic differentiation.
In summing, to the best of our knowledge, this work is the first to elucidate the mechanism of miR-133b regulating osteoblast viability, apoptosis, and differentiation. MiR-133b can enhance osteoblast viability and promote osteoblast differentiation by targeting GNB4. These findings provide new insights for the impact of miR-133b on osteoblast differentiation and bone formation, and lay a theoretical foundation for the treatment of osteoporosis. However, the relevant in vivo experiments and clinical effects need to be further study.
References
Abdallah BM, Kassem M (2012) New factors controlling the balance between osteoblastogenesis and adipogenesis. Bone 50:540–545
Bandow K, Maeda A, Kakimoto K, Kusuyama J, Shamoto M, Ohnishi T, Matsuguchi T (2010) Molecular mechanisms of the inhibitory effect of lipopolysaccharide (LPS) on osteoblast differentiation. Biochem Biophys Res Commun 402:755–761
Bartel DP (2004) MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116:281–297
Benjafield AV, Lin RC, Dalziel B, Gosby AK, Caterson ID, Morris BJ (2001) G-protein beta3 subunit gene splice variant in obesity and overweight. Int J Obes Relat Metab Disord 25:777–780
Cao FY, Fan JX, Long Y, Zeng X, Zhang XZ (2016) A smart fluorescence nanoprobe for the detection of cellular alkaline phosphatase activity and early osteogenic differentiation. Nanomedicine 12:1313–1322
Cauley JA (2017) Osteoporosis: fracture epidemiology update 2016. Curr Opin Rheumatol 29:150–156
Chen JF, Mandel EM, Thomson JM, Wu Q, Callis TE, Hammond SM, Conlon FL, Wang DZ (2006) The role of microRNA-1 and microRNA-133 in skeletal muscle proliferation and differentiation. Nat Genet. 38:228–233
Chen J, Qiu M, Dou C, Cao Z, Dong S (2015) MicroRNAs in bone balance and osteoporosis. Drug Dev Res 76:235–245
Chen R, Liao X, Chen F, Wang B, Huang J, Jian G, Huang Z, Yin G, Liu H, Jin D (2018) Circulating microRNAs, miR-10b-5p, miR-328-3p, miR-100 and let-7, are associated with osteoblast differentiation in osteoporosis. Int J Clin Exp Pathol 11:1383–1390
Chen X, Wang Z, Duan N, Zhu G, Schwarz EM, Xie C (2018) Osteoblast-osteoclast interactions. Connect Tissue Res. 59:99–107
Exton JH (1996) Regulation of phosphoinositide phospholipases by hormones, neurotransmitters, and other agonists linked to G proteins. Annu Rev Pharmacol Toxicol 36:481–509
Kahai S, Lee SC, Lee DY, Yang J, Li M, Wang CH, Jiang Z, Zhang Y, Peng C, Yang BB (2009) MicroRNA miR-378 regulates nephronectin expression modulating osteoblast differentiation by targeting GalNT-7. PLoS ONE 4:e7535
Kiyoi T (2018) Bone resorption activity in mature osteoclasts. Methods Mol Biol 1868:215–222
Li Z, Hassan MQ, Volinia S, Van Wijnen AJ, Stein JL, Croce CM, Lian JB, Stein GS (2008) A microRNA signature for a BMP2-induced osteoblast lineage commitment program. Proc Natl Acad Sci USA 105:13906–13911
Liu L, Zhang R (2014) Intermediate Charcot-Marie-Tooth disease. Neurosci Bull 30:999–1009
Luzi E, Marini F, Sala SC, Tognarini I, Galli G, Brandi ML (2008) Osteogenic differentiation of human adipose tissue-derived stem cells is modulated by the miR-26a targeting of the SMAD1 transcription factor. J Bone Miner Res 23:287–295
Lv H, Sun Y, Zhang Y (2015) MiR-133 is involved in estrogen deficiency-induced osteoporosis through modulating osteogenic differentiation of mesenchymal stem cells. Med Sci Monit 21:1527–1534
Lv L, Li Q, Chen S, Zhang X, Tao X, Tang X, Wang S, Che G, Yu Y, He L (2019) miR-133b suppresses colorectal cancer cell stemness and chemoresistance by targeting methyltransferase DOT1L. Exp Cell Res 385:111597
Oldham WM, Hamm HE (2008) Heterotrimeric G protein activation by G-protein-coupled receptors. Nat Rev Mol Cell Biol 9:60–71
Pang XG, Cong Y, Bao NR, Li YG, Zhao JN (2018) Quercetin stimulates bone marrow mesenchymal stem cell differentiation through an estrogen receptor-mediated pathway. Biomed Res Int 2018:4178021
Panizo S, Naves-Díaz M, Carrillo-López N, Martínez-Arias L, Fernández-Martín JL, Ruiz-Torres MP, Cannata-Andía JB, Rodríguez I (2016) MicroRNAs 29b, 133b, and 211 regulate vascular smooth muscle calcification mediated by high phosphorus. J Am Soc Nephrol 27:824–834
Papaioannou G, Mirzamohammadi F, Kobayashi T (2014) MicroRNAs involved in bone formation. Cell Mol Life Sci 71:4747–4761
Saddala MS, Lennikov A, Grab DJ, Liu GS, Tang S, Huang H (2018) Proteomics reveals ablation of PlGF increases antioxidant and neuroprotective proteins in the diabetic mouse retina. Sci Rep 8:16728
Sandhu SK, Hampson G (2011) The pathogenesis, diagnosis, investigation and management of osteoporosis. J Clin Pathol 64:1042–1050
Soong BW, Huang YH, Tsai PC, Huang CC, Pan HC, Lu YC, Chien HJ, Liu TT, Chang MH, Lin KP et al (2013) Exome sequencing identifies GNB4 mutations as a cause of dominant intermediate Charcot-Marie-Tooth disease. Am J Hum Genet 92:422–430
Sunahara RK, Dessauer CW, Gilman AG (1996) Complexity and diversity of mammalian adenylyl cyclases. Annu Rev Pharmacol Toxicol 36:461–480
Wang H, Sun Z, Wang Y, Hu Z, Zhou H, Zhang L, Hong B, Zhang S, Cao X (2016) miR-33-5p, a novel mechano-sensitive microRNA promotes osteoblast differentiation by targeting Hmga2. Sci Rep 6:23170
Wang QY, Zhou CX, Zhan MN, Tang J, Wang CL, Ma CN, He M, Chen GQ, He JR, Zhao Q (2018) MiR-133b targets Sox9 to control pathogenesis and metastasis of breast cancer. Cell Death Dis 9:752
Wang R, Zhang H, Ding W, Fan Z, Ji B, Ding C, Ji F, Tang H (2020) miR-143 promotes angiogenesis and osteoblast differentiation by targeting HDAC7. Cell Death Dis 11:179
Wiser O, Jan LY (2010) G-protein regulation of channels. Springer, New York
Wong SK, Chin KY, Suhaimi FH, Ahmad F, Ima-Nirwana S (2016) The relationship between metabolic syndrome and osteoporosis: a review. Nutrients 8:1
Yang L, Hou J, Cui XH, Suo LN, Lv YW (2017) MiR-133b regulates the expression of CTGF in epithelial-mesenchymal transition of ovarian cancer. Eur Rev Med Pharmacol Sci 21:5602–5609
Yu H, Lu Y, Li Z, Wang Q (2014) microRNA-133: expression, function and therapeutic potential in muscle diseases and cancer. Curr Drug Targets 15:817–828
Zeng Q, Wang Y, Gao J, Yan Z, Li Z, Zou X, Li Y, Wang J, Guo Y (2019) miR-29b-3p regulated osteoblast differentiation via regulating IGF-1 secretion of mechanically stimulated osteocytes. Cell Mol Biol Lett 24:11
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, J., Gao, Z. & Gao, P. MiR-133b Modulates the Osteoblast Differentiation to Prevent Osteoporosis Via Targeting GNB4. Biochem Genet 59, 1146–1157 (2021). https://doi.org/10.1007/s10528-021-10048-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10528-021-10048-9