Abstract
Apoptosis is an inevitable process during development and is evident in the formation of articular cartilage and endochondral ossification of growth plate. Mesenchymal stem cells (MSCs) can serve as alternative sources for cell therapy in focal chondral lesions or diffuse osteoarthritis. But there are few, if any, studies investigating apoptosis during chondrogenesis by MSCs. The aim of this study was to find the better condition to prevent apoptosis during chondrogenesis by MSCs. Apoptosis were evaluated in MSCs induced in different chondrogenic media by the use of Annexin V, TUNEL staining, lysosomal labeling with lysotracker and immunostaining of apoptotic markers. We found apparent apoptosis was demonstrated by Annexin V, TUNEL staining and lysosomal labeling during chondrogenesis. Meanwhile, the degree of apoptosis was related to the reagents of the defined chondrogenic medium. Adding serum in medium increased apoptosis, however, TGF-β1 inhibited apoptosis. The apoptosis was associated with the activation of caspase-3, the increase in the Bax/Bcl-2 ratio, the loss of lysosomal integrity, and the increase of PARP-cleavage. Pro-inflammatory cytokines, IL-1α, IL-1β and TNFα did not induce any increase in apoptosis. Interestingly, the inhibition of apoptosis by serum free medium supplemented with ITS was also associated with an increase in the expression of type II collagen, and a decrease in the expression of type X collagen, Runx2, and other osteogenic genes, while TGF-β1 increased the expression of Sox9, type II and type X collagen and decreased the expression of osteogenic genes. These data suggest apoptosis occurs during chondrogenesis by MSCs by cell death intrinsic pathway activation and this process may be modulated by culture conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Because of the lack of blood supply and subsequent wound-healing response of articular cartilage, repair of focal chondral lesions or diffused osteoarthritis by local chondrocytes has shown a disappointing result. The rapidly emerging field of stem cell technology holds great promise for regenerating functional tissue constituents by therapies based on cells with or without genetic modification. Mesenchymal stem cells or marrow stromal cells (MSCs) are an attractive cell source for cartilage repair, because they are readily available from patients, easily expanded in culture and able to undergo differentiation into mesenchymal tissues such as bone, fat and cartilage [1, 2].
For in vitro chondrogenesis, MSCs are maintained at a high density in pellets and cultured in a defined medium, prompting MSCs to differentiate and form three-dimensional (3D) structures expressing a series of chondrogenic genes [3] and synthesizing chondrogenic matrices such as type II collagen and aggrecan [4, 5]. The defined media used to induce chondrogenesis by MSCs are originally derived from the media for a prechondrocyte condensation in avian and mammalian embryonic cells, that is, a DMEM or α-MEM based medium supplemented with ITS-premix in the presence of certain growth factors [6, 7]. Despite the importance and the frequency in using it for chondrogenic induction of MSCs, there are few, if any, studies aimed at selecting and comparing the components used in the medium [8].
Chondrogenesis by MSCs consists of a life cycle of proliferation, cell condensation, chondrogenesis with the expression of aggrecan and type II collagen, hypertrophy change with the expression of type X collagen, and endochondral ossification with calcification and the deposition of calcium phosphate; the rate of each process depends on temporal and spatial cues within the microenvironments in vivo or in vitro. These differentiation events are usually accompanied by a programmed cell death [9], and the homeostatic maintenance of cellularity is destroyed both in chondral lesions and osteoarthritis [10–12].
Vascularization mediated by angiogenic factors plays an essential role in endochondral ossification through the induction of coupling resorption of cartilage with bone formation [13]. Conditional knockout (CKO) of vascular endothelial growth factor (VEGFA) also delayed invasion of blood vessels and delayed removal of terminal hypertrophic chondrocytes during embryonic bone development [14]. In contrast, VEGFA is crucial of chondrocyte survival, since massive cell death was seen in joint and epiphyseal region of VEGFA CKO endochondral bones [14]. Decrease in vascularization causes a decrease in blood flow. A recent report demonstrated short-term exposure of cartilage to blood resulted in chondrocyte apoptosis [15]. However, there are few, if any, papers mentioned the effects of blood components such as serum on chondrocyte survival.
In the current study, we hypothesized apoptosis occurred in the pellet cultures of chondrogenesis and aimed to find the better protocol to achieve chondrogenesis by MSCs by comparing the degree of apoptosis in different chondrogenic defined media, which were designed by modifying the components frequently used for the induction of chondrogenesis. We described which apoptotic pathway is involved in chondrogenesis by MSCs and especially compared the effects of serum, growth factors and cytokines on inducing apoptosis during chondrogenesis by MSCs.
Materials and methods
Cells
This study was approved by the Institutional Review Board of the Taipei Veterans General Hospital (94-05-16A). The MSCs were originally cultured from the bone marrow with protocols described previously [16], and immortalized by retroviral transduction with human papilloma virus E6E7 genes [17]. All the cells were maintained in Dulbecco’s modified Eagle’s medium containing 1 g/L of glucose (DMEM-LG; Gibco; Grand Island, NY), 100 U/mL penicillin, 10 μg/mL streptomycin, 0.25 μg/mL amphotericin B and 10% fetal bovine serum (FBS) of a pre-selected commercial lot (Gibco), and grown in 37°C incubator under 5% CO2 atmosphere with medium change twice per week. Even after long passage in culture, they behave like early passages of MSCs and maintain the potential for osteogenic, adipogenic and chondrogenic differentiation by protocols as described previously [17]. The chondrogenic potential of the cells has also been well demonstrated and investigated using collagen gel and pellet culture methods [18, 19].
Pellet cultures for chondrogenesis
Aliquots of MSCs 2.5 × 105 cells in 2 mL growth medium were spun down at 500 g for 10 min. The pelleted cells were incubated at 37°C, 5% CO2. After overnight incubation, the cells formed an essentially spherical aggregate that did not adhere to the walls of the tube. The FBS containing medium was then replaced with one of five defined chondrogenic media, DMEM-LG medium containing 10−7 M dexamethasone (Sigma) and 50 μg/mL ascobate-2-phosphate (Sigma), supplemented without [Serum-free medium: SF] or with 10% FBS [Serum-contained medium: SC] or ITS (Gibco) [Serum-free medium plus ITS: SF + ITS], without or with 10 ng/mL TGF-β1 (PreproTech) [Serum-contained medium plus TGF: SC + TGF, Serum-free medium plus ITS and TGF: SF + ITS + TGF]. Medium changes were carried out at 2- to 3-day intervals and pellets were harvested for further analysis at time points up to 21 days.
Evaluation of cell number, viability, and apoptosis
MSCs grown in monolayer and pellets cultured in SF, SC, SC + TGF, SC + ITS, and SF + ITS + TGF medium for 1 week were harvested, washed twice with PBS, and treated in collagenase I (Sigma) in Hank’s Buffered Salt Solution (HBSS) for 3 h at 37°C. The cells were then washed with PBS and resuspended in 400 μl of PBS. Trypan blue exclusion method was used to analyze the ratio of viability and the total viable cells for each pellet. Flow cytometric analysis of Annexin-V staining to detect the exposure of phosphatidylserine in apoptotic cells was performed using an Annexin-V-fluos kit (Roche, Indianapolis, IN). Otherwise, the pellets at 3 weeks were harvested, washed twice with PBS, fixed in 4% paraformaldehyde for 3 h at RT, and prepared for paraffin embedding. The 4 μm-thickness sections were used for TUNEL staining to detect the specific immuno-staining of the high concentrations of DNA 3′-OH ends in apoptotic cell.
Analysis of loss of lysosomal integrity
The micromass cultures were incubated with the fluorescent dye LysoTracker Red DND-99 (Invitrogen) at 75 nM for 1 h at 37°C as modified from previously described [20]. Lack of lysosomal retention of Lysotracker detected as decreased intensity of fluorescence which was determined by a fluorescence-equipped microscope.
Alcian blue staining, sirius red staining, and immunohistochemistry
The 4 μm-thickness sections were stained for H&E, Alcian blue staining, Sirius red staining, and also processed for immunohistochemistry. Alcian blue staining was performed with a standard protocol, and the stained sections were used for determination of cellularity, empty lacunae counts, and the presence of fibrillation. For the analysis of collagen expression with Sirius red staining, sections were rinsed with distilled water and incubated with 0.1% Sirius red in saturated picric acid for 90 min. Sections were rinsed 2 times with 0.01 N HCl for 1 min and then immersed in distilled water. After dehydration with 70% ethanol for 30 s, the sections were observed under polarized light after coverslipping. Immunohistochemistry studies were done to stain for activated caspase-3, Bcl-2, Bax, and type II collagen. For immunohistochemistry, paraffin sections were initially treated with blocking serum for 20 min, then incubated with first antibodies, reacted with horse radish peroxidase- or alkaline phosphatase-conjugated secondary antibodies, and finally processed for substrate reaction (Vector).
Western blot analysis of PARP, Bcl-2, and Bax
Pellets were lysed for 30 min in ice-cold 0.1 M PBS with 1% NP40, 0.5% sodium deoxycholate, 0.1% sodium dodecyl sulfate (SDS), 0.1 mg/mL phenylmethylsulfonyl fluoride, 30 μl/mL aprotinin, and 1 mM sodium orthovanadate (all from Sigma). The suspension was carefully homogenized with a loose pestle, followed by sonication. Total cell lysates was obtained by centrifugation at 8000 g for 30 min at 4°C. Aliquots of 20 μg lysates were separated in 10% SDS-polyacrylamide gel electrophoresis (SDS-PAGE) and electroblotted onto a PVDF filter. The membrane was hybridized with antibody against carboxyl-terminus of PARP, Bcl-2 and Bax. The filter was then exposed to chemiluminescent detection system (Perkin-Elmer Instruments, Inc.). The autoradiographs were then scanned and quantified by densitometry using Intelligent Quantifier software (BioImage Systems Corp., Ann Arbor, MI).
Quantitative RT-PCR
The method of real-time RT-PCR was performed as described [21]. Briefly, total RNA (1 μg) of each sample was reversely transcribed in 20 μL using 0.5 μg of oligo dT and 200 U Superscript III RT (Invitrogen, Carlsbad, CA). The amplification was carried out in a total volume of 25 μL containing 0.5 μM of each primer, 4 mM MgCl2, 12.5 μL of LightCycler™–FastStart DNA Master SYBR green I (Roche Molecular Systems, Alameda, CA) and 10 μL of 1:20 diluted cDNA. PCR reactions were prepared in duplicate and heated to 95°C for 10 min followed by 40 cycles of denaturation at 95°C for 15 s, annealing at 60°C for 1 min, and extension at 72°C for 20 s. Standard curves (cycle threshold values versus template concentration) were prepared for each target gene and for the endogenous reference (GAPDH) in each sample. The quantification of the unknown samples was performed by the LightCycler Relative Quantification Software version 3.3 (Roche) Table 1.
Statistics
Data and results are reported as means ± SD. Statistical comparisons between two groups were performed with unpaired Student’s t test.
Results
Chondrogenesis of MSCs
To confirm the ability of MSCs to undergo chondrogenesis, aliquots of 2.5 × 105 cells were centrifuged to form pellets and induced in serum-free medium by adding ITS + Premix in the presence of TGF-β1, dexamethasone, ascorbate-2-phosphate. Paraffin sections of pellets at 3 weeks of induction showed spherical cells with extracellular matrices stained by Alcian blue and type II collagen immunostaining (Fig. 1a). Quantitative RT-PCR further confirmed the expression of aggrecan, Cartilage Oligomeric Matrix Protein (COMP), and Col10A1 was increased in the 3-week induced pellets, compared with the control culture that was not induced for differentiation (Fig. 1b). These data confirmed the chondrogenic potential of MSCs used here.
Chondrogenesis by human mesenchymal stem cells. Pellets from aliquots of 2.5 × 105 MSCs were induced in DMEM-LG containing 10−7 M dexamethasone and 50 μg/mL ascobate-2-phosphate, supplemented with ITS and 10 ng/mL TGF-β1. a Alcian blue staining and immunohistochemistry demonstrate the synthesis of proteoglycan and type II collagen at 3 weeks of induction. (40 × original magnification) b Quantitative RT-PCR demonstrates the expression of aggrecan, COMP and Col10A1 in pellets at 3 weeks of induction (Chond), but not in un-induced pellets (CTR)
Cell number decreases during chondrogenesis by MSCs
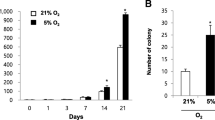
Since there are few, if any, studies examining the effects of various defined media on cell number changes and viability during chondrogenesis by MSCs, we induced aliquots of 2.5 × 105 cells in five different chondrogenic defined media and analyzed cell number and viability using the trypan blue exclusion method. At 1 week of induction, the average cell numbers recovered from pellets in SF, SC, SC + TGF, SF + ITS and SF + ITS + TGF media (details are given in “materials and methods”) were 4.13 × 104, 6.13 × 104, 3.73 × 104, 5.6 × 104 and 9.6 × 104, respectively, and the average viability was 51.6, 34.8, 32.1, 64.3 and 56.7%, respectively. These data suggest each medium induced a great loss of cell number and caused cell death during chondrogenesis by MSCs. Among them, pellets induced in serum contained media (SC and SC + TGF) were decreased in total viable cell number and viability compared with pellets in serum free media, (SF, SF + ITS and SF + ITS + TGF), while the supplement of ITS (SF + ITS and SF + ITS + TGF) increased the viability compared with SF (Fig. 2a). These data suggest serum-contained media induced the greatest loss in cell number or induced cell death, while the supplement of ITS increased the viability during chondrogenesis.
Cell death and apoptosis occurred during chondrogenesis by human mesenchymal stem cells. Pellets from aliquots of 2.5 × 105 MSCs were cultured in five different chondrogenic media. At 1 week of induction, cells were recovered and evaluated using trypan blue exclusion method for measuring the percentage of viable and dead cells (a Left panel) and the total viable cell numbers (a Right panel). b Cells were also assayed with Annexin V/PI staining to measure the percentage of viable cells (Annexin V-/PI-), early apoptotic cells (Annexin V +/PI-), late apoptotic cells (Annexin V +/PI +), and necrotic cells (Annexin V-/PI +). Representative data from three independent experiments are shown. c At 3 weeks of induction, paraffin sections of pellets were examined by TUNEL assay to evaluate the degree of apoptosis. (40 × original magnification)
MSCs undergo apoptosis during chondrogenesis
We then examined if the cell death was because of an increase in apoptosis during chondrogenesis. Cells were recovered from pellets at 1 week of induction and evaluated with Annexin V/PI staining. Pellets induced in serum contained media (SC and SC + TGF) were more stained by Annexin V than pellets induced in serum free media with the supplement of ITS (SF + ITS and SF + ITS + TGF) (Fig. 2b). For topographical analysis of apoptosis in chondrogenesis, the TUNEL staining was used to determine apoptosis in sections of the 3-week pellets. Similarly, all the pellets cultured in the five induction media were stained by TUNEL. Pellets grown in serum contained medium either in the presence of TGF-β1 (SC + TGF) or not (SC) were strongly stained by TUNEL. Pellets cultured in SC had the highest staining for TUNEL. Adding TGF-β1 into either serum containing or serum-free medium reduced TUNEL staining in the peripheral regions (Fig. 2c). No cells were found positive for PCNA further excluded the possibility that positive for TUNEL was due to the temporary DNA breaks associated DNA replication (Supplementary Fig. 1). These data indicated pellet culture for chondrogenesis by MSCs induced apoptosis, which could be partly alleviated by adding TGF-β1.
Apoptosis is associated with the activation of caspase-3, the loss of lysosomal integrity, the cleavage of PARP, and an increase in Bax/Bcl-2 ratio
To identify the pathways of apoptosis during chondrogenesis by MSCs, we first examined the same pathways taken by the apoptosis of mature chondrocytes. Apoptosis of chondrocyte in experimental and clinical osteoarthritis is mediated by caspase-3 activation, loss of lysosomal integrity with release of lysosomal enzymes, increasing Bax, and the cleavage of poly (ADP-ribose) polymerase (PARP) [11, 22–25], therefore, the expression of activated caspase-3 protein was first evaluated by immunohistochemistry (Fig. 3a). The intensity of activated caspase-3 immunostaining in SC and SC + TGF groups was greater than in SF + ITS and SF + ITS + TGF groups, consistent with TUNEL staining. Expression of the Bcl-2 protein was increased in pellets induced in SF + ITS and SF + ITS + TGF media, while Bax protein was mainly expressed in SC medium (Fig. 3a). Lysosomal labeling with lysotracker revealed the groups induced in serum contained medium (SC, SC + TGF) decreased in the labeling of lysotracker, while the groups induced in serum free medium plus ITS (SF + ITS, SF + ITS + TGF), especially in the presence of TGF-β1 increased in the labeling of lysotracker (Fig. 3b), suggesting the lysosomal integrity was inhibited by serum and stimulated by TGF-β1. Western blot analysis further demonstrated an increase of Bcl-2 in SF + ITS and SF + ITS + TGF media, while Bax protein was increased in SC medium (Fig. 3c). The average Bax/Bcl-2 ratios were 17.3-fold and 8.9-fold for SC and SC + TGF, respectively, and 4.1-fold and 3.1-fold for SF + ITS and SF + ITS + TGF, respectively (Fig. 3d). PARP, a DNA binding protein involved in base excision repair, is recognized as a specific substrate of caspase-3. The proteolytic activation of PARP by apoptosis results in its cleavage from 116 to 85 kDa. Induction of cells in SF + ITS and SF + ITS + TGF for 2 weeks showed minimum PARP cleavage, and SF, SC and SC + TGF resulted in slight increases in PARP cleavage (Fig. 3c and e). These data together suggested pellet culture-dependent apoptosis was associated with the activation of caspase-3, the loss of lysosomal integrity, an increase in Bax/Bcl-2 ratio, and PARP-cleavage, which were all inhibited by serum free medium supplemented with ITS and the addition of TGF-β1.
Expression of pro-apoptotic and anti-apoptotic markers during chondrogenesis by human mesenchymal stem cells. Pellets from aliquots of 2.5 × 105 (a) or 2.5 × 105 (b) MSCs were induced in five chondrogenic media. a Immunohistochemistry demonstrates the expression of activated caspase-3, Bcl-2 and Bax proteins at 3 weeks of induction. (200 × original magnification) b Lysotracker staining demonstrates the integrity of lysosome at 2 weeks of induction. Upper and lower pictures are from the same field. (80 × original magnification) c Western blotting demonstrates the expression of Bcl-2 and Bax proteins and the cleavage of PARP at 2 weeks of induction. d Ratio of Bax/Bcl-2 protein calculated from three individual blots. e Ratio of PARP cleavage calculated from three individual blots
Apoptosis is not associated with cell density and pro-inflammatory cytokines
Because chondrocytes in monolayer culture undergo apoptosis and the degree of apoptosis is related to cell density [26], we then assayed the percentage of MSCs expressing apoptosis marker in monolayer culture. MSCs underwent apoptosis neither in low density nor in confluence with the monolayer culture (data not shown). Because it was reported apoptosis of chondrocytes is induced by several pro-inflammatory cytokines [27], IL-1α, IL-1β and TNF-α were selected to understand their effects on apoptosis in mesenchymal chondrogenesis. Treating MSCs in SF + ITS media with IL-1α, IL-1β and TNF-α at 10 ng/mL, however, did not induce any increase in TUNEL staining, immunostaining for activated caspase-3, Bcl-2 and Bax (Fig. 4), suggesting apoptosis in chondrogenesis is not induced by the pro-inflammatory cytokines. The diversity in the degree of apoptosis responding to different conditions suggests the apoptosis of these chondrogenic cells may be cell type and context specific.
Effects of pro-inflammatory cytokine on apoptosis and the expression of pro-apoptotic and anti-apoptotic markers during chondrogenesis by human mesenchymal stem cells. Pellets from aliquots of 2.5 × 105 MSCs were induced in SF + ITS medium without or with TGF-β1 (10 ng/mL), in the absence or presence of IL-1α, IL-1β and TNF-α. Immunohistochemistry demonstrates the expression of TUNEL, activated caspase-3, Bcl-2 and Bax proteins at 3 weeks of induction. (200 × original magnification)
Effects of medium supplements on pellet size change and the expression of chondrogenic matrices
To investigate the effects of medium supplements on pellet size changes, we measured the pellet size at 1, 2 and 3 weeks of induction. The size significantly decreased along with the culture period in SF, SC and SC + TGF, but did not change in SF + ITS and SF + ITS + TGF groups (Supplementary Fig. 2). The decrease in pellet size in SF, SC and SC + TGF correlated with their increase of cell death and apoptosis, suggesting apoptosis and cell death caused the decrease in pellet size. We further investigated the effects of medium supplements on the expression of chondrogenic matrices. Except the pellets cultured in SF medium, pellets cultured in all the other media were positive for Sirius red staining, Alcian blue staining, and type II collagen immunostaining (Fig. 5a). Further, quantitative RT-PCR demonstrated the expression of Sox9 by all of the pellets, and of Col2A1 by pellets cultured in all the media except the SF medium, while the expression of Col0A1 was demonstrated in all the media except a very small expression in SF + ITS medium (Fig. 5b). Compared with the serum-contained media, SF + ITS media not only decreased in apoptosis but also increased in the Alcian blue staining, Sirius red staining, and the expression of Col2A1, but decreased in the expression of Col10A1, Runx2, osteocalcin and bone sialoprotein (SC vs SF + ITS; SC + TGF vs SF + ITS + TGF) (Fig. 5b and c). Interestingly, adding TGF-β1 also induced an increase in Alcian blue staining, Sirius red staining, and immunostaining for type II collagen, especially in the peripheral of pellets cultured in SF + ITS media (Fig. 5a). Similar with the effects on increasing chondrogenic matrices, TGF-β1 increased the expression of Sox9, Col2A1 and Col10A1 and decreased the expression of osteocalcin and bone sialoprotein (Fig. 5b). These data suggest serum free media supplemented with ITS or with the addition of TGF-β1 increased the expression/synthesis of chondrogenic matrices and decrease the expression of osteogenic genes.
Expression of chondrogenic proteins during chondrogenesis by human mesenchymal stem cells. Pellets from aliquots of 2.5 × 105 MSCs were induced in five different chondrogenic media. a Sirius red, Alcian blue staining and immunohistochemistry demonstrate the synthesis of proteoglycan and type II collagen at 3 weeks of induction. (40 × original magnification) b Quantitative RT-PCR demonstrates the expression of Sox9, Col2A1 and Col10A1 at 1 week of induction. c Quantitative RT-PCR demonstrates the expression of Runx2, bone sialoprotein (BSP) and osteocalcin (OC) at 3 weeks of induction. (*p < 0.05 and **p < 0.01s determined by the Student’s t test.)
Discussion
MSCs capable of cell renewal and differentiating into mesenchymal tissues are considered potential sources of cell therapy in the damage and degeneration of muscular skeletal system, such as the chondral lesion or osteoarthritis. Several induction media have been used for chondrogenesis by MSCs; however their effects on apoptosis during chondrogenesis were not thoroughly examined. In the current report, we demonstrated apoptosis occurred during chondrogenesis by MSCs in all the tested media, suggesting apoptosis is a common phenomenon of in vitro chondrogenesis. These results support the in vivo findings that apoptosis is an inevitable process during development and is evident in the formation of articular cartilage and endochondral ossification of the growth plate.
Our data demonstrated MSCs grown in monolayer revealed no obvious apoptosis. In contrast, apparent apoptosis was noted in pellet cultures of chondrogenesis by MSCs. Meanwhile, the degree of apoptosis was found to be related to the reagents of defined chondrogenic medium. Further, the decrease in apoptosis was associated with an increase in the expression of chondrogenic proteins such as type II collagen and aggrecan. These data suggest changing the components of the defined medium could control the apoptosis and the degree of chondrogenesis. Besides, apoptosis noted during chondrogenesis by MSCs was mediated by multiple apoptosis pathways, including activation of caspase-3, loss of lysosomal integrity, increase in pro-apoptotic protein, Bax, and cleavage of PARP. Therefore, molecules or signaling pathways modulating these apoptotic pathways may be applied for modulating apoptosis and differentiation efficiency in the chondrogenesis of MSCs.
The role of apoptosis in postnatal articular cartilage damage and degeneration has been implicated in osteoarthritis, consisting of a range of biomechanical, biochemical, and genetic factors [28] converging in a final common pathway [29] characterized by a progressive focal loss of articular cartilage. Normal cartilage homeostasis and structural integrity depend on chondrocytes [30], preserving the dynamic equilibrium between production of the extracellular matrix and its enzymatic degradation. Thus, chondrocyte viability is essential for maintaining the integrity of articular cartilage, and reduced cellularity (attributable to either necrosis or apoptosis) may predispose the aging individual to matrix degeneration and be associated with the onset and/or progression of osteoarthritis. In addition, the apoptosis noted in cartilage degeneration was also mediated by the similar pathways demonstrated in chondrogenesis by MSCs [11, 22–24], thus chondrogenesis by MSCs may serve as the in vitro model to study chondrocyte apoptosis in osteoarthritis.
The clear differences in apoptosis noted between monolayer growing and suspension differentiated MSCs may incur a concern that was the serum-free culture condition rather than chondrogenesis induced apoptosis in these cells. This concern could be excluded by a report which examined chondrocyte apoptosis in serum-free suspension culture finding commitment chondrocytes instead of noncommitment chondrocytes undergoing apoptosis [9]. These results together point out the differentiation status rather than culture condition induces apoptosis in chondrocyte and chondrogenic differentiated MSCs.
Vascularization mediated by VEGFA delayed invasion of blood vessels and removal of terminal hypertrophic chondrocytes during embryonic bone development [13, 14]. However, VEGFA is also crucial of chondrocyte survival in joint and epiphysel cartilages [14, 31]. These data are inconsistent in the effect of vascularization on chondrocyte survival. Recently, the involvement of angiogenesis in the development of osteoarthritis with loss of cartilage thickness has been documented by a lot of reports [32]. In the current study, we investigated the effect of serum, one component of blood and noted a significant increase in apoptosis and decrease in pellet size in the groups that contained serum (SC and SC + TGF) as compared to the groups those were induced without serum (SF + ITS and SF + ITS + TGF), suggesting the negative effect of serum on chondrocyte survival. These data were supported by an animal study which demonstrated the exposure of articular cartilage to blood induced degeneration of articular cartilage [33]. Thus, factors contained in serum or blood may have disadvantageous effects in immature or mature chondrocytes.
Although, the effects of pro-inflammatory cytokines such as TNFα and IL-1 on apoptosis have been studied in articular chondrocytes derived from normal [34], inflammatory [35], and osteoarthrotic joints [36] and hypertrophic chondrocytes undergoing endochondral ossification [37], there was no report mentioned their effects on the survival of MSCs undergoing chondrogenic differentiation. In addition, these reports did not reach a conclusion, some with negative effects [37], some with positive effects [35] and some without any effects on chondrocyte survival [34]. The current studies did not observe any effects of TNF-α, IL-1α, and IL-1β on the survival of MSCs undergoing chondrogenesis, supporting that the effects of these cytokines on chondrocytes survival are cell and text dependent.
Previous studies have successfully demonstrated the anti-apoptotic and anti-differentiation effects of TGFs and BMPs via the canonical Smad pathway [38] on chondrocytes in joint or epiphyseal plate and stages 25–26 chick embryonic mesenchyme [39, 40]. The inhibition of apoptosis by TGFs and BMPs causes a decrease in terminal hypertrophic differentiation of chondrocytes plays an essential role for maintaining normal articular cartilage [38]. Our data demonstrated apoptosis occurred during chondrogenesis or induced by serum in MSCs was associated with multiple apoptosis pathways and was inhibited by TGF-β1. Aside from, TGF-β1 also increased the expression/synthesis of chondrogenic matrices and decreased the expression of osteogenic genes. These results and previous reports suggest the positive roles of TGF-β-1 in the survival of chondrocytes and MSCs undergoing chondrogenesis, while TGF-β-1 induced apoptosis has been demonstrated in cells such as lymphocytes and hepatocytes [41, 42]. Thus, further studies should be conducted in the future for the underlying mechanisms that TGF-β-1 mediated the opposite effects on apoptosis of these cells. In summary, apoptosis occurring during chondrogenesis by MSCs is mediated by multiple pathways and can be modulated by reagents added in the define media. Therefore, to identify reagents or molecules that can modulate the apoptosis pathway during chondrogenesis by MSCs may help in applying MSCs to repair and regenerate chondral lesions or osteoarthritis.
References
Caplan AI (1991) Mesenchymal stem cells. J Orthop Res 9:641–650
Pittenger MF, Mackay AM, Beck SC et al (1999) Multilineage potential of adult human mesenchymal stem cells. Science 284:143–147
Sekiya I, Vuoristo JT, Larson BL, Prockop DJ (2002) In vitro cartilage formation by human adult stem cells from bone marrow stroma defines the sequence of cellular and molecular events during chondrogenesis. Proc Natl Acad Sci U S A 99:4397–4402
Johnstone B, Hering TM, Caplan AI, Goldberg VM, Yoo JU (1998) In vitro chondrogenesis of bone marrow-derived mesenchymal progenitor cells. Exp Cell Res 238:265–272
Mackay AM, Beck SC, Murphy JM, Barry FP, Chichester CO, Pittenger MF (1998) Chondrogenic differentiation of cultured human mesenchymal stem cells from marrow. Tissue Eng 4:415–428
Caplan AI, Stoolmiller AC (1973) Control of chondrogenic expression in mesodermal cells of embryonic chick limb. Proc Natl Acad Sci U S A 70:1713–1717
Denker AE, Nicoll SB, Tuan RS (1995) Formation of cartilage-like spheroids by micromass cultures of murine C3H10T1/2 cells upon treatment with transforming growth factor-beta 1. Differentiation 59:25–34
Tateishi K, Ando W, Higuchi C et al (2008) Comparison of human serum with fetal bovine serum for expansion and differentiation of human synovial MSC: potential feasibility for clinical applications. Cell Transplant 17:549–557
Gibson G, Lin DL, Roque M (1997) Apoptosis of terminally differentiated chondrocytes in culture. Exp Cell Res 233:372–382
Hashimoto S, Ochs RL, Komiya S, Lotz M (1998) Linkage of chondrocyte apoptosis and cartilage degradation in human osteoarthritis. Arthritis Rheum 41:1632–1638
Sharif M, Whitehouse A, Sharman P, Perry M, Adams M (2004) Increased apoptosis in human osteoarthritic cartilage corresponds to reduced cell density and expression of caspase-3. Arthritis Rheum 50:507–515
Blanco FJ, Guitian R, Vazquez-Martul E, de Toro FJ, Galdo F (1998) Osteoarthritis chondrocytes die by apoptosis. A possible pathway for osteoarthritis pathology. Arthritis Rheum 41:284–289
Gerber HP, Vu TH, Ryan AM, Kowalski J, Werb Z, Ferrara N (1999) VEGF couples hypertrophic cartilage remodeling, ossification and angiogenesis during endochondral bone formation. Nat Med 5:623–628
Zelzer E, Mamluk R, Ferrara N, Johnson RS, Schipani E, Olsen BR (2004) VEGFA is necessary for chondrocyte survival during bone development. Development 131:2161–2171
Hooiveld M, Roosendaal G, Wenting M, van den Berg M, Bijlsma J, Lafeber F (2003) Short-term exposure of cartilage to blood results in chondrocyte apoptosis. Am J Pathol 162:943–951
Hung SC, Chen NJ, Hsieh SL, Li H, Ma HL, Lo WH (2002) Isolation and characterization of size-sieved stem cells from human bone marrow. Stem Cells 20:249–258
Hung SC, Yang DM, Chang CF et al (2004) Immortalization without neoplastic transformation of human mesenchymal stem cells by transduction with HPV16 E6/E7 genes. Int J Cancer 110:313–319
Chang CH, Lin HY, Fang HW et al (2008) Chondrogenesis from immortalized human mesenchymal stem cells: comparison between collagen gel and pellet culture methods. Artif Organs 32:561–566
Chen WH, Lai MT, Wu AT et al (2009) In vitro stage-specific chondrogenesis of mesenchymal stem cells committed to chondrocytes. Arthritis Rheum 60:450–459
Tran TM, Temkin V, Shi B et al (2009) TNFalpha-induced macrophage death via caspase-dependent and independent pathways. Apoptosis 14:320–332
Chiou SH, Kao CL, Chen YW et al (2008) Identification of CD133-positive radioresistant cells in atypical teratoid/rhabdoid tumor. PLoS ONE 3:e2090
Lotz M, Hashimoto S, Kuhn K (1999) Mechanisms of chondrocyte apoptosis. Osteoarthritis Cartilage 7:389–391
Simonaro CM, Haskins ME, Schuchman EH (2001) Articular chondrocytes from animals with a dermatan sulfate storage disease undergo a high rate of apoptosis and release nitric oxide and inflammatory cytokines: a possible mechanism underlying degenerative joint disease in the mucopolysaccharidoses. Lab Invest 81:1319–1328
Pelletier JP, Jovanovic DV, Lascau-Coman V et al (2000) Selective inhibition of inducible nitric oxide synthase reduces progression of experimental osteoarthritis in vivo: possible link with the reduction in chondrocyte apoptosis and caspase 3 level. Arthritis Rheum 43:1290–1299
Takahashi T, Kitaoka K, Ogawa Y et al (2004) Lysosomal dysfunction on hydrogen peroxide-induced apoptosis of osteoarthritic chondrocytes. Int J Mol Med 14:197–200
Kuhn K, Hashimoto S, Lotz M (1999) Cell density modulates apoptosis in human articular chondrocytes. J Cell Physiol 180:439–447
Schuerwegh AJ, Dombrecht EJ, Stevens WJ, Van Offel JF, Bridts CH, De Clerck LS (2003) Influence of pro-inflammatory (IL-1 alpha, IL-6, TNF-alpha, IFN-gamma) and anti-inflammatory (IL-4) cytokines on chondrocyte function. Osteoarthritis Cartilage 11:681–687
Goldring MB (2000) The role of the chondrocyte in osteoarthritis. Arthritis Rheum 43:1916–1926
Westacott CI, Sharif M (1996) Cytokines in osteoarthritis: mediators or markers of joint destruction? Semin Arthritis Rheum 25:254–272
Kuettner KE (1992) Biochemistry of articular cartilage in health and disease. Clin Biochem 25:155–163
Maes C, Stockmans I, Moermans K et al (2004) Soluble VEGF isoforms are essential for establishing epiphyseal vascularization and regulating chondrocyte development and survival. J Clin Invest 113:188–199
Ashraf S, Walsh DA (2008) Angiogenesis in osteoarthritis. Curr Opin Rheumatol 20:573–580
Roosendaal G, TeKoppele JM, Vianen ME, van den Berg HM, Lafeber FP, Bijlsma JW (1999) Blood-induced joint damage: a canine in vivo study. Arthritis Rheum 42:1033–1039
Lopez-Armada MJ, Carames B, Lires-Dean M et al (2006) Cytokines, tumor necrosis factor-alpha and interleukin-1beta, differentially regulate apoptosis in osteoarthritis cultured human chondrocytes. Osteoarthritis Cartilage 14:660–669
Relic B, Bentires-Alj M, Ribbens C et al (2002) TNF-alpha protects human primary articular chondrocytes from nitric oxide-induced apoptosis via nuclear factor-kappaB. Lab Invest 82:1661–1672
Carames B, Lopez-Armada MJ, Cillero-Pastor B et al (2008) Differential effects of tumor necrosis factor-alpha and interleukin-1beta on cell death in human articular chondrocytes. Osteoarthritis Cartilage 16:715–722
Aizawa T, Kon T, Einhorn TA, Gerstenfeld LC (2001) Induction of apoptosis in chondrocytes by tumor necrosis factor-alpha. J Orthop Res 19:785–796
Yang X, Chen L, Xu X, Li C, Huang C, Deng CX (2001) TGF-beta/Smad3 signals repress chondrocyte hypertrophic differentiation and are required for maintaining articular cartilage. J Cell Biol 153:35–46
Buckland RA, Collinson JM, Graham E, Davidson DR, Hill RE (1998) Antagonistic effects of FGF4 on BMP induction of apoptosis and chondrogenesis in the chick limb bud. Mech Dev 71:143–150
Mello MA, Tuan RS (2006) Effects of TGF-beta1 and triiodothyronine on cartilage maturation: in vitro analysis using long-term high-density micromass cultures of chick embryonic limb mesenchymal cells. J Orthop Res 24:2095–2105
Freathy C, Brown DG, Roberts RA, Cain K (2000) Transforming growth factor-beta(1) induces apoptosis in rat FaO hepatoma cells via cytochrome c release and oligomerization of Apaf-1 to form a approximately 700-kd apoptosome caspase-processing complex. Hepatology 32:750–760
Lomo J, Blomhoff HK, Beiske K, Stokke T, Smeland EB (1995) TGF-beta 1 and cyclic AMP promote apoptosis in resting human B lymphocytes. J Immunol 154:1634–1643
Acknowledgments
Grants supported by Veterans General Hospital-Taipei (R92-001-6, Stem Cell Grant-supported by HealthBanks Biotech); National Science Council (94-2314-B-075-019; 97-2627-B-010-003) and National Yang-Ming University, Ministry of Education.
Conflict of interest
The authors have no conflict of interest to disclose with regard to the subject matter of this present manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ling-Lan Chen and Pei-Yin Kuo are equal contributors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, CY., Chen, LL., Kuo, PY. et al. Apoptosis in chondrogenesis of human mesenchymal stem cells: effect of serum and medium supplements. Apoptosis 15, 439–449 (2010). https://doi.org/10.1007/s10495-009-0431-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10495-009-0431-x