Abstract
Compared to HIV research on men who have sex with men, less is known about the risks and vulnerabilities for HIV among Male to Female (MTF) transgender persons, particularly in different geographic regions like Mexico. In Tijuana, Mexico, a border city experiencing a dynamic HIV epidemic, no precedent data exists on the MTF transgender population. Our aims were to estimate HIV prevalence and examine the behaviors and characteristics of the population. We conducted a cross-sectional study of 100 MTF transgender persons recruited through time location sampling in 2012. Participants underwent interviewer-administered (paper and pen) surveys and rapid tests for HIV. Descriptive univariate analyses were conducted on various factors, including sociodemographics, substance use, accessing social services (requested vs. received), stigma, and sex behaviors. A total of 22% tested positive for HIV, a prevalence higher than other key populations at risk for HIV in Tijuana.
Resumen
Comparado al estudio del VIH de hombres que tienen sexo con hombres (HSH), se sabe menos de los riesgos y vulnerabilidades de VIH entre hombre a mujer (HAM) personas transgeneras, particularmente en diferentes regiones geográficas como México. En Tijuana, México, una ciudad fronteriza que esta pasando por una etapa dinámica de la epidemia del VIH, no existe datos precedentes sobre la HAM populación transgenera. Nuestros objetivos eran estimar la prevalencia del VIH y examinar las características y comportamientos de la populación. Se realizo un estudio transversal de 100 HAM personas transgeneras reclutadas con muestreo por tiempo-lugar en el 2012. Los participantes se sometieron a entrevistas administradas (A papel y pluma) y prueba rápida de VIH. Se realizaron análisis descriptivos univariados sobre diversos factores, incluyendo sociodemográficas, uso se sustancias, accediendo seguros sociales (pedidos vs recibidos), stigma, y comportamiento sexual. Un total de 22% fueron positivos de VIH, una prevalencia más alto que cualquier otra populación en riesgo de VIH en Tijuana.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Compared to research on men who have sex with men, male to female (MTF) transgender persons have been relatively neglected in the HIV literature. For the purpose of this paper, the term MTF transgender persons is used for people who were assigned male at birth, but identify as women. In the United States, several studies have suggested a high burden of HIV infection among MTF transgender persons. In four studies looking at HIV infection among MTF transgender persons, the proportion who were confirmed to be HIV-positive ranged from 16 to 68% [1]. Whereas the HIV research on this key population has grown in the last 5–10 years, there has been a lack of representation of MTF transgender individuals from low and middle income countries in Latin America, including Mexico. Since risk and vulnerabilities for HIV infection vary across social contexts and geographical regions, there is a need to examine these topics within the socio-cultural context of MTF in different countries.
Since the beginning of the epidemic, HIV in Mexico has been characterized as concentrated, having prevalence higher than 5% in specific population groups [2]. The population of MTF transgender persons has been poorly studied in Mexico. The conditions of vulnerability to HIV infection faced by MTF transgender individuals are often very different than those faced by men who have sex with men (MSM) [3]. MTF transgender persons are often not considered in the design of programs and HIV prevention campaigns [3]. MTF transgender persons associate the construction of the female identity with a lack of autonomy to make their own decisions about their own bodies. In this social construction, domination by males is established. This social structure and gender inequity is shared by a large number of MTF transgender persons, which increases their vulnerability and risk of infection and transmission of sexually transmitted infection (STI) [4]. Qualitative studies suggest that the population lives in conditions of vulnerability and marginalization [5] that result in increased risk of acquiring sexually transmitted diseases, substance use [6], mental health problems [7] and complications related to transition from male to female [8], as well as barriers to access health services [9, 10]. In addition, there is a robust literature on how multiple negative economic, psychosocial, and health conditions co-occur and intersect to increase risks for HIV among disadvantaged and marginalized populations, including MSM in Tijuana, Mexico [11,12,13]. In a study conducted in Mexico City, a total of 585 MTF transgender persons were interviewed and tested for HIV. The prevalence who were HIV-positive ranged from 20 to 64%. However, data suggests that transgender women report a relatively high degree of anticipated stigma, or anticipated negative intrapersonal and interpersonal consequences from an HIV diagnosis, and that this decreases their likelihood of HIV testing [14]. Thus, current estimates of HIV prevalence or incidence are likely conservative.
Tijuana is located adjacent to San Diego, California, on the U.S. border, and is experiencing an escalating HIV epidemic [15]. Baja California has the second highest cumulative AIDS incidence among Mexico’s 32 states [15], and prevalence is highest among certain subgroups that include injection drug users (4%) [16], female sex workers (6%) [17] and their male clients (5%) [18], and men who have sex with men (17%) [19]. While these populations have been well examined [17], little is known about MTF transgender persons. Identifying the prevalence among MTF transgender persons in Tijuana is key to developing prevention strategies among this population and curbing the growing HIV epidemic in the US–Mexico border region.
There is a lack of documentation of HIV prevalence among MTF transgender persons in Tijuana and their risk factors. Due to lack of empirical data, HIV/AIDS risk among MTF transgender persons in Tijuana is not well understood [20]. MTF transgender persons face specific risk and multiple layers of social complications that make prevalence estimates challenging [21]. Designing interventions and policies according to the needs of MTF transgender persons has been difficult due to the absence of quantitative data on the socio-demographic and health conditions of the population [9]. These complications, coupled with the fact that some transgender people will never attempt to legally change their name and/or gender, complicate this method of prevalence estimation [21]. This study aims to estimate the HIV prevalence and examine the socio-demographics, HIV risk behaviors, and other characteristics among MTF transgender persons in Tijuana, Mexico.
Methods
Participants
The inclusion criteria for recruiting study participants were as follows: (1) Self-identify as a MTF transgender person and present 2 or more of the indicators of Gender Dysphoria (DSM-IV-TR) within at least 6 months of date of enrollment, (2) Be 18 years or older at the time of enrollment, (3) Willing to provide informed consent to participate in the study and receive an HIV test, and (4) Live in Tijuana at the time of enrollment. The study only had one cohort who was recruited in Tijuana, Mexico, in 2 months from February to March 2013.
After obtaining informed consent, trained interviewers conducted the survey. The study provided the structured questionnaire (paper and pen; interviewer administrated) and HIV tests; both procedures lasted approximately 1 hour and a half. When all procedures were complete, participants received a safer-sex kit and brochures (on HIV, HIV testing, and risk of self-administrated hormones), and $20.00 US Dollars to compensate them for the time spent completing the survey.
Materials and Measures
A checklist with indicators of Gender Dysphoria (DSM-IV-TR) was administered to all participants to determinate eligibility (criterion 1). The survey included socio-demographic questions such as age, education, income, sex work in the past month and lifetime, housing situation, gender identity, sexual orientation, sexual reassignment surgery, sexual risk behaviors, self-reported STIs and HIV, body modifications related with gender transition in a non-clinical environment [22], and HIV rapid testing. We also measured perceived stigma using an adapted version of a 10-item scale (α = 0.84) to measure stigma towards transgender persons [23]. Participants in the survey were required to complete both components (survey and testing) in order to be included in the analysis sample. For HIV testing, LAFON™ HIV-1/2 antibody rapid test were used for screening, all reactive results to HIV antibody rapid test were referred to health department and private medical insurances like Instituto Mexicano del Seguro Social (IMSS) for confirmatory testing.
Data Analyses
The data were analyzed using the statistical program IBM SPSS statistics, Version 17. Univariate analyses were conducted examining the characteristics of MTF transgender in Tijuana.
Results
Participant Characteristics
Table 1 summarizes sociodemographic and behavioral characteristics. Sociodemographics Most reported being single (98%); main sources of income in the past 6 months were from sex work (55%); most reported having a junior high school education or less (72%). Other characteristics not reported in the table are: (94%) of the participants were born outside of Baja California; the three most common reported states were Guerrero 17%, Sinaloa 16%, Sonora 12%, and 2% of participants were foreign born. The mean number of months residing in Tijuana was 131 months (range 1–360 months, SD 96.56). The average age was 32 years old (range 19–52, SD 8.03). The mean amount earned in the past month was $430 US Dollars. Fifty-seven percent lived in a rented house or an apartment, 18% owned a house or an apartment, and 17% lived in a motel; the mean length of time living in the actual residence was 39 months (range 1–264 months), only 2% were married with a woman before their transition. Only one participant had gone through sex reassignment surgery. Ninety-one percent reported feeling sexually attracted to men, 8% to men and women and 1% to none. Substance use Ninety-eight (98%) had never injected any drug at least in the last month; 1 (1%) participant injected speedball, and 1 (1%) injected methamphetamine (crystal) in the last month. The primary substances of choice were: alcohol (49, 49%), methamphetamine (21, 21%), marijuana (12, 12%), and 17 (17%) reported not using any type of drug or alcohol, whether by personal choice or because were in a process of rehabilitation.
Infectious diseases For diagnosis and treatment in the past year, the most reported STI diagnosed by a physician was syphilis (10%), and all received treatment, followed by Herpes simplex (2%; all received treatment). Forty-four percent self-reported they have been tested for tuberculosis, of whom 6% tested positive and received treatment, 90% had been previously tested for HIV, 12% self-reported they tested positive for HIV, and 10% were receiving HIV care locally. Most of the participants who had never been tested (n = 6, 60%) reported that they did not want to know their HIV status.
Social services requested and received
Table 2 summarizes the services requested and received by participants in the past year. The most requested service was STI screening (n = 56, 56%), followed by general medical care (n = 30, 30%), and counseling (n = 30, 30%). Of such requests, almost all were received (96.4%, 100%, and 96.7%, respectively). The types of services that were requested but least likely to be received were employment (n = 15, 65.2%), crisis intervention (n = 2, 66.7%), and permanent housing (n = 5, 71.4%).
Stigma Towards Transgender Persons
To measure stigma, we used an adapted version of the 10-item stigma towards homosexuality scale developed by Neilands et al. [23]. Table 3 summarizes responses to each item assessing stigma towards transgender persons. Of the ten items, participants tended to agree most with the following items: “I’m afraid to be hit or beaten up for being transgender” (51%) and “I’m afraid that people will make fun of me or call me names for being transgender” (46%).
Male Sex Partners and Sex Risks
Table 4 displays unprotected anal intercourse by different partner types. Other data not reported in the table provide a rich understanding of partner types and sex behaviors. Fifty-two percent of the participants reported not having a male primary private sex partner in the last 6 months, 43% reported having had one, 5% reported have had 2 or more male primary private sex partners, and among those who had a primary partner, only 28% reported still being with their male primary sex partner in the last month. The mean number for male casual private sex partners was 2.95 in the last 6 months with a standard deviation of 5.00, and a mean of 1.28 for male casual private sex partners in the last month with a standard deviation of 1.65. Other data provide an understanding of sex with male customers specifically.
Sex with Male Customers
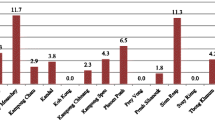
Seventy-five percent of participants reported they ever engaged in sex work in their lifetime. The mean age of starting in sex work was 20 years (range 10–48 years old; SD = 6.65). Sixty-six percent of participants were currently in sex work, and 11% exercised sex work to earn extra income apart from their part-time/full-time job. Among those who ever reported sex work in their lifetime, the methods ever used to acquire customers were: soliciting on the street (n = 62, 82.7%), bar/dance club (n = 25, 33.3%), internet (n = 22, 29.3%), print advertisement in a magazine or newspaper (n = 8, 10.7%), massage parlor (n = 2, 2.7%), and escort agency (n = 1, 1.3%). The mean number of days per week working in sex work was 4.37 (range 1–7, SD = 1.83), the mean number hours working in sex work was 29.80/week (range 1–84 h, SD = 19.57) with a mean number of customers of 12.69 (range 1–48 customers, SD = 11.13), and mean time spent per customer of 34.80 min (range 10–90 min, SD 17.1).
Participants who ever engaged in sex work reported carrying a mean of 17 condoms per day, 60 (80%) carried lubricant, and 16 (21.3%) reported carrying anything to defend themselves in case they needed it. The locations where participants had sex with customers were hotel room (54, 72%), participant’s house (21, 28%), and car (18, 24%). Forty-six (61.3%) reported that customers offered to pay more money to not use a condom for oral or anal sex and only 14 (18.7%) of the participants agreed not to use a condom. Forty-one (54.6%) reported always using condoms for receptive oral sex; the reasons why participants did not use condoms were because the customer offered to pay more to not use one (4, 5.3%), the customer did not want to use one (3, 4%), and because they believed that the customer looked healthy (4, 5.3%). When it comes to the use of condom for receptive anal sex, 53 (70.7%) participants reported always using condoms; the ones who did not use condoms reported that the customer offered to pay more not to use one (2, 2.7%), and because they believed that the customer looked healthy (3, 4%). The mean number of customers in the last week were 8.88 (SD = 7.97), and the mean for customers that were repeats was 2.61 (SD = 5.50).
Hormones and Surgery
Ninety-three percent of participants reported having ever used hormones in their lifetime; 67 (72%) were self-prescribed and bought without a prescription at a drug store; 7 (7.5%) were prescribed by a physician; and 7 (7.5%) from a friend’s recommendation. Eighty-eight (94.6%) ever injected hormones, only one participant reported having shared needles or syringes for hormones with others after being cleaned in boiling water, and 85 (96.6%) reported not having any problem to get new needles and syringes every time they need it. Injections were mainly performed by a friend 33 (37.5%), by themselves 25 (28.4%), and by a medical professional 21 (23.9%); the most common medical professional doing the hormone injections were nurses. Thirty-three (37.5%) reported obtaining the needles and syringes in drug stores, 30 (34.1%) got it from a friend, and 24 (27.3%) reported they came with the hormones.
Twenty-nine (33%) were currently injecting hormones, reported having no problem getting new needles and syringes, and none shared their needles and/or syringes with others to perform injections; 11 of these individuals (37.9%) performed injections by themselves, 6 (20.7%) by a medical professional, with a nurse being the most common. The needles and syringes were obtained mainly from a friend 14 (48.3%), 8 (27.6%) in a drug store and 7 (24.1%) reported they came with the hormones.
Twenty-seven percent ever had any silicone injections. The three main parts of the body where they had silicone injections were buttocks (11, 40.7%), hips (9, 33.3%) and breasts (4, 14.8%). None of the participants had shared needles or syringes to perform silicone injections and reported always getting new ones from friends (13, 48.1%), buying them in the drug store (10, 37%), and were performed by a non-medical person (14, 51.9%) who regularly performed this service for MTF transgender, a medical professional (7, 25.9%), or a friend (14.8%).
The sexual reassignment procedures were mainly performed in México in a medical setting (12, 75%). Nine (52.9%) of these participants were planning to have other sexual reassignment procedures done, such as breast implants (5, 55.6%), facial plastic surgery (2, 22.2%), construction of vagina (1, 11.1%), and hip enlargement (1, 11.1%).
HIV Prevalence
Twenty-two (22%) participants were positive on both a rapid and confirmatory HIV test. Among the 22 participants, 12 were previously diagnosed (had self-reported a previous diagnosis), and 10 were newly diagnosed in this study. HIV prevalence was highest among MTF transgender persons who reported only having sex with men.
Discussion
Our data indicate that HIV prevalence among MTF transgender persons (22%) is the highest reported among other at-risk populations in Tijuana [16,17,18,19]. Levels of risk behaviors observed in studies of MTF transgender persons corroborate with our finding of high prevalence [9, 24]. The majority of the participants who had never been tested reported that they did not want to know their HIV status, and this could be due to stigma associated with HIV. Stigma can directly threaten the physical wellbeing of those who are stigmatized through acts of violence and through experiences of prejudice that create serious stressors to health and well-being [25]. Indeed, almost half of the participants reported being afraid of experiencing physical or psychological violence as a result of being transgender.
Social service requests for STI screening, general medical care, and counseling were common in the sample and were mostly received. However, requests for employment opportunities, crisis intervention, and permanent housing, were the services least likely to be received when requested. This is consistent with the fact that Tijuana has relatively low resources and poor infrastructure to meet some basic needs of the community (e.g., jobs and housing), which may help to drive or exacerbate risks for HIV in the transgender community.
MTF transgender persons were more likely to have unprotected sex with a male primary partner who put them at a higher risk to be exposed to HIV than their sex work partners [26]. Male primary private sex partners of MTF transgender persons may represent a possible bridge for HIV transmission among different populations. In other studies, male primary private sex partners reported sex with male and female partners, as well as MTF transgender partners [27, 28].
Most of the participants reported currently engaging in sex work, and comparable data do not exist on MTF transgender population in Tijuana. Literature supports how engagement in sex work increases the risk of acquiring HIV [29, 30]. Stigma and discrimination from potential employers is associated with a higher likelihood for MTF transgender persons to turn to sex work when other sources of income are not available, thus putting them at a higher risk for acquiring HIV and other STIs [31]. In our sample 75% of participants reported ever engaging in sex work, and about 19% agreed not to use a condom when customers offered to pay more money to not use a condom for oral or anal sex, increasing the risk of HIV and other STI transmission and acquisition.
Less is known about transgender women and men compared to other key subpopulations, but transgender persons appear to be at heightened risk for substance abuse [32]. In our sample alcohol consumption was reported but the primary drug of choice was methamphetamine (21%). Heavy alcohol drinking and use of drugs remain a significant public health problem in Tijuana, which is located on a major drug trafficking route. Both alcohol and methamphetamine use has been associated with increased sexual risks for HIV [33]. It is important to identify the unique needs and concerns of transgender individuals and culturally sensitive programs that will be successful in recruiting and retaining these individuals in drug and/or alcohol dependence treatment services [34].
The findings in this article were subject to several limitations. Participants represented a convenience sample of MTF transgender persons, more research needs to be done to better estimate HIV prevalence with MTF transgender persons. We were unable to conduct a laboratory test to exclude for any physical intersex condition. The study is also cross-sectional. Although self-reports of sexual behaviors and drug use tend to be reliable [35, 36] respondents may have minimized their reported risk behaviors due to issues of social desirability or recall bias. However, previously there were no studies until now addressing the prevalence of HIV among the transgender population in Tijuana.
Conclusions
There is a growing concern of the rising HIV epidemic in Tijuana, Mexico, a city on the US-Mexico border that may affect epidemics on both sides of the border. Compared to other high-risk groups in Tijuana such as female sex workers and injection drug users in Tijuana, no research has been done to examine HIV in Tijuana among MTF transgender persons. We conducted a cross-sectional study and the findings may not generalize to all MTF transgender populations in Tijuana. A high proportion of MTF transgender persons were unaware of their HIV status. Alcohol and methamphetamine users may be at particular risk for HIV transmission. There is a need to increase effective intervention programs to address substance use and prevent HIV, and to develop public health policies in Mexico targeted towards the MTF transgender population. Despite the fact that these individuals are often invisible, they are nevertheless at risk for acquiring HIV. Additional research is needed to identify structural and organizational policy barriers experienced by transgender persons that force a binary gender selection, and how these are related to employment, social services, housing, health and mental health care, and legal assistance [24].
References
Simon PA, Reback CJ, Bemis CC. HIV prevalence and incidence among male-to-female transsexuals receiving HIV prevention services in Los Angeles County. AIDS Lond Engl. 2000;14(18):2953–5.
Gutiérrez JP, Sucilla-Pérez H, Conde-González CJ, Izazola JA, Romero-Martínez M, Hernández-Ávila M. Seroprevalencia de VIH en población mexicana de entre 15 y 49 años: resultados de la Ensanut 2012 [Internet]. Salud Pública de México 2014. http://www.redalyc.org/articulo.oa?id=10632372003. Accessed 28 Apr 2017.
Infante C, Sosa-Rubi SG, Cuadra SM. Sex work in Mexico: vulnerability of male, travesti, transgender and transsexual sex workers. Cult Health Sex. 2009;11(2):125–37.
Estrada-Montoya JH, García-Becerra A. Reconfiguraciones de género y vulnerabilidad al VIH/Sida en mujeres transgénero en Colombia. Gerenc Políticas Salud [Internet]. 2010 Jul 1;9(18). http://revistas.javeriana.edu.co/index.php/gerepolsal/article/view/2636. Accessed 28 Apr 2017.
Bockting WO, Robinson BE, Forberg J, Scheltema K. Evaluation of a sexual health approach to reducing HIV/STD risk in the transgender community. AIDS Care. 2005;17(3):289–303.
Ryan C, Russell ST, Huebner D, Diaz R, Sanchez J. Family acceptance in adolescence and the health of LGBT young adults. J Child Adolesc Psychiatr Nurs Off Publ Assoc Child Adolesc Psychiatr Nurses Inc. 2010;23(4):205–13.
Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: implications for public health intervention. Am J Public Health. 2001;91(6):915–21.
Protocols for Hormonal Reassignment of Gender [Internet]. Trans Health. 2012. http://www.trans-health.com/2012/protocols-for-hormonal-reassignment-of-gender/. Accessed 28 Apr 2017.
Colchero MA, Cortés-Ortiz MA, Romero-Martínez M, Vega H, González A, Román R, et al. HIV prevalence, sociodemographic characteristics, and sexual behaviors among transwomen in Mexico City. Salud Pública México. 2015;57:s99–106.
Bockting WO, Robinson BE, Rosser BR. Transgender HIV prevention: a qualitative needs assessment. AIDS Care. 1998;10(4):505–25.
Singer M. Introduction to syndemics: a critical systems approach to public and community health. San Francisco: Jossey-Bass Inc Pub; 2009.
Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–42.
Pitpitan EV, Smith LR, Goodman-Meza D, Torres K, Semple SJ, Strathdee SA, et al. “‘Outness’”as a moderator of the association between syndemic conditions and HIV risk-taking behavior among men who have sex with men in Tijuana, Mexico. AIDS Behav. 2016;20(2):431–8.
Golub SA, Gamarel KE. The impact of anticipated HIV stigma on delays in HIV testing behaviors: findings from a community-based sample of men who have sex with men and transgender women in New York City. AIDS Patient Care STDs. 2013;27(11):621–7.
Ruiz J, Facer M, Ritieni A, Sheppard H. HIV prevalence and risk behaviors among young latino MSM in San Diego, California and Tijuana, Mexico. In: XIV International AIDS Conference; 2002.
Magis-Rodríguez C, Brouwer KC, Morales S, Gayet C, Lozada R, Ortiz-Mondragón R, et al. HIV prevalence and correlates of receptive needle sharing among injection drug users in the Mexican-US border city of Tijuana. J Psychoact Drugs. 2005;37(3):333–9.
Brouwer KC, Strathdee SA, Magis-Rodríguez C, Bravo-García E, Gayet C, Patterson TL, et al. Estimated numbers of men and women infected with HIV/AIDS in Tijuana, Mexico. J Urban Health Bull N Y Acad Med. 2006;83(2):299–307.
Patterson TL, Goldenberg S, Gallardo M, Lozada R, Semple SJ, Orozovich P, et al. Correlates of HIV, sexually transmitted infections, and associated high-risk behaviors among male clients of female sex workers in Tijuana, Mexico. AIDS Lond Engl. 2009;23(13):1765–71.
Pitpitan EV, Goodman-Meza D, Burgos JL, Abramovitz D, Chavarin CV, Torres K, et al. Prevalence and correlates of HIV among men who have sex with men in Tijuana, Mexico. J Int AIDS Soc. 2015;18(1):19304.
Kenagy GP, Hsieh C-M. The risk less known: female-to-male transgender persons’ vulnerability to HIV infection. AIDS Care. 2005;17(2):195–207.
Meier SC, Labuski CM. The Demographics of the Transgender Population. In: Baumle AK, editor. International Handbook on the Demography of Sexuality [Internet]. Springer Netherlands; 2013. pp. 289–327. (International Handbooks of Population). http://springerlink.bibliotecabuap.elogim.com/chapter/10.1007/978-94-007-5512-3_16. Accesed 28 Apr 2017.
Nemoto T, Bödeker B, Iwamoto M. Social support, exposure to violence and transphobia, and correlates of depression among male-to-female transgender women with a history of sex work. Am J Public Health. 2011;101(10):1980–8.
Neilands TB, Steward WT, Choi K-H. Assessment of stigma towards homosexuality in China: a study of men who have sex with men. Arch Sex Behav. 2008;37(5):838.
Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17.
Link BG, Phelan JC. Conceptualizing Stigma. Annu Rev Sociol. 2001;1(27):363–85.
Operario D, Nemoto T, Iwamoto M, Moore T. Unprotected sexual behavior and HIV risk in the context of primary partnerships for transgender women. AIDS Behav. 2011;15(3):674–82.
Coan DL, Schrager W, Packer T. The role of male sexual partners in HIV infection among male-to-female transgendered individuals. Int J Transgenderism. 2005;8(2–3):21–30.
Wiessing LG, van Roosmalen MS, Koedijk P, Bieleman B, Houweling H. Silicones, hormones and HIV in transgender street prostitutes. AIDS Lond Engl. 1999;13(16):2315–6.
Iñiguez-Stevens E, Brouwer KC, Hogg RS, Patterson TL, Lozada R, Magis-Rodriguez C, et al. Estimaciones de Prevalencia del VIH por Género y Grupo de Riesgo en Tijuana, México: 2006. Gac Med Mex. 2009;145(3):189–95.
Patterson TL, Semple SJ, Staines H, Lozada R, Orozovich P, Bucardo J, et al. Prevalence and correlates of HIV infection among female sex workers in two Mexico-U.S. border cities. J Infect Dis. 2008;197(5):728–32.
Setia MS, Lindan C, Jerajani HR, Kumta S, Ekstrand M, Mathur M, et al. Men who have sex with men and transgenders in Mumbai, India: an emerging risk group for STIs and HIV. Indian J Dermatol Venereol Leprol. 2006;72(6):425–31.
Hughes TL, Eliason M. Substance use and abuse in Lesbian, Gay, bisexual and transgender populations. J Prim Prev. 2002;22(3):263–98.
Ramirez-Valles J, Garcia D, Campbell RT, Diaz RM, Heckathorn DD. HIV infection, sexual risk behavior, and substance use among Latino Gay and bisexual men and transgender persons. Am J Public Health. 2008;98(6):1036–42.
Lombardi EL, van Servellen G. Building culturally sensitive substance use prevention and treatment programs for transgendered populations. J Subst Abuse Treat. 2000;19(3):291–6.
Weatherby NL, Needle R, Cesari H, Booth R, McCoy CB, Watters JK, et al. Validity of self-reported drug use among injection drug users and crack cocaine users recruited through street outreach. Eval Program Plan. 1994;17(4):347–55.
James NJ, Bignell CJ, Gillies PA. The reliability of self-reported sexual behaviour. Aids. 1991;5(3):333–6.
Acknowledgements
The authors extend their thanks to the transgender community in Tijuana, as well as to Centro de Servicios SER, A.C where the study took place and providing all the facilities for study procedures for the study data collection and HIV testing. To Gerardo Jara and Katherine Castillo who were the interviewers.
Funding
This study was funded by an AIDS International Training in Research Program (AITRP) 1D43TW008633-01, and preparation of this manuscript was supported by NIDA Mentored Career Development Awards to the senior and fourth author (K01DA036447, K01DA036439).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All of the authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Universidad Autónoma de Baja California Research Ethics Committee in Tijuana and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Salas-Espinoza, K.J., Menchaca-Diaz, R., Patterson, T.L. et al. HIV Prevalence and Risk Behaviors in Male to Female (MTF) Transgender Persons in Tijuana, Mexico. AIDS Behav 21, 3271–3278 (2017). https://doi.org/10.1007/s10461-017-1931-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1931-2