Abstract
This paper presents an ecological-community model toward the explanation of variation in patterns of substance abuse (SA) service utilization among adolescents who are enrolled in Tennesssee’s Medicaid program (TennCare). Guided by a theoretical framework that draws from the social ecology work of Bronfenbrenner and health services utilization models promoted by Aday and Andersen, we apply a social indicators approach toward explaining the impact of community ecology on identification of SA and treatment engagement. Both county-level rates and individual-level treatment utilization are examined and hierarchical linear modeling is incorporated to examine the individual-in-community phenomenon. This study is an expansion of previous service utilization research and suggests that explanations of youth’s service utilization must necessarily include not only individual, familial, and service system characteristics, but community factors, as well.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Previous studies have documented the importance of community context on both physical and behavioral health status and service delivery. Low income communities and individuals living in neighborhoods with higher proportions of impoverished households experience poorer educational, occupational, physical, behavioral and mental health related outcomes for both adults and children (Jencks and Mayer 1990; Latkin and Curry 2003; LeClere et al. 1998; Wilson 1990). Some have demonstrated the importance of community and neighborhood characteristics on physical and mental health (Leventhal and Brooks-Gunn 2000), on adolescent mental health (Aneshensel and Sucoff 1996; Leventhal and Brooks-Gunn 2003), and among children using child welfare services (Hurlburt et al. 2004). Others have investigated variations in substance use and treatment outcomes among adolescents (Farrington 1991; Jencks and Mayer 1990; Yoshikawa 1994) including youth across different settings (Alison et al. 1999) A few have demonstrated the importance of community context on access to medical care, in general (Cunningham 1999; Cunningham and Kamper 1998) and more specifically the likelihood of pursuing behavioral health treatment (Rosenheck and Lam 1997) including substance abuse (SA) treatment (Mankowski et al. 2004). In addition, although some have investigated the impact of urban settings in accessing behavioral health care (Gresenz et al. 2000; Yuen et al. 1996), none have explained behavioral health service utilization using a community indicators approach with population individual-level data.
Community Indicators
The community indicators movement has sought to provide a system of measures, including economic, social, environmental and health-related indicators of well-being, all of which pertain to the “quality” of community life and development. Sparked by nationwide successes at monitoring economic indicators, the 1960s prompted an intensive interest in community and neighborhood indicators research. Many had hoped that the development of such systems could considerably strengthen local and national efforts toward assessing the health and wellness of communities, serving as an important tool for use in community program evaluation efforts (Bauer 1966). Some have noted, however, that at least initially, the community and neighborhood indicators movement was an “idea that came too early” (Kingsley 1999, p. 11). Financial, technological, and labor intensive constraints of the late sixties and early seventies, coupled with the recognition that even a well assembled collection of indicators could not entirely eliminate the need for customized data collection, all led to a decline in interest in the movement. More recent technological advancements, a more realistic understanding of potential data applications (Sawicki and Flynn 1996), and a pragmatic need on the part of policy makers to have greater access to and understanding of local information in support of evidenced based decision making and policy has marked a resurgence of interest in neighborhood indicators.
In many areas, advances in the compilation of community indicator networks has facilitated collaboration among social scientists and policy makers as they have worked to share data and gain insights at multiple levels of analysis within and across communities, including metropolitan regions, counties, cities, towns and neighborhoods (Sawicki and Craig 1996). This trend toward democratization of data represents an idealized vision that such resources may enhance democracy, citizen participation, resident empowerment and well-being (Chapin and Denhardt 1995). Indeed, in certain instances a community indicators approach has served to enable local residents, service advocates, and their agencies to enact substantively informed and directive tactics within specific neighborhoods and communities, linking proponents of change more closely to their effects, and increasing the likelihood of effective interventions and new developments (Speer et al. 2003). Additionally, for those working on issues that have a geographically bounded component, the availability of community indicators data provides further opportunity for data merging and community- or place-based analysis. This allows researchers to expand data sets to address a myriad of theoretical questions, as well as provide support for more locally-grounded initiatives. The use of community indicators has been specifically recommended for examining SA issues (Gruenewald et al. 1997).
Previous Research on Adolescent Substance Abuse and Treatment
In the past decade, studies have documented an increase in the use of alcohol and other drugs by adolescents (Johnston et al. 2002). In the 2003 National Survey on Drug Use and Health, 10.6% of adolescents reported binge drinking, 21.8% had used illicit drugs and 34.3% alcohol within the last year, with 8.9% using at a level severe enough to be classified as abusing or dependent on alcohol or other illicit drugs (SAMHSA 2004). While substance use and abuse involves a significant proportion of the adolescent population in the United States, only a small percentage seek or receive treatment (SAMHSA 2002). Access to treatment is important in reducing negative long-term consequences of adolescent SA, as it frequently co-occurs with other psychosocial and medical problems. Adolescents with a history of SA have a greater risk for depression (Deykin et al. 1987), chronic illnesses such as cardiovascular disease (CDCP 2002), auto accidents (CDCP 2002), and, for intravenous drug users, early death due to AIDS (CDCP 1997). Substance abusers are not only more likely participate in delinquent behavior, but are more likely to be victims of crime (Dakof 2000). Substance abuse among adolescents has been further linked to developmental lags, physiological effects on brain development, motivational deficits and other psychosocial dysfunction (Baumrind and Moselle 1985; Molidor et al. 2002). Approximately 90% of adults with a current SA disorder started before age 18, and half started before 15 (Dennis 2002). Therefore, early identification of SA problems and access to treatment are critical for adolescents.
However, little information is available about factors influencing treatment access. Research examining behavioral health service use by children and adolescents has typically been limited to individual characteristics and specific mental health needs of the population. We have been able to find only a few published studies applying community factors as predictors of SA (discussed below). Further, only a small number of studies link community indicators to access to care and none published to date link such factors to patterns of SA service utilization among adolescents.
This study is most closely an expansion of previous service utilization focused research, including that of Heflinger et al. (2002), whose work with a different population of children and adolescents investigated the impact of community and mental health service system factors on rates of child and adolescent psychiatric hospitalization. Community-level variables were found to be significant predictors and to increase explanation of variance in the model of hospitalization. Community predictors found to influence hospital use included county capacity for alternative placements while in state care, presence of a general or psychiatric hospital in the child’s home county, total county population, percent of county’s children living below the poverty level, and percentage of county’s children living in a single parent family household. Brooks-Gunn et al. (1998) found that residents in poor or middle income neighborhoods evidenced higher rates of emergency room visits than their more affluent counterparts. Other studies have also shown community characteristics to influence service use. Haas and colleagues (2004) demonstrated that the racial/ethnic composition of a county affected access to health care. Chow et al. (2003) found that community poverty impacted service use. Gresenz et al. (2000) found that greater HMO presence in a community led to higher overall access to care, while Fortney et al. (1999) and others (White 1986; Burgess and Defiore 1994; Schmitt et al. 2003) found that geographic factors, such as transportation and proximity to facility, impacted service use. Overall, however, research to explain the role of community context and ecological level characteristics as determinants of SA service utilization among adolescents is greatly limited.
In this analysis, community indicators are used to assess the broader impact of key aspects of community systems on a new set of adolescent service utilization measures being promoted by the Washington Circle Group (Cavanaugh and Doucette 2004; Garnick et al. 2002; McCorry et al. 2000): identification and treatment engagement, discussed in more detail below. Community indicators selected include a range of easily accessible publicly available measures that correspond to a theoretical model on service use. These indicators are bound within the context of county-level, geographic regions in Tennessee. Although more locally specific sub-strata (census tract or block level, for example) may be additionally informative, this analysis utilizes county-level indicators as a general step toward highlighting and understanding the importance of ecological characteristics on adolescent service utilization. The county level of analysis is also uniquely important as the county is the mechanism through which enrollment of TennCare recipients is organized and key state political and economic decisions are made and implemented.
Theoretical Model
For theoretical purposes, community indicators within the study are ecological constructs and understood as features, not only of groups of particular individuals living within a community, but of community systems as well (Prilleltensky et al. 2001). Our analysis includes community indicators in the context of resource-based advantage and disadvantage and assesses the impact of these ecological measures on the likelihood of two types of adolescent SA service utilization. This approach acknowledges the social-ecological context (Bronfenbrenner 1996) of individuals, in particular, that they live within families who reside in communities that are also influenced by broader societal factors. The potential mediating connections between community conditions and the mechanisms that produce particular behavioral and decision making outcomes are dealt with in fuller detail elsewhere (e.g., Schuck and Widom 2005). These and other studies have shown that a variety of social processes mediate the connection between community conditions and individual outcomes, including social capital, collective efficacy, availability of institutional resources, and normative routine activities (Sampson et al. 2002).
This framework also builds on the health services utilization models of Aday and Anderson (e.g., 1974, 1981; Andersen and Davidson 1996), as adapted by Heflinger and Brannan (2005, see Fig. 1). This model includes five sets of factors influential to service utilization and treatment outcomes, including predisposing, enabling, and needs of the population, as well as service system, and community factors. Predisposing characteristics of the population include demographic factors that may influence physical or behavioral health status as well as the use of services. Enabling characteristics of the population include the socioeconomic and psychosocial resources of youth and their families. Needs of the population usually indicate the reasons for the service and have been characterized in past research as the most powerful predictor of service use. In the case of behavioral health service use, the needs for the service may include the youth’s substance use and consequences of use, as well as emotional and behavioral symptoms or psychosocial functioning, or other problems that may affect service use. Service system characteristics include the policies, resources, and organization of the service system that are all sources of influence on the types and amounts of services potentially available and the procedures for accessing care. Community characteristics are local economic, social, and environmental measures, including concentration of poverty, population density, resource proximity, community disorder, strength and density of social ties, and other measures. Not only is the availability of treatment resources important, but also local norms and stigma associated with the use of services. Although some Aday and Andersen models include community resources under enabling characteristics (e.g., Gelberg et al. 2000), Heflinger and Brannan (2005) treated community characteristics as a separate set of variables—and level of analysis—that is critical for understanding service use. This approach was taken in this study.
Model of behavioral health services use and outcomes (Heflinger & Brannan, 2005) reprinted with permission of the authors
This theoretical framework serves as a conceptual guide toward understanding the relationship between ecological factors and service utilization and underscores the importance of county-level community factors in determining the likelihood of both access to and use of different types of health care. In addition, by adopting a community indicators approach, this study further acknowledges the particularistic nature of social service systems across geographic regions.
The purpose of this study was to examine the influence of the county-level factors shown in the theoretical model on two measures of adolescent service utilization for SA treatment, both independently as predictors at the aggregate level and as part of a multi-level analysis when added to other known individual and service system characteristics. This study focuses on one state’s Medicaid program and utilization of adolescent SA treatment and hypothesizes that, while individual need influences service use, community factors have unique explanatory value. In addition, it is hypothesized that community factors impact both the likelihood that substance abusing adolescents are identified as needing treatment, as well as, their likelihood of engaging in treatment once identified.
Methods
Overview: Medicaid in Tennessee
As the largest health insurance program in the country (Weil 2003), Medicaid is designed to provide health care coverage for low income individuals and families, the elderly, the blind and disabled, and Americans in need of long term care. TennCare, the Medicaid program implemented in the state of Tennessee under a Medicaid waiver to provide managed care and allow uninsured/uninsurable children and adults to enroll, provides health and behavioral health services to adults and children, including SA treatment (Saunders and Heflinger 2003). For anyone under the age of 21, a range of services is available including general medical care and the federal Early and Periodic Screening Diagnosis and Treatment program (CMS 2003; Tennessee Department 1999).
Other studies have found that those insured by Medicaid are more than twice as likely to get alcohol treatment than those with private insurance (Harwood et al. 2001), suggesting that data presented here may provide a more optimistic view of outcomes among adolescents accessing and engaging SA treatment, than might be expected for other insured populations. However, comparison of rates of adolescent access to Medicaid-funded SA treatment has demonstrated that Tennesse had lower service utilization rates than states in the Northwest (Heflinger et al. 2004).
Participants
This is a population-based study, including all adolescents who were enrolled in TennCare in fiscal year 2000. During this time period, almost 190,000 Tenneseans between the ages of 12 and 17 were enrolled in TennCare. Approximately one-third (37%) of these adolescents were minority, almost exclusively African-American, and nearly half were female (49%). Different analyses focused on different sets of participants. For identification, the entire enrolled population was included. For treatment engagement, only those youth who were identified, and thus, eligible for engagement, were included.
Claims Data
This study is a secondary analysis of claims/encounter and enrollment data from the Bureau of TennCare. For this study, paid claims/encounters were included for youth ages 12–17 across the ninety-five counties in the state of Tennessee for fiscal year (FY) 2000.
Measures
To test the theoretical models, measures at the individual youth and community levels were constructed.
Identification and Treatment Engagement
Dependent measures are “identification” of a SA problem, indicating initial access to care, and “engagement” of treatment. The operationalization of these variables follows the work of the Washington Circle Group (Cavanaugh and Doucette 2004; Garnick et al. 2002; McCorry et al. 2000) in developing performance measures for SA treatment that could be standardized and widely adopted (Hermann and Palmer 2002). In fact, these measures were adopted for inclusion in the Health Plan Employer Data and Information Set starting in 2004 (NCQA 2004), and Lee and colleagues (2004) have applied these to adolescents in the private sector. Adolescents identified as gaining access to care are defined as those who had at least one visit with a SA diagnosis. In this study, this was the first visit with a SA diagnosis following at least a 60 days “clean” period, assumed to reflect a new episode of treatment within that fiscal year. For county-level indicators, percent identified were calculated as adolescent members with any SA claim divided by the total number of youth enrolled in TennCare in that county.
Treatment engagement indicates that the service system has retained the adolescent client in SA treatment for at least two subsequent treatment visits following their identification services. Two important components of the engagement definition are the timing of those follow-up services and the type of identification service: after identification a patient is considered “initiated” into treatment by receiving one follow-up service within 14 days of identification and “engaged” after a second service in the next 30 days (i.e., two follow-up services must be received within approximately 6 weeks). If the identification service is inpatient or residential treatment, the person is assumed to be initiated, and therefore engagement requires only one follow-up service in the 30 days post-discharge. The county-level rate of engagement is the number of youth in the county who were engaged divided by the number of TennCare enrollees in the county who were identified, as specified above.
Individual-level Demographic Characteristics and Eligibility Status
The independent variables at the individual level were those available in the TennCare enrollment and encounter data sets and were dummy variables for youth’s gender (female vs. male), past SA and mental health treatment prior to identification (any vs. none), and type of Medicaid eligibility category found in the enrollment files for that fiscal year. Eligibility for TennCare was described using five categories: Uninsured or uninsurable (Tennessee Medicaid waiver categories), Supplemental Security Income (SSI), Title IV-E for youth in foster care (FC), and Temporary Assistance for needy Families (TANF), and Other Poverties, which included all other income-based eligibility categories. Since in the TennCare data very few (less than 1%) non-white enrollees were coded as other than black enrollees, we created a dichotomous variable for white versus racial minority, with white being the reference. For the engagement analyses, we also included a dummy variable indicating whether the treatment setting in which they were identified was an overnight setting (inpatient or residential treatment) or outpatient in order to examine the influence of service type. The individual-level variables were all obtained about each adolescent’s first SA claim. These independent variables reflect the individual-level predisposing and enabling factors in the theoretical model. Neither the enrollment nor the encounter/claims data sets included “need” variables that could be included in these analyses.
Community Indicators
At the county level, ecological variables related to county advantage and disadvantage were obtained from existing data sources. Measures reflecting educational attainment, family resources, minority presence, criminal justice activity, and treatment resources were chosen to tie into the previous literature and link to the theoretical model. Educational attainment is an indicator of a community’s social capital and is particularly salient with regards to at-risk youth (Coleman 1988; Furstenberg and Hughes 1995). Poverty and neighborhood disorder have often been linked with behavioral health problems (e.g., Aneshensel and Sucoff 1996). Prevalence of minority individuals has been shown to explain variation in access to services (Haas et al. 2004). Census 2000 data included variables on proportion of families within a county that are headed by a single parent, high school graduation rate as proportion of persons ages 25 or above, median family income, and proportion of racial minority residents. Measures of criminal justice activity reflect not only neighborhood disorder but attitudes about treatment versus incarceration (Breda 2001; Robinson et al. 2003). The number of drug-related arrests for persons (over age 15) per county were obtained from Uniform Crime Statistics. Data from the Tennessee Council of Juvenile and Family Court Judges were used to compute proportion of juveniles (under age 17) held in detention. Finally, availability of institutional resources was documented through enumeration of TennCare SA facilities and providers in each county from TennCare provider lists. From this, the proportion of providers to number of adolescent TennCare enrollees for each county was calculated.
Analyses
First, descriptive analyses were conducted to compare youth who were identified or engaged to those who were not. Next, two different approaches were taken to examine factors influencing each of the service utilization variables. As Luke (2005) has previously suggested and others have demonstrated (Robinson et al. 2003), multi-level modeling has been utilized to address the issue of context in community science.
Part I: County-level Analyses
The first set of analyses examined variation in county-level estimates of treatment access and treatment engagement by estimating separate linear regression models using the county rates as the dependent variables and the community indicators listed above as covariates.
Part II: Multi-level Analyses
The second set of analyses takes advantage of the project’s access to disaggregated data. Individuals living in the same counties likely share characteristics that influence their identification and engagement, such as similar treatment systems and cultural attitudes about substance use and treatment, which violates the usual assumption of independence of observations in analyses like Part I. The consequence of this violation is bias in test statistics due to an understatement of the standard errors (Raudenbush and Bryk 2003).
The analysis estimated two random effects models for each outcome variable.Footnote 1 Model 1 allows for a county-specific, random intercept term and individual-level covariates (e.g., youth’s race and gender) that influence an individual’s propensity to be identified or engaged by the treatment system. Model 2 uses the same individual-level covariates but adds county-level characteristics that potentially explain the random intercept. In both models, the level-1 slopes are fixed; only the intercept term is random. Conceptually, this represents the effect of living in a particular county on the county average probability of being identified or engaged by the treatment system. Both models used HLM software (Raudenbush et al. 2003) and report robust (heteroskedasticity-corrected) standard errors.
The multi-level analysis estimates a logistic regression of whether the individual had the particular outcome (i.e., identified or not; engaged or not) as a function of the individual-level covariates described above:
where X is the vector of individual-level regressors.
The intercept term, β 0j which represents the average effect in each of Tennessee’s 95 counties, is estimated as a random term with no covariates (Model 1, below)Footnote 2:
and also with the full set of county-level indicators (W) (Model 2, below):
The county-level variables help to “explain away” the variability in average identification and engagement rates across counties, which, in turn, improves our assessment of the role of individual-level factors like race and gender on the likelihood of using SA services.
Results
Of all of the adolescents enrolled during FY2000, 1,670 total youth (0.88%; SE = 0.0937) met the criteria for identification during that year; of those identified, 475 became engaged in treatment (28.4%; SE = 0.4513). County-level identification rates ranged from 0% to 2.3% (mean 0.97%, SD 0.5) of TennCare enrolled youth, and county-level engagement rates ranged from 0% to 100% (mean 25.5%, SD 19) of those who had been identified. Table 1 compares youth who were identified and engaged with those who were not. Those identified were significantly more likely to be white, male, older, and eligible through FC than those who were not identified. Note that the differences between engaged and not engaged youth, all of whom had been identified with at least one SA service, were primarily non-significant statistically.
A description of the community indicators is also informative. Across the ninety-five counties in the year 2000, the median family income was $30,959, ranging from $19,760 to $69,104. The proportion of families with children headed by a single parent was 11.4%. Total yearly drug arrests were 50 per 1,000 persons (0.5%). The mean number of juveniles detained was .94 per 1,000. Eleven (11.6%) of counties had no SA providers available within their county. Figure 2 presents a mapping of the concentration of TennCare SA treatment facilities/providers and enrolled TennCare youth by county. County-level identification rates ranged from 0% to 2.3%, with an average of 1.0% statewide. County-level engagement rates ranged from 0% to 100%, with an average of 25.5%.
Part I: County-level Analyses
Identification
When explaining adolescent SA identification rates among TennCare recipients by county, measures of both community disadvantage and advantage were found to be importantly linked to higher rates of identification (see Table 2). Disadvantage characteristics that were statistically significant predictors included higher proportion of single parent families, increased rates of drug related arrests among persons over the age of 25, and lower proportions of minority residents. Measures of greater community advantage that were significantly associated with higher rates of identification included higher median income, greater proportion of persons having graduated from high school, and greater concentration of treatment facilities. Also significantly predictive was the proportion of juveniles held in detention, with lower rates of detention linked to higher rates of SA identification.
Engagement
The county-level explanatory model of treatment engagement is less revealing, with higher median income as the only significantly predictive predictor. Excluding income level, other community indicators did not help explain further treatment engagement at the county level, and the overall model predicted only 4% of the variance (see Table 2).
Part II. Multi-level Analyses
Identification
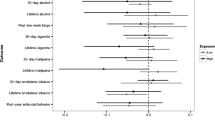
Table 3 presents the results of the multi-level logistic regression for identification of SA problems. Model 1 displays the effects of the individual-level covariates and the nesting of individual observations within counties. That is, the regression includes individual-level predictors only, but allows for each county to have its own unique contribution to change in the level of the intercept (i.e., the average rate of identification) through the random error term. Prior use of substance use or mental health treatment were the strongest predictors of a youth being identified.
Minority and female youth were significantly less likely than white or male youth to be identified with a substance use problem in FY2000. The (log) odds of being identified were nearly 2.5 times greater for FC youth relative to youth on SSI; youth enrolled in a poverty-related program were also more likely to be identified than youth on SSI. Youth in the TennCare expansion enrollment category—uninsured/uninsurable—were no more likely to be identified relative to youth on SSI.
Model 2 (also shown in Table 3) adds the county characteristics, which reduce the unexplained variance (i.e., the size of the unique county contribution to the average rate of identification) in the intercept at level-1. The greatest effect is of income: a unit increase in the (natural log) median income has 2.8 times the (log) odds of being identified. This corresponds to an increase in income from about $19,000–$52,000, or roughly the difference of being in one of the poorest counties of Tennessee and one of the wealthiest.
The other county characteristics have smaller, but significant effects on identification rates. Living in a county with a higher proportion of minority residents and a greater rate of juvenile detention had lower identification rates through TennCare. On the other hand, greater proportions of adults over 25 who graduated high school, single-parent families, and TennCare treatment facilities and higher drug arrest rates increased the chances of identification. Higher proportions on minority residents and greater numbers of juvenile in detention significantly decreased the chances of identification. The results for Model 1’s individual-level predictors hold even after accounting for county-level predictors of identification.
In each model, the random-intercept terms significantly differ from zero (Model 1: χ 2 (94) = 341.75, p < 0.001; Model 2: (χ 2 (87) = 170.09, p < 0.001). Comparing the fit of the two models in terms of their respective deviance statistics, the added county specific characteristics of Model 2 are significant. The unadjusted intraclass correlation (ICC) of observations for identification in a given county is .050. Adding the level-1 and level-2 covariates reduces the conditional ICC to .036 and .016, respectively. That is, after adjusting for the characteristics included in the model, observations in the same county have even less interdependence. Adding the level-1 covariates explains 57.8% of the variation in identification rates; adding the level-2 covariates raises that to 70.0%.
Engagement
Whereas nearly all the individual-level predictors were important in predicting identification, the results of Model 1 reveal none were important for predicting engagement (see Table 4). Youth of different races, genders, age, prior service use, and TennCare enrollment categories had equivalent chances of being engaged in treatment, as did those who were identified in outpatient versus inpatient/residential treatment. Except for income and juvenile detention rates, the county-level predictors from Model 2 were not significant, and adding the county-level variables failed to improve the model fit. As in the identification models, youth from counties with higher income had a greater chance of becoming engaged. Youth in counties with higher juvenile detention rates were less likely to engage in treatment.
The random intercepts in each engagement model significantly differ from zero (Model 1: χ 2 (92) = 150.91, p < 0.001; Model 2: χ 2 (85) = 126.93, p < 0.002). The unadjusted intraclass correlation (ICC) of observations for engagement in a given county is .053. Adding the level-1 and level-2 covariates reduces the conditional ICC to .050 and .027, respectively. That is, after adjusting for the characteristics included in the model, observations in the same county have less interdependence. However, the bulk of this reduction comes from adding the county-level factors. Adding the level-1 covariates explains 46.3% of the variation in engagement rates; adding the level-2 covariates raises that to 50.2%.
Figures 3 and 4 present the relationship between income and identification and engagement rates, respectively. The line represents the levels of income associated with a corresponding percent of enrollees identified (Fig. 3) or percent of those identified who became engaged in treatment (Fig. 4), evaluated at the means of the other regressors.
Limitations
This study includes only adolescents in Tennessee’s Medicaid service system, which limits its generalizability. In addition, only Medicaid/TennCare claims and encounter data were included. This may be an underestimate of total service use as the youth may receive services through other treatment sectors. However, in this state, the Medicaid program is intended to pay for all types of SA services for adolescents in their comprehensive benefit package. As in other states, the Substance Abuse, Prevention and Treatment Block Grant is the other source of publicly-funded SA services for adolescents in Tennessee (Northrup and Heflinger 2000) and is intended to be used for adolescents with no other public or private insurance. The focus of this study is on how Tennessee’s Medicaid program, which is intended as the primary insurer for this population, identifies and treats substance use problems among its enrollees. An additional limitation is that the encounter/claims data do not include a measure of the severity of the youth’s substance use problem (e.g., abuse versus dependence), which would be a measure of need in the theoretical model. However, the TennCare data are an important policy tool that can be used in every state to provide information on the performance of this publicly-funded service system.
Discussion
This study highlights the importance of ecological-community indicators in the explanation of variations in patterns of SA service utilization among adolescents receiving Medicaid-funded treatment in Tennessee. Our study suggests that while individual level attributes and need are important predictors of SA treatment, community factors have unique explanatory value. In both county- and individual-level analyses, aggregated community-level indicators were found to be importantly linked to identification for SA treatment. Most notably, higher rates of high school graduation rates, drug related arrests, median income, concentration of single-parent families, and presence of treatment facilities are found to be important predictors of which counties had higher identification of SA problems among their resident adolescents. Lower rates of minority residents and of juveniles held in detention were additionally related.
In both descriptive and multi-level analyses, female and minority youth, and those youth living in counties with higher proportions of minority residents, were less likely to be identified for SA treatment. These findings correspond with those of Heflinger et al. (2006), who examined gender and racial disparities in SA treatment utilization. The addition of the significant county-level indicator in this study suggests that these disparities are systemic. As noted previously, once youth enter the treatment system by being identified, however, race and gender factors are not related to rates of treatment engagement. These finding underscore the importance of using multi-level modeling to explaining behavioral outcomes.
Another important individual-level finding for Tennessee relates to the TennCare eligibility expansion enrollment category of uninsured and uninsurable children. Youth in this expansion category were no more likely to use services than youth in the SSI enrollment category, while those in the poverty or FC categories were more likely to be identified. This is important for Tennessee because the state is in the process of disenrolling older teens in the expansion category from the TennCare program as a money-saving strategy (THCC 2005). Normally, the SSI category is thought of as a high service use category, but most disabled children do not have substance use problems, so having lower identification rates makes them likely to be a low-use category in this context. Likewise, these findings indicate that disenrollment of youth in the uninsured/uninsurable category would not lead to expected cost savings.
An additional concern is the low rate, in general, of treatment identification and even lower rate of engagement. Recent estimates for Tennessee indicate a rate of substance dependence or abuse of 7.9% (SAMHSA 2004), which is far above the less than 1% identification rate found here. The lack of identification and engagement likely does not reflect an absence of need for services within the TennCare population, but a dearth of needed resources. In addition, even though Medicaid benefits are equivalent across individuals, our analysis reveals that access to services differ at the county level. Such findings can be used by community researchers and advocates to challenge policy proposals that decrease resources to certain groups.
Community practitioners and resources will also want to consider systemic-level changes in service delivery, for instance at the county or state level. One option would be the integration of or better communication between resources or systems of service provision. Bird and colleagues (1998) described models for integrating primary care, mental health, and SA treatment. Gale and Deprez (2003) recommended a public health approach—not only should concern be focused on those who have been identified with SA problems, but also on the entire at-risk population. Early identification of children and adolescents at risk for behavioral health problems should be incorporated into school systems and primary care models. In addition to prevention strategies, however, Tseng and colleagues (2002) stressed the need to move toward models focusing on promotion of wellness and social competence. The Substance Abuse and Mental Health Services Administration (2006) emphasizes an approach that includes prevention and well as treatment, and attention to supporting recovery and resilience.
When working at the system level, it is also critical to acknowledge the local context in behavioral health interventions. Miller and Willoughby (1997) proposed changes in the system of SA treatment delivery that accounted for “a need for greater attention to the community context within which SA occurs, and to local culture-specific resources that can stimulate and support change” (p. 83). They criticized individually-focused interventions and advocated for a system that was not only based on brief, more readily available therapy, but also on interventions using other community resources. Utilization of natural community resources such as the family unit, employee services, and pastoral care was suggested.
It should be noted that, by far, the largest effect among the county-level predictors for both identification and engagement was median family income. This seems self-evident as counties with higher incomes likely have more resources with which to treat youth with substance problems. The availability of TennCare-approved SA treatment providers was significant in predicting identification but not treatment engagement, and since TennCare operates as an insurance program rather than on a public-clinic model, wealthier counties do not have an obvious resource advantage in treating this population. Consumers, family members, service providers and administrators, community practitioners and researchers, and state agency personnel should be encouraged to participate in joint planning and action and advocate for both community- and state-wide changes that could improve access to care. Two obvious community-level targets, based on these findings, are decreasing community poverty and enhancing educational outcomes for all residents.
Mulder et al. (2003) described a community-level intervention using an “asset identification perspective.” They move from a participatory community needs assessment to strategies for mobilizing community residents to advocate for and build the needed resources. Motivation techniques, social reinforcement, and conflict management are all recognized as effective tools in building community-based sustainable interventions. Similarly, they emphasized the need to recognize the uniqueness of communities and to use culturally adapted methods and procedures.
Such approaches could also address community attitudes and stigma about substance use problems and treatment. This relates to what may appear to be a counter-intuitive finding in the inverse relationship between juvenile detention rates and SA system outcomes. One might expect higher detention rates to lead to greater identification or treatment engagement, as youth involved with illegal drugs may be expected to have greater law enforcement contact. However, youth in detention may access SA services through different mechanisms than the TennCare insurance program or enter the correctional instead of the treatment system. Perhaps this finding also indicates that counties have different strategies for dealing with their troubled youth. Some counties may lean towards incarceration or draw on law enforcement as the only mobilized resource, while some provide a greater focus on treatment. Attention to these community and court attitudes is also important (Breda 2001) in order to improve access to treatment.
The analysis applied in this study, in examining both county-level rates of service use and county-level predictors of individual service use, is important for demonstrating the overall impact of ecological conditions on adolescent behavior and treatment, an important finding given the fact that the administration of such services are often managed at the county level. These findings underscore the importance of community context in the likelihood of substance abusing identification and follow-up treatment and suggest that researchers, policy makers and service providers ought to pay additional attention to community ecology as an independent predictor of adolescent behavior and health service utilization. Further supported is the assertion that more locally specific studies are needed. Although aggregated data demonstrate important results regarding the impact of community, important, too, is the particular nature and functioning of the TennCare system across geographic, in this case county, boundaries. Further analysis conducted at the census tract or block level may be additionally informative for understanding directly how local conditions impact adolescents with SA problems and their ability to access and use this publicly-funded treatment system.
Notes
Fixed effects specifications were tested, but the random effects specification was superior. (Results available from authors.)
The model was estimated alternatively with a fixed- or random-intercept. The random-intercept model fit better.
References
Aday, L. A., & Andersen, R. A. (1974). A framework for the study of access to medical care. Health Services Research, 9, 208–220.
Aday, L. A. & Anderson, R. (1981). Equitiy of access to medical care: A conceptual and Empirical Overview. Medical Care, 19(Suppl. 12), 4–27.
Alison, K. W., Crawford, P. E., Leone, E., Tricket, A., Perez-Febles, A., Burton, L., & Le Blanc, R. (1999). Adolescent substance use: Preliminary examinations of school and neighborhood context. American Journal of Community Psychology, 27(2), 111–142.
Andersen, R. M., & Davidson, P. L. (1996). Measuring access and trends. In R. M. Anderson, T. H. Rice, & G. F. Kominski (Eds.), Changing the U.S. health care system: Key issues in health services, policy, and management (pp. 13–40). San Francisco: Jossey-Bass.
Aneshensel, C., & Sucoff, C. (1996). The neighborhood context of adolescent mental health. Journal of Health and Social Behavior, 37, 293–310.
Bauer, R. A. (1966). Social indicators. Cambridge:MIT.
Baumrind, D, & Moselle, K. A. (1985). A developmental perspective on adolescent drug abuse. In J. S. Brook, D. J. Lettieri, D. W. Brook, & B. Stimmel (Eds.), Alchohol and substance abuse in adolescence (pp. 41–76). New York: The Hawthorne Press.
Bird, D. C., Lambert, D., Hartley, D., Beeson, P. G., & Coburn, A. F. (1998). Rural models for integrating primary care and mental health services. Administration and Policy in Mental Health, 25(3), 287–308.
Breda, C. (2001). The mental health orientation of juvenile courts. Journal of Behavioral Health Services Research, 28(1), 89–95.
Bronfenbrenner, U. (1996). The ecology of human development: Experiments by nature and design. Cambridge: Harvard University Press.
Brooks-Gunn, J., McCormick, M. C., Klebanov, P. K., & McCarton, C. (1998). Health care use of 3 year-old low birthweight premature childhood: Effects of family and neighborhood poverty. The Journal of Pediatrics, 132(6), 971–975.
Burgess, J. F., & Defiore, D. A. (1994). The effect of distance to VA facilities on the choice and level of utilization of VA outpatient services. Social Science and Medicine, 39, 95–104.
Cavanaugh, D. A., & Doucette, S. A. (2004). Using administrative data to assess the process of treatment services for adolescents with substance use disorders. Journal of Psychoactive Drugs, 36(4), 473–481.
Centers for Disease Control, Prevention (CDCP). (1997). Update: Trends in AIDS incidence, deaths, and prevalence—United States, 1996. Morbidity and Mortality Weekly Report, 46(8), 165–178.
Centers for Disease Control and Prevention (CDCP). (2002). Youth risk behavior surveillance—United States, 2001. Morbidity and Mortality Weekly Report, 51, No SS-4.
Center for Medicaid, & Medicaid Services (CMS). (2003). Overview of the Medicaid Program. Washington, DC: Author.
Chapin, L. W., & Denhardt, R. (1995). Putting ‘Citizens First’ in Orange County, Florida. National Civic Review, 84(3), 210–217.
Chow, J. C. C., Jaffe, K., & Swanson, L. (2003). Racial/ethnic disparities in the use of mental health services in poverty areas. American Journal of Public Health, 93(5), 792–797.
Coleman, J. S. (1988). Social capital in the creation of human capital. American Journal of Sociology, 94(Suppl. 95), S95–120.
Cunningham, P. J. (1999). Pressures on safety net access: The level of managed care penetration and uninsurance rate in a community. Health Services Research, 34(1, Part II):255–270.
Cunningham, P. J., & Kemper, P. (1998). Ability to get medical care for the uninsured: How much does it vary across communities? Journal of the American Medical Association, 280(10), 921–927.
Dakof, G. (2000). Understanding gender differences in adolescent drug abuse: Issues of comorbidity and family functioning. Journal of Psychoactive Drug, 32(1), 25–32.
Dennis M. L. (2002). Treatment research on adolescents drug and alcohol abuse: Despite progress, many challenges remain (Invited Commentary). Connection. Washington, DC: Academy for Health Services Research and Health Policy.
Deykin, E. Y., Levy, J. C., & Wells, V. (1987). Adolescent depression, alcohol and drug abuse. American Journal of Public Health, 77(2), 178–182.
Farrington, D. (1991). Childhood aggression and adult violence. In D. Peplet & K. H. Rub (Eds.), The development and treatment of childhood aggression (pp. 5–29). Hillsdale: Lawrence Erlbaum.
Fortney, J., Rost, K., Zhang, M., & Warrren, J. (1999). The impact of geographic accessibility on the intensity and quality of depression treatment. Medical Care, 37(9), 884–893.
Furstenberg, F. F., & Hughes, M. E. (1995). Social capital and successful development among at-risk youth. Journal of Marriage and the Family, 57(3), 580–592.
Gale, J. A., & Deprez, R. D. (2003). A public health approach to the challenges of rural mental health service integration. In B. H. Stamm (Ed.), Rural behavioral health care: An interdisciplinary guide (pp. 95–108). Washington, DC: American Psychological Association.
Garnick, D. W., Lee, M. T., Chalk, M., Gastfriend, D., Horgan, C. M., McCrory, F., McLellen, A. T., & Merrick, E. L. (2002). Establishing the feasibility of performance measures for alcohol and other drugs. Journal of Substance Abuse Treatment, 23, 375–385.
Gelberg, L., Andersen, R. M., & Leake, B. D. (2000). The behavioral model for vulnerable populations: Applications to medical care use and outcomes for homeless persons. Health Services Research, 34(6), 1273–1302.
Gresenz, C. R., Stockdale, S. E., & Wells, K. B. (2000). Community effects on access to behavioral health care access to behavioral health care. Health Services Research, 35(1), 293–306.
Gruenewald, P. J., Treno, A. J., Taff, G., & Klitzne, M. (1997). Measuring community indicators: A systems approach to drug and alcohol problems. London: Sage.
Haas, J. S., Phillips, K. A., Sonneborn, D., McCulloch, C. E., Baker, L. C., Kaplan, C. P., Perez-Stable, E. J., & Liang, S. (2004). Variation in access to health care for different racial/ethnic groups by the racial/ethnic composition of an individual’s county of residence. Medical Care, 42(7), 707–714.
Harwood, H. J., Field, T., & Tunkelrott, T. (2001). Evaluating the performance of substance abuse detoxification providers using treatment engagement as an outcome measure (NIDA Contract No. P50 DA 10233). Falls Church: The Lewin Group.
Heflinger, C. A., & Brannan, A. M. (2005). Substance use disorders and service use among rural youth: Proposal submitted to NIDA. Nashville: Vanderbilt University.
Heflinger, C. A., Chatman, J., & Saunders, R. C. (2006). Racial and gender differences in utilization of Medicaid substance abuse services among adolescents. Psychiatric Services, 57, 504–511.
Heflinger, C. A., Saunders, R. C., Mulkern, V., Hughes, D., Gabriel, R., Deck, D., Wamber-lacey, D., & Perry, P. (2004). Access to Medicaid-financed substance abuse treatment services for adolescents. Nashville :Vanderbilt University.
Heflinger C. A., Simpkins C. G., & Foster E. M. (2002). Modeling child and adolescent psychiatric hospital utilization: A framework for examining predictors of service use. Children’s Services. Social Policy, Research, and Practice 5(3), 151–172.
Hermann, R. C., & Palmer, R. H. (2002). Common ground: A framework for selecting core quality measures for mental health and substance abuse care. Psychiatric Services, 53(3), 281–287.
Hurlburt, M., Leslie, L., Landsverk, J., Barth, R., Burns, B., Gibbons, R., Slymen, D., & Zhang, J. (2004). Contextual predictors of mental health service use among children open to child welfare. Archives of General Psychiatry, 61, 1217–1224.
Jencks, C., & Mayer. S. (1990). The social consequences of growing up in a poor neighborhood. In L. Lynn, Jr. & M. McGeary, (Eds.), Inner-city poverty in the United States (pp. 111–186). Washington D.C.: National Academy Press.
Johnston, L. D., O’Malley, P. M., & Bachman, J. G (2002). Monitoring the future National survey results on drug use, 1975–2001. Volume I: Secondary school students (NIH Publication No. 02–5106). Bethesda: National Institute on Drug Abuse.
Kingsley, G. (Ed.). (1999). Building and operating neighborhood indicator systems: A guidebook. A national neighborhood indicator partnership report. Washington, DC: Urban Institute.
Latkin, C. A., & Curry, A. D. (2003). Stressful neighborhoods and depression: A prospective study of the impact of neighborhood disorder. Journal of Health & Social Behavior. 44(1), 34–44.
LeClere, F. B., Rogers, R. G., & Peters, K. (1998). Neighborhood social context and racial differences in women’s heart disease mortality. Journal of Health & Social Behavior, 39, 91–10.
Lee, M. T., Garnick, D. W., Miller, K., & Horgan, C. M. (2004). Adolescents with substance abuse: Are health plans missing them? Psychiatric Services, 55, 116.
Levanthal, T., & Brooks-Gunn, J. (2000). The neighborhoods they live-in: The effects of neighborhood residence on child and adolescent outcomes. Psychological Bulletin, 126, 309–337.
Leventhal, T., & Brooks-Gunn, J. (2003). Moving to opportunity: An experimental study of neighborhood effects on mental health. American Journal of Public Health, 93(9), 1576–1582.
Luke, D. A. (2005). Getting the big picture in community science: Methods that capture context. American Journal of Community Psychology, 35(3/4), 185–200.
Mankowski, E., Humphrey, K., & Moos, R. (2004). Individual and contextual predictors of involvement in twelve-step self-help groups after substance abuse treatment. American Journal of Community Psychology, 29(4), 537.
McCorry, F., Garnick, D. W., Bartlett, J., Cotter, F., & Chalk, M. (2000). Developing performance measures for alcohol and other drug services in managed care plans. Journal of Quality Improvement, 26(11), 633–643.
Miller, W. R., & Willoughby, K. V. (1997). Designing effective alcohol treatment systems for rural populations: Cross-cultural perspectives. In U.S.D.H.H.S. Substance Abuse and Mental Health Services Administration, Bringing excellence to substance abuse services in rural and frontier America (pp. 83–92), TAP Series 20, Rural Information Center Health Service (RICHS). (Rockville: U.S.D.H.H.S.) (DHHS Publication No. (SMA) 97–3134.
Molidor, C., Nissen, L., & Watkins, T. (2002). The development of theory and treatment with substance abusing female juvenile offenders. Child and Adolescent Social Work Journal, 19(3), 209–225.
Mulder, P. L., Linkey, H., & Hager, A. (2003). Needs assessment in rural communities. In B. H. Stamm (Ed.), Rural behavioral health care: An interdisciplinary guide (pp. 67–80). Washington, DC: American Psychological Association.
National Committee for Quality Assurance (NCQA). (2004). The Health Plan Employer Data and Information Set (HEDIS). Washington, DC: Author. Available at http://www.ncqa.org.
Northrup, D., & Heflinger, C. A. (2000). Substance abuse treatment services for publicly-funded adolescents in the state of Tennessee. Nashville: Vanderbilt Institute for Public Policy Studies, Center for Mental Health Policy.
Prilleltensky, I., Nelson, J., & Peirson, L. (Eds.). (2001). Promoting family wellness and preventing child maltreatment. University of Toronto Press.
Raudenbush, S. W., & Bryk, A. S. (2003). Hierarchical Linear Models : Applications and data analysis methods (2nd ed.). Newbury Park: SAGE Publications.
Raudenbush, S. W., Bryk, A. S., Cheong, Y. F., & Congdon, R. T. (2003). HLM5 hierarchical linear modeling. Chicago: Scientific Software International.
Robinson, J., Lawton, B., Taylor, R, & Perkins, D. (2003). Multilevel longitudinal impacts of incivilities: Fear of crime, expected safety, and block satisfaction. Journal of Quantitative Criminology, 19(3), 237–274.
Rosenheck, R., & Lam, J. A. (1997). Client and site characteristics as barriers to service use by homeless persons with serious mental illness. Psychiatric Services, 48(3), 387–390.
Sampson, R. J., Morenoff, J. D., & Gannon-Rowley, T. (2002). Assessing “neighborhood effects”: Social processes and new directions in research. Annual Review of Sociology, 28, 443–478.
Saunders, R. C., & Heflinger, C. A. (2003). Access to patterns of use of behavioural health services among children and adolescents in TennCare. Psychiatric Services, 54, 1364–1371.
Sawicki, D., & Craig, W. J. (1996). The democratization of data. Journal of the American Planning Association, 62(4), 512–523.
Sawicki, D., & Flynn, P. (1996). Neighborhood indicators: A review of the literature and an assessment of conceptual and methodological issues. Journal of the American Planning Association: 62(2), 165–182.
Schuck, A., & Widom, K. S. (2005). Understanding the role of neighborhood context in the long-term criminal consequences of child maltreatment. American Journal of Community Psychology, 36, 207–222.
Schmitt, S. K., Phibbs, C. S., & Piette, J. D. (2003). The influence of distance on utilization of out patient mental health after care following inpatient substance abuse treatment. Addictive Behaviors 28(6), 1183–1192.
Speer, P. W., Ontkush, M., Schmitt, B., Raman, P., Jackson, C., Rengert, K. M., & Peterson, N. A. (2003). The intentional exercise of power: Community organizing in Camden, New Jersey. Journal of Community and Applied Social Psychology, 13, 399–408.
Substance Abuse and Mental Health Services Administration (SAMHSA). (2002). Results from the 2000–2001 National Household Survey on Drug Abuse: Volume 3 (Table 5.28).
Substance Abuse, Mental Health Services Administration (SAMHSA). (2004). Results of the 2002–2003 National Survey of Drug Use and Health. Rockville: Author.
Substance Abuse, Mental Health Services Administration (SAMHSA). (2006). The Matrix Priority Programs: Addressing Unmet and Emerging Needs. Rockville: Author.
Tennessee Department of Finance and Administration, Bureau of TennCare. (1999). TennCare Standard Operating Procedures (TSOP-36 & Addendum: Early and Periodic Screening, Diagnosis, and Treatment (EPSDT)). Nashville: Author.
Tennessee Health Care Campaign (THCC). (2005). TennCare Fact Sheet on ALL the Cuts. Nashville: Author. Available at: http://www.tenncare.org/GovernorsPlan/who_will_be_cut.html. Accessed May 24, 2006.
Tseng, V., Chesir-Teran, D., Becker-Klein, R., Chan, M. L., Duran, V., Roberts, A., & Bardoliwalla, N. (2002). Promotion of social change: A conceptual framework. American Journal of Community Psychology, 30, 401–427.
Weil, A. (2003). There is something about Medicaid. Health Affairs, 22, 13–30.
White, S. L. (1986). Travel distance as time price and the demands for mental health services. Community Mental Health Journal, 22, 303–313.
Wilson, W. J. (1990). The truly disadvantaged: The inner-city, the underclass, and public policy. Chicago: University of Chicago Press.
Yoshikawa, H. (1994). Prevention as cumulative protection: Effects of early family support and education on chronic delinquency and its risks. Psychological Bulletin, 115, 28–54.
Yuen, E. J., Gerdes, J. L., & Gonzales, J. J. (1996). Patterns of rural mental health care: An exploratory study. General Hospital Psychiatry, 18(1), 14–21.
Acknowledgements
Preparation of this article was supported by Center for Substance Abuse Treatment in the Substance Abuse and Mental Health Services Administration (1KD1 TI112328) and the National Institute on Drug Abuse (RO1 DA12982, R21 DA017682).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jones, D.L., Heflinger, C.A. & Saunders, R.C. The Ecology of Adolescent Substance Abuse Service Utilization. Am J Community Psychol 40, 345–358 (2007). https://doi.org/10.1007/s10464-007-9138-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10464-007-9138-8