Abstract
Young men who have sex with men (YMSM) under 25 years old are among the few populations with increasing numbers of new HIV infections in parts of the world where HIV incidence is declining overall. In this systematic review, we synthesize the literature on HIV prevalence among MSM in Latin America and the Caribbean focusing on YMSM. Results were stratified according to study population sampling method used (probability and non-probability based). Forty-seven studies from 17 countries were published in the last 10 years. Among studies using probability-based sampling method (N = 21), HIV prevalence among MSM ranged from 1.2 to 32.6%. HIV prevalence tended to increase over time in studies sampling at different time points. HIV prevalence among YMSM exceeded 5.0% in more than a half of studies (51%; N = 22/43). Our review corroborates the high and potentially rising incidence of HIV among YMSM and characterizes the region’s greatest challenge to ending the epidemic.
Resumen
Los hombres jóvenes que tienen sexo con hombres (JHSH) menores de 25 años se encuentran entre las pocas poblaciones con un aumento en las nuevas infecciones por VIH en regiones del mundo donde la incidencia del VIH está disminuyendo en general. En esta revisión sistemática, resumimos la literatura sobre la prevalencia del VIH entre HSH en América Latina y el Caribe, con un enfoque en JHSH. Los resultados se estratificaron por método de muestreo de la población de estudio (probabilístico y no probabilístico). Nuestra investigación encontró 47 estudios de 17 países publicados en los últimos 10 años. Entre los estudios que utilizaron muestreo probabilístico (N = 21), la prevalencia del VIH entre HSH osciló entre 1.2% y 32.6%. La prevalencia del VIH aumentó con el tiempo en ciudades que repitieron el método de muestreo. La prevalencia del VIH entre JHSH superó el 5.0% en más de la mitad de los estudios (51%; N = 22/43). Nuestro análisis corrobora la alta y potencialmente creciente incidencia de VIH entre JHSH y caracteriza el mayor desafío de la región para poner fin a la epidemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Latin America and the Caribbean (LAC), an estimated 2.5 million people were living with HIV by 2019, and more than 133,000 new infections were detected, of whom 22,500 were aged 15 to 24 years [1]. The HIV epidemic in LAC is concentrated in key populations. While the HIV prevalence in the adult general population is 0.4% in Latin America and 1.1% in the Caribbean, rates among men who have sex with men (MSM) have been estimated as 12.6% in Latin America and 4.5% in the Caribbean from 2015–2019 [2]. HIV infection among MSM in the region has been associated with behavior (e.g., condomless anal sex, sex with multiple partners) and structural factors (e.g. economic instability, low socioeconomic status) [3,4,5,6,7,8].
Despite the emergence of new HIV prevention technologies and strategies such as treatment as prevention (TasP, endorsed by World Health Organization [WHO] in 2014), pre-exposure prophylaxis (PrEP, recommended by WHO since 2015), and HIV self-testing (recommended by WHO since 2017) [9], the number of new infections has decreased only slightly over the last decade and is on the rise among young key populations [2]. The overall number of people on PrEP across the region remains insufficient to have a significant impact on the epidemic. PrEP through the public health system is currently only available in Bahamas, Barbados, Brazil, and Cuba, and through private clinics, the Internet, nongovernmental organizations, and pilot studies in Chile, Colombia, Costa Rica, Dominican Republic, Ecuador, Guatemala, Haiti, Jamaica, Mexico, Panama, Paraguay, Peru, Suriname and Uruguay [2, 10]. It is estimated that 23% of people living with HIV in LAC still do not know their status by 2019. In Brazil, among 16,667 MSM responding web-based surveys between 2016 and 2018, 17% reported have never been tested for HIV in their lifetime, with higher percentages in low-income cities [11]. In addition, the “undetectable equals untransmittable” (U = U) slogan is still not correctly understood by different populations including MSM [12], jeopardizing prevention benefits of TasP.
Data from the United States and Asian countries find that young MSM (YMSM) aged 15–24 are at higher risk of HIV infection compared to young heterosexual men and to older MSM [2, 13,14,15]. Lack of access to appropriate sexual education and preventive strategies, condomless and PrEP-less sex, use of alcohol and drugs during sex, transactional sex, and low perceived HIV risk are some of the factors associated with higher vulnerability to HIV among YMSM [11, 16,17,18,19]. Structural barriers in LAC may affect PrEP implementation and continuation among YMSM. Results from ImPrEP study (a large multicountry demonstration PrEP study currently ongoing in Brazil, Mexico and Peru) have shown that early continuation (attending 2 following-up visits) among 1,843 YMSM was 67%, being lower among those at higher social vulnerability, such as nonwhite and less educated [20]. A large web-based survey also identified an association between socioeconomic disparities and HIV prevalence among Latin-American MSM [21]. Homophobia, stigma, and fear of disclosing sexual orientation are other barriers YMSM face in accessing prevention and care services, as well as participation in research [22,23,24].
Gathering rigorous data on YMSM is increasingly needed to guide TasP, PrEP, and other effective interventions if we are to end the HIV epidemic in LAC by 2030 [25]. An important data challenge identified in LAC to date has been utilization of methods that produce representative samples of hidden and hard-to-reach populations in research on key populations like YMSM. In fact, data from non-probability-based samples constitute a large body of the literature on MSM. Probabilistic methods for sampling YMSM do exist. Respondent-driven sampling (RDS) is an approach that approximates probabilistic sampling and has been endorsed by the WHO, the Joint United Nations Program on HIV/AIDS (UNAIDS), Global Fund, and the Centers for Disease Control and Prevention (CDC). Time-location sampling (TLS) and true population-based surveys are sometimes conducted with MSM, though more costly and much less frequently. In this systematic review, we sought to synthesize the literature on HIV prevalence of MSM in LAC using data from probabilistic and non-probabilistic studies. We aimed to assess HIV prevalence in MSM over the years, particularly in YMSM, outcomes associated with the HIV care cascade, and factors associated with HIV infection in the YMSM population in LAC.
Methods
Protocol and Registration
This study was registered with the international database of systematic reviews in health and social care (PROSPERO). This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement [26].
Search of studies.
We performed a bibliographic search on MEDLINE, EMBASE, and Virtual Health Library (VHL, Pan American Health Organization/BIREME) restricted for publications between January 2010 and May 2020. Included publications had to be published from 2010 onwards but data collection could have been initiated prior. There was no language restriction. The VHL search was performed in English, Portuguese, Spanish, and French. The search strategy combined terms derived from four domains: (a) MSM; (b) HIV/AIDS; (c) HIV prevalence; and (d) the countries of LAC (see Supplementary file 1 for the full PubMed search strategy).
Eligibility Criteria
The literature search aimed to include studies reporting HIV prevalence in MSM living in LAC. Peer-reviewed publications and conference abstracts were included if they met all the following criteria: (i) published after 2010; (ii) conducted in LAC; and (iii) reported HIV prevalence. We excluded studies that (i) did not report the HIV prevalence specifically for MSM (studies that reported combined prevalence for MSM and trans women were included, however); (ii) repeated estimates reported in another study already included; (iii) did not provide original data (e.g., reviews). The systematic review did not include other sources of grey literature such as theses, dissertations, monographies, or reports. Two investigators (LEC, TST) reviewed all abstracts and full text publications independently to verify if they met the eligibility criteria.
Data Extraction
Two investigators (LEC, TST) independently extracted data from the selected publications using a predefined form and discussed disagreements to resolve discrepancies. Data extracted included: (i) recruitment setting (sites, cities, countries); (ii) year of data collection; (iii) study sample characteristics (sample size, proportion of MSM and trans women, age); (iv) HIV prevalence and 95% confidence intervals (95% CI) in MSM of all ages and among YMSM; (v) factors associated with HIV prevalence; and (vi) HIV care cascade outcomes (previous HIV testing, awareness of HIV status, antiretroviral therapy [ART] use, viral suppression). Results were stratified into probability and non-probability sampling methods. Investigators attempted to reach all publication corresponding authors to request YMSM prevalence estimates that were not included in the publications.
Results
Search Results
Our search found 47 unique studies, described in 49 publications, and conducted in 17 countries from 2006 to 2020 (Suppl Fig. S1), although no eligible studies were published from 2017 to 2020. Studies’ sample sizes varied from 41 to 7,823 participants. Most studies included only participants age 18 years and above; six studies included participants under 18 years. Nineteen studies included both MSM and trans women.
HIV Prevalence
Results of studies that used probabilistic sampling methods (N = 21), including RDS, TLS, stratified sampling of military conscripts, and stratified household sampling are shown in Table 1. Five of these 21 studies (23.8%) were conducted in Brazil. A total of 21,817 MSM were included in the 21 studies, with 11,118 (51.0%) from Brazil. Among those studies, HIV prevalence among all-age MSM ranged from 1.2% (95% CI 0.3, 3.6) in Santos, Brazil conducted in 2009 [27] to 32.6% (95% CI 18.0, 47.8) in Colón, Panama in 2012 [28]. Among cities that repeated studies at different time points, HIV prevalence tended to have increased over time in Belo Horizonte, Campo Grande, Curitiba, Manaus, Recife, and Salvador in Brazil and Quito, Ecuador [5, 27, 29, 30]. HIV prevalence tended to have decreased over time in Brasilia and Rio de Janeiro in Brazil and Bogota, Colombia [27, 30,31,32]. Nationally in Brazil, HIV prevalence was 1.23% among MSM who were conscripts in 2007 compared to 1.32% in 2016 [33, 34]. Overall, the proportion of YMSM (aged 18–24) included in these studies are shown in fifteen studies and ranged from 0.5% in Salvador, Brazil in 2009 to 78.4% in Brasilia, Brazil in 2016 [27, 30].
Results of studies that used non-probabilistic methods of recruitment (e.g., targeted outreach, peer referral, clinic clients, or non-governmental and community-based organization clients) are shown in Table 2 (N = 26 studies). At total of 32,403 individuals were included in those studies with 12,857 (39.7%) from Peru. HIV prevalence among MSM ranged from 2.2% (95% CI 0.9, 5.3) in Haiti in 2016 [7] to 32.3% (95% CI 25.2, 47.9) in Jamaica in 2008 [8]. The proportion of YMSM included in these studies (N = 7) ranged from 61.7% in Jamaica in 2011 to 75.0% in Haiti in 2016 [7, 35].
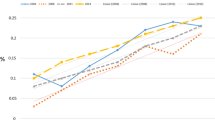
Nineteen studies (15 that used probability-based sampling methods and 4 non-probability-based sampling) reported HIV prevalence estimates among YMSM (aged < 25) (Fig. 1). HIV prevalence was greater than 5.0% in more than a half (51%; 22/43) of the estimates. The highest HIV prevalence among YMSM was found in RDS surveys conducted in Panama City in 2012 (17.3%, 95% CI 9.6, 27.3) and in Colón, Panama in 2012 (15.6%, 95% CI 4.9, 32.4%) [28]. Among studies using non-probabilistic recruitment methods reporting HIV prevalence among YMSM, the highest estimates were in Jamaica using targeted outreach in 2008 (28.3%) [8] and peer referral in 2011 (24.1%) [35].
HIV Care Cascade
HIV testing history and awareness of HIV status among all-age MSM are shown in Table 3. The proportion of MSM who had previously tested ranged from 26.8% among patients at three STI clinics in Escuintla province, Guatemala in 2007 [36] to 85.1% (95% CI 74.9, 91.6) in a national survey in Haiti nine years later in 2016 [7]. Few studies provided the proportion of awareness of HIV-positive status. In an RDS survey in San Salvador, El Salvador in 2008 [37], only 11.0% of HIV-positive participants were aware of their status, contrasting with 64.0% in Santiago, Chile in 2016 [38]. Only one study, a national survey in Haiti in 2016, reported the proportion of HIV-positive individuals on ART (86%, 5 out of 6) and those on ART with an undetectable viral load (80%, 4 out of 5) [7].
Specifically for YMSM, one study conducted from 2007 to 2009 in Buenos Aires, Argentina reported prior HIV testing in 30.5% of YMSM, and 33.3% who tested HIV-positive were aware of their HIV status (2 out of 6) [39]. In Brazil, a pooled analysis of RDS surveys in 10 cities in 2009 identified that 28.0% of MSM aged less than 20 years had a prior HIV test. In addition, never testing for HIV was independently associated with younger age [40].
Factors Associated with HIV Infection
Several studies characterized factors associated with HIV infection among MSM of all ages (Table 4), but none reported associations specifically among YMSM. In addition to various indicators of sexual risk behavior, older age, lower socio-economic status, trans women gender identity, drug use, and prior violence experiences were associated with higher HIV prevalence among MSM.
Discussion
In this systematic review, we documented the high and potentially rising HIV prevalence among YMSM living in LAC. Estimates greater than 10% were observed in all sub-regions, from Meso and Central America, the Caribbean, the Andes, and the South American Cone [28, 30, 35, 41, 42]. The high HIV prevalence was consistent across survey methods. Although several RDS studies have evaluated HIV prevalence among MSM in the region over the past 10 years, none of them specifically targeted YMSM. Unfortunately, many reports of epidemiologic data on key populations do not disaggregate by age, as in most of the studies included in this review. Moreover, it is hard to estimate the population size of YMSM, and this group may be underrepresented in studies due to disparities between young and older MSM with respect to such factors as internalized and external homophobia, economic insecurity, and lack of social and parental support [43].
Globally, YMSM are disproportionately affected by HIV and are one of the few populations with worrisome increases in the numbers of new cases, despite stabilizing rates in other groups. HIV surveillance data from Bangkok, Thailand, has shown an increasing prevalence among MSM aged 22 years and under, from 13% in 2003 to 24% in 2014 [44]. In Nigeria, HIV incidence was four- and three- fold higher in MSM aged 16 to 19 years and 20 to 24 years, respectively, compared to MSM aged 25 years or older [45]. Data estimated a 2.5-fold higher HIV incidence in YMSM when compared to older MSM in the city of Atlanta, Georgia, United States [46], and even higher incidence among young Black MSM [47]. In Brazil, researchers detected an increase in HIV prevalence among MSM from 2009 to 2016 and hypothesized that this was due to a higher proportion of younger participants enrolled in the later surveys [48]. Also, a web-based survey conducted in 2018 among 7,055 YMSM found a high self-reported HIV prevalence, reaching 15.3%, 8.4% and 7.7% in Peru, Mexico, and Brazil, respectively [21].
YMSM may be more vulnerable to HIV infection than older MSM in LAC [2, 13,14,15]. Riskier sexual practices, low HIV risk perception, and adverse social economic disparities may be drivers of risk for this young population. In Brazil, pooled data from RDS surveys conducted in 12 cities in 2016 found that YMSM were more likely to have condomless receptive anal sex than older MSM (41.9% and 29.7%, respectively, p < 0.001) [49]. Among YMSM included in this analysis, condomless receptive anal sex was associated with poor self-rated health status, high risk perception, gay/homosexual sexual identity, and transactional sex. In addition, a temporal trend of increased risk behavior was observed among Brazilian YMSM from 2009 to 2016, including higher numbers of sexual partners, more frequent condomless insertive and receptive anal sex, and more frequent use of illicit drug [48]. Additionally, a Brazilian national web-based survey conducted in 2017 showed that YMSM were more likely to experience condomless receptive anal sex and transactional sex, but had lower perceived HIV risk, lower HIV testing, and lower PrEP awareness compared to older MSM [50]. Still in Brazil, younger age (18 to 24 years) increased the odds of high-risk behavior among 16,667 MSM who responded to web-based surveys from 2016 to 2018 [11]. Similar findings were observed in a Nigerian study, which observed an association between decreasing age and increased likelihood of condomless anal sex, no prior testing for HIV, and having rectal gonorrhea [45].
None of the studies included in this review evaluated factors associated with HIV prevalence specifically among YMSM, including socioeconomic disparities. Countries in LAC have among the highest wealth inequalities in the world [51], and social determinants are related to adverse health outcomes [52]. For example, low-income was associated with self-reported HIV prevalence among Brazilian and Peruvian YMSM [21]. Among PrEP users in a demonstration project in Brazil, Black YMSM with low income were less likely to have optimal ART adherence [53]. Also in Brazil, racial minorities status and lower education, which are often associated with poverty, were related to worse outcomes along the HIV care continuum, including HIV status awareness, being on ART, and virologic suppression [54]. Taken together, findings corroborate that social determinants most likely contribute to the increased HIV risk among YMSM. Echoing our findings, a systematic review in the United States identified that YMSM were more likely to experience depression, polysubstance use, low income, decreased health care access, and earlier sexual debut than older MSM. The authors also observed that YMSM living with HIV were less likely to be aware of their infection, on ART, or virologically suppressed [43].
Although several studies have found a positive association between older age and HIV infection among MSM in LAC [4, 5, 29, 31, 37]. This finding is expected as prevalence includes cumulative cases over longer periods of time for older persons. HIV prevalence among young persons may be a proxy for HIV incidence, considering that lifetime sexual exposure is shorter and risks leading to acquiring infection are more recent among YMSM. In support of this hypothesis, the study in El Salvador found a three-fold higher proportion of recent infection by the BED-CEIA assay among YMSM compared to older MSM (34.8% versus 9.6%, p < 0.01) [37].
This systematic review has several limitations. First, our original goal was to assess HIV prevalence among YMSM living in LAC and its trend over the last 10 years. The rationale used to select the systematic review study period was to capture data that could describe the state of HIV epidemic pre- and post- major HIV public health policies such as TasP and PrEP and how they impacted the HIV epidemic. Unfortunately, no studies were conducted solely with YMSM. Second, in order to have comparable research findings with probability-based methods, we initially limited our review to studies using RDS. We widened our search to other sampling and recruitment methods as none of the RDS studies targeted YMSM specifically. The wider inclusion allowed for other probabilistic methods (such as TLS, stratified sampling among military conscripts, and household surveys) and non-probabilistic methods. Third, the scarcity of data on YMSM did not allow to assess factors associated with HIV infection, nor to evaluate the HIV care continuum specifically among YMSM. Fourth, some of the studies included trans women. Their inclusion may have increased the HIV prevalence as trans women have an estimated global HIV prevalence higher than for MSM [55]. We acknowledge that trans women are a different population, often mistakenly grouped with MSM. Despite limitations, this study provides a compendium of knowledge on HIV prevalence among YMSM in LAC published in four languages during the last decade and sheds light to the gaps in the literature for this highly vulnerable population.
Conclusions
Current data demonstrate that HIV prevalence among YMSM in LAC is high. However, there is a dearth on studies specifically focusing on HIV prevalence and its associated factors specifically among YMSM. Areas requiring further investigation include socioeconomic and racial disparities, sexual behavior and sexual networks, and individual and structural barriers along the HIV care and prevention continuums. Studies aiming to address those gaps will need to specifically prioritize YMSM using rigorous sampling methods. There is an urgent need for larger epidemiological studies focusing on YMSM to support strategies and policies aiming to decrease HIV incidence in this highly vulnerable group.
Change history
26 July 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10461-021-03400-y
References
UNAIDS. AIDSinfo [Internet]. [cited 2020 Dec 15]. Available from: https://aidsinfo.unaids.org/
UNAIDS. 2020 Global AIDS Report [Internet]. 2020 [cited 2020 Dec 15]. Available from: https://www.unaids.org/sites/default/files/media_asset/2020_global-aids-report_en.pdf
Torres RMC, Cruz MMD, Périssé ARS, Pires DRF. High HIV infection prevalence in a group of men who have sex with men. Braz J Infect Dis. 2017;21:596–605.
Johnston LG, Vaillant TC, Dolores Y, Vales HM. HIV, hepatitis B/C and syphilis prevalence and risk behaviors among gay, transsexuals and men who have sex with men. Dominican Republic Int J STD AIDS. 2013;24:313–21.
Jacobson JO, Sánchez-Gómez A, Montoya O, Soria E, Tarupi W, Chiriboga Urquizo M, et al. A continuing HIV epidemic and differential patterns of HIV-STI risk among MSM in Quito, Ecuador: an urgent need to scale up HIV testing and prevention. AIDS Behav. 2014;18:88–98.
Bautista-Arredondo S, Colchero MA, Romero M, Conde-Glez CJ, Sosa-Rubí SG. Is the HIV Epidemic Stable among MSM in Mexico? HIV Prevalence and Risk Behavior Results from a Nationally Representative Survey among Men Who Have Sex with Men. PLoS ONE [Internet]. 2013. https://doi.org/10.1371/journal.pone.0072616.
Zalla L.C., Herce M.E., Edwards J.K., Michel J., Weir S.S. The burden of HIV among female sex workers, men who have sex with men and transgender women in Haiti: results from the 2016 Priorities for Local AIDS Control Efforts (PLACE) study. J Int AIDS Soc [Internet]. 2019;22. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L2004361751
Figueroa JP, Weir SS, Jones-Cooper C, Byfield L, Hobbs MM, McKnight I, et al. High HIV prevalence among men who have sex with men in Jamaica is associated with social vulnerability and other sexually transmitted infections. West Indian Med J. 2013;62:286–91.
WHO. Guidelines on HIV self-testing and partner notification [Internet]. 2016 [cited 2020 Dec 15]. Available from: https://www.who.int/hiv/pub/vct/hiv-self-testing-guidelines/en/
Luz PM, Veloso VG, Grinsztejn B. The HIV epidemic in Latin America: accomplishments and challenges on treatment and prevention. Current Opinion in HIV and AIDS. 2019;14:366–73.
Torres TS, Marins LMS, Veloso VG, Grinsztejn B, Luz PM. How heterogeneous are MSM from Brazilian cities? An analysis of sexual behavior and perceived risk and a description of trends in awareness and willingness to use pre-exposure prophylaxis. BMC Infect Dis. 2019;19:1067.
Torres TS, Cox J, Marins LM, Bezerra DR, Veloso VG, Grinsztejn B, et al. A call to improve understanding of Undetectable equals Untransmittable (U = U) in Brazil a web-based survey. J Intern AIDS Soc [Internet]. 2020. https://doi.org/10.1002/jia2.25630.
Gangamma R, Slesnick N, Toviessi P, Serovich J. Comparison of HIV Risks among Gay, Lesbian, Bisexual and Heterosexual Homeless Youth. J Youth Adolescence. 2008;37:456–64.
van Griensven F, de van Wijngaarden JWL. A review of the epidemiology of HIV infection and prevention responses among MSM in Asia. AIDS. 2010;24:S30-40.
Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in Young Men Who Have Sex with Men: A Review of Epidemiology, Risk and Protective Factors, and Interventions. Journal of Sex Research. 2011;48:218–53.
Salomon EA, Mimiaga MJ, Husnik MJ, Welles SL, Manseau MW, Montenegro AB, et al. Depressive Symptoms, Utilization of Mental Health Care, Substance Use and Sexual Risk Among Young Men Who have Sex with Men in EXPLORE: Implications for Age-Specific Interventions. AIDS Behav. 2009;13:811–21.
Agronick G, O’donnell L, Stueve A, Doval AS, Duran R, Vargo S. Sexual Behaviors and Risks Among Bisexually- and Gay-Identified Young Latino Men. AIDS Behav. 2004;8:185–97.
Torres TS, Konda KA, Vega-Ramirez EH, Elorreaga OA, Diaz-Sosa D, Diaz S, et al. Characteristics of younger MSM and association of age with PrEP awareness and willingness in Brazil, Mexico and Peru. Mexico City, Mexico;
de Gomes RR, das GBCM, Kerr LRFS, Guimarães MDC. . Fatores associados ao baixo conhecimento sobre HIV/AIDS entre homens que fazem sexo com homens no Brasil. Cad Saúde Pública (Online). 2017;33:e00125515–e00125515.
Veloso VG. Abstract Supplement Oral Abstracts from the 23rd International AIDS Conference, 6–10 July 2020. J Intern AIDS Soc. 2020. https://doi.org/10.1002/jia2.25547.
Torres TS, Coelho LE, Konda KA, Vega-Ramirez EH, Elorreaga OA, Diaz-Sosa D, et al. SOCIOECONOMIC DISPARITIES ARE ASSOCIATED WITH HIV IN YOUNG MSM WITHIN LATIN AMERICA. 2020. CROI Conference, Boston 2020. Available from: https://www.croiconference.org/abstract/socioeconomic-disparities-are-associated-with-hiv-in-young-msm-within-latin-america/
Ojikutu BO, Bogart LM, Higgins-Biddle M, Dale SK, Allen W, Dominique T, et al. Facilitators and Barriers to Pre-Exposure Prophylaxis (PrEP) Use Among Black Individuals in the United States: Results from the National Survey on HIV in the Black Community (NSHBC). AIDS Behav. 2018;22:3576–87.
Quinn K, Bowleg L, Dickson-Gomez J. “The fear of being Black plus the fear of being gay”: The effects of intersectional stigma on PrEP use among young Black gay, bisexual, and other men who have sex with men. Soc Sci Med. 2019;232:86–93.
Logie CH, Newman PA, Weaver J, Roungkraphon S, Tepjan S. HIV-Related Stigma and HIV Prevention Uptake Among Young Men Who Have Sex with Men and Transgender Women in Thailand. AIDS Patient Care and STDs. 2016;30:92–100.
UNAIDS. Fast-track commitments to end AIDS by 2030 [Internet]. 2016 [cited 2020 Dec 15]. Available from: https://www.unaids.org/sites/default/files/media_asset/fast-track-commitments_en.pdf
Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9.
Kerr LRFS, Mota RS, Kendall C, de Pinho A, Mello MB, Guimarães MDC, et al. HIV among MSM in a large middle-income country. AIDS. 2013;27:427–35.
Hakre S, Arteaga GB, Nunez AE, Arambu N, Aumakhan B, Liu M, et al. Prevalence of HIV, syphilis, and other sexually transmitted infections among MSM from three cities in Panama. J Urban Health United States. 2014;91:793–808.
Sanchez-Gomez A, Jacobson JO, Montoya O, Magallanes D, Bajana W, Aviles O, et al. HIV, STI and Behavioral Risk Among Men Who have Sex with Men in a Setting of Elevated HIV Prevalence Along Ecuador’s Pacific Coast. AIDS Behav. 2015;19:1609–18.
Kerr L, Kendall C, Guimarães MDC, Salani Mota R, Veras MA, Dourado I, et al. HIV prevalence among men who have sex with men in Brazil: results of the 2nd national survey using respondent-driven sampling. Medicine. 2018;97:S9-15.
Rubio Mendoza ML, Jacobson JO, Morales-Miranda S, Sierra Alarcón CÁ, Luque NR. High HIV Burden in Men Who Have Sex with Men across Colombia’s Largest Cities: Findings from an Integrated Biological and Behavioral Surveillance Study. PLoS ONE. 2015. https://doi.org/10.1371/journal.pone.0131040.
Zea MC, Reisen CA, del Río-González AM, Bianchi FT, Ramirez-Valles J, Poppen PJ. HIV Prevalence and Awareness of Positive Serostatus Among Men Who Have Sex With Men and Transgender Women in Bogotá. Colombia Am J Public Health. 2015;105:1588–95.
Szwarcwald CL, de Andrade CLT, Pascom ARP, Fazito E, Pereira GFM, da Penha IT. HIV-related risky practices among Brazilian young men, 2007. Cad saúde pública. 2011;27:s19-26.
Sperhacke RD, Da Motta LR, Kato SK, Vanni AC, Paganella MP, De Oliveira MCP, et al. HIV prevalence and sexual behavior among young male conscripts in the Brazilian army, 2016. Medicine. 2018;97:S25-31.
Figueroa JP, Cooper CJ, Edwards JK, Byfield L, Eastman S, Hobbs MM, et al. Understanding the high prevalence of HIV and other sexually transmitted infections among socio-economically vulnerable men who have sex with men in jamaica. PLoS ONE [Internet]. 2015. https://doi.org/10.1371/journal.pone.0117686.
Lahuerta M, Sabidó M, Giardina F, Hernández G, Palacios JF, Ortiz R, et al. Comparison of users of an HIV/syphilis screening community-based mobile van and traditional voluntary counselling and testing sites in Guatemala. Sex Transm Infect. 2011;87:136–40.
Creswell J, Guardado ME, Lee J, Nieto AI, Kim AA, Monterroso E, et al. HIV and STI control in El Salvador: results from an integrated behavioural survey among men who have sex with men. Sex Transm Infect. 2012;88:633–8.
Stuardo Ávila V, Fuentes Alburquenque M, Muñoz R, Bustamante Lobos L, Faba A, Belmar Prieto J, et al. Prevalence and Risk Factors for HIV Infection in a Population of Homosexual, Bisexual, and Other Men Who Have Sex with Men in the Metropolitan Region of Chile: A Re-emerging Health Problem. AIDS Behav. 2020;24:827–38.
Balan IC, Frasca T, Pando MA, Marone RO, Barreda V, Dolezal C, et al. High Substance Use and HIV Risk Behavior Among Young Argentine Men Who Have Sex with Men. AIDS Behav United States. 2018;22:1373–82.
Brito AM, Kendall C, Kerr L, Mota RMS, Guimarães MDC, Dourado I, et al. Factors Associated with Low Levels of HIV Testing among Men Who Have Sex with Men (MSM) in Brazil. PLoS ONE. 2015;10:e0130445.
Andrinopoulos K, Kerrigan D, Figueroa JP, Reese R, Gaydos CA, Bennett L, et al. Establishment of an HIV/sexually transmitted disease programme and prevalence of infection among incarcerated men in Jamaica. Int J STD AIDS. 2010;21:114–9.
Pitpitan EV, Smith LR, Goodman-Meza D, Torres K, Semple SJ, Strathdee SA, et al. “Outness” as a Moderator of the Association Between Syndemic Conditions and HIV Risk-Taking Behavior Among Men Who Have Sex with Men in Tijuana. Mexico AIDS Behav. 2016;20:431–8.
Jeffries WL, Greene KM, Paz-Bailey G, McCree DH, Scales L, Dunville R, et al. Determinants of HIV Incidence Disparities Among Young and Older Men Who Have Sex with Men in the United States. AIDS Behav. 2018;22:2199–213.
AIDS TB and STIs Control Division. HIV/AIDS epidemic and status of prevention and alleviation efforts, Bangkok, 2010–2014. Bangkok, Thailand. 2015.
Nowak RG, Mitchell A, Crowell TA, Liu H, Ketende S, Ramadhani HO, et al. Individual and Sexual Network Predictors of HIV Incidence Among Men Who Have Sex With Men in Nigeria. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2019;80:444–53.
Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25:445–54.
Balaji AB, Bowles KE, Le BC, Paz-Bailey G, Oster AM, NHBS Study Group. High HIV incidence and prevalence and associated factors among young MSM 2008. AIDS. 2013;27:269–78.
Guimarães MDC, Kendall C, Magno L, Rocha GM, Knauth DR, Leal AF, et al. Comparing HIV risk-related behaviors between 2 RDS national samples of MSM in Brazil, 2009 and 2016. Medicine (Baltimore). 2018;97:S62–8.
Rocha GM, Guimarães MDC, de Brito AM, Dourado I, Veras MA, Magno L, et al. High Rates of Unprotected Receptive Anal Intercourse and Their Correlates Among Young and Older MSM in Brazil. AIDS Behav. 2019. https://doi.org/10.1007/s10461-019-02459-y.
Torres TS, Luz PM, De Boni RB, de Vasconcellos MTL, Hoagland B, Garner A, et al. Factors associated with PrEP awareness according to age and willingness to use HIV prevention technologies: the 2017 online survey among MSM in Brazil. AIDS Care. 2019;31:1193–202.
UNITED NATIONS ECONOMIC COMMISSION FOR LATIN AMERICA AND THE CARIBBEAN. SOCIAL PANORAMA OF LATIN AMERICA 2019. [Internet]. 2020 [cited 2020 Jun 4]. Available from: https://www.cepal.org/en/publications/44989-social-panorama-latin-america-2019
Bilal U, Alazraqui M, Caiaffa WT, Lopez-Olmedo N, Martinez-Folgar K, Miranda JJ, et al. Inequalities in life expectancy in six large Latin American cities from the SALURBAL study: an ecological analysis. The Lancet Planetary Health. 2019;3:e503–10.
Grinsztejn B, Hoagland B, Moreira RI, Kallas EG, Madruga JV, Goulart S, et al. Retention, engagement, and adherence to pre-exposure prophylaxis for men who have sex with men and transgender women in PrEP Brasil: 48 week results of a demonstration study. Lancet HIV. 2018;5:e136–45.
Pascom ARP, Meireles MV, Benzaken AS. Sociodemographic determinants of attrition in the HIV continuum of care in Brazil, in 2016. Medicine. 2018;97:S69-74.
Baral SD, Grosso A, Holland C, Papworth E. The epidemiology of HIV among men who have sex with men in countries with generalized HIV epidemics. Curr Opin HIV AIDS. 2014;9:156–67.
Pando MA, Balán IC, Marone R, Dolezal C, Leu C-S, Squiquera L, et al. HIV and other sexually transmitted infections among men who have sex with men recruited by RDS in Buenos Aires, Argentina: High HIV and HPV infection. PLoS ONE [Internet]. 2012. https://doi.org/10.1371/journal.pone.0039834.
Soares CC, Georg I, Lampe E, Lewis L, Morgado MG, Nicol AF, et al. HIV-1, HBV, HCV, HTLV, HPV-16/18, and Treponema pallidum infections in a sample of Brazilian men who have sex with men. PLoS ONE. 2014;9:e102676.
de Veras MASM, Calazans GJ, de Ribeiro MCA, de Freitas Oliveira CA, Giovanetti MR, Facchini R, et al. High HIV Prevalence among Men who have Sex with Men in a Time-Location Sampling Survey, São Paulo. Brazil AIDS Behav. 2015;19:1589–98.
Morales-Miranda S, Loya-Montiel I, Ritter J, Rocha-Jiménez T, Gordon L, García J, et al. Factors associated with HIV testing among men who have sex with men in Guatemala City. Int J STD AIDS. 2019;30:577–85.
Kim AA, Morales S, Lorenzana De Rivera I, Paredes M, Juarez S, Alvarez B, et al. Short Communication: HIV incidence among vulnerable populations in Honduras: Results from an integrated behavioral and biological survey among female sex workers, men who have sex with men, and Garifuna in Honduras, 2006. AIDS Res Hum Retroviruses. 2013;29:516–9.
Pitpitan EV, Goodman-Meza D, Burgos JL, Abramovitz D, Chavarin CV, Torres K, et al. Prevalence and correlates of HIV among men who have sex with men in Tijuana, Mexico. Journal of the International AIDS Society. 2015;18:19304.
Hernandez F, Arambú N, Alvarez B, Romero L, GoinsEBeteta J, Paz-Bailey G, et al. High incidence of HIV and low HIV prevention coverage among men who have sex with men in Managua. Nicaragua Sex Transm Infect. 2011;87:A146.
Aguilar G, Samudio T, Kawabata A, Cano C, Estigarribia G, Lopez G, et al. Prevalence of HIV/AIDS and syphilis, knowledge, practices of men who have sex with men in Asunción and Metropolitan Area, Paraguay, 2014. Int J STD AIDS. 2015;26:80.
Clark JL, Konda KA, Silva-Santisteban A, Peinado J, Lama JR, Kusunoki L, et al. Sampling methodologies for epidemiologic surveillance of men who have sex with men and transgender women in Latin America: an empiric comparison of convenience sampling, time space sampling, and respondent driven sampling. AIDS Behav United States. 2014;18:2338–48.
Colón-López V, Ortiz AP, Del Toro-Mejías L, Clatts MC, Palefsky JM. Epidemiology of anal HPV infection in high-risk men attending a sexually transmitted infection clinic in Puerto Rico. PLoS ONE. 2014;9:e83209.
Pando MA, Gómez-Carrillo M, Vignoles M, Rubio AE, Dos Ramos Farias MS, Vila M, et al. Incidence of HIV type 1 infection, antiretroviral drug resistance, and molecular characterization in newly diagnosed individuals in Argentina: A global fund project. AIDS Res Hum Retroviruses. 2011;27:17–23.
Castro CAV de. Diferenciação entre soroconversão recente e de longo termo na infecção pelo HIV-1: implicações nos estudos sobre dinâmica da epidemia, diversidade viral, vigilância da resistência aos antirretrovirais e patogênese. 2011;xxi,168-xxi,168.
Fernandes FRP, Zanini PB, Rezende GR, Castro LS, Bandeira LM, Puga MA, et al. Syphilis infection, sexual practices and bisexual behaviour among men who have sex with men and transgender women: a cross-sectional study. Sex Transm Infect. 2015;91:142–9.
Pascom ARP, de Barros CHD, Lobo TDM, Pasini EN, Comparini RA, de Mesquita FC. Point-of-care HIV tests done by peers. Brazil Bull WHO. 2016;94:626–30.
Hernandez I, Johnson A, Reina-Ortiz M, Rosas C, Sharma V, Teran S, et al. Syphilis and HIV/Syphilis Co-infection Among Men Who Have Sex With Men (MSM) in Ecuador. Am J Mens Health. 2017;11:823–33.
Solomon MM, Nureña CR, Tanur JM, Montoya O, Grant RM, McConnell J. Transactional sex and prevalence of STIs: a cross-sectional study of MSM and transwomen screened for an HIV prevention trial. Int J STD AIDS. 2015;26:879–86.
García JI, Sabidó M, Nikiforov M, Smith A, Hernández G, Ortiz R, et al. The UALE project: a cross-sectional approach for trends in HIV/STI prevalence among key populations attending STI clinics in Guatemala. BMJ Open. 2018;8:e022632.
Morales MS, Galindo AC, Arana F, Loya I. Trends in risk behavior and HIV and syphilis infection among MSM Who Attend in STI Clinics in Guatemala. Sex Transm Infect [Internet]. 2013. https://doi.org/10.1136/sextrans-2013-051184.0883.
Budhwani H, Hearld KR, Barrow G, Peterson SN, Walton-Levermore K. A comparison of younger and older men who have sex with men using data from Jamaica AIDS Support for Life: characteristics associated with HIV status. Int J STD AIDS. 2016;27:769–75.
Perez-Brumer AG, Konda KA, Salvatierra HJ, Segura ER, Hall ER, Montano SM, et al. Prevalence of HIV, STIs, and Risk Behaviors in a Cross-Sectional Community- and Clinic-Based Sample of Men Who Have Sex with Men (MSM) in Lima. Peru PLoS ONE [Internet]. 2013. https://doi.org/10.1371/journal.pone.0059072.
Clark JL, Segura ER, Montano SM, Leon SR, Kochel T, Salvatierra HJ, et al. Routine laboratory screening for acute and recent HIV infection in Lima. Peru Sex Transm Infect. 2010;86:545–7.
Lipsitz MC, Segura ER, Castro JL, Smith E, Medrano C, Clark JL, et al. Bringing testing to the people - benefits of mobile unit HIV/syphilis testing in Lima, Peru, 2007–2009. Int J STD AIDS. 2014;25:325–31.
Smith E, Blas M, Konda K, Silvana S, Cabello R. STIs among MSM in a developing country: Limited access to health services. J Int Assoc Phys AIDS. 2010;9:66.
Bayer AM, Garvich M, Diáz DA, Sánchez H, García PJ, Coates TJ. “Just getting by”: A cross-sectional study of male sex workers as a key population for HIV/STIs among men who have sex with men in Peru. Sex Transm Infect. 2014;90:223–9.
Castillo R, Konda KA, Leon SR, Silva-Santisteban A, Salazar X, Klausner JD, et al. HIV and Sexually Transmitted Infection Incidence and Associated Risk Factors among High-Risk MSM and Male-to-Female Transgender Women in Lima. Peru J Acquired Immune Defic Syndr. 2015;69:567–75.
Verre MC, Peinado J, Segura ER, Clark J, Gonzales P, Benites C, et al. Socialization patterns and their associations with unprotected anal intercourse, HIV, and syphilis among high-risk men who have sex with men and transgender women in Peru. AIDS Behav. 2014;18:2030–9.
McLean SA, Galea JT, Prudden HJ, Calvo G, Sánchez H, Brown B. Association between sexual role and HIV status among Peruvian men who have sex with men seeking an HIV test: a cross-sectional analysis. Int J STD AIDS. 2016;27:783–9.
Passaro RC, Haley CA, Sanchez H, Vermund SH, Kipp AM. High HIV prevalence and the internet as a source of HIV-related service information at a community-based organization in Peru: a cross-sectional study of men who have sex with men. BMC Public Health. 2016;16:871.
Allan-Blitz L-T, Herrera MC, Calvo GM, Vargas SK, Caceres CF, Klausner JD, et al. Venue-Based HIV-Testing: An Effective Screening Strategy for High-Risk Populations in Lima. Peru AIDS Behav. 2019;23:813–9.
Balan IC, Frasca T, Pando MA, Mabragana M, Marone RO, Barreda V, et al. (2016) [Summary of the LINKS Study: Factors associated with HIV infection among men who have sex with men in Buenos Aires, Argentina]. Actual SIDA Infectol. 24 (91)
Carballo-Diéguez A, Balán IC, Dolezal C, Pando MA, Marone R, Barreda V, et al. HIV testing practices among men who have sex with men in Buenos Aires. Argentina AIDS Care. 2014;26:33–41.
Rubio Mendoza ML, Jacobson JO, Morales-Miranda S, Sierra Alarcón CÁ, Luque NR. High HIV Burden in Men Who Have Sex with Men across Colombia’s Largest Cities: Findings from an Integrated Biological and Behavioral Surveillance Study. PLoS ONE. 2015;10:e0131040.
Funding
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Lara E. Coelho and Thiago S. Torres performed the literature search and data analysis. Lara E. Coelho, Thiago S. Torres and Emilia M. Jalil drafted the manuscript. Valdilea G. Veloso, Beatriz Grinsztejn, Erin C Wilson, Willi McFarland critically revised and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical Approval
Not required/applicable.
Informed Consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Coelho, L.E., Torres, T.S., Veloso, V.G. et al. The Prevalence of HIV Among Men Who Have Sex With Men (MSM) and Young MSM in Latin America and the Caribbean: A Systematic Review. AIDS Behav 25, 3223–3237 (2021). https://doi.org/10.1007/s10461-021-03180-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03180-5