Abstract
In Mexico City, male sex workers (MSWs) are up to 126 times more likely to be living with HIV than the general public. We conducted interviews with 23 MSWs in Mexico City to examine their subjective understandings about their sexual risk behaviors and explore opportunities about HIV pre-exposure prophylaxis (PrEP) as a prevention approach in this group. Despite knowledge about sexual HIV risks, most participants reported condomless anal sex with clients. There was very little prior knowledge about PrEP, but very high interest in using a daily pill for prevention. Several participants expected an increase in condomless anal sex if taking PrEP, because of monetary incentives from clients or a perceived increase in pleasure. Additionally, seasonal sex workers expressed interest in using PrEP only during months when they were performing sex work. PrEP implementation efforts through Mexico’s healthcare system should recognize the varying needs and sexual risk behaviors of MSWs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Men who exchange sex with other men for money or non-monetary goods (male sex workers; MSWs) in Mexico City are more likely to be infected with HIV compared to men who have sex with men (MSM) overall (Galárraga et al., 2014). Recent studies estimate HIV prevalence among MSM in Mexico City to be 18%, and as high as 38% among MSWs (compared to only 0.3% in the overall population). In fact, condoms are not used in 16–22% of sex work encounters in Mexico City (Galárraga et al., 2014), which may be in part due to physical coercion and market inducements to not use condoms (Biello et al., 2017a; Galárraga et al., 2014; Grov, 2014; Infante, SosaRubi, & Cuadra, 2009; Mimiaga, Reisner, Tinsley, Mayer, & Safren, 2009; Monteiro et al., 2015). Additionally, MSWs have higher rates of drug (including stimulants) and alcohol use, psychosocial conditions (e.g., depression), violence, and homelessness, and lower rates of health insurance and access to healthcare services compared to MSM in Mexico overall—all of which have been shown to be associated with higher risk for HIV (Galárraga & Sosa-Rubí, 2016).
Given that HIV risk in this population is complex, it cannot be addressed through condom distribution alone. Rather, HIV prevention programs for MSWs in Mexico City will likely require combination prevention modalities that incorporate novel approaches beyond condom use, including HIV pre-exposure prophylaxis (PrEP). PrEP, a once-daily oral pill (emtricitabine/tenofovir disoproxil fumarate), is highly effective in the prevention of HIV among at-risk individuals if adherence is high (~ 4+ doses per week) (Choopanya et al. 2013; Grant et al., 2010, 2014; McCormack et al. 2016). However, PrEP is not yet available to the general public through Mexico’s universal healthcare system. Currently, the externally funded “ImPrEP” demonstration study in Mexico City is among the first to provide access to PrEP for a limited number of at-risk MSM and MSWs in the country (Pan American Health Organization, 2017).
In studies done in the U.S., MSWs reported greater willingness to use PrEP compared to MSM overall (Mgbako et al., 2019), while interest in preventive HIV care stemmed from appeasing requests from intimate partners, and knowing of positive HIV tests among friends and family (Underhill et al., 2014). Barriers to preventive HIV care included a de-prioritization of health concerns during periods of substance use or relative to other basic needs, as well as apprehension about sexual partners being unsupportive of PrEP use (Biello et al., 2017b; Underhill et al., 2014). Further, a recent meta-analysis comparing rates of STIs between MSM using PrEP, MSM not using PrEP, found that MSM using PrEP were much more likely to be diagnosed with Chlamydia, Gonorrhea, or Syphilis, which may be due in part to increased number of condomless sex acts (Kojima, Davey, & Klausner, 2016). Notably, the participants included in these studies were not from low- or middle-income countries (LMIC).
Research among MSWs in LMIC is limited overall, and there is a paucity of research exploring PrEP as a prevention modality for MSWs in these areas. Recent work has found substantial interest in using PrEP among MSWs in some LMIC, despite low levels of baseline awareness of the medication (Oldenburg et al., 2014; Restar et al., 2017; Yi et al., 2017). In Mexico, there is some evidence to suggest that men who sell sex to other men may be more interested in using PrEP than MSM overall (Edeza et al., 2019). Given this potential interest in PrEP among MSWs in Mexico, and its association with increased STI incidence among MSM groups more broadly in other countries, there is a critical need to contextualize the state of PrEP knowledge and interest among this group. To date, there has been no qualitative research examining knowledge, interest, and potential barriers to PrEP uptake and adherence among MSWs or other high-risk MSM in Mexico. Considering the state of the HIV epidemic among MSWs in Mexico City and the ongoing demonstration project, we conducted qualitative interviews with male sex workers to better understand the state of awareness and interest in this prevention modality among this community.
Method
Participants
We recruited MSWs (hereafter “participants”) in Mexico City through Clinica Especializada Condesa, the largest specialty HIV prevention and care clinic in the country. Recruitment was carried out during regularly scheduled street outreach at a large public park known for street-based male sex work, in conjunction with an outreach staff member. Additionally, potential participants were informed about the study through the Punto Seguro (or “Safe Point”) program housed in Clinica Especializada Condesa, which provides STI and HIV prevention and care for MSWs, during their regularly scheduled clinical appointments. Potential participants were invited to screen, and if eligible were invited to participate in in-depth interviews. Participants were eligible if they were cis-gender men, 18 years of age or older, self-reported being HIV-negative or unsure of their status, and had exchanged sex for money at least three times in the past month with a non-monogamous partner. Purposive sampling helped to maximize diversity in participant age and experience with sex work. Eligible participants provided verbal informed consent in a private space within the clinic. Participants received a small meal and a grocery store gift card worth 300 MXN (approximately 16 USD at the time of the study) in exchange for their time. All study procedures were approved by the Ethics Committee at the Instituto Nacional de Salud Pública, in Cuernavaca, Mexico.
PrEP is currently not approved for HIV prevention through Mexico’s formal healthcare system. The ImPrEP demonstration project is currently recruiting up to 3000 at-risk individuals, including MSWs, to test the effectiveness of PrEP in the Mexican context. This study was completed 6 months prior to the beginning of this demonstration project in Mexico City.
Measures and Procedure
The researcher, who has been trained in and has experience with conducting qualitative interviews, conducted audio-recorded interviews with participants individually, in a private room at Clinica Especializada Condesa, during daytime business hours. Participants completed an informed consent process prior to providing brief demographic data and completing the interview. The researcher used a semi-structured interview guide with open-ended questions in the following domains: sex work and sex behaviors; access to health services; knowledge, interest, and concerns about PrEP; and perceptions about a conditional economic incentive intervention for medication adherence. After asking about prior knowledge of PrEP, the researcher provided a brief description of the medication as provided by the Centers for Disease Control (2017). In-depth interviews were selected for data collection in light of the sensitive personal topics elicited by the questions and to also provide opportunity for rapport building, a key procedure for ensuring candid responses (Legard, Keegan, & Ward, 2003). Interviews were conducted in Spanish and lasted approximately 45 min—domains were restricted in order to ensure interviews lasted less than 1 h to improve feasibility and reduce participant burden. Recordings were subsequently transcribed by a local professional service.
Data collection was carried out by a Mexican–American, cis-gender male Ph.D. student–researcher who is a native Spanish speaker, and had received formal training and has significant experience in qualitative methods for data collection.
Data Analysis
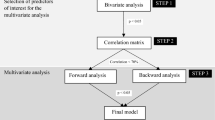
The domains of sex work and sex behaviors, access to health services, and knowledge, interest, and concerns about PrEP are the subject of this analysis, as they relate directly to contextualizing HIV risk and indications for PrEP, as well as PrEP acceptability within this group. Consistent with best practices for thematic analyses (Braun & Clarke, 2006), the researcher wrote detailed memos after the interviews to track emerging themes, which were discussed with other research staff and local outreach worker. These themes were further explored in subsequent interviews by refining probing questions in the semi-structured interview guide. Once all interviews were complete, two research staff members (both with formal training in qualitative research methods and native Spanish speakers) analyzed the data for key themes surrounding PrEP knowledge and interest.
First, the two team members read two full transcripts each and created a list of preliminary codes and definitions from their initial readings. This initial codebook was then applied to two additional full transcripts by each team member independently, who subsequently met to discuss and compare code application, modify the preliminary codebook, and resolve any other discrepancies or concerns. This process was repeated three additional times, until the team members felt that the codebook was refined appropriately for the data, and coding practices were consistent between the team members. Finally, all transcripts were divided between the two team members, and independently coded in Spanish using NVivo (QSR International Pty Ltd. Version 11, 2015). Weekly meetings were held to address any outstanding questions throughout the coding process. The current analysis focuses on key themes surrounding sexual HIV-risk behaviors, and knowledge and interest in PrEP.
Results
A total of 23 participants completed in-depth semi-structured interviews (Table 1). The average age of participants was 30 years old, and most participants identified as Mexican (22, 95%) and currently lived in Mexico City (20, 87%). All reported having had an HIV test at least once in their lifetime. A total of 14 (61%) participants reported having exchanged sex for money at least 10 times in the past 30 days; of these, 3 estimated having exchanged sex for money at least 100 times in the past 30 days. Sex workers who worked exclusively on public streets (14, 61%) were the majority; the remaining participants worked online only (2, 9%) or through another method or combination of methods (7, 30%). A minority of participants (6, 23%) had completed a high school education or greater.
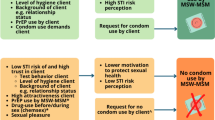
From qualitative interviews, we identified the following key themes: (1) drivers of inconsistent condom use with clients; (2) interest in PrEP to reduce worry about HIV infection during times of recognized risk; (3) interest in using PrEP themselves as a mechanism for protecting their intimate sexual partners from HIV; and (4) expected changes in sexual behavior when on PrEP. Key themes are described below with illustrative quotes, translated into English by bilingual study staff.
Drivers of Inconsistent Condom Use
Though all participants recognized the role of condoms in reducing their risk for HIV infection, over half reported that they did not always use condoms with clients. A number of drivers of inconsistent condom use with clients were discussed by MSWs, including higher transaction prices for condomless sex, alcohol and drug use, client types and HIV beliefs. While many participants reported earning between 150 to 500 MXN per client, some explained that they could earn significantly more for condomless sex. When asked about why he chooses to have condomless sex with only certain clients, one participant replied:
P5: “Because they pay me more when I don’t use it.”
Interviewer: “About how much more do they pay you for not using a condom?”
P5: “500 [MXN]” (24 years old).
Alcohol use with clients was common among the sample, particularly when meeting a client for the first time and negotiating a price. However, participants did not generally report alcohol consumption to the point of inebriation with clients, and as such, very few participants reported not using condoms because of alcohol consumption alone.
P09: “If I do end up drinking a beer, I stop there and that’s it. At most, at most I might drink two beers with a client.”
Although drug use was less common, many participants reported having used stimulants, solvents and poppers at least once before or during sex with a client. Additionally, though few participants reported being intoxicated from alcohol alone, many did report mixing alcohol with other drugs during the course of a transaction with a client. This could potentiate the effects of either substance and impact condom use. When asked about mixing drugs with alcohol before sex, one participant responded:
P14: “Well, to me when I combine [crack] with alcohol, well it produces a different effect, you don’t feel like, well for me I get turned on more with crack and alcohol…” (29 years old)
The impact of stimulant use on participant’s desire to use condoms was elaborated more explicitly by one 37-year-old participant, who described cocaine use during sex. He stated that he perceived sex while on cocaine to be more exciting when not using a condom:
P15: “Yes because you feel more stimulated with the drug, so the arousal is different. So when you use the condom, it’s like you cut off the exciting sensation that you are feeling because of the effects of the cocaine, right?” (37 years old)
Additionally, previous relationships with clients could impact condom use negotiations. Despite believing that condoms were the safest way to have sex, some participants recounted having condomless sex with repeated clients who they perceived to be HIV-negative. When asked about condom use, one 28-year-old participant explained:
P2: “When I don’t end up using a condom, it is with repeated partners that I know are okay, that I know have gotten tested…”
Considerations about condom use often involved misconceptions about HIV itself. Many participants stated that they could discern when somebody was seropositive by their appearance alone. These participants stated that they always used condoms with clients who looked “sick” or “unhealthy”, but were open to condomless sex with clients perceived to be healthy.
P4: “So like, I’m willing to [forego condoms], depending on what the client looks like, if I see him looking yellow or odd then no—‘You know what? No’. If he is more or less healthy than I’ll say ‘yeah, let’s go’.” (30 years old)
Relatedly, some participants believed that healthy lifestyle choices, such as getting enough sleep and exercising, could reduce their risk of HIV infection from condomless sex.
P2: “…And when I don’t end up using a condom it’s with stable partners that I know are okay, that I know have gotten tested, and I’m also very careful in terms of my health, I’m very healthy, I try to sleep well, exercise, like have my immune system always at 100%” (28 years old)
Additionally, a small number of participants believed in home remedies as a contingency plan for exposure to HIV. These included things like ingesting lemon juice or raw garlic to prevent an HIV infection after condomless anal sex, and factored into decisions to use condoms. As one 51-year-old participant explained:
P1: “Because for me, [condoms] are for everything, and well they’re the safest, the safest. I prefer to use condoms, but well sometimes in the heat of it, or for an extra bill, I say well I can just drink some lemon juice later and see.”
Interest in PrEP to Reduce Worry About HIV Infection
Almost all participants stated that they were unfamiliar with PrEP prior to the interview. Among the minority that had prior knowledge of PrEP, some were unsure if it was for treatment or prevention, and two had received accurate but limited information about it through friends or through travel abroad. Notably, no participants had prior knowledge of PrEP as a once-daily medication for HIV prevention. Some, however, equated the side effects of antiretroviral medications used for treatment with PrEP. As one 40-year-old participant stated:
P17: “PrEP, well…I’ve come [to the clinic] with friends that have HIV, and they would get some medication here, I’m not sure if they are still giving it out… they make you dizzy, right?”
However, despite gaps in knowledge about PrEP among the participants, most expressed interest in the medication after receiving information about it during the interview. Participants often explained their interest in PrEP as stemming from the expected “psychological tranquility, more than anything” (P04).
In particular, participants highlighted that it would be beneficial in cases where alcohol or drugs influenced their decision to forego condoms. When asked about his interest in using PrEP, a 28-year-old participant explained:
P2: “[PrEP] would be useful for avoiding more infections, in a way, because we as [sex] workers sometimes drink alcohol and we forget to use a condom, or we take something, a drug, and then we forget to use a condom.”
Others acknowledged that they simply preferred not to use condoms with a particular type of partner, and PrEP would put them at ease when having condomless sex with these individuals. For example, one 24-year-old participant described always using condoms with clients, but when asked about his non-transactional, casual female sexual partners, he explained:
P21: “…a woman right now, if she wants to [use a condom] then no, and if she doesn’t, then no, and I normally don’t use a condom with women because that is what I like… I would feel a bit more secure that I have like a plan B…”
Notably, participants who did use condoms consistently commented that they may sometimes still be at risk for HIV. These participants highlighted risk situations which were unavoidable and noted that PrEP would help relieve concerns about HIV infection during these times. For example, when asked if he would be interested in using PrEP even though he always uses condoms with clients, one participant responded:
P03: “Of course, because one day you might unexpectedly feel the condom break, and you are already inside [the client], no?” (27 years old)
Similarly, another participant explained that he would be interested in PrEP when traveling abroad, because of a perceived increase in opportunities for both sex work and non-transactional sex, which might involve condomless sex, and therefore, present risk for HIV.
P2: “For me, using PrEP all of my life, I wouldn’t be about that. But, for example when I travel to countries where sexuality is more open, where the parties are bigger, where there is more work, like Germany, then there I would use [PrEP]…I would want to use PrEP to have more pleasure…I would only use it in places where I want to enjoy myself to the fullest or be totally liberated.” (28 years old)
Overall, participants uniformly saw value in PrEP for reducing concerns about HIV infection during instances planned or accidental condomless sex. This perceived value of PrEP stemmed from protecting themselves during times when they recognized that they were at increased risk for HIV infection.
Interest in PrEP Relating to Protecting Intimate Sexual Partners
Participants also commented that their interest in PrEP was rooted in a desire to protect their non-paying intimate partners from HIV infection. These participants recognized the importance of condoms when having sex with clients, but preferred to have condomless sex with their primary intimate partners. When asked about expected changes in sex work if he were to use PrEP, one 19-year-old participant responded:
P20: “I would take [PrEP] daily, more than anything because I have my girlfriend, we have relations, no? It’s, like, the well-being of both of us, no? Because I don’t just get involved with men, but also with my girl, right?”
A handful of participants were in relationships with other individuals who also sold sex. These individuals noted that PrEP would benefit both themselves and their partners, by preventing transmission of HIV between them. In response to being asked if his partner, also a sex worker, would mind if she knew he was taking PrEP, one participant responded:
P09: “No, because she knew since beforehand what I do, since she met me she knows what I work in. Likewise, I knew what she works in. On the contrary…I feel like it would protect me as much as her.” (36 years old)
Additionally, a minority of participants reported engaging in sex work seasonally or periodically. Among these men, some reported traveling to Mexico City only when specific clients contacted them, while others reported traveling to do sex work for a few months at a time, and returning to their home outside of the city when not performing sex work.
P15: “No, there are times when its temporary, like I take 2 or 3 months and then afterward I’ll leave for another 2 months, 3 months and come back and so on, every 3 months, for example.” (37 years old)
Most of these men had primary intimate partners back home, not all of whom knew about their sex work. These men expressed remorse at not being forthright about their sex work with their primary partners back home.
P14: “I want to have a home, a family, right? Yeah and it can only be if I’m well and being sincere, because I also can’t be deceiving my woman, and telling her that I’m here working, doing things that she doesn’t know about. I want to be, like be more direct already, right?” (29 years old)
Because of the clandestine nature of this seasonal sex work, these participants were interested in taking PrEP only as needed, or when traveling to Mexico City to perform sex work for a few months (and their usual place of residence was elsewhere). This interest in discrete intervals of PrEP use stemmed from wanting to protect their partners, as well as wanting their sex work to remain hidden from their family back home. As one 37-year-old participant stated when asked about using daily PrEP:
Interviewer: “Would you be willing to use this pill?”
P15: “Well in my case, only when I’m busy with work, of course, working in sex work, right?”
Interviewer: “So only when you are working at [sex work venue]”
P15. “Exactly!”
In summary, despite very limited foundational knowledge about PrEP for HIV prevention, participants expressed interest in using PrEP as a mechanism for preventing themselves from acquiring HIV and subsequently transmitting it to their intimate sexual partners. This interest was rooted in a desire to protect the partners themselves. Participants were particularly interested in PrEP use during periods when they perceived themselves to be at risk for HIV.
Expected Changes in Sexual Behavior
About one-third of participants reported that they expected having more condomless sex if they were using PrEP because of the protection it would provide. As one participant stated directly:
P4: “I think [PrEP] would be very useful, very useful, because it would give us peace of mind, more than anything…but, on the other hand, I also think that it would encourage me to accept more sex without a condom.” (30 years old)
Some of these participants indicated that they would continue to use condoms most of the time, but would not be as cautious, particularly when they were with a client they had worked with previously, or when they wanted the sensation of condomless sex, which was perceived as more pleasurable.
P11: “Yes of course. If I’m on PrEP and a good client that I trust a lot is asking that we don’t use a condom, probably yes.” (33 years old)
P11: “Probably [I would not use condoms], because I would let myself get carried away by the sensation. It is a very different feeling using a condom compared to ‘bareback’, no?”
Condomless sex while on PrEP was also contextualized in the presence of market inducements. Participants commented on the importance of condoms, but also noted that their economic needs caused them to accept anal sex with clients of unknown serostatus. In particular, participants mentioned that although they would not charge more for condomless sex while on PrEP, they would accept more clients of unknown serostatus.
P08: “Well, I think I would have a bit more clients…yes, because there wouldn’t be as much fear of running the risk of an infection or something like that, like getting an HIV infection or something. Yes, because you go out to work to get some money, you go, but well you never know what diseases he might have…” (23 years old)
Participants also noted that substance use altered their interest in using a condom. PrEP, in these instances, would provide peace of mind. As 36-year-old participant P18 responded when asked about expected changes in his sexual behavior if he were to use daily PrEP:
P18: “Well, since I know I’m taking something, I would stop doing it, well, I could also…. It might be that since I’m using [PrEP], I can feel safer, right? I do try [to use condoms], but when I don’t, well it has happened before, it was because of my state of sobriety, right?”
Interviewer: “So, would the frequency with which you use condoms change?”
P18: “Yes, even though I try to use condoms…”
Discussion
Our findings highlight inconsistent condom use among MSWs in Mexico City, despite acknowledgment of the HIV risk associated with condomless anal sex. Complex factors, including substance use, relationships with clients, monetary incentives, and misconceptions about HIV influenced participants’ decisions to use condoms with their clients. Notably, participants commented that considerations for using condoms with non-paying sexual partners differed from those for clients. Additionally, there was little baseline knowledge of, but high interest and perceived utility in using PrEP for HIV prevention among our sample. This was coupled with an expected increase among a number of participants in condomless anal sex if using PrEP, due to the perceived increase in pleasure and additional monetary incentives from some clients to forego condom use. Although there is some evidence of knowledge and interest in PrEP among MSM in the country overall (Edeza et al., 2019), this study marks the first qualitative exploration of perspectives on PrEP among male sex workers in Mexico, specifically.
Mexico has not yet adopted comprehensive PrEP guidelines, and it is not available through the public health system. The ongoing ImPrEP demonstration project, which began providing PrEP and related care to a limited number (n = 3000) of at-risk MSM in Mexico in 2018, marks the formal entry of the medication into the Mexican context. Notably, however, this demonstration project does not incorporate any adherence-promoting intervention beyond standard clinical counseling and is not intended to address any of the identified barriers to condom use among MSWs.
Given our findings regarding inconsistent condom use despite knowledge of HIV risk, interventions focused on adherence to PrEP may be especially important for this population. Optimal risk reduction for MSM through daily PrEP (~ 96%+) is obtained from 4 or more doses per week (Anderson et al., 2012); therefore, suboptimal adherence may not reduce the HIV risk inherent in condomless anal sex with multiple partners of unknown serostatus. Barriers to adherence among male sex worker communities in other contexts, including housing instability, substance use, economic need, and migration (Bacon et al., 2006; Baral et al., 2015; Boyer et al., 2017; Mimiaga et al., 2009; Nerlander et al., 2017) are mirrored in our sample and may also present challenges to optimal daily PrEP use in this context. As such, PrEP adherence interventions for MSWs will be critically important and should be implemented in conjunction with PrEP distribution through the formal healthcare system.
Additionally, a number of MSWs in Mexico City may be engaging in seasonal or episodic sex work, and therefore, may not be interested in PrEP when they are not performing sex work. These individuals may not be at risk for HIV when they are not performing sex work; many in our sample reported having female sexual partners with whom they were monogamous in their city of origin. Taking daily PrEP presents an additional risk of disclosure for those who perform seasonal sex work—their intimate partners could recognize the medication as being HIV-related, but would otherwise not have known about their sexual risk or sex work. Further, among those MSWs who travel for sex work with specific clients, there may be little incentive to adhere to PrEP and associated clinical care in the weeks or months between appointments with clients. Because of the unpredictability of these types of seasonal or episodic sex work, traditional PrEP implementation methods may fall short. Innovative prevention modalities such as episodic (Elsesser et al., 2016) or seasonal PrEP (Cremin, Morales, Jewell, O’Reilly, & Hallett, 2015) might be most effective for some individuals who intend to use PrEP only when actively performing sex work. These prevention modalities do raise additional concerns about best practices for monitoring adherence, as well as connecting MSWs to PrEP care during discontinuous periods of PrEP use, and as such further work is needed to explore the potential of these PrEP modalities to reach a subpopulation of MSWs who are not interested in consistent PrEP use, but still present periods of high risk for HIV infection.
Findings from this study should be taken in the context of some limitations. Firstly, despite the interviewer’s attempt to build rapport with participants and use neutral language, their responses to sensitive questions about sexual behaviors may have been influenced by social desirability bias, particularly since interviews were conducted in a formal clinical setting that emphasizes risk reduction. Additionally, our sample was recruited from a public venue at which outreach staff from Clinica Especializada Condesa often conduct HIV testing, or from the clinic itself; as such, participants may have been more closely linked to health services and more receptive to participating in an interview at a clinical setting. Further, interviews lasted approximately 45 min, which may not have been sufficient time for participants to fully process newly received information about PrEP for HIV prevention; relatedly, probes about seasonal sex work were added after several interviews had already been completed, as this was an emerging theme which begs to be explored further in future work. Lastly, Mexico City is the largest and wealthiest urban center in the country, and the context of male sex work in this city may be very different than in the rest of the country. Despite these limitations, this study represents the first qualitative assessment of knowledge and interest in PrEP among MSWs in Mexico, as well as one of the first to qualitatively explore drivers of inconsistent condom use in this same group.
Conclusion
Ongoing efforts to distribute PrEP to at-risk MSM and MSWs in Mexico should consider tailored prevention counseling to meet the needs of individuals who engage in different sexual behaviors according to their type of sexual partner, and to ensure that those most at risk for HIV are adequately protected. In light of complex barriers to consistent condom use and self-reported expected increases in condomless sex, in particular, implementation efforts should consider innovative approaches to PrEP use, such as episodic and seasonal PrEP, in addition to adherence-promoting interventions for MSWs. Regardless of the modality for implementation, it is clear from myriad reported complexities surrounding condom use during sex work that successful PrEP expansion efforts to this population will need to consider the complexity and varying nature of sexual risk among this group.
References
Anderson, P. L., Glidden, D. V., Liu, A., Buchbinder, S., Lama, J. R., Guanira, J. V., … Grant, R. M. (2012). Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Science Translational Medicine,4(151), 151ra125. https://doi.org/10.1126/scitranslmed.3004006.
Bacon, O., Lum, P., Hahn, J., Evans, J., Davidson, P., Moss, A., & Page-Shafer, K. (2006). Commercial sex work and risk of HIV infection among young drug-injecting men who have sex with men in San Francisco. Sexually Transmitted Diseases,33(4), 228–234. https://doi.org/10.1097/01.olq.0000204914.91923.ad.
Baral, S. D., Friedman, M. R., Geibel, S., Rebe, K., Bozhinov, B., Diouf, D., … Cáceres, C. F. (2015). Male sex workers: Practices, contexts, and vulnerabilities for HIV acquisition and transmission. The Lancet,385(9964), 260–273.
Biello, K. B., Oldenburg, C. E., Mitty, J. A., Closson, E. F., Mayer, K. H., Safren, S. A., & Mimiaga, M. J. (2017b). The “safe sex” conundrum: Anticipated stigma from sexual partners as a barrier to PrEP Use among substance using MSM engaging in transactional sex. AIDS and Behavior,21(1), 300–306. https://doi.org/10.1007/s10461-016-1466-y.
Biello, K. B., Thomas, B. E., Johnson, B. E., Closson, E. F., Navakodi, P., Dhanalakshmi, A., … Mimiaga, M. J. (2017a). Transactional sex and the challenges to safer sexual behaviors: A study among male sex workers in Chennai, India. AIDS Care,29(2), 231–238.
Boyer, C. B., Greenberg, L., Chutuape, K., Walker, B., Monte, D., Kirk, J., … Adolescent Medicine Trials Network. (2017). Exchange of sex for drugs or money in adolescents and young adults: An examination of sociodemographic factors, HIV-related risk, and community context. Journal of Community Health,42(1), 90–100. https://doi.org/10.1007/s10900-016-0234-2.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology,3(2), 77–101.
Centers for Disease Control. (2017). Hoja informativa sobre la PrEP [Press release]. Retrieved from https://www.cdc.gov/hiv/pdf/prep_gl_patient_factsheet_prep_spanish.pdf.
Choopanya, K., Martin, M., Suntharasamai, P., Sangkum, U., Mock, P. A., Leethochawalit, M., … Vanichseni, S. (2013). Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): A randomised, double-blind, placebo-controlled phase 3 trial. The Lancet,381(9883), 2083–2090. https://doi.org/10.1016/S0140-6736(13)61127-7.
Cremin, I., Morales, F., Jewell, B. L., O’Reilly, K. R., & Hallett, T. B. (2015). Seasonal PrEP for partners of migrant miners in southern Mozambique: A highly focused PrEP intervention. Journal of the International AIDS Society,18, 19946. https://doi.org/10.7448/IAS.18.4.19946.
Edeza, A., Galarraga, O., Novak, D., Mayer, K., Rosenberger, J., Mimiaga, M., & Biello, K. (2019). The role of sexual risk behaviors on PrEP awareness and interest among men who have sex with men in Latin America. Interntaional Journal of STD & AIDS. https://doi.org/10.1177/0956462419825944.
Elsesser, S. A., Oldenburg, C. E., Biello, K. B., Mimiaga, M. J., Safren, S. A., Egan, J. E., … Mayer, K. H. (2016). Seasons of risk: Anticipated behavior on vacation and interest in episodic antiretroviral pre-exposure prophylaxis (PrEP) among a large national sample of U.S. men who have sex with men (MSM). AIDS and Behavior,20(7), 1400–1407. https://doi.org/10.1007/s10461-015-1238-0.
Galárraga, O., & Sosa-Rubí, S. G. (2016). Male sex workers: HIV risk and behavioral economics. In S. Cunningham & M. Shah (Eds.), The Oxford handbook of the economics of prostitution (pp. 282–310). Oxford: Oxford University Press.
Galárraga, O., Sosa-Rubí, S. G., González, A., Badial-Hernández, F., Conde-Glez, C. J., Juárez-Figueroa, L., … Mayer, K. H. (2014). The disproportionate burden of HIV and STIs among male sex workers in Mexico City and the rationale for economic incentives to reduce risks. Journal of the International AIDS Society,17(1), 19218. https://doi.org/10.7448/IAS.17.1.19218.
Grant, R. M., Anderson, P. L., McMahan, V., Liu, A., Amico, K. R., Mehrotra, M., … Glidden, D. V. (2014). Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: A cohort study. The Lancet Infectious Diseases,14(9), 820–829. https://doi.org/10.1016/S1473-3099(14)70847-3.
Grant, R. M., Lama, J. R., Anderson, P. L., McMahan, V., Liu, A. Y., Vargas, L., … Glidden, D. V. (2010). Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New England Journal of Medicine,363(27), 2587–2599. https://doi.org/10.1056/NEJMoa1011205.
Grov, C. (2014). Male clients of male escorts: Satisfaction, sexual behavior, and demographic characteristics. Journal of Sex Research,51(7), 827–837. https://doi.org/10.1080/00224499.2013.789821.
Infante, C., Sosa-Rubi, S. G., & Cuadra, S. M. (2009). Sex work in Mexico: Vulnerability of male, travesti, transgender and transsexual sex workers. Culture, Health & Sexuality,11(2), 125–137. https://doi.org/10.1080/13691050802431314.
Kojima, N., Davey, D. J., & Klausner, J. D. (2016). Pre-exposure prophylaxis for HIV infection and new sexually transmitted infections among men who have sex with men. AIDS,30(14), 2251–2252. https://doi.org/10.1097/qad.0000000000001185.
Legard, R., Keegan, J., & Ward, K. (2003). In-depth interviews. Qualitative Research Practice: A Guide for Social Science Students and Researchers,6(1), 138–169.
McCormack, S., Dunn, D. T., Desai, M., Dolling, D. I., Gafos, M., Gilson, R., … Gill, O. N. (2016). Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): Effectiveness results from the pilot phase of a pragmatic open-label randomised trial. The Lancet,387(10013), 53–60. https://doi.org/10.1016/S0140-6736(15)00056-2.
Mgbako, O., Park, S. H., Mayer, K. H., Schneider, J. A., Goedel, W. C., Hambrick, H. R., & Duncan, D. T. (2019). Transactional sex and preferences for pre-exposure prophylaxis (PrEP) administration modalities among men who have sex with men (MSM). Journal of Sex Research, 56, 650–658. https://doi.org/10.1080/00224499.2018.1449190.
Mimiaga, M. J., Reisner, S. L., Tinsley, J. P., Mayer, K. H., & Safren, S. A. (2009). Street workers and internet escorts: Contextual and psychosocial factors surrounding HIV risk behavior among men who engage in sex work with other men. Journal of Urban Health: Bulletin of the New York Academy of Medicine,86(1), 54–66. https://doi.org/10.1007/s11524-008-9316-5.
Monteiro, J. F. G., Marshall, B. D. L., Escudero, D., Sosa-Rubí, S. G., González, A., Flanigan, T., … Galárraga, O. (2015). Preventing HIV transmission among partners of HIV-positive male sex workers in Mexico City: A modeling study. AIDS and Behavior,19(9), 1579–1588. https://doi.org/10.1007/s10461-014-0915-8.
Nerlander, M. L., Hess, K. L., Sionean, C. E., Rose, C., Thorson, A., Broz, D., & Paz-Bailey, G. (2017). Exchange sex and HIV infection among men who have sex with men: 20 US Cities, 2011. AIDS and Behavior,21(8), 2283–2294. https://doi.org/10.1007/s10461-016-1450-6.
Oldenburg, C. E., Biello, K. B., Colby, D., Closson, E. F., Nguyen, T., Trang, N. N., … Mimiaga, M. J. (2014). Engagement with peer health educators is associated with willingness to use pre-exposure prophylaxis among male sex workers in Ho Chi Minh City, Vietnam. AIDS Patient Care and STDs,28(3), 109–112.
Pan American Health Organization. (2017). HIV prevention in the spotlight. An analysis from the perspective of the health sector in Latin America and the Caribbean, 2017. Retrieved from http://iris.paho.org/xmlui/handle/123456789/34381.
Restar, A. J., Tocco, J. U., Mantell, J. E., Lafort, Y., Gichangi, P., Masvawure, T. B., … Sandfort, T. G. (2017). Perspectives on HIV pre-and post-exposure prophylaxes (PrEP and PEP) among female and male sex workers in Mombasa, Kenya: Implications for integrating biomedical prevention into sexual health services. AIDS Education and Prevention,29(2), 141–153.
Underhill, K., Morrow, K. M., Colleran, C. M., Holcomb, R., Operario, D., Calabrese, S. K., … Mayer, K. H. (2014). Access to healthcare, HIV/STI testing, and preferred pre-exposure prophylaxis providers among men who have sex with men and men who engage in street-based sex work in the US. PLoS ONE,9(11), e112425. https://doi.org/10.1371/journal.pone.0112425.
Yi, S., Tuot, S., Mwai, G. W., Ngin, C., Chhim, K., Pal, K., … Mburu, G. (2017). Awareness and willingness to use HIV pre-exposure prophylaxis among men who have sex with men in low- and middle-income countries: A systematic review and meta-analysis. Journal of the International AIDS Society,20(1), 21580. https://doi.org/10.7448/ias.20.1.21580.
Funding
The funding for this study was received from NIH/NIMH Research Supplement to Promote Diversity in Health-Related Research (3R34MH110369-02S1), Brown University Minority Health and Health Disparities International Research Training Program, and NIH/NIMH Planning Grant “Prep Seguro: Antiretroviral-Based HIV Prevention Among Men at High Risk in Mexico” (5R34MH114664-02).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
We declare no ethical issues observed in data collection or analyses. All study procedures and documents were approved by the Ethics Committee at the Mexican National Institute of Public Health (Comité de Ética en Investigación del Instituto Nacional de Salud Pública), in Cuernavaca, Mexico.
Informed Consent
All participants provided verbal informed consent prior to participating in study procedures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Edeza, A., Galárraga, O., Santamaria, E.K. et al. “I Do Try To Use Condoms, But…”: Knowledge and Interest in PrEP Among Male Sex Workers in Mexico City. Arch Sex Behav 49, 355–363 (2020). https://doi.org/10.1007/s10508-019-01473-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-019-01473-4