Abstract
Most youth cessation treatment research consists of efficacy studies in which treatments are evaluated under optimal conditions of delivery. Less is known about the effectiveness of youth cessation treatments delivered in real-world, community based settings. A national sample of 41 community-based youth cessation programs participated in a longitudinal evaluation to identify site, program, and participant characteristics associated with successful cessation. Validated quit rates were comparable to those in randomized controlled trials; 7-day abstinence at the end of program averaged 14% and 30-day abstinence at 12 months averaged 12%. Multivariate GEE models explored predictors of smoking cessation at the end of the programs and at 12 months. Results showed correlates of both short- and long-term cessation. Findings point to the importance of both individual and community-level variables, including motivation, opportunities for and encouragement to engage in activities outside of academics, having youth participate in treatment before they become highly dependent smokers, and community norms and ordinances that discourage youth purchase, use and possession of tobacco. Providing evidence-based treatment to youth in community-based settings results in successful cessation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Among the more than 47 million smokers in the United States, more than 3 million are youth aged 18 and younger (Centers for Disease Control and Prevention 2010). Nearly one-fifth of high school seniors in the United States were current smokers in 2010, with more than half of them reporting daily smoking (Johnston et al. 2011). With the majority of children smoking their first cigarette by age 13, many older teens have well-established addictions to tobacco (Johnston et al. 2008). Continued efforts to promote and support smoking cessation among these new generations of smokers are critical.
Surveys of youth tobacco users indicate that the majority of youth smokers want to quit smoking and make serious attempts to do so (Marshall et al. 2006). Among respondents to the 2009 Youth Risk Behavior Survey, 51% of youth who smoked cigarettes in the 12 months prior to the survey reported trying to quit smoking (Centers for Disease Control and Prevention 2011). Among respondents to the 2007 Youth Risk Behavior Survey, 61% of youth who smoked daily reported making a serious quit attempt in the prior year and 12% of those who attempted cessation were abstinent for at least the 30 days prior to the survey (Centers for Disease Control and Prevention 2009). This translates to an approximate 7% quit rate overall. Most youth attempted to quit without using treatment. Among respondents to the 2009 National Youth Tobacco Survey (NYTS) (National Youth Tobacco Survey Dataset 2009) who reported making one or more serious quit attempts, only 7.5% said that they participated in a behavioral program; 14.6% used pharmacotherapy; 2.4% called a quit line; and 3.1% visited an internet quit site. Youth most often reported using nicotine gum (8.4%), nicotine patch (4.4%), or a program in school (4.3%) to help them stop smoking.
The evidence base for youth cessation program efficacy is modest. There are fewer than 50 experimental studies of youth cessation programs and even fewer randomized controlled trials, compared to more than 8,700 studies of adult smoking cessation treatments (Fiore et al. 2008). The available evidence indicates that youth tobacco cessation treatment significantly increases the likelihood of cessation compared to no-treatment (Grimshaw and Stanton 2006; Sussman et al. 2006). Treatment components that focus on increasing motivation for cessation and on cognitive-behavioral strategies such as problem solving and coping skills improve outcomes with youth smokers (Curry et al. 2009).
The vast majority of youth cessation treatment research comprises efficacy studies in which youth cessation interventions were evaluated under optimal conditions of delivery. Less is known about the effectiveness of youth cessation treatments delivered in real-world settings. This paper reports the outcomes from a national evaluation of community-based youth cessation programs, conducted as part of a Robert Wood Johnson Foundation initiative, helping young smokers quit (HYSQ). Previous work under the auspices of HYSQ included a national survey to assess the prevalence and characteristics of community-based youth cessation programs (Curry et al. 2007; Emery et al. 2010; Houser-Marko et al. 2010; Sterling et al. 2009). In this paper we describe participant, program, and community site characteristics as well as smoking cessation outcomes at the end of treatment and at the 12-month follow-up. Multivariate analyses are used to identify individual, program, and site-level characteristics that are associated with outcomes.
Methods
Design
A detailed description of the overall design and implementation of this study has been published previously (Curry et al. 2010). The evaluation comprised a longitudinal observational study of community-based smoking cessation programs. The study did not aim to estimate general treatment outcomes across a representative sample of programs, but focused on identifying aspects of community-based youth cessation programs that are associated with successful cessation. Our design was guided by a heuristic framework delineating a multi-level approach that encompassed the site context of the program, program characteristics, and participant characteristics.
Program Recruitment
Based on available funds for the evaluation and staffing logistics, we targeted recruitment of 40 programs, each serving a minimum of 15 youth per year. National recruitment focused on both programs that had been identified in our previous national survey of youth cessation programs (in-reach strategy; Curry et al. 2007) and dissemination of information via national organizations and interest groups, departments of education, and the Centers for Disease Control and Prevention contacts with tobacco control officers from all 50 states and the District of Columbia (out-reach strategy). Programs interested in potentially being involved in the evaluation completed a web-based application process designed for this project.
Using the information from our national survey of programs (Curry et al. 2007) we developed eligibility criteria designed to ensure the inclusion of state-of-the-art, replicable, and viable community-based youth cessation programs. To be eligible for consideration, programs were required to meet the following 8 criteria:
-
Provided direct smoking cessation services, primarily through an in-person group setting;
-
Primarily served high school age youth (75% of participants are aged 14–18 years)
-
Have offered the program at least once before and planned to offer it during the study period;
-
Used a written program manual and used trained treatment providers;
-
Included at least four of six cognitive-behavioral components (self-monitoring, disrupting smoking patterns, contingency control, coping skills training, general health and lifestyle balance, social support);
-
Was not currently participating in a research effort (other than for self-evaluation);
-
Served a minimum of 15 eligible participants per year;
-
Had a minimum number of four treatment sessions and minimum session length of 30 min.
In addition, applicant programs needed to provide a letter of support from a senior leader of the sponsoring organization, agree to insert an extra session for baseline data collection prior to beginning the program, and designate a specific person in their organization who would serve as the primary liaison with the Helping Young Smokers Quit field team. Programs and liaisons received modest financial incentives for participation paid in increments over the 12-month evaluation period. Programs could receive a total of $2200.00 ($1000.00 following baseline data collection; $600 at the completion of the 6-month and again following 12-month follow-up completion). Program liaisons received a total of $300.00, paid in $100.00 increments at the same times as the program incentives. Recruitment proceeded from initial review of written applications to telephone interviews, with finalists participating in an on-site visit for enrollment in the evaluation.
Data Collection
Data collection occurred at multiple levels including abstraction of state and local tobacco control ordinances, key informant surveys with community leaders, and organizational leader interviews to assess program site context; program leader surveys to measure program components; and repeated in-person surveys of youth cessation program participants at pretreatment baseline, end of program, 6 and a 12-month follow-ups (Curry et al. 2010). The timeframe for data collection spanned October 2004–October 2006. All of the survey data collection activities received review and approval by the University of Illinois at Chicago and Westat Institutional Review Boards. Both IRB’s granted a waiver of active, written parental consent for the participant surveys. Youth under age 18 provided active assent to the survey and youth age 18 and over provided active consent. A complete description of the survey constructs for all data collection can be found in Curry et al. 2010. Copies of all surveys can be obtained as electronic supplementary material from the journal.
Program Characteristics
Program characteristics were determined by interviews with program leaders and leaders of the organization that offered the youth cessation program. Program leaders completed attendance records and responded to a telephone survey after the completion of each group they led. Organizational leaders completed a one-time telephone survey approximately 6 months after the start of the study. A total of 77 of the possible 79 program leaders completed surveys (97.5% response). There were 65 individuals eligible to be interviewed as organizational leaders (some programs involved more than one sponsoring organization (e.g., a school and a voluntary organization) and 64 individuals completed surveys (98% response).
Participant Characteristics
Program participants completed surveys at baseline (prior to the start of the program), end of program, 6 and 12 months post-program. Self-reported abstinence was biochemically confirmed at each follow-up with carbon monoxide testing. A total of 878 youths assented to participate in the evaluation and completed baseline surveys. Respondents to the end of program survey were 801 (91% response rate); 672 participants completed the 6 month survey (77% response rate); 601 participants completed the 12 month survey (68% response rate). Overall 550 youth completed all four surveys (63% response rate). Twenty-one program participants indicated on their baseline survey that they had never smoked a cigarette not even a puff and so were participating as supportive friends of smokers; these 21 were not included in analyses.
Site Characteristics
Site characteristics were obtained from interviews with sponsoring organization leaders, community leaders, and tobacco control ordinances. Organizational leaders combined with other sources identified a total of 120 community leaders to interview. This included 33 education leaders, 31 health leaders, and 56 individuals in juvenile justice. Of the 120 eligible leaders, 94 completed surveys (78% response rate). In addition to these interviews, we collected information about 19 types of smoking-related ordinances at the state (n = 18) and local (n = 55 cities and counties) levels. A total of 91 state ordinances, 31 city and 33 county-level ordinances were identified.
Analytic Models
Data analysis focused on how site, program, and participant level variables were related to three primary outcomes of interest: 7-day abstinence at the end of program; serious quit attempts at the end of the program (among non-abstainers); and 30-day abstinence at the 12-month follow-up. Our analyses comprised a multi-step process as follows:
Descriptive and Bivariate Analyses
These analyses were conducted within the three levels of variables (site, program, and participant) in order to describe the characteristics of programs and participants and to provide an initial bivariate assessment of associations among site, program, and participant variables and the three primary outcomes.
Assessment of Missing-Data Patterns and Use of Multiple Imputation
Although we obtained high response rates for all surveys and the item-response rate of missing on each survey was low (average across all variables = 2%; range 0–10%), missing data with longitudinal, multi-level data analysis can be problematic. To address this issue, we conducted multivariate regression analyses to model missing items as a function of our outcomes of interest to assess whether data are missing at random. Confirming that data were missing at random, we used multiple imputation to create analytic datasets with complete cases.
Evaluation of Variables of Interest
Our surveys included multiple variables related to the key constructs that were evaluated as candidates for the multivariate analyses by regressing each outcome of interest on potential multivariate predictors. Variables with the strongest explanatory power were retained in the analyses. Selection of the final variables for the multivariate models occurred separately for each level of data using backward variable selection for each outcome. The initial number of within-level variables considered was 53 youth-level, 23 program-level, and 41 site-level. The youth level variables were reduced to 20, and the number of program- and site-level variables remained the same.
Construction of Final, Multi-Level Model
Once the final set of variables was determined within each level, these were combined into a comprehensive data set with youth-, program-, and site-level data. The final data included variables averaged from imputed datasets. Using the combined dataset, logistic regression models utilizing backward selection, with an inclusion criterion of p < .15 were used to reduce the number of variables in the final model. After we obtained a computationally manageable and conceptually relevant model for each of the three major outcomes, multivariate GEE models using PROC GENMOD in SAS V9.2 (SAS 2011) was used to model the response variables, adjusting for program-level clustering. To control for demographics and because we were interested a priori in whether program attendance or mandated participation was associated with outcomes, the following variables were forced into each model: participant age, gender, race, proportion of program sessions attended, whether the youth reported their participation was mandated, whether the program included mandatory participation.
Results
Program Recruitment
Web-based applications were accepted during a 2-month period in 2004. From 107 initial applicants we identified 81 as eligible for an initial telephone interview. From the telephone interviews we selected 45 programs for site visits and completed site visits and enrolled 43 programs in the evaluation. Two programs withdrew, leaving a final sample of 41 participating programs.
Program Characteristics
The program characteristics are summarized in Table 1. Most programs were offered in schools and used multiple strategies to recruit participants. Programs enrolled an average of 14 youth per group offering and, on average 11 of 14 (79%) of youth participants completed more than half of the program. Over one-third of the programs reported having some participants who were mandated to the program. Programs averaged 9 sessions of approximately 1-h each. Supplemental components were reported with some frequency; the most common was access to telephonic support from a quit line. Over 80% of programs offered some type of incentive for attendance and over half reported offering incentives for cessation. The most commonly reported incentives were clothing, accessories, or trinkets (40%), food (19%) and gift certificates (13%). Only 3% of programs reported offering a cash incentive.
By design, all of the programs included at least 4 cognitive-behavioral components and the vast majority addressed issues related to youth including tobacco marketing and non-tobacco issues such as mental health, other drug and alcohol use, school success and careers. Overall, the group sessions were fairly didactic with 74% of facilitators indicating that they used structured lectures most/all of the time. Using 1–5 point scales, group cohesion was relatively high, with facilitators indicating good levels of group interaction, closeness, and supportiveness among group members.
Facilitators were predominantly women with an average age of 40 years. The vast majority were white. Two-thirds of the facilitators had ever smoked, only 4% were current smokers. Facilitators reported an average of 60 h of smoking cessation training and had nearly 5 years of experience.
Youth Participant Characteristics
Baseline characteristics of the 857 youth participants who were ever smokers are summarized in Table 2. Participants averaged 16.8 years of age and were evenly divided by gender. Over one quarter of participants was non-white race and 13% indicated Hispanic ethnicity. Nearly half of the participants indicated that they were employed for pay, and common outside activities included involvement in sports and attending church at least monthly. Nearly one-third of the participants were overweight as indicated by a body mass index (BMI) greater than or equal to 25, and a high proportion indicated they were trying to lose weight. Over half of the participants indicated that they exercised more than once per month. Binge drinking was reported by nearly two-thirds of the participants. A sizeable minority of participants reported depressive symptomatology and moderately high levels of perceived stress. A third of participants reported having a diagnosis of attention deficit disorder (ADD) or attention deficit hyperactivity disorder (ADHD). Problems with alcohol and school problems were frequently reported.
On average, participants smoked their first whole cigarette at age 11.8. Prior to the start of the program 85% reported ever smoking daily and 91% had smoked during the past 7 days, averaging 6.8 cigarettes per day. As an indicator of addiction to nicotine, over a third of participants reported smoking within 15 min of waking. A similar proportion reported that they smoked with their parents. Use of other tobacco products was common. With regard to quitting history, over 80% indicated that they had ever quit smoking for at least 1 day and 75% had quit smoking for one or more days during the past 12 months. Just over half of the participants indicated that they had been asked about their smoking status by a health professional in the past 12 months; only a third reported being advised to quit by a health professional in the past 12 months. Prior use of behavioral treatment was reported by half of the participants and just under a quarter of participants reported using pharmacotherapy.
Smoking among family and friends was commonly reported. Three-quarters of participants indicated they lived with at least one a smoker, although 50% reported that smoking was prohibited inside their homes. Nearly all participants had at least one close friend who smoked. Participants reported moderate levels of strong support for quitting from their mother, father, or friends.
Level of motivation to quit was modest. One quarter of the sample indicated they were not even seriously thinking about quitting, which mirrors the proportion who indicated that they were mandated for treatment. Only 20% of participants indicated that they would definitely not be smoking in 5 years. On a 10-point scale, participants averaged 6.1 level of motivation and 6.4 level of confidence in quitting. Their average intrinsic motivation was greater than extrinsic motivation for quitting. Just over half of the participants believed that they would definitely stick with the program until the end, but only a quarter thought that the program would definitely help them quit.
Site Characteristics
Site-level information is summarized in Tables 3 and 4. The vast majority of sponsoring organizations had written policies that prohibit smoking on their premises and many had additional written policies that prohibit the possession of tobacco products and wearing clothes or carrying accessories with tobacco logos on the premises. Over 80% of organizational leaders believed that their organizational policies were just right with the remainder feeling they were too lenient. Most of the programs began with staff initiative. The average annual dollars spent on the program was about $3700.00 and most organizational leaders reported that their resources to implement the program were adequate. The majority of organizations reported involvement in other youth health issues, including alcohol and drug use prevention or treatment, nutrition or weight management, violence prevention, and mental health.
Most organizational leaders reported that community leaders were very or somewhat aware of their program and that leaders who were aware of the program were supportive. On a 10-point scale, organizational leaders rated the perceived priority of youth tobacco use in their community higher than community leaders (means = 6.5 and 5.6, respectively). Overall, community leaders most frequently rated drug or alcohol use as the biggest concern facing youth in their communities. Tobacco use was selected by only 3% of respondents.
A minority of communities had tobacco control ordinances limiting smoking in publicly owned buildings, public gathering places, or prohibiting adult use on school property. Although a majority of communities required tobacco retailer licensing, only 1% explicitly prohibited tobacco vending machines. Some youth restrictions were common, including ordinances limiting or prohibiting purchase or possession of tobacco among youth, and penalties for the sale of tobacco to minors. Fewer ordinances existed for youth tobacco use overall or in specified places such as school property or school buses.
Among communities with ordinances, enforcement was reported at 80% or higher for no smoking in public buildings, limiting or prohibiting tobacco vending machines, and enforcement of no student and no adult use of tobacco on school grounds, and no use of tobacco on school buses. Less frequent enforcement was reported for youth possession, tobacco use, and purchase.
Smoking Cessation Outcomes
Table 5 reports smoking cessation outcomes using intent to treat analyses. Abstinence rates are biochemically confirmed. Cessation outcomes were similar when calculated across all youth respondents and as the average percent abstinent by treatment program. Fourteen percent of youth reported 7-day abstinence at the end of treatment; the average percent abstinent by program was 13%, but ranged from 0 to 50% across the 76 program implementations. Six and twelve-month abstinence rates were similar; at 12 months 12.5% of youth reported being abstinent for at least 30 days. Among youth who were not abstinent at the end of their program, 74% reported making at least one serious quit attempt; 3 or more serious quit attempts was reported by 19% of participants.
Outcome Modeling
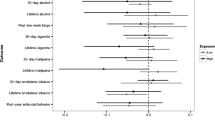
Tables 6, 7, and 8 summarize the significant predictors from the final GEE models for each of the three primary outcomes, including beta coefficients, odds ratios, confidence intervals, and p values.
End of Program Abstinence
As indicated in Table 6 7-day abstinence at the end of program was significantly associated with participant and site-level variables. In addition to variables that were forced into the model, the final model included 11 participant-level variables and six site-level variables. One participant-level variable (father’s support) did not reach significance in the final model. The following variables were associated with a significantly lower likelihood of quitting: white, non-Hispanic race, involvement only in sports as an outside activity, alcohol use and alcohol-related trouble, smoking more than 5 cigarettes per day, living with a smoker, previously trying pharmacotherapy, having a community or state-level ordinance that prohibits smoking on school buses that is enforced all the time, stricter clean indoor-air restrictions. A significantly higher likelihood of quitting was associated with the following variables: higher rate of program attendance, high baseline confidence in quitting, the presence of smoking restrictions in the home, higher than precontemplation stage of readiness to quit, support for smoke-free public places, prohibition of smoking on the premises where the cessation program is offered, prohibitions on youth tobacco possession and tobacco use on school property.
Serious Quit Attempts at the End of Program
Results presented in Table 7 are restricted to the 738 youth who reported smoking at the end of the program. Among these participants, making one or more serious quit attempts during the program was associated with participant-, program-, and site-level variables. In addition to the variables that were forced into the model, the final model included seven participant-level, five program-level, and four site-level variables. Two participant-level variables (time to first cigarette and ever expelled from school) and one site-level variable (compliance checks for sales to minors) did not reach significance in the final model. Continuing smokers were less likely to report one or more serious quit attempts if they were older, reported higher baseline confidence, reported prior use of pharmacotherapy, participated in a program with sessions that lasted longer than 50 min, had a facilitator with less than 5 years of experience, and were in a community with ordinances that banned tobacco advertising. A higher likelihood of reporting one or more serious quit attempts among continuing smokers was associated with involvement in a mixture of sports and non-sports activities, higher baseline motivation to quit, prior cessation of at least 1 day, a program leader with a close and supportive style, and community ordinances that prohibit youth tobacco possession and that prohibit tobacco use on school buses.
30-Day Abstinence at 12 Months
At the 12-month follow-up the model included 13 participant-level variables, six program-level variables and three site-level variables, in addition to those variables that were forced into the model. Four participant-level variables (abstinent at least 30 days at baseline, asked by doctor if smoked, involvement in extra-curricular activities, and household smoking bans) and one program-level variable (coverage of future plans) did not reach significance in the final model. Youth were less likely to report a minimum of 30-day abstinence at the 12 month follow-up if they had the following characteristics: had ever smoked daily; heard about the program from a friend only or just from a flyer, poster, or school assembly; reported their mother as somewhat versus very supportive of their quitting; would use a promotional item from a tobacco company; were in a program with a higher number of sessions than average, were in a program with incentives for quitting, were in a program with a leader that was older than average, lived in a community with an ordinance that prohibited youth tobacco use that was not enforced all the time, living in a community with a stricter clean indoor air law. Variables associated with a higher likelihood of 30 day abstinence at the 12 month follow-up were: greater attendance at the program sessions; longer time to first cigarette after waking; father very supportive of quitting; starting the program with the strong intention to stick with it; participation in a program that only has volunteer participation; and organizational leadership that is aware and supportive of the program.
Discussion
A prior national survey found a high prevalence of community-based youth cessation programs that included evidence-based components, were delivered by trained professionals, and were committed to program evaluation (Curry et al. 2007). The national survey did not obtain information about specific program implementation and outcomes from either participants or program leaders. The current study extended this work and implemented a rigorous, longitudinal evaluation that included multi-level data collection. The evaluation benefited from high levels of cooperation from program participants, program leaders, and organizational and community leaders which enabled a rich description of youth cessation programs as implemented in real-world settings.
By design, the programs that participated in this evaluation were homogenous with regard to format (group), setting (primarily school-based), and content (all programs included cognitive-behavioral components). Customization of program content for youth was evident in the high percentage of programs that addressed tobacco marketing and youth-related non-tobacco issues. Included in a majority of programs was attention not just to tobacco and other drugs, but stress and depression and youths’ future plans. Overall, the programs provided rather intensive treatment that occurred over an average of 9 sessions lasting an hour each with dedicated program leaders. These youth cessation programs operated in supportive organizations and communities. A sizeable majority of organizational leaders indicated that staff initiative was a primary reason for offering the program, and organizational leaders felt that youth tobacco use was a moderately high priority for their organization. Community representatives perceived youth tobacco as somewhat less of a priority. The ordinance review also showed a high prevalence of local or state tobacco control ordinances. While some ordinances had an impressively high rate of enforcement, the lowest rates of enforcement were reported for ordinances related to youth tobacco possession, use, and purchase. This is a major lost opportunity as there is robust evidence that enforcement contributes to reduced levels of youth tobacco use (Stead and Lancaster 2005; Jason et al. 1999).
The cessation programs attracted a diverse group of adolescent smokers. In contrast to adult programs, where the majority of participants are female, half of the youth participants were male. The gender balance reflects a relatively high percentage of programs that reported both mandated and volunteer participants. Previous analyses (Houser-Marko et al. 2011) showed that males were over-represented in mandated participants. Program participants were experienced with tobacco cessation efforts, as evidenced by prior quit attempts and some treatment use. However, there was considerable pessimism about their future as non-smokers, with only 20% believing they would definitely not be smoking in 5 years.
High retention of participants in the evaluation, particularly at the end of program follow-up, along with biochemical validation of self-reported smoking status provided reliable estimates of short-and long-term quit rates in these community-based programs. The observed quit rates of 12–13% across the 12-month follow-up period are impressive and even higher than quit rates that are reported in research studies. For example, in a recent meta-analysis of 48 studies, Sussman and colleagues reported an aggregate quit rate for youth cessation interventions of 9.14% compared to 6.24% for control conditions (Sussman et al. 2006). There was considerable range in quit rates, however, across programs; almost 20% reported no abstainers at the end of the program, and about 30% reported quit rates greater than 20%.
Exploration of youth-, program-, and site-level correlates of outcomes was complex to execute and even more complex to interpret. Creating a multi-level model required an iterative process of variable selection. While our priority was to identify a parsimonious set of conceptually-driven variables to test, we acknowledge an element of data-driven model building to our approach. Our findings do not point to a single set of correlates with short- and long-term outcomes. The only variable associated with both end of program and 12-month abstinence was program attendance. As would be expected, higher attendance was associated with a higher likelihood of abstinence at both time points.
It is notable that no program-level variables were associated with end-of-program abstinence. The multivariate model suggests that lower-risk youth, from supportive home and community environments were most likely to achieve initial abstinence. Program-level variables did emerge as important correlates of long-term outcome. Long-term abstinence is most likely among voluntary versus mandatory participants, in programs with supportive organizational leadership, and with younger providers. The youth-level correlates of 12-month abstinence suggest that less dependent smokers were more likely to succeed and that these youth were more intrinsically motivated to attend and stick with the program.
Tobacco dependence is a chronic relapsing condition that typically requires multiple serious quit attempts. Thus, it is of interest to identify correlates of serious quit attempts among the majority of youth smokers who do not achieve abstinence. Here we find both participant- and program-level factors are key, although the pattern of results has some interesting twists. Younger youth with involvement in outside activities who are highly motivated, have supportive fathers, have previously tried to quit and reject tobacco company promotional items were more likely to make a quit attempt. Programs with sessions under 50 min that were facilitated by individuals with a close and supportive style resulted in more quit attempts among participants, even though they did not achieve abstinence at the end of the program. Two variables have interesting associations: very supportive mothers were a disadvantage as was higher confidence.
Most puzzling in our findings are some of the associations between site-level variables and outcome. Less strict clean indoor air laws were positively associated with 12-month abstinence and bans on tobacco advertising on school property were negatively associated with serious quit attempts and the end of program. Moreover, inconsistent enforcement of bans on school buses and youth tobacco use was also associated with better outcomes at the end of program and 12 months. We are cautious about over-interpreting these findings and would suggest that further research, including replication of these measures in other cohorts is needed.
This study is the largest longitudinal evaluation of community-based youth cessation programs reported to date. We are heartened by the observed quit rates that rival those in randomized controlled efficacy trials. The commitment of community-based organizations and the adults who conduct the cessation programs was evident at every step of this evaluation. The observed correlates of positive outcomes are consistent with those reported in randomized trials and point to the importance of motivation, opportunities for and encouragement to engage in activities outside of academics, having youth participate in treatment before they become daily, highly dependent smokers, and community norms/ordinances that discourage youth purchase, use and possession. Clearly, there is no magic bullet for youth cessation programming. That only a few program-level variables emerged as correlates in our multivariate models likely points to the homogeneity of program characteristics and the high level of commitment to quality programming associated with a willingness to participate in this evaluation. Thus, our take-home message is simple. Providing evidence-based treatment to youth does result in successful cessation and in serious involvement in the quitting process even if youth do not quit. These programs are vital resources for the health of our youth.
References
Centers for Disease Control and Prevention. (2009). High school students who tried to quit smoking cigarettes—United States, 2007. Morbidity and Mortality Weekly Reports, 58, 428–431.
Centers for Disease Control and Prevention. (2010). Youth risk behavior surveillance, United States, 2009. Morbidity and Mortality Weekly Reports, 59(SS-5), 12–13.
Centers for Disease Control and Prevention. (2011). Youth risk behavioral surveillance system. Accessed at http://apps.nccd.cdc.gov/youthonline/app/default.aspx. November 17, 2011.
Curry, S. J., Emery, S. E., Sporer, A. K., Mermelstein, R., Flay, B. R., Berbaum, M., et al. (2007). A national survey of tobacco cessation programs for youths. American Journal of Public Health, 97, 171–177.
Curry, S. J., Mermelstein, R. J., & Sporer, A. K. (2009). Therapy for specific problems: Youth tobacco cessation. Annual Review of Psychology, 60, 229–255.
Curry, S. J., Mermelstein, R. J., Sporer, A. K., Emery, S. L., Berbaum, M. L., Campbell, R. T., et al. (2010). A national evaluation of community-based youth cessation programs: design and implementation. Evaluation Review, 34(6), 487–512.
Emery, S. L., Lee, J., Curry, S. J., Johnson, T., Sporer, A. K., Mermelstein, R., et al. (2010). Finding needles in a haystack: A methodology for identifying and sampling community-based youth smoking cessation programs. Evaluation Review, 34(1), 35–51.
Fiore, M. C., Jaen, C. R., Baker, T. B., Bailey, W. C., Benowitz, N. L., Curry, S. J., et al. (2008). Treating tobacco use and dependence: 2008 update. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service.
Grimshaw, G. M., & Stanton, A. (2006). Tobacco cessation interventions for young people. Cochrane Database of Systematic Reviews, 4, CD003289.
Houser-Marko, L., Sporer, A., Emery, S. L., Hund, L., Lee, J., & Curry, S. J. (2010). Use of program evaluation in community youth tobacco cessation programs. American Journal of Health Behavior, 34(2), 177–185.
Houser-Marko, L., Curry, S. J., Mermelstein, R. J., Emery, S., & Pugach, O. (2011). A comparison of mandated versus volunteer adolescent participants in youth tobacco cessation programs. Addictive Behaviors, 36(9), 937–940.
Jason, L. A., Berk, M., Schnopp-Wyatt, D. L., & Talbot, B. (1999). Effects of enforcement of youth access laws on smoking prevalence. American Journal of Community Psychology, 27(2), 143–160.
Johnston, L. D., O’Malley, P. M., Bachman, J. G., & Schulenberg, J. E. (2008). Monitoring the future national survey results on drug use, 1975–2007: Volume I, Secondary school students (NIH Publication No. 08-6418A). Bethesda, MD: National Institute on Drug Abuse.
Johnston, L. D., O’Malley, P. M., Bachman, J. G., & Schulenberg, J. E. (2011). Monitoring the future national results on adolescent drug use: Overview of key findings, 2010. Ann Arbor, Institute for Social Research, the University of Michigan.
Marshall, M., Schooley, M., Ryan, H., Cox, P., Easton, A., Healton, C., et al. (2006). Youth tobacco surveillance—United States, 2001–2002. Surveillance Summaries, Morbidity and Mortality Weekly Reports, 55, 1–56.
National Youth Tobacco Survey (NYTS). (2009). Dataset. Obtained from http://www.cdc.gov/tobacco/data-statistics/surveys/nyts.
SAS. (2011). SAS/STAT (R) 9.2. User’s guide. Second Edition. The GENMOD Procedure. Available at support.sas.com/documentation.
Stead, L. F., & Lancaster, T. (2005). Interventions for preventing tobacco sales to minors. Cochrane Database of Systematic Reviews, 1, CD01497.
Sterling, K. L., Curry, S. J., Emery, S., Sporer, A. K., Mermelstein, R. J., Berbaum, M., et al. (2009). Internally-developed teen smoking cessation programs: characterizing the unique features of programs developed by community-based organizations. International Journal of Environmental Research in Public Health, 6(3), 1026–1040.
Sussman, S., Ping, S., & Dent, C. (2006). A meta-analysis of teen cigarette smoking cessation. Health Psychology, 25, 549–557.
Acknowledgments
This study was funded by the Robert Wood Johnson Foundation (grant 04-6782). Support was also provided by the National Cancer Institute and the Centers for Disease Control and Prevention through the U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute (contract 233-02-0087). We acknowledge the Youth Tobacco Cessation Collaborative for its visionary work to advance the evidence base for youth tobacco cessation treatment and C. Tracy Orleans of The Robert Wood Johnson Foundation for establishing the Helping Young Smokers Quit initiative.
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the authorship and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authorship on the title page is alphabetized after the 4th author.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Curry, S.J., Mermelstein, R.J., Emery, S.L. et al. A National Evaluation of Community-Based Youth Cessation Programs: End of Program and Twelve-Month Outcomes. Am J Community Psychol 51, 15–29 (2013). https://doi.org/10.1007/s10464-012-9496-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10464-012-9496-8