Abstract
We explored the association between HIV-related stigma and experiences of intimate partner violence (IPV) and depression with viral load suppression, and medication and visit adherence in postpartum women receiving lifelong antiretroviral therapy (ART) (N = 200). We administered a cross-sectional survey to 200 women with HIV at 12 months postpartum who were enrolled in the MOTIVATE trial. The MOTIVATE study is a cluster-randomized trial evaluating the impact of community mentor mothers and text messaging on PMTCT outcomes in southwestern Kenya. Simple and multivariable logistic regression analysis was performed in STATA. Women who experienced stigma or IPV were more likely to miss clinic visits (internalized stigma aOR 1.30 95%CI 1.03–1.64; anticipated stigma aOR 1.20 95%CI 1.04–1.42; IPV aOR 15.71 95%CI 1.47–167.80), report difficulty taking ART drugs (internalized stigma aOR 1.32 95%CI 1.10–1.58; anticipated stigma aOR 1.14 95%CI 1.01–1.30) and not taking medication as prescribed (IPV aOR 2.00 95%CI 1.05–3.74). Depression was additionally associated with decreased odds of viral load suppression (aOR 0.16 95%CI 0.04–0.76). There is need to develop tailored psychosocial interventions within PMTCT programs that appropriately address mental health, stigma, and violence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Women living with HIV often suffer from gender-based violence [1, 2] depression [2, 3], and experience both externalized/anticipated and internalized HIV-related stigma [1, 3,4,5]. Findings from community surveys across various geographic settings indicate that nearly 70% of HIV-infected women report depression, HIV-related internalized stigma, discrimination and/or intimate partner violence (IPV) [2]. The prevalence of these psychosocial factors is particularly elevated among pregnant women living with HIV [2, 6,7,8,9].
The associations between depression, IPV, HIV-related stigma and HIV infection are most likely bidirectional [9, 10]. This complexity, as well as, overlap of disease burden and presentation, often results in providers focusing on HIV alone and failing to recognize and counseling for the co-existing HIV-related stigma, depression and IPV [11]. The under-recognition of depression, stigma and IPV among HIV-infected pregnant and postpartum women can have deleterious effects on their ability to engage and adhere to prevention of mother-to-child transmission of HIV (PMTCT) interventions. Studies show that HIV-related stigma is a significant barrier to adherence to medication and clinic visits, which are critical for PMTCT and overall maternal health [12, 13]. Additionally, a recent systematic review among persons living with HIV and AIDS in Sub-Saharan African found that the likelihood of ART adherence was 55% lower among those with depressive symptoms compared to those without [14]. Similarly, experiencing IPV has been associated with decreased adherence to PMTCT interventions during and after pregnancy [15].
Over time, PMTCT programs are finding that in addition to providing drugs, peer and community support strategies can promote uptake, adherence and lifelong retention in care, improve mental health, reduce HIV-related stigma, and abate potential IPV arising from engagement into care [16, 17]. Within the context of a community-based cluster-randomized trial evaluating the impact of community mentor mothers (cMMs) and mobile phone text messaging on PMTCT outcomes [18], we sought to evaluate the association of psychosocial factors (HIV-related stigma, depression, and IPV) with PMTCT adherence and retention in HIV-infected postpartum women receiving lifelong ART in western Kenya. Causal relationships with poor adherence difficulty taking ART as prescribed, missed clinic visits and laboratory detected viral loads > 1000 copies/mL were hypothesized for each of these psychosocial factors. Analyses controlled for socio-demographic characteristics and exposure to the MOTIVATE interventions.
Methods
We undertook a cross-sectional survey with women participating in a cluster-randomized controlled trial, the Mother and Infant Visit Adherence and Treatment Engagement (MOTIVATE) study (parent study). Full details of this trial have been published previously [18]. Briefly, MOTIVATE is a cluster randomized 2X2 factorial, controlled trial in western Kenya testing the individual and combined impact of cMMs and text messages on ART adherence and retention in HIV care in the context of Option B+ (PMTCT national policy) [18]. The interventions include: (1) cMMs who conduct home visits in the community to assist participants with safe disclosure, support safe infant feeding, promote safer sex and family planning, encourage early infant testing and follow up, and promote ART adherence and return for HIV care visits; (2) mobile phone text messages with bi-directional communication that send reminders to adhere to care and provide messages on healthy behaviors during pregnancy and the postpartum periods in the participants’ preferred language with the option to communicate directly with staff; (3) integration of both cMM and text messages; or (4) standard of care. The study enrolled women living with HIV who were 18 years or older; willing to have home visits (or meetings with a cMM in an alternate location); and had access to a mobile phone. Between December 2015 and August 2017, trained study nurses recruited women (N = 1338) from 24 antenatal care (ANC) clinics providing PMTCT. These ANC clinics were public Ministry of Health facilities whose ART services are supported by local CDC-PEPFAR funded partners and free to patients.
Study Setting
The study was conducted in three counties (Homabay, Migori and Kisumu) of southwestern Kenya. This southwestern region accounts for approximately one-third of all HIV infections in Kenya. This region has consistently battled the highest HIV prevalence rates of any region in the country, with current estimates at: 13.3% in Migori country, 16.3% in Kisumu country, and 20.7% in Homa Bay County [19].
Sub-study Population
For this cross-sectional sub study, we enrolled women (n = 200) who were participating in the MOTIVATE study and who were at least 12 months postpartum at the time of the study. All women were retained in HIV care at the time of enrollment. The goal of this sub-study was to determine associations of HIV-related stigma, depression, and IPV with self-reported ART medication and HIV care visit adherence, and viral load suppression among HIV-infected postpartum women receiving Option B+ PMTCT services and enrolled in one of the four MOTIVATE study arms in southwestern Kenya.
Data Collection
Verbal, interviewer-administered quantitative surveys were used to collect data from participants between May and September 2017. Surveys were conducted in the participant’s preferred language (Dholuo, Kiswahili or English) and entered into tablet-based REDCap database application [20] maintained by the University of Colorado, Denver. We also abstracted participant data from the MOTIVATE study database based on participants health records at the local clinics. The survey modules included: measures of socio-demographic characteristics; depression; anticipated and internalized stigma; self-reported PMTCT adherence and ART experiences; male partner involvement; and intervention experience and perceptions. Participants were paid a small travel reimbursement.
Measures
Socio-demographic variables used in the analysis included age, marital status, highest educational level, parity (number of biological children the woman had birthed), ownership of a personal mobile phone, and presence electricity in the house. Depression was measured using the eight-item Patient Health Questionnaire Depression Scale (PHQ-8), which asks how frequently in the past 2 weeks participants experienced depression symptoms, including little interest or pleasure in doing things, feeling down, depressed, or hopeless, trouble sleeping, little energy, poor appetite or over-eating, feeling bad about self, difficulty concentrating, or moving or speaking slowly [21]. The PHQ-8 is similar to the PHQ-9, which has been previously validated in sub-Saharan settings, except that it omits one item that assesses suicidal ideation [22]. Due to a lack of crisis mental health services in the study setting, we could not ethically inquire about suicidal ideation. The PHQ-8 is scored just like the PHQ-9 and its total score ranges from 0 to 24. Responses are on a 4-point Likert scale (not at all, several days, more than half the days, nearly every day). We aggregated the responses, creating an overall score, which was used to generate a binary variable for major depression (Yes/No). Cut-points on the PHQ-8 are identical to the PHQ-9. Scores of 5, 10, 15, and 20 represent cut-points for mild, moderate, moderately severe and severe depression, respectively. For this analysis, any score ≥ 10 was classified as major depression [21, 23]. The PHQ-8 used in the study had good internal consistency (Cronbach’s alpha = 0.72). Internalized stigma was measured using a modified version of the self-stigma subscale of the HIV/AIDS Stigma Instrument-PLWA (HASI-P), which has been used throughout sub-Saharan African settings, including Kenya [24]. This subscale includes 6 items on Negative Self-Perception, namely “in the last 12 months, have you felt:” (1) shame, (2) guilt, (3) self-blame, (4) blaming others, (5) low self esteem, and (6) deserving of punishment. The original scale includes seven items with a question regarding suicidality. Again we omitted the question on suicidality for reasons stated above. Responses were on a 4-point Likert scale (never, rarely, sometimes, often), from which we generate a binary variable indicating any experiences of internalized stigma (Yes/No).
We used a five-item anticipated HIV-related stigma scale to measure participants’ perceived fears of repercussions after HIV status disclosure, including (1) discrimination, (2) being kicked out of the community, (3) violence, (4) losing employment, or (5) being kicked out of their house. These measures are based on similar measures used in other studies to assess anticipated stigma in sub-Saharan Africa and other global settings [25,26,27]. Responses were on a 4-point Likert scale (strongly disagree, disagree, agree, strongly agree) from which we generate a binary variable indicating any experiences of anticipated stigma (Yes/No).
Regarding IPV, participants were asked how often they experienced incidences of physical and verbal partner violence using questions adapted from previous measures of affective (emotional) support and interactions within heterosexual couples [28, 29]. Questions asked how often the male partner has physically hurt her during a disagreement; and how often the male partner has said cruel or angry things during a disagreement (all the time, most of the time, more often than not, occasionally, rarely, never). We subsequently created binary variables for the analysis from these response categories indicating any experiences with physical or emotional IPV.
We measured ART adherence by asking women if they have ever had any difficulty taking ART (Yes/No) and how often they took their medication the way they were supposed to (as prescribed) in the past 30 days (never, rarely, sometimes, usually, almost always, always). Using this variable, we created an adherence to ART variable (yes/no) using a cut-off of taking as prescribed almost always/always. We also asked participants how often they missed clinic visits in the past year. Any missed clinic visit in the past year was considered non-adherent.
Viral load measurements were conducted after 6 months of ART for those newly initiating (or at time of pregnancy identification for those already on ART). In line with existing national guidelines at time of study implementation, those with viral load < 1000 copies/mL were considered virally suppressed [30].
Statistical Analyses
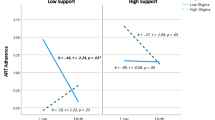
Redcap survey data were exported into Stata 14 for statistical analysis. Descriptive statistics were used to characterize study variables. Adjusted and non-adjusted logistic regression models were used to examine the association of internalized and anticipated HIV-related stigma, IPV, and depression with: (1) difficulty taking ART, (2) taking medication as prescribed, (3) missing clinic visits and (4) viral load suppression. Analyses, in each model, controlled for age, partner HIV status, education, parity, electricity and intervention arm. For each variable investigated, the proportion of missing responses was < 5%. It was hypothesized that the relationship between HIV-related internalized stigma and the study outcomes would be different among women with depression and women without depression. In order to investigate this hypothesis, interaction terms were included in the adjusted logistic regression models. The interaction between internalized stigma and depression fell short of statistical significance in all models run for difficulty taking ART (Coeff 0.02 SE 0.02 95%CI − 0.01 to 0.06), taking medication as prescribed (Coeff − 0.01 SE 0.02 95%CI − 0.06 to 0.03), missing clinic visits (Coeff 0.00 SE 0.02 95%CI − 0.03 to 0.04) and viral load suppression (Coeff − 0.01 SE 0.02 95%CI − 0.05 to 0.03). As such we dropped the interaction term from the models and reran the models.
Results
Sociodemographic Characteristics
The total sample size was 200 women (see Table 1). The mean age of the women was 28.5 (SD 5.1) years. Among the women surveyed, 88.5% were currently married. A total of 73.0% reported completion of primary-level education, but only 48.5% could easily read a newspaper. Approximately 73.7% of women owned a personal mobile phone. The average number of births per participant was 3.5 births (SD 1.7). Women’s main source of income was predominantly from “selling things” (31.5%) or doing “farming or agricultural work” (30.5%). At least 17.0% of women reported food insecurity (i.e., sometimes or often experiencing no resources to buy food in the past month). Disclosure of one’s HIV positive status to their husband/partner was high with 95.5% of women reporting they told their partner they were HIV-positive.
Prevalence of IPV, HIV-Related Stigma, and Depression
Of the 200 women included in the analysis, 25.5% met criteria for major depression, 56.7% reported HIV-related internalized stigma, 42.9% experienced HIV-related anticipated stigma and 58.0% had experienced IPV [combined physical (53.9% and emotional (93.3%)].
Description of Outcomes
Of the 200 women included in the analysis, 126 (63.0%) Reported adherence to both ART and clinic visits. Yet, 8.5% reported having missed at least one clinic visit in the past one year, 11.3% reported difficulty taking ART, 18.3% reported not taking medication as had been prescribed in the last 30 days and 11.6% had not achieved viral load suppression.
Risk Factors for IPV, Stigma, and Depression
In the multivariable models, living in a house with more than one room (aOR 0.34 95%CI 0.14–0.78) and having electricity (aOR 0.22 95%CI 0.05–0.99) were significantly associated with decreased odds of major depression. Within this population, major depression and internalized stigma were highly correlated. We found that experiencing internalized stigma significantly increased the odds of reporting depressive symptoms (aOR 1.22 95%CI 1.09–1.36). Major depression also significantly increased the odds of experiencing internalized stigma (aOR 4.29 95%CI 1.72–10.71). IPV neither predicted nor is predicted by any stigma and major depression or by any other covariates in the model. Likewise, anticipated stigma was neither predictive nor predicted by internalized stigma, depression, IPV or other factors in the model.
Association Between IPV, Stigma, and Depression with PMTCT Outcomes
Table 2 presents the results of the unadjusted and adjusted models. Women who experienced either internalized or anticipated stigma were more likely to miss clinic visits (internalized stigma aOR 1.22 95%CI 1.08–1.38; anticipated stigma aOR 1.21 95%CI 1.04–1.42). Experiencing IPV was also significantly associated with increased odds of missing clinic visits (aOR 15.72 95%CI 1.47–167.79). Having depressive symptoms was not associated with missing clinic visits.
Experiencing IPV was significantly associated with decreased odds of taking ART as prescribed (aOR 0.18 95%CI 0.04–0.72). In addition, experiencing anticipated stigma was marginally associated with decreased odds of taking ART as prescribed (aOR 0.83 95%CI 0.68–1.00). Neither having major depressive symptoms nor experiencing internalized stigma were associated with taking ART as prescribed. However, women who experienced either internalized or anticipated stigma were more likely to report difficulty taking ART drugs (internalized stigma aOR 1.32 95%CI 1.10–1.58; anticipated stigma aOR 1.14 95%CI 1.01–1.30). There was however, no statistically significant association between difficulty taking ART drugs with depressive symptoms or IPV. Moreover, in this cohort of women, having major depressive symptoms was statistically significantly associated with reduced odds of viral load suppression (aOR 0.16 95%CI 0.04–0.76).
Discussion
In this paper, we present results on association of depression, stigma and IPV with postpartum women’s adherence and engagement in PMTCT from a cross-section of HIV-infected women enrolled in the MOTIVATE study. We found a high prevalence of major depressive symptoms (26%), endorsement of any internalized stigma (57%), endorsement of any anticipated stigma (43%) and physical and emotional IPV (58%). Several systematic reviews in sub-Saharan Africa corroborate these high prevalence findings [7, 9, 31]. A cross sectional survey of 2042 postpartum women using an adapted WHO questionnaire in Zimbabwe found that 63.1% of respondents reported physical, emotional and/or sexual IPV during pregnancy [32]. Owing to the large diversity in the methods and conceptualization of depression, prevalence has ranged from as low as 10% in observational studies in Tanzania [33] to nearly 50% in a cross-sectional study of 663 South African women using the Edinburgh Postnatal Depression Scale [34]. In addition, our results show that stigma, depression, and IPV experienced by HIV-infected women had an impact on their adherence to ART and attendance of clinic visits, as well as viral load suppression. Our study also found that women who reported major depressive symptoms had lower odds of viral load suppression. Extant literature demonstrates that depression affects HIV treatment outcomes through both immunological pathways and health behavior pathways [33, 35]. Depression has been associated with low CD4 counts [36], high viral loads and increased mortality [37, 38]. It is likely that the feelings of worthlessness, loss of interest and lack concentration that characterize depression are causal pathways through which depression affects adherence [39] and impedes efforts to achieve viral suppression. While our study did not show any associations between adherence to medication and clinic visits (likely due to the small sample size and lack of statistical power to detect small differences), studies show that it is plausible that depression can work independent of non-adherence behaviors to affect HIV treatment outcomes for patients on ART [36]. We recommend additional research exploring the mechanisms behind such associations.
The observed high prevalence of depressive symptoms in HIV infected postpartum women, and poor viral load suppression underscores the need for identification and clinical management of depression during perinatal period. The majority of participants in this study (80.0%) were exposed to the cMM and/or text messaging interventions of the MOTIVATE parent study. Yet, a high prevalence of depressive symptoms at 12 months postpartum was observed in the sample. This highlights the need for mobile and community-based interventions to incorporate the mental health needs of HIV-infected women in low resource, high HIV-prevalence settings.
In this study, experiencing IPV was associated with increased odds of missing clinic appointments and not taking ART as prescribed. These findings support prior research indicating that IPV impacts mother-to-child-transmission because it affects adherence to both medication and clinic visits [40, 41]. A recent systematic review found that IPV was associated with lower ART use, decreased odds of self-reported ART adherence and significantly poorer viral suppression among women [42]. IPV likely hinders medication and clinic adherence through several social mechanisms, such as decreased HIV status disclosure to partners and poor spousal communication, which are important predictors of positive PMTCT experiences [43,44,45]. Abusive male partners are also less likely to take part in PMTCT services, including accompanying women to visits or picking up medication; which in turn, makes adherence more arduous on the woman [46, 47].
IPV may also impact MTCT outcomes through cognitive/mental pathways. IPV can increase the risk of emotional distress, depression, and post-traumatic stress disorder, which are often not noticed by health care providers; yet, are known barriers to HIV-related medical adherence [40, 42]. Unfortunately, the high prevalence of IPV in this study affirms numerous studies done in sub-Saharan Africa showing high burdens of IPV among women, especially women living with HIV [7]. Besides the plausible bidirectionality of the relationship between IPV and HIV [40, 42], it is likely that underlying structural factors such as poverty, women disempowerment and acceptance of domestic violence as a cultural norm further aggravate the situation [7, 15]. In a setting such as southwestern Kenya where a high IPV prevalence intersects with a high HIV prevalence, it is likely that siloed-interventions that target individual woman or health care workers alone without addressing the underlying structural and cultural specific contexts of gender inequities and violence will be unsuccessful [15].
In terms of stigma, we found that women who experienced HIV-related stigma were more likely to miss clinic visits and to report difficulty taking ART drugs. These findings are consistent with those of other studies, which have found that HIV-related stigma adversely affects multiple steps along the PMTCT cascade [48] and affects other factors that may impede medication and clinic visit adherence such as HIV serostatus disclosure, social support and mental wellbeing [48, 49]. HIV-related stigma can also contribute to depressive symptoms, compounding the negative impact on women living with HIV. In addition to having direct negative effects on depression, HIV-related stigma can also lead to refusal of HIV-testing [25], lack of HIV-status disclosure [45, 49]; and avoidance of the ANC clinic and HIV care [50], which can result in negative maternal and infant PMTCT health outcomes. The high levels of HIV-related stigma in the women in this study and persistent high prevalence in sub-Saharan Africa despite ART expansion and numerous interventions, implies that further study on multi-faceted adaptive interventions that can be scaled up on a national or regional level to effectively target stigma are warranted [51].
The findings of this cross-sectional survey need to be considered in view of several limitations. Firstly, self-reporting is prone to social desirability and recall biases. Several measures were implemented to minimize this problem, including use of pre-validated and standardized tools to collect the information and use of well- trained, local gender-matched interviewers. Secondly, the study was conducted among a sample of women enrolled in the MOTIVATE trial evaluating the impact of community mentor mothers and text messaging on PMTCT outcomes. As such, this sample may not be representative of the whole of women accessing PMTCT services in Kenya. Regarding study measures: Both internalized and anticipated HIV-related stigma were measured using fairly robust measures but we chose to dichotomize this variable for our primary analyses for ease of interpretation. We recognize that this may have resulted in loss of information and reduced statistical power. However this disadvantage is balanced by the fact that use of binary measures for analysis of HIV-related stigma has been done in numerous studies in this population [50, 52] and that in rerunning the analysis with the scales and not as binary measures, there was no difference in the direction and magnitude of relationships. Secondly, viral load levels included in the analysis were those done within the last year and might therefore not represent the most current levels. However, this represents the actual in-country guidelines for testing which are done once every 6 months. The sample size for this study was small which increases the likelihood of a type II error and a bias towards the null. Finally, we analyzed cross-sectional data and this does not allow any inferences to be made regarding causality and temporality with respect to the relationship between depression, HIV-related stigma and IPV and difficulty taking ART, taking medication as prescribed, missing clinic visits and 4) viral load suppression.
Conclusion
These cross-sectional results indicate that stigma, depression, and IPV experienced by HIV-infected women may impact their adherence to medication and clinic visits, which are critical for PMTCT and maternal health. The high prevalence of these issues underscores the importance of developing tailored psychosocial and structural interventions to improve mental health and reduce stigma and IPV to improve adherence and engagement in care within PMTCT.
References
Orza L, Bewley S, Chung C, Crone ET, Nagadya H, Vazquez M, et al. “Violence. Enough already”: findings from a global participatory survey among women living with HIV. J Int AIDS Soc. 2015;18(Suppl 5):20285.
Narasimhan M, Orza L, Welbourn A, Bewley S, Crone T, Vazquez M. Sexual and reproductive health and human rights of women living with HIV: a global community survey. Bull World Health Organ. 2016;94(4):243–9.
Orza L, Bewley S, Logie CH, Crone ET, Moroz S, Strachan S, et al. How does living with HIV impact on women’s mental health? Voices from a global survey. J Int AIDS Soc. 2015;18(Suppl 5):20289.
Kohler PK, Ondenge K, Mills LA, Okanda J, Kinuthia J, Olilo G, et al. Shame, guilt, and stress: Community perceptions of barriers to engaging in prevention of mother to child transmission (PMTCT) programs in western Kenya. AIDS Patient Care STDs. 2014;28(12):643–51.
Turan JM, Nyblade L. Global maternal and child health goals will not be achieved without addressing HIV-related stigma. J Acquir Immune Defic Syndr. 2013;64(1):e9–10.
Mitchell J, Wight M, Van Heerden A, Rochat TJ. Intimate partner violence, HIV, and mental health: a triple epidemic of global proportions. Int Rev Psychiatry (Abingdon, Engl). 2016;28(5):452–63.
Shamu S, Abrahams N, Temmerman M, Musekiwa A, Zarowsky C. A systematic review of African studies on intimate partner violence against pregnant women: prevalence and risk factors. PLoS ONE. 2011;6(3):e17591.
Turan B, Stringer KL, Onono M, Bukusi EA, Weiser SD, Cohen CR, et al. Linkage to HIV care, postpartum depression, and HIV-related stigma in newly diagnosed pregnant women living with HIV in Kenya: a longitudinal observational study. BMC Pregnancy Childbirth. 2014;14:400.
Sowa NA, Cholera R, Pence BW, Gaynes BN. Perinatal depression in HIV-infected African women: a systematic review. J Clin Psychiatry. 2015;76(10):1385–96.
Campbell JC, Baty ML, Ghandour RM, Stockman JK, Francisco L, Wagman J. The intersection of intimate partner violence against women and HIV/AIDS: a review. Int J Injury Control Saf Promot. 2008;15(4):221–31.
Asch SM, Kilbourne AM, Gifford AL, Burnam MA, Turner B, Shapiro MF, et al. Underdiagnosis of depression in HIV: who are we missing? J Gen Intern Med. 2003;18(6):450–60.
Turan JM, Nyblade L. HIV-related stigma as a barrier to achievement of global PMTCT and maternal health goals: a review of the evidence. AIDS Behav. 2013;17(7):2528–39.
Knettel BA, Cichowitz C, Ngocho JS, Knippler ET, Chumba LN, Mmbaga BT, et al. Retention in HIV care during pregnancy and the postpartum period in the Option B+ era: systematic review and meta-analysis of studies in Africa. J Acquir Immune Defic Syndr. 2018;77(5):427–38.
Nakimuli-Mpungu E, Bass JK, Alexandre P, Mills EJ, Musisi S, Ram M, et al. Depression, alcohol use and adherence to antiretroviral therapy in sub-Saharan Africa: a systematic review. AIDS Behav. 2012;16(8):2101–18.
Hampanda KM. Intimate partner violence and HIV-positive women’s non-adherence to antiretroviral medication for the purpose of prevention of mother-to-child transmission in Lusaka, Zambia. Soc Sci Med. 1982;2016(153):123–30.
Matheson R, Moses-Burton S, Hsieh AC, Dilmitis S, Happy M, Sinyemu E, et al. Fundamental concerns of women living with HIV around the implementation of Option B+. J Int AIDS Soc. 2015;18(Suppl 5):20286.
Phiri S, Tweya H, van Lettow M, Rosenberg NE, Trapence C, Kapito-Tembo A, et al. Impact of facility- and community-based peer support models on maternal uptake and retention in Malawi’s Option B+ HIV prevention of mother-to-child transmission program: a 3-arm cluster randomized controlled trial (PURE Malawi). J Acquir Immune Defic Syndr. 1999;2017(75 Suppl 2):S140–8.
Odeny TA, Onono M, Owuor K, Helova A, Wanga I, Bukusi EA, et al. Maximizing adherence and retention for women living with HIV and their infants in Kenya (MOTIVATE! study): study protocol for a randomized controlled trial. Trials. 2018;19(1):77.
National AIDS Control Council. Kenya HIV estimates: report 2018. Nairobi: Ministry of Health; 2018.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–73.
Cholera R, Gaynes BN, Pence BW, Bassett J, Qangule N, Macphail C, et al. Validity of the patient health questionnaire-9 to screen for depression in a high-HIV burden primary healthcare clinic in Johannesburg, South Africa. J Affect Disord. 2014;167:160–6.
Kroenke K, Spitzer RL, Williams JB, Lowe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345–59.
International Parenthood Federation (IPF), Global Network of People Living with HIV (GNP+), International Community of Women Living with HIV (ICW), UNAIDS. The people living with HIV Stigma Index: an index to measure the stigma and discrimination experienced by people living with HIV. London: International Parenthood Federation; 2008.
Turan JM, Bukusi EA, Onono M, Holzemer WL, Miller S, Cohen CR. HIV/AIDS stigma and refusal of HIV testing among pregnant women in rural Kenya: results from the MAMAS Study. AIDS Behav. 2011;15(6):1111–20.
Weiser SD, Heisler M, Leiter K, Percy-de Korte F, Tlou S, DeMonner S, et al. Routine HIV testing in Botswana: a population-based study on attitudes, practices, and human rights concerns. PLoS Med. 2006;3(7):e261.
Siedner MJ, Tsai AC, Dworkin S, Mukiibi NF, Emenyonu NI, Hunt PW, et al. Sexual relationship power and malnutrition among HIV-positive women in rural Uganda. AIDS Behav. 2012;16(6):1542–8.
Schuster TL, Kessler RC, Aseltine RH. Supportive interactions, negative interactions, and depressed mood. Am J Community Psychol. 1990;18(3):423–38.
Turner RJ, Frankel BG, Levin DM. Social support: conceptualization, measurement, and implications for mental health. Res Community Mental Health. 1983;3:67–111.
National AIDS and STI Control Programme. Guidelines on use of antiretroviral drugs for treating and preventing HIV infection in Kenya. Nairobi: National AIDS & STI Control Program, Ministry of Health Kenya; 2018.
Devries KM, Mak JYT, García-Moreno C, Petzold M, Child JC, Falder G, et al. The global prevalence of intimate partner violence against women. Science. 2013;340(6140):1527–8.
Shamu S, Abrahams N, Zarowsky C, Shefer T, Temmerman M. Intimate partner violence during pregnancy in Zimbabwe: a cross-sectional study of prevalence, predictors and associations with HIV. Trop Med Int Health. 2013;18(6):696–711.
Belenky NM, Cole SR, Pence BW, Itemba D, Maro V, Whetten K. Depressive symptoms, HIV medication adherence, and HIV clinical outcomes in Tanzania: a prospective, observational study. PLoS ONE. 2014;9(5):e95469.
Peltzer K, Rodriguez VJ, Jones D. Prevalence of prenatal depression and associated factors among HIV-positive women in primary care in Mpumalanga province, South Africa. SAHARA J. 2016;13(1):60–7.
Evans DL, Leserman J, Pedersen CA, Golden RN, Lewis MH, Folds JA, et al. Immune correlates of stress and depression. Psychopharmacol Bull. 1989;25(3):319–24.
Bouhnik AD, Preau M, Vincent E, Carrieri MP, Gallais H, Lepeu G, et al. Depression and clinical progression in HIV-infected drug users treated with highly active antiretroviral therapy. Antiviral Ther. 2005;10(1):53–61.
Cook JA, Grey D, Burke J, Cohen MH, Gurtman AC, Richardson JL, et al. Depressive symptoms and AIDS-related mortality among a multisite cohort of HIV-positive women. Am J Public Health. 2004;94(7):1133–40.
Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, Boland RJ, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA. 2001;285(11):1466–74.
Rao D, Feldman BJ, Fredericksen RJ, Crane PK, Simoni JM, Kitahata MM, et al. A structural equation model of HIV-related stigma, depressive symptoms, and medication adherence. AIDS Behav. 2012;16(3):711–6.
Hatcher AM, Woollett N, Pallitto CC, Mokoatle K, Stockl H, MacPhail C, et al. Bidirectional links between HIV and intimate partner violence in pregnancy: implications for prevention of mother-to-child transmission. J Int AIDS Soc. 2014;17:19233.
Lopez EJ, Jones DL, Villar-Loubet OM, Arheart KL, Weiss SM. Violence, coping, and consistent medication adherence in HIV-positive couples. AIDS Educ Prev. 2010;22(1):61–8.
Hatcher AM, Smout EM, Turan JM, Christofides N, Stockl H. Intimate partner violence and engagement in HIV care and treatment among women: a systematic review and meta-analysis. AIDS (London, England). 2015;29(16):2183–94.
Awiti Ujiji O, Ekstrom AM, Ilako F, Indalo D, Wamalwa D, Rubenson B. Reasoning and deciding PMTCT-adherence during pregnancy among women living with HIV in Kenya. Culture Health Sex. 2011;13(7):829–40.
Spangler SA, Onono M, Bukusi EA, Cohen CR, Turan JM. HIV-positive status disclosure and use of essential PMTCT and maternal health services in rural Kenya. J Acquir Immune Defic Syndr. 2014;67(Suppl 4):s235–42.
Onono MA, Cohen CR, Jerop M, Bukusi EA, Turan JM. HIV serostatus and disclosure: implications for infant feeding practice in rural south Nyanza, Kenya. BMC Public Health. 2014;14:390.
Msuya SE, Mbizvo EM, Hussain A, Uriyo J, Sam NE, Stray-Pedersen B. Low male partner participation in antenatal HIV counselling and testing in northern Tanzania: implications for preventive programs. AIDS Care. 2008;20(6):700–9.
Akama E, Mburu M, Mutegi E, Nyanaro G, Otieno JP, Ndolo S, et al. Impact of a rapid results initiative approach on improving male partner involvement in prevention of mother to child transmission of HIV in Western Kenya. AIDS Behav. 2018;22(9):2956–65.
Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3 Suppl 2):18640.
Tsai AC, Bangsberg DR, Kegeles SM, Katz IT, Haberer JE, Muzoora C, et al. Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Ann Behav Med. 2013;46(3):285–94.
Turan JM, Hatcher AH, Medema-Wijnveen J, Onono M, Miller S, Bukusi EA, et al. The role of HIV-related stigma in utilization of skilled childbirth services in rural Kenya: a prospective mixed-methods study. PLoS Med. 2012;9(8):e1001295.
Chan BT, Tsai AC, Siedner MJ. HIV treatment scale-up and HIV-related stigma in sub-Saharan Africa: a longitudinal cross-country analysis. Am J Public Health. 2015;105(8):1581–7.
Medema-Wijnveen JS, Onono M, Bukusi EA, Miller S, Cohen CR, Turan JM. How perceptions of HIV-related stigma affect decision-making regarding childbirth in rural Kenya. PLoS ONE. 2012;7(12):e51492.
Acknowledgement
We thank the Kenyan women who participated in this cross-sectional survey and the research assistants who collected the data. We acknowledge the support of the Kenya Medical Research Institute (KEMRI), the Director of KEMRI and the Director of the Centre for Microbiology Research (CMR). Funding for the MOTIVATE! study is supported by Award Number R01HD080477 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) (USA). Funding for the sub-study was supported by Award Number 4T32AI007447 from the National Institute of Allergy and Infectious Diseases (NIAID). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NICHD, NIAID or the NIH. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
The ethics committees of the Kenya Medical Research Institute, the University of Colorado Denver and the University of Alabama at Birmingham gave scientific and ethical approval for the study. Informed consent was obtained prior to commencement of all study procedures including administration of the survey questionnaire. Research assistants referred women who reported violence or depression for follow-up and referrals to services.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Onono, M., Odwar, T., Abuogi, L. et al. Effects of Depression, Stigma and Intimate Partner Violence on Postpartum Women’s Adherence and Engagement in HIV Care in Kenya. AIDS Behav 24, 1807–1815 (2020). https://doi.org/10.1007/s10461-019-02750-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02750-y