Abstract
Informed by the Health Care Empowerment Model, a measure of PrEP Empowerment was developed and assessed for preliminary reliability and validity. Participants (N = 100) were invited to complete a survey during regular clinic visits. A subset (n = 84) volunteered to provide blood samples to assess plasma tenofovir (TFV) levels for recent PrEP adherence. A five-factor measure explained 70% of the total variance. Associations with internalized PrEP stigma, PrEP adherence self-efficacy, and plasma TFV were assessed. Results supported the multidimensional nature of PrEP Empowerment and reliability and validity. Additional research is needed in populations with varying PrEP experience and greater gender and ethnic representation.
Resumen
Basado en el modelo de empoderamiento de atención médica, se desarrolló y evaluó una medida de empoderamiento de la PrEP para determinar su confiabilidad y validez preliminares. Se invitó a los participantes (N = 100) a completar una encuesta durante las visitas regulares a la clínica. Un subconjunto (n = 84) se ofreció como voluntario para proporcionar muestras de sangre para evaluar los niveles de tenofovir (TFV) en plasma para la adherencia reciente a la PrEP. Una medida de cinco factores explicó el 70% de la varianza total. Se evaluaron las asociaciones con el estigma internalizado de la PrEP, la autoeficacia de la PrEP y el TFV plasmático. Los resultados respaldaron la naturaleza multidimensional de PrEP Empowerment y la confiabilidad y validez. Se necesita investigación adicional en poblaciones con diferentes experiencias de PrEP y una mayor representación étnica y de género.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Health Care Empowerment Model conceptualizes patient participation and engagement in healthcare [1]. The model specifies a process of healthcare engagement including being engaged, informed, collaborative, committed, and tolerant of uncertainties. Importantly, the model presupposes an interaction between context (e.g., stigma, treatment availability), personal resources (e.g., insurance, problem-solving skills), and intrapersonal processes (e.g., depression, hope) [2]. Given the many factors involved in accessing and adhering to pre-exposure prophylaxis (PrEP)—a highly efficacious HIV prevention tool—the Health Care Empowerment Model is apt for explaining patient engagement and adherence in PrEP care.
In spite of its efficacy and a decade after being FDA-approved for HIV prevention, PrEP is not reaching the populations that need it most [3]. Individuals residing in the Southern United States (US) face a number of barriers to accessing and adhering to PrEP including rurality, lack of health insurance coverage, low health literacy, intersectional stigma, lack of primary care providers, and lack of knowledge around who can benefit from PrEP [4]. Given these barriers individuals interested in using PrEP for HIV prevention in the South need resources intra-personally, interpersonally, and contextually yielding healthcare empowerment.
Here we present findings on an adapted scale for “PrEP Empowerment.” Items were adapted from the Health Care Empowerment Scale [2] and from qualitative and cognitive interviews with current and potential PrEP users in Birmingham, Alabama USA. The adapted measure was then tested with 100 current PrEP users attending clinic visits to assess its preliminary reliability and validity. We aimed to develop a measure that can be used in future research on PrEP empowerment to validate its use in identifying individuals likely to be engaged in PrEP care, to identify changes in PrEP empowerment via interventions to enhance engagement in PrEP care, and to identify champions of PrEP who can help empower others who may benefit from PrEP.
Method
Measure Development Procedures
The empowerment measure was developed in two phases. First, 44 individual qualitative in-depth interviews were conducted with current and potential PrEP users to elicit their perspectives and attitudes about PrEP in their communities, those qualitative findings were previously published [5]. During thematic analysis of those interviews, empowerment arose as a theme related to PrEP uptake. The research team met to develop measures relevant to understanding PrEP adherence and adapted interview content related to empowerment with existing validated items of health care empowerment [2] for PrEP. The item inventory was then tested in cognitive interviews with 17 current PrEP users.
Participants, Recruitment, and Scale Testing Procedures
In the current study, participants were current PrEP users recruited from the only two community-based clinics in Birmingham, Alabama providing PrEP services. One clinic is an HIV primary clinic that provides a PrEP clinic one day per week. The other clinic is an LGBTQ + primary care facility. Recruitment occurred between May and November 2018. Eligibility criteria were adults who were able to complete a survey in English, who were willing and able to provide informed consent, and who were returning for a PrEP clinic visit (i.e., they were already established on PrEP for HIV prevention). Potential participants were approached by research staff during their regular PrEP clinic visit and asked if they would like to participant in a research survey on attitudes about PrEP. Study procedures were explained verbally and in writing and participants provided informed consent prior to taking part in any procedures. Surveys were administered via Qualtrics [6] on a laptop or tablet in a private clinic room. Participants were reimbursed $30 for their time. Participants could elect to give an additional blood sample to measure plasma tenofovir (TFV) levels while completing their lab work and receive an additional $10. The study protocol was approved by the authors’ Institutional Review Board in accordance with the Declaration of Helsinki.
Measures
Demographic and PrEP information.
Participants reported their age, gender, race, sexual orientation, and form of health insurance. They reported the time they had been taking PrEP in months.
PrEP Empowerment.
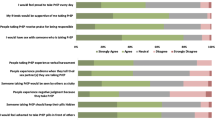
Participants responded to the 19 PrEP empowerment items adapted for the present study using a five-point Likert scale. Item wording is shown in Table 1.
Internalized PrEP Stigma.
An adapted 8-item internalized PrEP stigma scale was developed for this study, items reported elsewhere.[7] Participants responded to each item (e.g., “Being on PrEP makes me think I am a slut.”) using a 4-point Likert scale. Internal consistency of the scale was very good (α = 0.94).
PrEP Adherence Self-efficacy.
Participants responded to 11 items about PrEP adherence self-efficacy adapted for this study from the HIV adherence self-efficacy scale [8, 9]. Participants were given the stem, “How confident do you feel you can do these things related to PrEP?” and responded to scenarios such as, “integrate PrEP into your daily routine,” and “take PrEP daily as prescribed.” They responded on a scale from 0 = cannot do at all, to 10 = completely certain can do. Internal consistency was good (α = 0.79).
Blood plasma TFV level.
Participants who volunteered for the optional blood draw had 1mL of blood drawn during their regular clinic lab work during their visit when other study measures were completed. Specimens were centrifuged immediately, and the plasma was transferred to a polypropylene vial with screw top cap and labeled with the participant ID number, date and time of the blood draw. Plasma samples were frozen at -20 °C until transferred to a lab for plasma TFV measurement. Continuous TFV levels were measured where quantifiable. For this analysis, TFV concentrations were dichotomized as below the limit of quantification (< 10ng/mL) or quantifiable suggestive of recent dosing (> 10ng/mL).
Data Analysis
Prior to analysis all data were cleaned and checked for data entry and computational errors. Data were managed using SPSS software [10] version 27. Exploratory factor analysis was done using principal axis factoring with varimax rotation. Linear and logistic regression were used to assess the associations between the composite mean score of each factor with (1) continuous internalized PrEP stigma, (2) continuous PrEP adherence self-efficacy, and (3) dichotomous plasma TFV detectability. Age (continuous), gender (0 = man, 1 = woman, transgender, or other), race (0 = white, 1 = Black, Hispanic/Latinx, Asian, and multi-race), and health insurance (0 = any, 1 = none) were included as covariates in all regression analyses. Unstandardized beta coefficients and 95% confidence intervals (CI) are reported for linear regression models to promote interpretation based on the measures used, adjusted odds ratios are reported for logistic regressions.
Results
Participants (N = 100) were 36 years old on average (SD:11, range: 20–65), 91 were male, with the other 9 being cisgender women, transgender women, or other gender identity. Most (66) were white, 23 were Black, 6 Hispanic or Latinx, 1 Asian, and 4 multi-race. The majority were gay, lesbian or queer (81); 11 were bisexual or pansexual, and 6 were heterosexual. Most (86) had postsecondary education, and 94 had health insurance. Mean time taking PrEP was 16 months (SD: 13, range: 1–50 months). Internalized PrEP stigma was low on average (M = 1.20, SD: 0.42). PrEP adherence self-efficacy was high on average (M = 9.46, SD: 0.66). Of the 84 participants who provided blood samples, 68 (81%) had quantifiable levels of TFV in their plasma.
Factor Structure and Internal Consistency
Correlations between items were checked for suitability for factor analysis and all items were correlated > 0.30 with one or more other items [11]. Bartlett’s test of sphericity was significant (p < 0.001), and Kaiser-Myer-Olkin (KMO) was 0.82, suggesting suitable factorability. Principal axis factoring with evaluation of eigenvalues above 1.00 and scree plot revealed five factors explaining 70% of the total variance. Factors were named based on common themes within items. Factor 1, “PrEP self-empowerment” explained 35% of the variance; Factor 2 “Commitment to HIV prevention” explained an additional 14%; Factor 3 “PrEP healthcare empowerment” an additional 8%; Factor 4 “PrEP advocacy” an additional 7%, and Factor 5 “PrEP education” an additional 6%. All items had primary loadings of above 0.4 with their factor. A few items loaded across more than one factor and were assigned to the factor with the greater loading value. Items within each factor are described in Table 1.
The four items within “PrEP self-empowerment” had good internal consistency (Cronbach’s α = 0.89), as did the six items in “Commitment to HIV prevention” (Cronbach’s α = 0.85), as did the three items in “PrEP healthcare empowerment” (Cronbach’s α = 0.76), and the three items in “PrEP Advocacy” (Cronbach’s α = 0.72). The internal consistency for the “PrEP education” three-item factor was questionable (Cronbach’s α = 0.60) but adequate for evaluation of validity.
Associations with Internalized PrEP Stigma, PrEP Adherence Self-Efficacy, and Plasma TFV
In linear regression using the outcome of internalized PrEP stigma, “PrEP self-empowerment” (B= -0.24; 95% CI = -0.35, -0.14; p < 0.01), “Commitment to HIV prevention” (B=-0.38; 95% CI = -0.56, -0.20; p < 0.01), and “PrEP advocacy” (B=-0.22; 95% CI = -0.30, -0.14; p = 0.33) were all negatively associated. “PrEP healthcare empowerment” (B=-0.06; 95% CI = -0.15, 0.04; p-0.25), and “PrEP Education” (B = 0.003; 95% CI = -0.13, 0.13; p = 0.96) were not significantly associated with internalized PrEP stigma.
In linear regression analyses, “PrEP self-empowerment” (B = 0.21; 95% CI = 0.03, 0.39; p = 0.02), “Commitment to HIV prevention” (B = 0.35; 95% CI = 0.06, 0.64; p = 0.02), ”PrEP healthcare empowerment” (B = 0.23; 95% CI = 0.09, 0.37; p < 0.01), and PrEP advocacy” (B = 0.22; 95% CI = 0.09, 0.35; p < 0.01) were all positively associated with PrEP adherence self-efficacy. “PrEP education” (B = 0.03; 95% CI = -0.17, 0.23; p = 0.75) was not significantly associated with PrEP adherence self-efficacy.
In logistic regression analyses among the subset of participants (n = 84) that provided plasma samples, “PrEP self-empowerment” (aOR = 0.65; 95% CI = 0.25, 1.66; p = 0.37), “Commitment to HIV prevention” (aOR = 1.95; 95% CI = 0.49, 7.75; p = 0.35), “PrEP healthcare empowerment” (aOR = 1.83; 95% CI = 0.94, 3.57; p = 0.07), and “PrEP advocacy” (aOR = 1.49; 95% CI = 0.81, 2.76; p = 0.20) were not significantly associated with quantifiable TFV in plasma. “PrEP Education” was related to quantifiable TFV (aOR = 2.71; 95% CI = 1.08, 6.75; p = 0.03).
Discussion
The present study evaluated the development, preliminary reliability and validity of a measure of PrEP empowerment analogous to the concept of Health Care Empowerment [1]. Questions were derived from the existing HIV Health Care Empowerment Scale [2] and narratives from current and potential PrEP users. The measure was then tested in individual cognitive interviews before administering to current PrEP users attending the only two community PrEP clinics in Birmingham, Alabama. Results show the measure is reliable and yields a multi-factor structure. We categorized the factors as follows: (1) PrEP self-empowerment, (2) Commitment to HIV prevention, (3) PrEP healthcare empowerment; (4) PrEP Advocacy; and (5) PrEP education. Relationships between each of the five factors with internalized PrEP stigma, PrEP adherence self-efficacy, and recent PrEP adherence via blood plasma TFV level were evaluated.
In preliminary cross-sectional analyses, “PrEP self-empowerment,” “Commitment to HIV prevention” and “PrEP advocacy” were all inversely related to internalized PrEP stigma. It’s possible individuals feeling more empowered when initiating PrEP are more resistant to internalized stigma, or the process of PrEP empowerment leads to a lowering of stigma. Interventions aiming to empower individuals pursuing PrEP care could further evaluate this process. In terms of PrEP adherence self-efficacy, every empowerment factor except for “PrEP education” was positively associated with confidence in one’s ability to adhere with their PrEP plan. This aligns with prior research finding health care empowerment related to treatment self-efficacy in HIV population studies [2]. “PrEP healthcare empowerment” was marginally related and “PrEP education” was significantly related to greater likelihood of quantifiable TFV in plasma samples. Navigating healthcare systems and insurance can be challenging with accessing PrEP, particularly in the US South [3,4,5]. Individuals who feel more empowered to overcome these barriers in their PrEP care and to educate others may be the most likely to adhere to PrEP.
The PrEP Empowerment Scale has several potential uses in research and clinical practice. First building on theory of healthcare empowerment, PrEP empowerment is a multi-dimensional construct that may relate to outcomes including self-efficacy and adherence. Additional research needs to be conducted to assess the scale and its components with pertinent HIV prevention outcomes including adherence and healthcare engagement. Qualitative and longitudinal research could be used to evaluate the process of developing PrEP empowerment over time and experience with PrEP. The PrEP Empowerment measure could be used to help identify individuals who are committed to PrEP for HIV prevention and therefore likely to adhere. It may also help identify gaps were individuals interested in PrEP could use additional resources to become more engaged and empowered in their HIV prevention regimen such as resources for navigating insurance and cost barriers, providing information, or strengthening intrapersonal resources. The scale might also be used to identify individuals who may serve as peer advocates in community implementation of PrEP.
Results of this study should be interpreted in light of some limitations. Analyses examined cross-sectional associations between PrEP empowerment and potential outcomes on a theoretical basis to establish validity and should not be interpreted as causal. Future prospective and longitudinal work may use or adapt this scale to examine future adherence and engagement to support these results. This sample included 100 participants established on PrEP and does not represent all individuals who could benefit from PrEP. Participants were current PrEP users engaged in care and were predominantly white and male. Sample size limited power in these analyses. Additional research is needed to validate this scale in other populations including racial and ethnic minorities, women, transgender individuals, and people who inject drugs who could benefit from PrEP and who may not have yet accessed PrEP care. We did not assess other HIV prevention approaches participants were using other than PrEP, such as condom use and asking about sexual partner serostatus and/or viral suppression. Future research should assess other prevention strategies to determine how sole reliance on PrEP versus multiple HIV prevention strategies impacts empowerment and adherence. Finally, we used plasma TFV levels as an objective measure of recent PrEP adherence. However, plasma TFV is subject to “white coat adherence”—dosing in anticipation of a medical visit—and limits inference about long-term adherence due to its short half-life of 17 h [12]. Future studies may consider this measure in addition to cumulative measures of PrEP adherence such as blood spots or hair samples.
Conclusions
Results from this preliminary study of a PrEP empowerment scale suggest a multidimensional measure that should be tested in future research to determine its validity and applicability to populations not established on PrEP. Certain factors related to lower internalized PrEP stigma, higher PrEP adherence self-efficacy, and higher likelihood of recent PrEP adherence. This PrEP Empowerment scale was developed with the input of community members engaged in PrEP care and could measure a potentially important set of variables that can contribute to our theoretical understanding of empowerment in HIV prevention attitudes and behaviors. The measure may also be used for identifying individuals who will advocate for themselves and their communities for HIV prevention.
References
Johnson MO. The shifting Landscape of Health Care: toward a model of Health Care empowerment. Am J Public Health. 2011;101:265–70. https://doi.org/10.2105/AJPH.2009.189829.
Johnson MO, Rose CD, Dilworth SE, Neilands TB. Advances in the conceptualization and measurement of Health Care empowerment: development and validation of the Health care empowerment inventory. PLoS ONE. 2012;7(9):e45692. https://doi.org/10.1371/journal.pone.0045692.
Zhang C, McMahon J, Fiscella K, Przybyla S, Braksmajer A, LeBlanc N, et al. HIV Pre-Exposure Prophylaxis implementation Cascade among Health Care Professionals in the United States: implications from a systematic review and Meta-analysis. AIDS Patient Care STDs. 2019;33:507–27. https://doi.org/10.1089/apc.2019.0119.
Sullivan PS, Mena L, Elopre L, Siegler AJ. Implementation strategies to increase PrEP uptake in the South. Curr HIV/AIDS Rep. 2019;16:259–69. https://doi.org/10.1007/s11904-019-00447-4.
Rice WS, Stringer KL, Sohail M, Crockett KB, Atkins GC, Kudroff K, et al. Accessing pre-exposure Prophylaxis (PrEP): perceptions of current and potential PrEP users in Birmingham, Alabama. AIDS Behav. 2019;23:2966–79. https://doi.org/10.1007/s10461-019-02591-9.
Qualtrics [Internet], Provo UT. USA: Qualtrics; 2005. Available from: https://www.qualtrics.com.
Van Gerwen OT, Yigit I, Crockett KB, Turan B. The Relationship between HIV Pre-exposure Prophylaxis Stigma and Treatment Adherence among current HIV pre-exposure Prophylaxis users in the Southeastern U.S. AIDS Behav. 2023;27:1478–85. https://doi.org/10.1007/s10461-022-03883-3.
Johnson MO, Neilands TB, Dilworth S, Morin SF, Remien RH, Chesney MA. The role of self-efficacy in HIV Treatment Adherence: validation of the HIV Treatment Adherence Self-Efficacy Scale (HIV-ASES). J Behav Med. 2007;30:359–70. https://doi.org/10.1007/s10865-007-9118-3.
Golub SA, Fikslin RA, Goldberg MH, Peña SM, Radix A. Predictors of PrEP Uptake among patients with Equivalent Access. AIDS Behav. 2019;23:1917–24. https://doi.org/10.1007/s10461-018-2376-y.
IBM Corp. IBM SPSS Statistics for Windows. Armonk, NY: IBM Corp; 2017.
Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4th ed. Needham Heights, MA: Allyn & Bacon; 2001.
Brooks KM, Anderson PL. Pharmacologic-based methods of adherence assessment in HIV prevention. Clin Pharmacol Ther. 2018;104:1056–9. https://doi.org/10.1002/cpt.1201.
Funding
This research was supported by the University of Alabama at Birmingham Center for AIDS Research, a National Institutes of Health (NIH) funded program (P30 AI027767) that was made possible by the following institutes: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIDDK, NIGMS, and OAR. KBC receives research funding from the National Heart Lung and Blood Institute under award number K23 HL156758-01A1. The contents of this publication are the sole responsibility of the authors and do not represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
This study was conducted in accordance with the ethical standards of the authors’ Institutional Review Board and with the 1964 Helsinki declaration and its later amendments.
Informed Consent
Description of all study procedures was provided verbally and in writing and informed consent was obtained from all participants prior to their participation.
Conflict of Interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Crockett, K.B., Batey, D.S. & Turan, B. Development and Preliminary Validation of the PrEP Empowerment Scale. AIDS Behav 27, 3645–3650 (2023). https://doi.org/10.1007/s10461-023-04078-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-023-04078-0