Abstract
Ferulic acid (FA) is a polyphenol very abundant in vegetables and maize bran. Several lines of evidence have shown that FA acts as a potent antioxidant in vitro, due to its ability to scavenge free radicals and induce a robust cell stress response through the up-regulation of cytoprotective enzymes such as heme oxygenase-1, heat shock protein 70, extracellular signal-regulated kinase 1/2 and Akt. Furthermore, FA inhibited the expression and/or activity of cytotoxic enzymes including inducible nitric oxide synthase, caspases and cyclooxygenase-2. On this basis, FA has been proposed for the treatment of several age-related diseases such as neurodegenerative disorders, cardiovascular diseases, diabetes and cancer. However, although the great abundance of in vitro data, the real efficacy of FA in humans has not been demonstrated so far. New efforts and resources should be transferred to clinical research for the complete evaluation of the therapeutic potential of FA in chronic diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several years ago artichoke-derived polyphenols, such as 1,5-dicaffeiylquinic acid as well as the caffeic acid mono-methylester [also known as ferulic acid (FA)] and di-methylester were extensively studied by Preziosi et al. (1957), Preziosi and Loscalzo (1957a, b,1958) for their coleretic, hypolipidemic and diuretic functions. Recently, polyphenols have been proposed as novel agents in the prevention of free radical-related diseases such as neurodegenerative disorders, cancer, acute and chronic inflammation and aging (see below). Polyphenols are widely distributed in the plant kingdom, and are integral part of diet, with significant amounts being reported in vegetables, fruit and beverages (Clifford 1999; D’Archivio et al. 2007).
FA [(E)-3-(4-hydroxy-3-methoxy-phenyl)prop-2-enoic acid)] (Fig. 1) is a common polyphenolic compound most abundant in vegetables, especially artichokes, eggplants (~90% of total polyphenols) and in maize bran (~3.1% of total polyphenol content) (D’Archivio et al. 2007; Rechner et al. 2001a, b; Saulnier et al. 1995). Moreover, FA is an effective component of Chinese medicinal herbs such as Angelica sinensis, Cimicifuga heracleifolia and Lignsticum chuangxiong (Ou and Kwok 2004). During the last decade, scientists focused their attention on FA especially for its direct antioxidant property, even if this latter is not the only interesting aspect of this molecule.
In this review the pharmacological profile of FA has been summarized. In particular, the possible use of FA in the therapy of free radical-related syndromes such as neurodegenerative disorders, cancer, cardiovascular and skin diseases has been discussed. Finally, the potential effects deriving from the concomitant administration of FA with common drugs have been analyzed.
Chemistry of FA
Polyphenols are a group of phenolic compounds with several hydroxyl groups on the aromatic ring(s) of the molecules (D’Archivio et al. 2007). They are ubiquitous in the plant kingdom and commonly divided into five groups: flavonoids (flavonols/flavones, flavanones, flavan-3-ols, isoflavones and anthocyanins), phenolic acids (hydroxybenzoic acids, hydroxycinnammic acids), phenolic alcohols, stilbenes and lignans (Rechner et al. 2001a, b; D’Archivio et al. 2007). FA belongs to the phenolic acid group. A key intermediate in the polyphenol biosynthetic pathway is hydroxycinnamic acid, which derives from shikimic acid, a common precursor of many alkaloids, aromatic amino acids and indole derivatives (Rechner et al. 2001). Shikhimic acid is transformed to phenylalanine in the so called “shikhimic pathway” and then converted by an ammonia lyase to trans-cinnamic acid. The hydroxylation at the 4-position of the aromatic ring transforms trans-cinnamic acid to 4-hydroxycinnamic acid or p-coumaric acid. The hydroxylation of p-coumaric acid at the 3-position of aromatic ring yields caffeic acid and further O-methylation leads to FA (Rechner et al. 2001a, b) (Fig. 2). FA has two isomers: the cis form is a yellow oily liquid, whereas the trans form is crystalline (Ou and Kwok 2004). In plant cell wall, FA is present as monomer and dimer. Both of them are covalently conjugated through ester-linkage with mono-, di-, and poly-saccharides [5-O-feruloyl-L-arabinofuranose (FAA) and 5-O-feruloyl-arabinoxylane (FAXn) are the most common forms of FA in cereals], glycoproteins, polyamines, lignin and the hydroxy fatty acids suberin and cutin (Bourne and Rice-Evans 1998; Clifford 1999; Ou and Kwok 2004; Saulnier et al. 1994) (Fig. 3).
The synthetic pathway leading to FA. “Shikimic pathway” leads to the biosynthesis of most plant phenolics and it is present also in fungi, bacteria but is not found in animals. Through this way shikimic acid was converted by shikimate kinase (1) to shikimate-3-phospate which than leads to the formation of 5-O-(1-carboxyvinyl)-3-phosphoshikimate (PS) by the action of 5-enolpyruvilshikimate-3-phosphate (EPSP) synthase (2) that utilize phosphoenolpyruvate (PEP) like substrate. PS is than converted by chorismate synthase (3) to chorismate that is a key substrate in this way. Chorismate is transformed in turn in prephenate by chorismate mutase (4) and than prephenate by the action of prephenate dehydratase (5) yields phenylpyruvate. Phenylpyruvate is converted to l-phenylalanine by an aminotransferase (6). Phenylalanine by an ammonia-lyase (7) is transformed in trans-cinnamic acid. The hydroxylation at the 4-position of the aromatic ring by the action of cinnamic acid 4-hydroxylase (8) transforms trans-cinnamic acid to 4-hydroxycinnamic acid or p-coumaric acid. The hydroxylation of p-coumaric acid at the 3-position of aromatic ring by p-coumaric acid 3-hydroxylase (9) yields caffeic acid and further O-methylation by the action of caffeic acid O-methyl transferase (10) leads to FA. SAM, S-adenosylmethionine; SAH, S-adenosylhomocysteine
Pharmacokinetics of FA
Humans may consume as much as 80–165 mg FA/meal which correspond to 8–16 μmol/kg of body weight. Since FA is present in food as a conjugated form [e.g. in bran, 95.8% of FA was present in a bound form and only 4.2% on a free form (Rondini et al. 2004)], many studies have been carried out to establish if conjugation modifies FA pharmacokinetic parameters. Both FA and FAA are recovered intact after incubation at strong acidic pH in vitro, a common way to mimic stomach acidic environment (Zhao et al. 2004). However, in situ administration of 8 μmol/kg of body weight of FA or FAA to rats indicated that only the free form undergoes intestinal transit whereas the conjugated form remains unabsorbed (Zhao et al. 2004). The major site for FA absorption is the colon where the polyphenol is released from parent compounds by microbial cinnamoyl esterase (Couteau et al. 2001), xylanase and FA esterase (FAEs) (Kroon et al. 1997) (Fig. 2). Within the colon FA is absorbed mainly by passive diffusion (~90%) and only a small percentage by active transport via the monocarboxylic acid transporter (MCT) (Poquet et al. 2008). The fate of FA upon its absorption has been largely analyzed. In the rat, after oral administration, the peak plasma concentration of FA or its metabolites is reached after 15–30 min (Rondini et al. 2002, 2004; Zhao et al. 2003). FA undergoes a marked first-pass effects which limits its bioavailability. Studies in rodents and humans demonstrated that after oral administration of FA or FAA, the glucuronide (~3–20%) and sulfoglucuronide (~60–90%) metabolites are the more abundant in plasma, whereas only a low percentage of unmodified FA (~9–20%) has been found (Bourne and Rice-Evans 1998; Rondini et al. 2002, 2004; Zhao et al. 2003, 2004). These metabolic changes have been shown to take place in the liver (Silberberg et al. 2006). The presence or absence of the (poly)saccharide moieties significantly affected the plasma concentration of both FA and its main metabolite. In fact, 30 min after the oral administration of FA or FAA (70 μmol/kg of body weight) to rats, the plasma concentration of FA was 2.7 and 0.7 μM, respectively, whereas FA-sulfoglucuronide was 45 and 13.6 μM, respectively (Zhao et al. 2003). FA and its metabolites are excreted mainly through the urine. In the rat, the urinary excretion FA is very rapid and reaches a plateau 1.5 h after the administration (Rondini et al. 2002), whereas in humans it is much slower with a plateau between 7 and 9 h after consumption (Buorne and Rice-Evans 1998). However, the unmodified FA recovered in urine represents only 4–5% of ingested FA and these results are similar in both humans and rodents (Buorne and Rice-Evans 1998; Rondini et al. 2002). As for plasmatic concentration, also urinary excretion is influenced by FA conjugation. After bran consumption, the rate of FA elimination is 15-fold slower than after the intake of the pure molecule (Rondini et al. 2002, 2004) (Fig. 4).
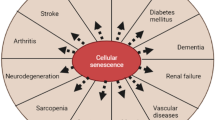
The multiple intracellular targets through which FA has been shown to exert protective effects in vitro. For further information, see text. ACE, angiotensin-converting enzyme; COX-2, cyclooxygenase-2; ERK 1/2, extracellular signal-regulated kinases 1/2; HO-1, heme oxygenase-1; Hsp70, heat shock protein-70; iNOS, inducible Nitric Oxide Synthase; NO, nitric oxide; p38, p38 mitogen-activated protein kinase
Pharmacodynamics of FA
In vitro studies clearly demonstrated that FA has antioxidant and anti-inflammatory properties which has been hypothesized to be very useful in the treatment of several diseases. FA has two main structural motifs that contribute to its direct free radical scavenger activity: (a) the presence of both the 3-methoxy and, more importantly, 4-hydroxyl groups on the benzene ring, which either stabilize the resulted phenoxyl radical intermediate or even terminate the free radical chain reaction; (b) the carboxylic acid group with the adjacent unsaturated carbon-carbon double bond which can further contribute to stabilize the phenoxyl radical intermediate or provides additional attack site for free radicals (Graf 1992).
FA (25–50 μM) significantly attenuated peroxyl radical-induced cell death in hippocampal neuronal cells (Kanski et al. 2002). Moreover, in the same experimental system, FA (250–500 μM) reduced both protein oxidation and lipid peroxidation induced by hydroxyl radicals (Kanski et al. 2002). Similarly, FA (~200 μM) reduced hydrogen peroxide-induced lipid peroxidation in peripheral blood mononuclear cells (PBMCs) and this effect was more evident than that of other polyphenols such as caffeic acid and ellagic acid (Khanduja et al. 2006). Srinivasan et al (2005) have shown that FA (20 mg/kg) prevented liver damage secondary to carbon tetrachloride administration in female rats. In this study, FA significantly decreased both plasma indicators of liver toxicity (transaminases, alkaline phosphatase and γ-glutamyl transferase) as well as tissue markers of lipid and protein oxidation [Thiobarbituric acid-reactive substances (TBARS), lipid hydroperoxides and protein carbonyls] (Srinivasan et al. 2005). Particularly interesting is the interaction between FA and the nitric oxide (NO) synthases (NOS), because NO is involved in the pathogenesis of inflammatory disorders (Calabrese et al. 2007a). Long term administration of FA or FA ethyl ester (FAEE) inhibited the expression of endothelial and inducible NOS (iNOS) in mouse hippocampus (Cho et al. 2005) and in rat cortical neurons (Sultana et al. 2005). Moreover, pre-treatment of rat neuronal cells with 25 μM FAEE for 1 h significantly decreased beta amyloid (Aβ)-stimulated iNOS up-regulation (Sultana et al. 2005). FA and derivatives have been shown to regulate the cell stress response by interacting with the heat shock proteins (Hsp). Hsp are a highly conserved family of stress proteins expressed at low levels under physiological conditions but show dramatically increased expression in response to oxidative or nitrosative stress (Calabrese et al. 2007a; Mancuso et al. 2007b). From a mechanistic point of view, Hsp are chaperone molecules and facilitate the folding of cellular proteins, prevent protein aggregation and target improperly folded proteins to specific degradative pathways (proteasome) (Calabrese et al. 2006a; Mancuso et al. 2007a). Among Hsp a key role has been attributed to heme oxygenase-1 (HO-1 or Hsp32) and Hsp70. HO-1, the inducible form of HO, degrades heme into ferrous iron, carbon monoxide and biliverdin (BV), that is then reduced by biliverdin reductase (BVR) to bilirubin (BR), a molecule which has been shown to counteract oxidative and nitrosative stress (Calabrese et al. 2007a; Mancuso 2004; Mancuso et al. 2006, 2007b). Hsp70 is a functional chaperone and acts by inhibiting key effectors of the apoptotic machinery (Calabrese et al. 2006a). FAEE increased HO-1 expression in many in vitro systems, including rat neurons, gerbil synaptosomes and dermal fibroblasts and this effect was paralleled by a significant cytoprotection against reactive oxygen species (ROS)- and glucose oxidase-related oxidative damage (Calabrese et al. 2008; Joshi et al. 2006; Kanski et al. 2002; Scapagnini et al. 2004). Similarly, FAEE up-regulated Hsp70 in rat cortical neurons and prevented ROS- and Aβ-induced toxicity (Joshi et al. 2006; Sultana et al. 2005). The ability of FA and its congeners to up-regulate both HO-1 and Hsp70, puts this polyphenol in the “hormetin” family arena as the final outcome is to increase the cell stress response and prevent oxidative injury in several tissues (Rattan 2008a,b). Furthermore, the hormetic role of FA may be also important for the maintenance of a good homeostasis not only in case of free radical-related diseases, but also under “physiologic” conditions, such as aging. In fact, during senescence there is an increased production of ROS within the cell and which damage protein, lipid and DNA. Compelling evidence demonstrated that hormetic stimuli, such as mild heat shock, contribute to the maintenance of youth morphology, activate pro-survival systems and increases lifespan (Rattan 2008a).
FA and neurodegenerative disorders
Alzheimer’s disease (AD) or Parkinson’s disease (PD) are neurodegenerative disorders associated with chronic neuroinflammation, and both oxidative and nitrosative stress mainly contribute to the neurotoxic damage. Neurodegenerative disorders are also known as “protein conformational disease” because they are characterized by dysfunctional aggregation of proteins in non-native conformations. In fact, the beta conformation in proteins is particularly susceptible to perturbations in the quality control system and ROS are responsible for the development and/or pathogenetic progression of aging and neurodegenerative diseases (Barnham et al. 2006; Butterfield 2002; Hinault et al. 2006).
AD is characterized by neuronal loss, alterations in neurotransmitter systems and presence of neurofibrillary tangles composed of abnormal tau paired helical filaments. A prominent feature of AD is the formation of senile plaques in selected regions of the brain. An amyloid deposit composed mainly of Aβ occupies the plaque center (Calabrese et al. 2006a; Mancuso et al. 2007b) and induces neuroinflammation by producing ROS and proinflammatory cytokines in astrocytes and microglial cells (Cho et al 2005; Jin et al. 2005, 2006; Sultana et al. 2005; Yan et al. 2001). Neuroinflammation and the following free radical production contribute to the destruction of brain areas, such as amygdala, hippocampus and cortex (Mancuso et al. 2007b).
FA, by its antioxidant and anti-inflammatory properties could exert beneficial effects in AD. Intracerebroventricular (i.c.v.) administration of Aβ (410 pmol) decreased choline acetyltransferase activity (~31%) and caused a marked memory deficits in mice (Yan et al. 2001). Pre-treatment with FA (14–19 mg/kg per os day for 4 weeks) significantly reversed the neuroinflammation [evaluated by using glial fibrillary acidic protein (GFAP) as a marker of gliosis and inteleukin-1β (IL-1β)] in mouse hippocampus secondary to i.c.v. injection of Aβ and ameliorated memory loss as well (Yan et al. 2001). This last effect has been related not only to the pro-inflammatory feature of the cytokine, but also to the ability of IL-1 β to inhibit long-term potentiation in the hippocampus (Katsuki et al. 1990).
Another target for FA is the apoptotic cascade. An important family of proteins that are involved in the regulation of apoptosis are the mammalian mitogen-activated protein kinases (MAPK) that can be subdivided in extracellular signal-regulated kinases (ERK), that regulate cells growth and differentiation (Robinson and Cobb 1997), and stress-activated protein kinases, including Jun N-terminal kinase (JNK) and p38-mitogen-activated protein kinase (p38-MAPK) (Wang et al. 1998). In addition, the serine/threonine kinase Akt/protein kinase B (PKB) (activated via the phosphoinositide 3-kinase (PI3K)-dependent signaling pathway when cells are exposed to growth factor, insulin and certain cytokines), received attention for its anti-apoptotic role (Zhou et al. 2000). I.c.v. injection of Aβ led to a significant increase in activated-p38 MAPK and IL-1β expression in the rat hyppocampal CA1 region and this effect was counteracted by sodium ferulate (50-250 mg/kg/day by intragastric route for 4 weeks) (Jin et al. 2005). In the same paper FA, as above, partly reverted the Aβ-induced inactivation of ERK1/2 as well as increased the activation of Akt/PKB (Jin et al. 2005).
Morover, FA attenuated Aβ-induced caspase activation. In fact, i.c.v. injection of Aβ initiated the processing of inactive procaspase-9 into its active form that was responsible for procaspase-3 and procasapse-7 activation in the rat. In this system, pretreatment with FA (100 and 200 mg/kg body weight intragastric for 3 weeks) inhibited caspase-9, -3, and -7 activation thus contributing to prevents neurotoxicity (Jin et al. 2006).
FA and cancer
Free radicals play a main role in the etiology of cancer (Comporti 1989) and therefore dietary antioxidants have been receiving particular attention as potential inhibitors of uncontrolled cell growth. The anti-carcinogenic activity of FA has been shown to be related to its ability to scavenge ROS and stimulate cytoprotective enzymes. By so doing, FA reduce lipid peroxidation, DNA single-strand breakage, inactivation of certain proteins, and disruption of biological membranes (Hirose et al. 1999).
Nicotine is believed to have a key role in the pathogenesis of lung cancer due to the production of free radicals in many cells including leucocytes. In rat lymphocytes, FA (10–150 μM) counteracted nicotine-induced lipid peroxidation and GSH depletion (Sudheer et al. 2007). In the same study, nicotine has been shown to significantly impair the antioxidant cell defense system, but the co-administration of FA (150 μM) counteracted the nicotine-induced decrease in superoxide dismutase catalase, glutathione peroxidase, vitamin A, E and C contents and this antioxidant effect was comparable to that elicited by N-acetylcysteine treatment (Sudheer et al. 2007). An interesting corollary from the study by Sudheer et al. is that the antioxidant effects of FA is achieved in lymphocytes, namely immune cells involved in the chronic response to inflammatory diseases. This finding is in good agreement with previous studies demonstrating the activation of Hsp in lymphocytes of patients suffering from AD and type 2 diabetes mellitus, two clinical conditions characterized by a strong oxidative damage (Calabrese et al. 2006b, 2007b). Taken together, these lines of evidence underlie the common denominator in the cytoprotective effect of FA and heat shock, i.e. the induction of a systemic hormetic response.
Another mechanism for the anticarcinogenic action of FA seems to be the stimulation of detoxification enzyme. UDP-glucuronosyltransferases (UGTs) catalyse the conjugation of endogenous and exogenous compounds with glucuronic acid, resulting in less biologically active molecules, with an enhanced water solubility which facilitates the excretion through bile or urine. UDP-glucuronosyltransferases have been divided into two families: UGT1 and UGT2. The former mainly catalyses the conjugation of exogenous agents like drugs, peptides, etc., whereas the latter glucuronidate endogenous molecules such as steroid hormones and bile acids (King et al. 2001). FA enhanced significantly UGT enzyme activity in the liver contributing to a better detoxification of potentially carcinogenic compounds and subsequently to the prevention of gastrointestinal cancer (van der Logt et al. 2003). Moreover, FA derivatives reduced neoplastic cell growth by acting on both cyclooxygenase (COX) and caspases. COX exists as two main isoforms named COX-1 and COX-2, constitutive and inducible, respectively. These isoforms are homodimers with a molecular weight of about 70 kDa per monomer. Each monomer contains a heme molecule as prosthetic group (Kurumbail et al. 2001). The COX activity is responsible for the synthesis of PGG2 from two molecules of oxygen and a molecule of arachidonic acid, whereas the peroxidase activity catalyses a net two electron reduction of the 15-hydroperoxyl group of PGG2 yielding PGH2, with the release of an oxidizing radical (Rouzer and Marnett 2003; Yamagata et al. 1993). Finally, PGH2 is transformed by tissue-specific isomerases (PG synthases) into PGE2, PGD2, PGF2 and PGI2 (Thun et al. 2002). These bioactive lipids are involved in many patho-physiological conditions including inflammation, apoptosis, and cancer (Patrono et al. 2001; Thun et al. 2002). In particular, COX-2 is up-regulated in many types of cancer, and non-steroidal antinflammatory drugs, which inhibit COX activity, has been proposed as anticancer drugs (Jayaprakasam et al. 2006; Patrono et al. 2001; Thun et al. 2002). FA derivatives, such as octyl and dodecyl esters, markedly inhibited the growth of breast, lung, colon and central nervous system tumor cells with an IC50 ranging from 17.05 to 4.29 μg/ml for breast and colon, respectively (Jayaprakasam et al. 2006). Furthermore, ferulates up to lateral chain length C8 exhibited a significant COX-2 enzyme inhibition, although the inhibitory activity is not strictly selective and decrease considerably for esters with chain length >C8 (Jayaprakasam et al. 2006). On the other hand, in tumor cells, octyl esters of FA induced apoptosis, through the release of cytocrome c from mitochondria and the activation of caspase-3 (Cione et al. 2008).
FA and cardiovascular disease
Cardiovascular diseases include coronary heart disease, cerebrovascular disease, raised blood pressure (hypertension), peripheral artery disease, rheumatic heart disease, congenital heart disease and heart failure. The major causes of cardiovascular disease are tobacco use, physical inactivity, unhealthy diet, obesity, lipid levels hypertension and diabetes mellitus (Riccioni et al. 2007). Cardiovascular disease is the number one cause of death globally (Centers for Disease Control and Prevention (CDC) 2001; Riccioni et al. 2007). The risk to develop cardiovascular disease is directly related to the blood pressure, in fact a 5 mmHg decrease in blood pressure has been equated to a 16% decrease in cardiovascular disease (FitzGerald et al. 2004). Previous studies have shown that sodium ferulate decreases serum lipids, inhibits platelet aggregation and prevents thrombus formation (Wang et al. 2004; Zhui et al. 2000). The discovery of the antihypertensive and antihyperlipidemic properties of FA was very surprising and opened a new frontier in the potential “clinical” use of this molecule. FA (1-100 mg/kg body weight orally administered) dose-dependently decreased blood pressure in both spontaneously hypertensive rats (SHR) and stroke-prone spontaneously hypertensive rats (SHRSP) with a maximum effect (−34 mmHg) 2 h after FA oral administration (Ohsaki et al. 2008; Suzuki et al. 2002). Interestingly, at the dose of 50 mg/kg body weight the antihypertensive effect of FA was comparable to that obtained with 10 mg/kg body weight of captopril, an angiotensin-converting- enzyme (ACE) inhibitor (Suzuki et al. 2002). The antihypertensive effect of FA seems to be due not only to the inhibition of ACE activity (Ohsaki et al. 2008) but also NO production seems to be involved. In fact, the removal of endothelium or the incubation of SHR thoracic aorta with L-NAME, an inhibitor of NOS, abolished the vasorelaxant effect of FA (Suzuki et al. 2007).
Atherosclerosis, another important form of cardiovascular disease, is characterized by a chronic inflammatory response of vessel wall promoted by oxidized lipid and cholesterol transported by low density lipoproteins (LDL) which follows the accumulation of macrophages and formation of foam cells (Hassan et al. 2006). The atherosclerothic plaque thus formed, decreases vascular elasticity, promotes luminal stenosis and thrombus formation which predispose to cardio-cerebral and peripheral vascular disease (Robbie and Libby 2001). FA reduced both triglyceride (−26 mg/dl and −1.77 mmol/l in rats and rabbits, respectively) and total cholesterol (−10.2 mg/dl) plasma levels along with a significant decrease in blood pressure (see above) in SHRSP and rabbits fed with an high-lipid diet (Ohsaki et al. 2008; Wang et al. 2004). Observation of atherosclerotic plaque area highlighted that rabbits treated with FA has a smaller atherosclerotic plaques than control group (Wang et al. 2004). The mechanism(s) involved in the lipid lowering activity of FA are still unknown. However, an increased uptake of cholesterol by the liver, probably mediated by high density lipoproteins has been recently proposed (Ohsaki et al. 2008).
FA and diabetes
Diabetes mellitus (DM) is a chronic disease caused by inherited and/or acquired deficiency in production of insulin by the pancreas, or by the resistance of peripheral tissues to insulin. Insulin deficiency results in increased concentrations of glucose in the blood, which in turn injures many of the body’s systems, in particular blood vessels and nerves (Edelman 1998; von Herrath et al. 2007). In animal models of DM, FA exerted beneficial effects by acting at many levels. First, FA lowered blood glucose in a model of db/db mice followed by a significantly increase in plasma insulin with a negative correlation between blood glucose and plasma insulin (Jung et al. 2007). Second, the polyphenol inhibited the activity of α-glucosidase which converts carbohydrates into monosaccharides which can be absorbed through the intestine and results in a high glucose level in diabetic subject (Jung et al. 2007). Third, FA increased the activity of glucokinase, a key enzyme in the regulation of blood glucose levels because it facilitates the phosphorylation of glucose to glucose-6-phosphate, the first step in both glycogen synthesis and glycolysis in the liver (Jung et al. 2007). A common complication in diabetic patients is nephropathy characterized by high protein levels in the urine. Although the mechanism of diabetic nephropathy has not yet been clarified because of the complexity of the pathophysiology of DM, numerous factors have been reported to be involved including activation of the renin-angiotensin system (Giacchetti et al. 2005), activation of protein kinase Cβ (Inoguchi et al. 2003) and acceleration of oxidative stress (Kiritoshi et al. 2003). In a rat model of DM, FA significantly lowered urinary proteins level compared to the control group and suppressed the expression of transforming growth factor-β1 (TGF-β1) which is involved in the activation of mesangial cells (Fujita et al. 2008). Inflammatory cytokines may produce more severe inflammation by increasing ROS generation and inflammatory cells chemotaxis. When mesangial cells are activated by TGF-β1, the glomerular structure undergoes mesangial hyperthrophy and fibrosis. Therefore one possible mechanism by which FA exert its protective effects against nephropathy is by reducing oxidative stress in this process.
FA and skin
The best known acute effect of excessive ultraviolet (UV) exposure is erythema, the familiar skin reddening termed sunburn. Chronic exposure to UV radiation also causes a number of degenerative changes in the cells, fibrous tissue and blood vessels of the skin. These include freckles, nevi and lentigines, which are pigmented areas of the skin, and diffuse brown pigmentation (Hölzle 1992). Physiologically, prolonged sun exposure and UV radiation accelerates skin aging, and the gradual loss of skin’s elasticity results in wrinkles and dry, coarse skin (Makrantonaki and Zouboulis 2007). Unlike chronologically aged skin that results from a general atrophy and a gradual decline in the production of the dermal matrix (Frances and Robert 1984), photoaged skin is characterized by a gross increase in skin elastic fibers (elastin, fibrillin, and desmosine), glycosaminoglycans, collagen cross-linking, epidermal thickening, and dermal cysts (Kligman et al. 1985; Kligman 1996).
UV-induced skin damage principally depends on ROS formation: a photon of radiation interacts with trans-urocanic acid in skin that generate singlet oxygen that can activate the entire oxygen free radical cascade with oxidation of nucleic acid, proteins and lipids resulting in skin cancer and photoaging change (Handson and Simon 1998). FA has been shown to be a strong UV absorber (Graf 1992) and this finding represents an interesting background supporting its use as topical protective agent against UV radiation-induced skin damage. FA is absorbed by skin at the same rate both at acidic and neutral pH indicating that pH does not influence the skin penetration and the molecule could be absorbed both under undissociated and dissociated form (Saija et al 2000). Moreover FA proved to afford a significant protection to the skin against UVB-induced erythema in a time dependent manner (Saija et al 2000). On the other hand, FA is used also to stabilize antioxidant products present in many formulation for topical use such as vitamin C and vitamin E. FA alone or in association with vitamin C and vitamin E provided about 4- to 8-fold protection against solar-simulated radiation damage probably interacting with pro-oxidative intermediates (Lin et al. 2005). Very recently, it has been shown that topical treatment with a solution containing 15% vitamin C, 1% vitamin E and 0.5% FA, provided an effective photoprotection solar-simulated ultraviolet-induced photodamage in the pig (Lin et al. 2008). On this basis, it has been proposed to potentiate the photoprotective activity of FA by increasing the deliver of the polyphenol contained in commercially available sunscreens. At least two types of new drug-delivery-systems (DDS) containing FA, such as solid-lipid nanoparticles and cyclodextrins, have been developed and the amount of polyphenol absorbed by the skin increased significantly and, more importantly, the formation of FA degradation products have been avoided (Anselmi et al. 2008; Souto et al. 2005). As a matter of fact, the preparation of novel FA-DDS may be very useful also to increase the bioavailability of the polyphenol if administered per os. This approach may improve the targeting of FA in several tissues, and increase its in several anti-aging strategies.
Very recently, a novel mechanism for the cytoprotective effect of FA has been proposed. In human dermal fibroblasts, FAEE decreased both hydrogen peroxide-induced cytotoxicity and protein/lipid oxidation with a mechanism which has been proposed to be mediated by the up-regulation of HO-1 and Hsp70 (Calabrese et al. 2008). This last finding strengthens the hormetic behavior of FA and opens new avenues for the use of nutriceuticals to potentiate the cell stress response.
Conclusions and perspectives
As discussed in this review, the cytoprotective effect of FA in many experimental systems is well established. However, the potential use of supplemental FA in the therapy of age-related human pathologies is still to be confirmed. The main concerns derive from the pharmacokinetics of FA and in particular its poor bioavailability and metabolic fate. The first question to be addressed in further clinical studies should be the following: after oral supplementation in humans, does FA reach tissue concentrations similar to those which have been shown to be effective in preclinical studies? Unfortunately, no studies in humans are available and data in rodents have shown a plasma concentration ~1–3 μM (Zhao et al. 2003) which is lower than that used very often in several in vitro studies. Furthermore, studies in rodents have clearly shown that following intravenous administration, FA accumulated in liver, kidney and lung, whereas the concentration reached in other tissues such as brain or heart is negligible (Li et al. 2008; Qin et al. 2007). Taken together, these data do not allow to predict the real cytoprotective role of FA in human diseases such as neurodegenerative disorders in which its functional role has been claimed based on in vitro studies. However, an attempt to overcome this limitation was made and FA has been complexed with liposomes, nanoparticles and niosomes in order to improve its absorption and tissue distribution. Using these new delivery systems, FA was better absorbed and its concentration increased in many organs, even if in the brain it was still low (Li et al. 2008; Qin et al. 2007). The second question to be addressed is the remarkable stimulation of UGT by FA (van der Logt et al. 2003). This effect should be taken into consideration because many drugs, including benzodiazepines, morphine, acetaminophen and organic nitrates are metabolised by UGT and therefore its stimulation could decrease the plasma concentrations of these drugs and reduce their pharmacological effects. For instance, the concomitant administration of FA with benzodiazepines may reduce their sedative effect as well as the antipyretic activity of acetaminophen or the useful effects of organic nitrates in the treatment of angina pectoris. All these drug interactions should be careful considered in selected populations such as aged patients, for whom the supplementation with FA have been claimed. It is possible to conclude that clinical research on FA and its potential use in human diseases needs to be potentiated. So far, the “therapeutic” use of FA in some human age-related pathologies could be only considered an attractive hypothesis.
References
Anselmi C, Centini M, Maggiore M et al (2008) Non-covalent inclusion of ferulic acid with alpha-cyclodextrin improves photo-stability and delivery: NMR and modeling studies. J Pharm Biomed Anal 46:645–652. doi:10.1016/j.jpba.2007.11.037
Barnham KJ, Cappai R, Beyreuther K et al (2006) Delineating common molecular mechanisms in Alzheimer’s and prion diseases. Trends Biochem Sci 31:465–472. doi:10.1016/j.tibs.2006.06.006
Bourne LC, Rice-Evans C (1998) Bioavailability of ferulic acid. Biochem Biophys Res Commun 253:222–277. doi:10.1006/bbrc.1998.9681
Butterfield DA (2002) Amyloid beta-peptide (1–42)-induced oxidative stress and neurotoxicity: implications for neurodegeneration in Alzheimer’s disease brain. A review. Free Radic Res 36:1307–1313. doi:10.1080/1071576021000049890
Calabrese V, Guagliano E, Sapienza M et al (2006a) Redox regulation of cellular stress response in neurodegenerative disorders. Ital J Biochem 55:263–282
Calabrese V, Sultana R, Scapagnini G et al (2006b) Nitrosative stress, cellular stress response, and thiol homeostasis in patients with Alzheimer’s disease. Antioxid Redox Signal 8:1975–1986. doi:10.1089/ars.2006.8.1975
Calabrese V, Mancuso C, Calvani M et al (2007a) Nitric oxide in the central nervous system: neuroprotection versus neurotoxicity. Nat Rev Neurosci 8:766–775. doi:10.1038/nrn2214
Calabrese V, Mancuso C, Sapienza M et al (2007b) Oxidative stress and cellular stress response in diabetic nephropathy. Cell Stress Chaperones 12:299–306. doi:10.1379/CSC-270.1
Calabrese V, Calafato S, Puleo E et al (2008) Redox regulation of cellular stress response by ferulic acid ethyl ester in human dermal fibroblast: role of vitagenes. Clin Dermatol (in press)
Centers for Disease Control and Prevention (CDC) (2001) Prevalence of healthy lifestyle characteristics–Michigan, 1998 and 2000. MMWR Morb Mortal Wkly Rep 50(35):758–761
Cho JY, Kim HS, Kim DH et al (2005) Inhibitory effects of long-term administration of ferulic acid on astrocyte activation induced by intracerebroventricular injection of beta-amyloid peptide (1–42) in mice. Prog Neuropsychopharmacol Biol Psychiatry 29:901–907. doi:10.1016/j.pnpbp. 2005.04.022
Cione E, Tucci P, Senatore V et al (2008) Synthesized esters of ferulic acid induce release of cytochrome c from rat testes mitochondria. J Bioenerg Biomembr 40:19–26. doi:10.1007/s10863-007-9097-7
Clifford MN (1999) Chlorogenic acids and other cinnamates-nature, occurrence and dietary burden. J Sci Food Agric 79:362–372. doi:10.1002/(SICI)1097-0010(19990301)79:3<362::AID-JSFA256>3.0.CO;2-D
Comporti M (1989) Three models of free radical-induced cell injury. Chem Biol Interact 72:1–56. doi:10.1016/0009-2797(89)90016-1
Couteau D, McCartney AL, Gibson GR et al (2001) Isolation and characterization of human colonic bacteria able to hydrolyse chlorogenic acid. J Appl Microbiol 90:873–881. doi:10.1046/j.1365-2672.2001.01316.x
D’Archivio M, Filesi C, Di Benedetto R et al (2007) Polyphenols, dietary sources and bioavailability. Ann Ist Super Sanita 43:348–361
Edelman SV (1998) Type II diabetes mellitus. Adv Intern Med 43:449–500
FitzGerald RJ, Murray BA, Walsh DJ (2004) Hypotensive peptides from milk proteins. J Nutr 134:980S–988S
Frances C, Robert L (1984) Elastin and elastic fibers in normal and pathologic skin. Int J Dermatol 23:166–179. doi:10.1111/j.1365-4362.1984.tb04506.x
Fujita A, Sasaki H, Doi A et al (2008) Ferulic acid prevents pathological and functional abnormalities of the kidney in Otsuka Long-Evans Tokushima Fatty diabetic rats. Diabetes Res Clin Pract 79:11–17. doi:10.1016/j.diabres.2007.08.009
Giacchetti G, Sechi LA, Rilli S et al (2005) The renin-angiotensin-aldosterone system, glucose metabolism and diabetes. Trends Endocrinol Metab 16:120–126. doi:10.1016/j.tem.2005.02.003
Graf E (1992) Antioxidant potential of ferulic acid. Free Radic Biol Med 13:435–448. doi:10.1016/0891-5849(92)90184-I
Hassan HH, Denis M, Krimbou L et al (2006) Cellular cholesterol homeostasis in vascular endothelial cells. Can J Cardiol 22(Suppl B):35B–40B
Hinault MP, Ben-Zvi A, Goloubinoff P (2006) Chaperones and proteases: cellular fold-controlling factors of proteins in neurodegenerative diseases and aging. J Mol Neurosci 30:249–265. doi:10.1385/JMN:30:3:249
Hirose M, Takahashi S, Ogawa K et al (1999) Phenolics: blocking agents for heterocyclic amine-induced carcinogenesis. Food Chem Toxicol 37:985–992. doi:10.1016/S0278-6915(99)00092-7
Hölzle E (1992) Pigmented lesions as a sign of photodamage. Br J Dermatol Suppl 41:48–50
Inoguchi T, Sonta T, Tsubouchi H et al (2003) Protein kinase C-dependent increase in reactive oxygen species (ROS) production in vascular tissues of diabetes: role of vascular NAD(P)H oxidase. J Am Soc Nephrol 14:S227–S232. doi:10.1097/01.ASN.0000077407.90309.65
Jayaprakasam B, Vanisree M, Zhang Y et al (2006) Impact of alkyl esters of caffeic and ferulic acids on tumor cell proliferation, cyclooxygenase enzyme, and lipid peroxidation. J Agric Food Chem 54:5375–5381. doi:10.1021/jf060899p
Jin Y, Yan EZ, Fan Y et al (2005) Sodium ferulate prevents amyloid-beta-induced neurotoxicity through suppression of p38 MAPK and upregulation of ERK-1/2 and Akt/protein kinase B in rat hippocampus. Acta Pharmacol Sin 26:943–951. doi:10.1111/j.1745-7254.2005.00158.x
Jin Y, Fan Y, Yan EZ et al (2006) Effects of sodium ferulate on amyloid-beta-induced MKK3/MKK6–p38 MAPK-Hsp27 signal pathway and apoptosis in rat hippocampus. Acta Pharmacol Sin 27:1309–1316. doi:10.1111/j.1745-7254.2006.00414.x
Jung EH, Kim SR, Hwang IK et al (2007) Hypoglycemic effects of a phenolic acid fraction of rice bran and ferulic acid in C57BL/KsJ-db/db mice. J Agric Food Chem 55:9800–9804. doi:10.1021/jf0714463
Kanski J, Aksenova M, Stoyanova A et al (2002) Ferulic acid antioxidant protection against hydroxyl and peroxyl radical oxidation in synaptosomal and neuronal cell culture systems in vitro: structure-activity studies. J Nutr Biochem 13:273–281. doi:10.1016/S0955-2863(01)00215-7
Katsuki H, Nakai S, Hirai Y et al (1990) Interleukin-1 beta inhibits long-term potentiation in the CA3 region of mouse hippocampal slices. Eur J Pharmacol 181:323–326. doi:10.1016/0014-2999(90)90099-R
Khanduja KL, Avti PK, Kumar S et al (2006) Anti-apoptotic activity of caffeic acid, ellagic acid and ferulic acid in normal human peripheral blood mononuclear cells: a Bcl-2 independent mechanism. Biochim Biophys Acta 1760:283–289
King C, Tang W, Ngui J et al (2001) Characterization of rat and human UDP-glucuronosyltransferases responsible for the in vitro glucuronidation of diclofenac. Toxicol Sci 61:49–153. doi:10.1093/toxsci/61.1.49
Kiritoshi S, Nishikawa T, Sonoda K et al (2003) Reactive oxygen species from mitochondria induce cyclooxygenase-2 gene expression in human mesangial cells: potential role in diabetic nephropathy. Diabetes 52:2570–2577. doi:10.2337/diabetes.52.10.2570
Kligman LH (1996) The hairless mouse model for photoaging. Clin Dermatol 14:183–195. doi:10.1016/0738-081X(95)00154-8
Kligman LH, Akin FJ, Kligman AM (1985) The contributions of UVA and UVB to connective tissue damage in hairless mice. J Invest Dermatol 84:272–276. doi:10.1111/1523-1747.ep12265353
Kroon PA, Faulds CB, Ryden P et al (1997) Release of Covalently Bound Ferulic Acid from Fiber in the Human Colon. J Agric Food Chem 45:661–667. doi:10.1021/jf9604403
Kurumbail RG, Kiefer JR, Marnett LJ (2001) Cyclooxygenase enzymes: catalysis and inhibition. Curr Opin Struct Biol 11:752–760. doi:10.1016/S0959-440X(01)00277-9
Li FQ, Su H, Wang J et al (2008) Preparation and characterization of sodium ferulate entrapped bovine serum albumin nanoparticles for liver targeting. Int J Pharm 349:274–282. doi:10.1016/j.ijpharm.2007.08.001
Lin FH, Lin JY, Gupta RD et al (2005) Ferulic acid stabilizes a solution of vitamins C and E and doubles its photoprotection of skin. J Invest Dermatol 125:826–832. doi:10.1111/j.0022-202X.2005.23768.x
Lin JY, Tournas JA, Burch JA et al (2008) Topical isoflavones provide effective photoprotection to skin. Photodermatol Photoimmunol Photomed 24:61–66. doi:10.1111/j.1600-0781.2008.00329.x
Makrantonaki E, Zouboulis CC (2007) Molecular mechanisms of skin aging: state of the art. Ann N Y Acad Sci 1119:40–50. doi:10.1196/annals.1404.027
Mancuso C (2004) Heme oxygenase and its products in the nervous system. Antioxid Redox Signal 6:878–887
Mancuso C, Pani G, Calabrese V (2006) Bilirubin: an endogenous scavenger of nitric oxide and reactive nitrogen species. Redox Rep 11:207–213. doi:10.1179/135100006X154978
Mancuso C, Bates TE, Butterfield DA et al (2007a) Natural antioxidants in Alzheimer’s disease. Expert Opin Investig Drugs 16:1921–1931. doi:10.1517/13543784.16.12.1921
Mancuso C, Scapagnini G, Currò D et al (2007b) Mitochondrial dysfunction, free radical generation and cellular stress response in neurodegenerative disorders. Front Biosci 12:1107–1123. doi:10.2741/2130
Ohsaki AY, Shirakawa H, Koseki T, Komai M (2008) Novel effects of a single administration of ferulic acid on the regulation of blood pressure and the hepatic lipid metabolic profile in stroke-prone spontaneously hypertensive rats. J Agric Food Chem 56(8):2825–2830
Ou S, Kwok KC (2004) Ferulic acid: pharmaceutical functions, preparation and applications in food. J Sci Food Agric 84:1261–1269. doi:10.1002/jsfa.1873
Patrono C, Patrignani P, García Rodríguez LA (2001) Cyclooxygenase-selective inhibition of prostanoid formation: transducing biochemical selectivity into clinical read-outs. J Clin Invest 108(1):7–13
Poquet L, Clifford MN, Williamson G (2008) Transport and metabolism of ferulic acid through the colonic epithelium. Drug Metab Dispos 36:190–197. doi:10.1124/dmd.107.017558
Preziosi P, Loscalzo B (1957a) Pharmacodynamic research on the active principle of Cynara scolimus(1, 4-dicaffeiylquinic acid): effect on blood cholesterol values & on triton-induced hypercholesterolemia. Boll Soc Ital Biol Sper 33:679–682
Preziosi P, Loscalzo B (1957b) Experimental evaluation of 1, 4-dicaffeiylquinic acid, the active principle of artichoke. Arch Ital Sci Farmacol 7:249–296
Preziosi P, Loscalzo B (1958) Pharmacological properties of 1, 4 dicaffeylquinic acid, the active principle of Cynara scolimus. Arch Int Pharmacodyn Ther 117:63–80
Preziosi P, Loscalzo B, Bianchi A (1957) Pharmacodynamic research on the active principle of Cynara scolimus (1, 4-dicaffeiylquinic acid): effect on choleresis. Boll Soc Ital Biol Sper 33:672–674
Qin J, Chen D, Hu H (2007) Body distributioin of RGD-mediated liposome in brain-targeting drug delivery. Yakugaku Zasshi 127:1497–1501. doi:10.1248/yakushi.127.1497
Rattan SI (2008a) Hormesis in aging. Ageing Res Rev 7:63–78. doi:10.1016/j.arr.2007.03.002
Rattan SI (2008b) Principles and practice of hormetic treatment of aging and age-related diseases. Hum Exp Toxicol 27:151–154. doi:10.1177/0960327107083409
Rechner AR, Pannala AS, Rice-Evans CA (2001a) Caffeic acid derivatives in artichoke extract are metabolised to phenolic acids in vivo. Free Radic Res 35:195–202. doi:10.1080/10715760100300741
Rechner AR, Spencer JP, Kuhnle G et al (2001b) Novel biomarkers of the metabolism of caffeic acid derivatives in vivo. Free Radic Biol Med 30:1213–1222. doi:10.1016/S0891-5849(01)00506-8
Riccioni G, Bucciarelli T, Mancini B et al (2007) The role of the antioxidant vitamin supplementation in the prevention of cardiovascular diseases. Expert Opin Investig Drugs 16:25–32. doi:10.1517/13543784.16.1.25
Robbie L, Libby P (2001) Inflammation and atherothrombosis. Ann N Y Acad Sci 947:167–179
Robinson MJ, Cobb MH (1997) Mitogen-activated protein kinase pathways. Curr Opin Cell Biol 9:180–186. doi:10.1016/S0955-0674(97)80061-0
Rondini L, Peyrat-Maillard MN, Marsset-Baglieri A et al (2002) Sulfated ferulic acid is the main in vivo metabolite found after short-term ingestion of free ferulic acid in rats. J Agric Food Chem 50:3037–3041. doi:10.1021/jf011295i
Rondini L, Peyrat-Maillard MN, Marsset-Baglieri A et al (2004) Bound ferulic acid from bran is more bioavailable than the free compound in rat. J Agric Food Chem 52:4338–4343. doi:10.1021/jf0348323
Rouzer CA, Marnett LJ (2003) Mechanism of free radical oxygenation of polyunsaturated fatty acids by cyclooxygenases. Chem Rev 103:2239–2304. doi:10.1021/cr000068x
Saija A, Tomaino A, Trombetta D et al (2000) In vitro and in vivo evaluation of caffeic and ferulic acids as topical photoprotective agents. Int J Pharm 199:39–47. doi:10.1016/S0378-5173(00)00358-6
Saulnier L, Vigouroux J, Thibault JF (1995) Isolation and partial characterization of feruloylated oligosaccharides from maize bran. Carbohydr Res 272:241–253. doi:10.1016/0008-6215(95)00053-V
Scapagnini G, Butterfield DA, Colombrita C et al (2004) Ethyl ferulate, a lipophilic polyphenol, induces HO-1 and protects rat neurons against oxidative stress. Antioxid Redox Signal 6:811–818
Silberberg M, Morand C, Mathevon T et al (2006) The bioavailability of polyphenols is highly governed by the capacity of the intestine and of the liver to secrete conjugated metabolites. Eur J Nutr 45:88–96. doi:10.1007/s00394-005-0568-5
Souto EB, Anselmi C, Centini M et al (2005) Preparation and characterization of n-dodecyl-ferulate-loaded solid lipid nanoparticles (SLN). Int J Pharm 295:261–268. doi:10.1016/j.ijpharm.2005.02.005
Srinivasan M, Rukkumani R, Ram Sudheer A et al (2005) Ferulic acid, a natural protector against carbon tetrachloride-induced toxicity. Fundam Clin Pharmacol 19:491–496. doi:10.1111/j.1472-8206.2005.00332.x
Sudheer AR, Muthukumaran S, Kalpana C et al (2007) Protective effect of ferulic acid on nicotine-induced DNA damage and cellular changes in cultured rat peripheral blood lymphocytes: a comparison with N-acetylcysteine. Toxicol In Vitro 21:576–585. doi:10.1016/j.tiv.2006.11.006
Sultana R, Ravagna A, Mohmmad-Abdul H et al (2005) Ferulic acid ethyl ester protects neurons against amyloid beta- peptide(1–42)-induced oxidative stress and neurotoxicity: relationship to antioxidant activity. J Neurochem 92:749–758. doi:10.1111/j.1471-4159.2004.02899.x
Suzuki A, Kagawa D, Fujii A et al (2002) Short- and long-term effects of ferulic acid on blood pressure in spontaneously hypertensive rats. Am J Hypertens 15:351–357. doi:10.1016/S0895-7061(01)02337-8
Suzuki A, Yamamoto M, Jokura H et al (2007) Ferulic acid restores endothelium-dependent vasodilation in aortas of spontaneously hypertensive rats. Am J Hypertens 20:508–513. doi:10.1016/j.amjhyper.2006.11.008
Thun MJ, Henley SJ, Patrono C (2002) Nonsteroidal anti-inflammatory drugs as anticancer agents: mechanistic, pharmacologic, and clinical issues. J Natl Cancer Inst 94:252–266
van der Logt EM, Roelofs HM, Nagengast FM et al (2003) Induction of rat hepatic and intestinal UDP-glucuronosyltransferases by naturally occurring dietary anticarcinogens. Carcinogenesis 24:1651–1656. doi:10.1093/carcin/bgg117
von Herrath M, Sanda S, Herold K (2007) Type 1 diabetes as a relapsing-remitting disease? Nat Rev Immunol 7:988–994. doi:10.1038/nri2192
Wang B, Ouyang J, Liu Y et al (2004) Sodium ferulate inhibits atherosclerogenesis in hyperlipidemia rabbits. J Cardiovasc Pharmacol 43:549–554. doi:10.1097/00005344-200404000-00010
Wang X, Martindale JL, Liu Y et al (1998) The cellular response to oxidative stress: influences of mitogen-activated protein kinase signalling pathways on cell survival. Biochem J 333:291–300
Yamagata K, Andreasson KI, Kaufmann WE et al (1993) Expression of a mitogen-inducible cyclooxygenase in brain neurons: regulation by synaptic activity and glucocorticoids. Neuron 11:371–386. doi:10.1016/0896-6273(93)90192-T
Yan JJ, Cho JY, Kim HS et al (2001) Protection against beta-amyloid peptide toxicity in vivo with long-term administration of ferulic acid. Br J Pharmacol 133:89–96. doi:10.1038/sj.bjp. 0704047
Zhao Z, Egashira Y, Sanada H (2003) Ferulic acid sugar esters are recovered in rat plasma and urine mainly as the sulfoglucuronide of ferulic acid. J Nutr 133:1355–1361
Zhao Z, Egashira Y, Sanada H (2004) Ferulic acid is quickly absorbed from rat stomach as the free form and then conjugated mainly in liver. J Nutr 134:3083–3088
Zhou H, Li XM, Meinkoth J et al (2000) Akt regulates cell survival and apoptosis at a postmitochondrial level. J Cell Biol 151:483–494. doi:10.1083/jcb.151.3.483
Zhui Y, Jing-Ping OY, Yongming L et al (2000) Experimental study of the antiatherogenesis effect of Chinese medicine angelica and its mechanisms. Clin Hemorheol Microcirc 22:305–310
Acknowledgments
The authors are grateful to Prof. Paolo Preziosi MD, Emeritus of Pharmacology at the Catholic University School of Medicine in Roma, for his helpful comments and suggestions and for reading the manuscript. This work was supported by Fondi Ateneo 2007 and 2008 to C.M.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barone, E., Calabrese, V. & Mancuso, C. Ferulic acid and its therapeutic potential as a hormetin for age-related diseases. Biogerontology 10, 97–108 (2009). https://doi.org/10.1007/s10522-008-9160-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10522-008-9160-8