Abstract
Infant colic, excessive crying of unknown cause, is a major burden to families and effects about 10–30 % of infants. Despite decades of research, the exact cause and treatment of infant colic has remained elusive. The use of Lactobacillus reuteri (DSM 17938) in infant colic is somewhat controversial and hence, we designed this study to evaluate its efficacy in infantile colic. We recruited predominantly or exclusively breastfed infants, aged less than 4 months in a placebo controlled observational randomized study. Participants’ were assigned to receive L. reuteri at a dose 108 colony forming units (n = 21) and placebo (n = 21). Placebo was an identical formulation without live micro-organisms. Treatment was given to subjects for 21 days and they were followed for 4 weeks. Treatment success (primary outcome), daily reduction in crying time, parent satisfaction and reduction in maternal depression (secondary outcomes) were assessed at the end of study period. Treatment success was observed in all infants (100 %) of the probiotic group while it was seen in 15.7 % of the placebo group. Mean daily crying time was more significantly reduced to 32.1 ± 8.3 min/day (P < 0.01) from 200.9 ± 6.3 min/day in the probiotic group as compared to the placebo group (120.6 ± 20.0 min/day). Moreover, throughout the study period, parent’s satisfaction and improvement in maternal depression (Edinburgh postnatal depression scale) was also significantly higher in the probiotic group. In our study population, reduction in crying time was significant (P < 0.01) even during first week of initiation of therapy. We conclude that L. reuteri (DSM 17938) reduces daily crying time and maternal depression during infantile colic. We suggest L. reuteri may be a safe and efficacious option for reducing infant colic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infantile colic is defined by Wessel’s diagnostic criteria as sudden, brief and repetitive paroxysmal, excessive, inconsolable crying for >3 h a day, at least 3 days a week and for ≥1 week in an otherwise healthy baby (Urbańska and Szajewska 2014; Savino et al. 2010; Wessel et al. 1954). The true incidence of infantile colic is difficult to estimate as it depends on a number of factors such as feeds, study design, method of data collection and also the definition of colic, although the incidence varies between 5 and 25 % (Roberts et al. 2004). Colicky infants have episodes of crying peaking at about 6 weeks of age, most often noted in the evening. Maternal depression is one of the noticeable effects of infantile colic, both of which in combination affect the well being of the family (Urbańska and Szajewska 2014; Pinyerd 1992.; Vik et al. 2009; Abacı et al. 2013).
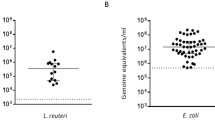
The diagnosis requires a certain degree of clinical suspicion, as an infant cry is usually multifactorial ranging from simple attention seeking and hunger to a potentially serious underlying issue (Freedman et al. 2009). The exact aetiology of infantile colic remains elusive; however, multiple factors including an aberrant intestinal flora affecting motor function, increased presence of hydrogen gas in the gut due to Gram-negative organisms, altered counts of intestinal Lactobacillus or abundant Escherichia coli have been proposed. About five percent of cases may have an underlying organic cause necessitating further investigation (Freedman et al. 2009; Roberts et al. 2004). The treatment options available for infantile colic include simethicone (anti-flatulence), dicyclomine and cimetropium. Dicyclomine and cimetropium are not the first choice due to their apnoeic episode and sedative effects respectively.
Probiotics refer to orally administered living organisms with potential health benefits to the host. Lactobacillus and Bifidobacterium species are the organisms most commonly used as probiotics among infants. The easy availability, low cost and the safety profile have led to increasing use of probiotics in the field of pediatrics and neonatology. They have been documented to have potential benefits for several ailments such as management of diarrhoea and acute gastroenteritis. There is also limited evidence of the role which probiotics may play in managing functional abdominal pain and gastroesophageal reflux (Urbańska and Szajewska 2014).
Despite a few studies showing benefits of using Lactobacillus reuteri DSM 17938 for reduction in crying time during infant colic there is still a lack of consensus regarding its use in the management of infantile colic (Sung et al. 2012; Savino et al. 2007, 2010; Szajewska et al. 2013). More placebo controlled randomized studies are needed to establish its efficacy for the treatment of infant colic. The present trial was designed and conducted with the aim of exploring the role which L. reuteri could play in the management of infant colic.
Methodology
Approval was obtained from institutional review board of the Children’s Hospital of Zhengzhou China (Reference no. PED/11/235RS) following which this randomized single blind placebo controlled study was conducted over a period of 14 months (February 2013–April 2014). Infants less than 4 months of age, weighing between 2.5 and 4.00 kg and exclusively or predominantly breastfed were included in the study. Infants with acute or chronic gastrointestinal illness, fed on cow`s milk or those who underwent a course of probiotic or antibiotic treatment 1 week prior to enrolment were excluded from the trial. Parents who were interested in participating were consented and requested to record symptoms of colic on structured diaries (provided by the researchers) for 1 week. Computer based randomization was used to allocate the participants to groups. An oil based suspension containing L. reuteri DSM 17938 or placebo was given to the treatment and placebo group, respectively, for 28 days. Parents were blinded to the treatment, with regular follow ups arrange at the end of first, second, third and fourth week after initiating treatment. No other drugs were administered during the study period, unless indicated. End of treatment was the 28th day from the first dose.
Definitions
In the current study, terms were defined as follow:
-
Infant colic: Episode of crying that lasted ≥3 h a day, for 3 days before initiation of treatment.
-
End of treatment: On 28th day of treatment.
-
Adverse effects: Any unusual presentation in infants e.g. vomiting, constipation or rashes.
-
Treatment success: Percentage of infants achieving reduction in the daily average crying time i.e. ≥50 % during study period.
-
Patient satisfaction: Patient who answered “yes” in the patient satisfaction questionnaire.
-
Predominantly breast-fed: The main source of nourishment in these infants is mother’s milk; however, they may receive water or water based drink but no dairy products.
Detailed instructions regarding the use, storage (2–8 °C) of the formulation and recording of the symptoms in the diaries were given. The study protocol was duly explained with the timing of drug administration, which was recorded. Parents were asked to maintain a structured infant colic diary by recording dosing time, daily crying time and any adverse events (vomiting, constipation etc.). This was an objective validated baby day diary which has been used in previous study and is easy to use (Radesky et al. 2013). The diary was modified as we decided to measure only the crying time. The parents were asked to enter the details at a suitable time, rather than at the end of day as this could have led to a potential bias as it was based on what they could recall. Use of Cow’s milk and formula feed was advised against in both mother and infants. For parental satisfaction, a questionnaire was also included in the diary, inquiring about their opinion regarding the efficacy of the treatment with options of yes, no and don’t know provided. Maternal depression was assessed using the Edinburgh postnatal depression scale (EPDS).
Parents were requested to bring diaries and remaining drugs during their last follow-up visit. All diaries were assessed and statistically analysed by a different set of physicians who were blinded to the groups. The primary outcome of the study was treatment success, which was assessed as percentage of children achieving a reduction in daily average crying time of ≥50 % at the end of 4th week (28th day) of the study period. Secondary outcomes were mean reduction of daily average crying time, parental satisfaction and reduction in maternal depression.
Statistical analysis
The data has been presented as mean ± standard deviation for continuous variables. Comparison between the groups were performed using unpaired students t test for continuous variables and Fischer’s exact test or Chi square test for categorical variables. Student t test was used to compare the birth weights of study groups and mean values of continuous variables approximating a normal distribution. Mann–Whitney test was used for non-normally distributed variables. All the values were presented as mean ± SD (standard deviation)/median. Interquartile range was expressed for continuous variables when appropriate and number or percentages were used for categorical variables. Sample size calculation was based on the primary outcome of reduction in crying time by at least 50 % through power analysis while assuming α = 0.05 and a power of 0.80. This indicated a sample size of 30 for each group but we were unfortunately unable to reach this target, thereby reducing the power of our study. All the reported results having P value less than 0.05 were considered statistically significant. SPSS 20 (SPSS Inc, Chicago, IL) was used for analysis of data. We started with a null hypothesis of no statistical significance between the treatment and placebo group with an alternative hypothesis that the treatment group may have a reduction in the mean crying time as compared to placebo.
Results
Out of 73 infants identified, a total of 42 infants meeting the inclusion criteria were included in the study with 21 infants in each group (Fig. 1). We had to exclude 31 subjects from our study as: the parents of 14 infants did wish to complete the daily diary; three infants had an episode of diarrhoea; six children had already received a course of probiotic therapy in the preceding week; and eight children as they were also on alternative (conventional Chinese) medicine for the same problem. Subsequently, two patients from the placebo group and one patient from the treatment group were excluded due to noncompliance with completing of daily progress in the diary, lost to follow up and discontinuation of study without any reason, respectively. Thus thirty nine patients (20 from treatment group and 19 from placebo group) completed study. There was no reported adverse events in either group during the study duration.
Demographic profiles (Table 1) including weight, age, height, family history of allergy, family history of gastrointestinal disease, family history of atopy, exposure of smoking, mean crying time and EPDS score were comparable across the two groups with no statistical differences.
At the start of the study, all infants had crying time >180 min/day as defined by inclusion criteria. Treatment success (primary outcome) was found in all infants in the treatment group while it was only observed in 3 infants of the placebo group as shown in Table 2. Data were assessed for statistical analysis at the end of every week by incorporating the recording throughout that week.
A statistically significant reduction in the mean daily crying time (secondary outcome) was observed (32.05 ± 8.30 min/day; P < 0.01) in the treatment group as compared to the placebo group (120.63 ± 20.01 min/day) with a P value of <0.01. The difference in the mean crying time between both the groups was statistically significant throughout the treatment period (Table 3).
Similar statistical difference was also noted while comparing parental satisfaction and maternal depression which was measured as EPDS score (Table 4).
Discussion
The aim of this study was to evaluate effectiveness of L. reuteri for the treatment of colicky infants and we conclude that L. reuteri (108 CFUs) appears superior when compared to placebo in managing colicky infants as reduction in daily crying time and improvement of maternal depression was noted. L. reuteri reduced mean daily crying time by 19, 44, 59 and 84 % at first, second, third and fourth week of treatment respectively. Statistically significant results were observed after the first dose of L. reuteri. Treatment satisfaction was observed with all participants in the probiotic group. Reduction in maternal depression was also notable in treatment group (51.3 %) as compared to placebo group (27.6 %). Overall L. reuteri appears superior for treatment of infantile colic as compared to placebo. Few randomized trials have been conducted in the past with the aim of evaluating the efficacy of L. reuteri in managing infantile colic (Sung et al. 2012; Savino et al. 2007, 2010; Szajewska et al. 2013). One such trial had randomized 50 exclusively breast fed infants who were suffering from infantile colic according to the modified Wessel’s criteria for 21 days, and they reported a significant reduction in the daily crying time Savino et al. (2010). Similar results were also obtained another similar trial which involved 80 exclusively or predominantly breast fed infants (>50 %) of less than 5 months (Szajewska et al. 2013). Szajewska et al. (2013) also observed a daily average reduction in crying time by more than 50 %. However, these studies have been challenged by a more recent trial where 167 breast or formula fed infants of less than 3 months presenting with infantile colic were randomized to receive L. reuteri and then compared with placebo Sung et al. (2014). Interestingly, Sung et al. (2014) observed that at 1 month mean crying time was reduced in both the groups. They also noted that the mean crying time was higher in the treated group as compared to the placebo group with no improvement noted in infants sleep, maternal mental health and the quality of life for both family and infants. This was an interesting finding which was contrary to the previous studies and to our own findings. These three trials had followed up the patients on day 21, whereas we followed the patients from day 7 to day 28.
Despite these earlier studies a clear consensus does not exist for the use of L. reuteri in this population. One of the larger trials involving 167 patients has recommended caution in formulating any guidelines on the use of L. reuteri to help reduce the crying or fussing time in breast fed infants. Sung et al. (2014) also recommended that further trials are needed before any consensus can be reached. Our study is a step in this direction. What is now needed is large scale randomized trial to improve our level of evidence to help build a guideline for use of probiotic L. reuteri. Not all studies have demonstrated its efficacy in managing infant colic Sung et al. (2014) and a possible explanation of this placebo effect could be explained by the reassurance feeling which the parents receive upon the start of the study and receipt of test medication. However, important caveats regarding our study are the small sample size and exclusion of neonates who were formula fed or on cow’s milk due to which this result could not be generalized to all the infants, particularly those who are formula fed.
The mechanism of action of probiotics is still debated. Various mechanisms have been proposed at various stages Iqbal et al. (2014); Roberts et al. 2004; Urbańska and Szajewska 2014) including improvement of gut motility, visceral pain and gut function (Indrio et al. 2008; Wang et al. 2010). L. reuteri is a predominant autochthonous (indigenous) Lactobacillus in infants, children and adults. L. reuteri also secretes antimicrobial substances like reuterin, reutericin, reutericyclin, lactic acid and acetic acid that inhibit the growth of harmful bacteria in humans. Besides this, L. reuteri also modulates the host immune system (Walter et al. 2011). These various mechanisms may underpin its use for several medical complications including acute diarrhoea, antibiotic associated diarrhea, gastric regurgitation, reduction of side effects of anti-pyloric therapy, reduction of abdominal pain intensity and infant colic (Urbańska and Szajewska 2014). The strengths of our study were the method of allocation and concealment, blinding, critical data analysis, similar demographic profile of both groups (Table 1) and daily follow-up of parents by telephone calls to remind them regarding use of diaries. However, the limitations of our study included our reliance on the parents assessment and relying on information from diaries. Other major limitations of our study were: inability to reach our target sample size, which reduced the power of our study; our data analysis and the assessment was not based on an intention to treat as we designed our study purely as an observational trial. Inability to reach a desired sample size in our study clearly limits the significance of our findings. Consequently implementing them into clinical practice and guidelines should be only done following a larger randomised clinical trial. Our study was also limited by being only a single blind study with non-exclusion of crying due to other potential causes.
Overall, we conclude that L. reuteri is likely to help in reducing the crying time in infants with infantile colic; however, this effect may be more pronounced in exclusively breast fed infants rather than formula fed babies. Further randomized trials are needed to help develop a guideline based recommendation for the use of L. reuteri in the management of infantile colic. L. reuteri formulation as a dose of 108 CFU appears to be superior in reducing daily crying time as compared to placebo. The probiotics safety profile also supports its use for colicky infants. Although infant colic has a natural course in an infant’s life with remission of symptoms with over time, its early diagnosis and prompt treatment can improve maternal mental health and family functioning. Additional blinded studies with larger numbers of patients and addressing the above mentioned limitations are needed before final recommendations for the use of probiotics in treatment of infant colic can be made.
References
Abacı FB et al (2013) Psychosocial status and quality of life in mothers of infants with colic. Turk J Pediatr 55(4):391–395. http://www.ncbi.nlm.nih.gov/pubmed/24292032. Accessed 6 Aug 2014
Freedman SB, Al-Harthy N, Thull-Freedman J (2009) The crying infant: diagnostic testing and frequency of serious underlying disease. Pediatrics 123(3):841–848. http://www.ncbi.nlm.nih.gov/pubmed/19255012. Accessed 20 July 2014
Indrio F et al (2008) The effects of probiotics on feeding tolerance, bowel habits, and gastrointestinal motility in preterm newborns. J Pediatr 152(6):801–806. http://www.ncbi.nlm.nih.gov/pubmed/18492520. Accessed 6 Aug 2014
Iqbal MZ et al (2014) Review: probiotics and their beneficial effects against various diseases. Pak J Pharm Sci 27(2):405–415. http://www.ncbi.nlm.nih.gov/pubmed/24577933. Accessed 6 Aug 2014
Pinyerd BJ (1992) Infant colic and maternal mental health: nursing research and practice concerns. Issues Compr Pediatr Nurs 15(3):155–167. http://www.ncbi.nlm.nih.gov/pubmed/1308232. Accessed 6 Aug 2014
Radesky JS et al (2013) Inconsolable infant crying and maternal postpartum depressive symptoms. Pediatrics 131(6):e1857–e1864. http://www.ncbi.nlm.nih.gov/pubmed/23650295. Accessed 20 Dec 2014
Roberts DM, Ostapchuk M, O’Brien JG (2004) Infantile colic. Am Fam Physician 70(4):735–740. http://www.ncbi.nlm.nih.gov/pubmed/15338787. Accessed 6 Aug 2014
Savino F et al (2007). Lactobacillus reuteri (American Type Culture Collection Strain 55730) versus simethicone in the treatment of infantile colic: a prospective randomized study. Pediatrics 119(1):e124–e130. http://www.ncbi.nlm.nih.gov/pubmed/17200238. Accessed 17 July 2014
Savino F et al (2010) Lactobacillus reuteri DSM 17938 in infantile colic: a randomized, double-blind, placebo-controlled trial. Pediatrics 126(3):e526–e533. http://www.ncbi.nlm.nih.gov/pubmed/20713478. Accessed 19 July 2014
Sung V et al (2012) Probiotics to improve outcomes of colic in the community: protocol for the baby biotics randomised controlled trial. BMC pediatr 12:135. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3508922&tool=pmcentrez&rendertype=abstract. Accessed 17 July 2014
Sung V et al (2014) Treating infant colic with the probiotic Lactobacillus reuteri: double blind, placebo controlled randomised trial. BMJ (Clin Res Ed) 348:2107. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3972414&tool=pmcentrez&rendertype=abstract. Accessed 17 July 2014
Szajewska H, Gyrczuk E, Horvath A (2013) Lactobacillus reuteri DSM 17938 for the management of infantile colic in breastfed infants: a randomized, double-blind, placebo-controlled trial. J Pediatr 162(2):257–262. http://www.ncbi.nlm.nih.gov/pubmed/22981952. Accessed 17 July 2014
Urbańska M, Szajewska H (2014) The efficacy of Lactobacillus reuteri DSM 17938 in infants and children: a review of the current evidence. Eur J Pediatr. http://www.ncbi.nlm.nih.gov/pubmed/24819885. Accessed 6 Aug 2014
Vik T et al (2009) Infantile colic, prolonged crying and maternal postnatal depression. Acta Paediatr (Oslo Nor 1992) 98(8):1344–1348. http://www.ncbi.nlm.nih.gov/pubmed/19432839. Accessed 6 Aug 2014
Walter J, Britton RA, Roos S (2011) Host-microbial symbiosis in the vertebrate gastrointestinal tract and the Lactobacillus reuteri paradigm. Proc Natl Acad Sci USA 108(Suppl):4645–4652. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3063604&tool=pmcentrez&rendertype=abstract. Accessed 6 Aug 2014
Wang B et al (2010) Lactobacillus reuteri ingestion and IK(Ca) channel blockade have similar effects on rat colon motility and myenteric neurones. Neurogastroenterol Motil Off J Eur Gastrointest Motil Soc 22(1):98–107, e33. http://www.ncbi.nlm.nih.gov/pubmed/19788711. Accessed 6 Aug 2014
Wessel MA et al (1954) Paroxysmal fussing in infancy, sometimes called colic. Pediatrics 14(5):421–435. http://www.ncbi.nlm.nih.gov/pubmed/13214956. Accessed 6 Aug 2014
Author information
Authors and Affiliations
Corresponding author
Additional information
Guo-Lin Mi and Lei Zhao contributed equally to this research.
Rights and permissions
About this article
Cite this article
Mi, GL., Zhao, L., Qiao, DD. et al. Effectiveness of Lactobacillus reuteri in infantile colic and colicky induced maternal depression: a prospective single blind randomized trial. Antonie van Leeuwenhoek 107, 1547–1553 (2015). https://doi.org/10.1007/s10482-015-0448-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10482-015-0448-9