Abstract
HIV-exposed infants born to depressed women may be at risk for adverse developmental outcomes. Half of HIV-infected women in rural South Africa (SA) may suffer from pregnancy-related depression. This pilot study examined the impact of depression in HIV-infected women in rural SA on infant development. Mother-infant dyads (N = 69) were recruited in rural SA. Demographics, HIV disclosure, depression, male involvement, and alcohol use at baseline (18.35 ± 5.47 weeks gestation) were assessed. Male involvement, depression, infant HIV serostatus and development were assessed 12 months postnatally. Half of the women (age = 29 ± 5) reported depression prenatally and one-third reported depression postnatally. In multivariable logistic regression, not cohabiting with their male partner, nondisclosure of HIV status, and postnatal depression predicted cognitive delay; decreased prenatal male involvement predicted delayed gross motor development (ps < 0.05). Assessing pregnancy-related depression among HIV-infected women and infant development and increasing male involvement may reduce negative developmental outcomes among HIV-exposed or infected infants.
Resumen
Los bebés expuestos al VIH, provenientes de mujeres deprimidas, pueden estar a riesgo de resultados adversos en el desarrollo. La mitad de las mujeres infectadas con VIH, en Sudáfrica (SA) rural, pueden sufrir de depresión relacionada con el embarazo. Este estudio piloto examinó el impacto de la depresión en el desarrollo infantil entre mujeres infectadas con VIH en SA rural. Parejas (N = 69) de madre e infante fueron reclutadas en SA rural. Se evaluaron datos demográficos, revelación de estatus de VIH a su pareja masculina, depresión, participación masculina en el embarazo y consumo de alcohol al inicio del estudio (18,35 ± 5,47 semanas de gestación). La participación masculina, depresión, el estatus serológico de VIH y el desarrollo infantil se evaluaron 12 meses postnatalmente. La mitad de las mujeres (edad = 29 ± 5) presentaron depresión prenatal y un tercio depresión postparto. En regresión logística multivariable, no vivir con su pareja, no revelar su estatus de VIH, y depresión postnatal predijeron retraso cognitivo; la disminución de participación masculina durante el embarazo predijo el desarrollo motor grueso retardado (p < 0,05). Evaluar la depresión relacionada con el embarazo entre mujeres infectadas con VIH y el desarrollo infantil; así, como aumentar la participación de las parejas masculinas pudieran reducir los resultados adversos en el desarrollo de niños expuestos a, o infectados por, el VIH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depression during pregnancy is not unusual and occurs in 14–23% of women [1], increasing the risk of post-partum depression [2]. In Africa, 11–36% [3] of women become depressed during pregnancy, and 18–48% post-partum [4,5,6]. In fact, depression during pregnancy is widespread in sub-Saharan Africa, e.g., in a sample drawn from rural South Africa, Mpumalanga Province, about half of pregnant HIV-infected women reported depressed mood [7], compared to an estimated 13–19% in high-income countries [8]. Pregnancy-related depression is associated with several adverse outcomes for women living with HIV (WLHIV) [4, 9,10,11,12,13,14,15] and is likely to be accompanied by social isolation, interpersonal disengagement, decreased male partner involvement during pregnancy, and lower rates of perceived social support by family and friends [7, 16,17,18,19]. In addition to affecting maternal outcomes, maternal depression has been associated with multiple adverse effects for infants, including delayed development, behavioral and emotional problems, preterm birth and low birth weight [4, 20]. In general, children of mothers with pre- and postnatal depression have been found to perform poorly on cognitive assessments [21,22,23,24], display insecure attachment [25], and may exhibit less playfulness and positive affect [8, 26, 27]. In a previous study, teachers reported that boys born to mothers with postpartum depression and low socioeconomic status were more active and distractible, impairing school adjustment [25]. Despite high rates of depression among pregnant WLHIV in South Africa and the risk of its detrimental influence on infant development, the impact of maternal pre- and postnatal depression on infant development has not been examined in that setting.
Infants born to WLHIV are also at increased risk of delayed development, poor stress regulation, lower birth weight and physical growth [4, 28,29,30], which may persist into childhood and adulthood [31,32,33], e.g., delayed cognitive functioning or learning disabilities among uninfected infants and children of HIV-infected mothers [34, 35]. Developmental delays in early infancy have significant implications across the life span. Developmental delay has been associated with the emergence of behavioral problems by age two [36, 37] that may continue through adolescence [38]. Psychopathological trajectories among developmentally delayed children may be exacerbated by maternal depression [39, 40]; early developmental delays have been associated with challenges with employment and independent living in adulthood [41].
A recent meta-analysis on the effect of parent psychopathology on infant outcomes identified only four studies conducted in sub-Saharan Africa [42]. Studies identified in South Africa found no association between postnatal depression and social withdrawal in HIV-infected mother-infant dyads at 10–12 months of age [43]. In other South African studies, postnatal maternal depression predicted externalizing symptoms in 2-year old infants, and was mediated by stunted infant growth [44], and postpartum depression was associated with insecure attachment at 18 months of age, and was mediated by the quality of the infant-mother relationship [45]. Finally, a cross-sectional study in Ethiopia found maternal depression to be associated with delays in most developmental outcomes [46].
This pilot study evaluated the effect of maternal depression on infant development at 12 months of age, assessing cognitive functioning, expressive and receptive communication, and fine and gross motor skills among infant-mother dyads living in Mpumalanga Province, a rural area with one of the highest rates of antenatal HIV in South Africa [47]. The primary study hypothesis was that the combined effect of pre- and post-natal depression would be stronger than pre- or post-natal depression alone. It was anticipated that results could provide guidance for healthcare provider interventions to enhance infant outcomes [48], as well as inform the development of pedagogical approaches to manage developmental delay among infants born to depressed HIV-affected families.
Method
Prior to study onset, ethical approval was obtained from the Department of Health, the Human Sciences Research Council (HSRC) and the University of Miami Miller School of Medicine.
Participants and Procedures
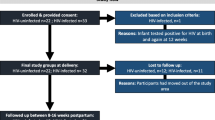
Participants were recruited from an ongoing cluster randomized clinical trial in 12 community health centers (CHCs) in Mpumalanga Province, South Africa aimed at testing the impact of male partner participation during the antenatal and postnatal periods on clinic attendance, medication adherence, and family planning [47]. The current study was retrospectively designed with a cross-sectional add-on follow-up on infant development; a randomly chosen subset of mothers (N = 69) from the larger study were invited to participate with their infants at 12-months of age; all women invited agreed to participate. Participating women for the larger trial and the present study were HIV-infected and at least 18 years of age with an identified male partner. Candidates were enrolled after provision of informed consent. Baseline assessments were completed at 7–21 weeks (M = 18.35 weeks; SD = 5.47) of pregnancy, and 12-months assessments 8–17 months (M = 16.41 months; SD = 2.81) later.
Maternal assessments at baseline and 12-month follow-up were conducted using an Audio Computer Assisted Self Interview system to obtain more accurate reporting of sensitive information in comparison with standard interviewing [49]. All materials for maternal assessments were provided in English and local languages (Sesotho, Zulu) and assessments were approximately 60 min in duration. Blood samples were collected from infants by heel stick and stored as dried blood spots (DBS). Two clinical psychologists from the US trained two assessors in administration of the Bayley Scales of Infant Development-III [50] (BSID-III); training included and role-playing and hands-on practice assessments with infants in the same age range as those in the study. The BSID-III was administered to infant participants in the presence of their mothers. Participants were compensated 100 South African Rand (ZAR; ~ US$10).
Study personnel received advanced training to assist women who self-reported severe depression or thoughts of self-harm, to assess level of risk, and to refer for further assessment, hospitalization, or outpatient treatment, as needed [47]. At all times, CHCs had access to licensed psychiatric nurses and social workers, and were able to contact psychiatrists and clinical psychologists at the district hospital as needed. All women who reported thoughts of self-harm or severe depression were counseled, and a total of n = 16 women were referred for further treatment after evaluation.
Measures
Sociodemographics, and HIV-Related Questions
At baseline, women were asked to self-report on demographic information, such as age, education, income, relationship status including living arrangements with male partner, disclosure of HIV serostatus to the male partner, time since HIV diagnosis, and alcohol use in the past month. Alcohol use was assessed using a dichotomous response to the question “Have you had more than two drinks with alcohol in the past month?”
Infant Development
The BSID-III [50] screening test was used to evaluate five domains of infant development at 12 months of age: cognitive, receptive communication, expressive communication, fine motor, and gross motor skills. The BSID-III has been previously used in South Africa to assess infants at 3, 6, 9, and 12 months of age [51]. An earlier version (second edition) of the BSID has also been used in children of a mean age = 15.8 months in South Africa [52], which was administered by a trained researcher fluent in English and a local language, as in this study. Raw scores were dichotomized into competent or at emerging risk/at risk using standard validated cut-offs [50] to (1) maximize predictive power given the small sample size, (2) use a standard metric across infants, and (3) identify infants who would normally be classified to be at risk in clinical settings and in need of intervention. Neurodevelopmental testing guidelines recommend dichotomization of test scores and also advise against the use of 1-SD cut-offs [53]. The BSID has been previously used in South Africa to assess infants at 3, 6, 9, 12, and 16 months of age without adaptation [52]. In addition, as in previous studies, adaptation or translation of the assessment was not deemed necessary due to the age of the infants and to maximize the generalizability of the findings [30, 54, 55]. Although translation and adaptation of the assessment were not deemed necessary due to the age of the infants, an assessor was available to explain the procedures and translate instructions for the mother as necessary. Assessors were two Bachelor- and Master-degree level research personnel at the HSRC fluent in English and the local languages spoken by the mothers (Sesotho, Zulu); both assessors had extensive assessment and data collection experience in this setting and had worked with the present sample for three years at the time of BSID-III administration. After training, the assessors administered additional practice tests; two licensed clinical psychologists in the US provided ongoing supervision. Two doctoral students in developmental and clinical psychology reviewed scoring for each of the individual assessments to ensure accuracy.
Maternal Depression
Pre- and postnatal depressive symptomatology was assessed at baseline and 12-months, respectively, using the 10-item Edinburgh Postnatal Depression Scale [56], which contains items appropriate to pre-and post-partum depression. Women indicated the frequency of depressive symptoms over the past 7 days. For prenatal depression, baseline scores were used (α = 0.78), and for postnatal depression, 12-month follow-up scores were used (α = 0.74). Continuous depression scores were used as independent variables; for prevalence rates, a cut-point of ≥ 12 was used to define depressive symptoms, as in previous studies in South Africa [57].
Male Involvement
Mother-reported male involvement during pregnancy was measured using an adaptation of the Male Involvement Index, used in previous research in South Africa and Uganda [7, 58], which consisted of 11 items addressing male partner involvement at baseline (antenatal care) and 12-month follow-up (postpartum). Total possible scores range from 0 to 11, with higher scores representing greater male partner involvement. Reliability for this scale was acceptable (α = 0.81). Male involvement was assessed in relation to infant development based on previous research showing that male involvement is associated with decreased risk of developmental delays [64]; as such, it was important to control for this variable when assessing the impact of maternal depression on infant development.
Infant HIV Status
Infant HIV status at 12-months of age was assessed using an HIV polymerase chain reaction (PCR) test. Five drops of blood were obtained from the infant using a sterile lancet and a Guthrie card with five wells. The DBS was collected by trained nursing staff at each study CHC and couriered to an independent laboratory at the University of Cape Town Division of Pharmacology for confirmation of HIV status.
Statistical Analyses
Univariate analyses were used to describe the sample, and 95% confidence intervals (CI) were calculated using 1000 bootstrap samples for prevalence estimates. Bivariate analyses were used to assess bivariate associations between domains of cognitive development (competent or at emerging risk/at risk) and maternal demographic and psychosocial characteristics, as well as depression and infant HIV status.
A series of multivariable logistic regression models were then built to examine cognitive, receptive and expressive communication, and fine and gross motor functioning as outcomes, and pre- and postnatal depression independent variables; all models accounted for the effect of using two trained assessors to administer the BSID-III assessments and infant HIV serostatus. Because infant age and development are closely related as part of natural developmental progression, the inclusion of age as a statistical control was redundant. As such, given the total possible scores for each of the subscales depended on infant age, in months and days, and infant age ranged from 10 to 19 months for this study, raw scores were dichotomized into “competent” versus “at emerging risk”/“at risk for developmental delay”, which allowed all infants to be on the same scale regardless of age [50]. Demographic and psychosocial variables associated with cognitive, receptive and expressive communication, and fine and gross motor development at p < 0.10 in bivariate analyses were also included as independent variables in all models. Additive interactions between pre- and postnatal depression predicting the aforementioned domains of infant development, consistent with the primary study hypothesis, were tested for all models. A cutoff of p < 0.05 was used for statistical significance. Statistical Analysis Software (SAS) v9 was used for all statistical analyses.
Results
Demographic and Psychosocial Characteristics
Women were 19–41 years old (M = 29.23; SD = 5.26). One-third (32%) had completed 12 years of education and had a monthly household income of 1000 ZAR (~ US$100). Two-thirds of women were not married and were not cohabiting with their partner. Women had been diagnosed with HIV for a mean of 34 months (SD = 48.68); 45% were diagnosed with HIV during the current pregnancy, and 59% had disclosed their HIV serostatus to their partner. Male involvement during pregnancy was moderate (M = 6.95; SD = 2.89). Pre- and postnatal depressive symptoms were on average 11.69 (SD = 5.67) and 8.83 (SD = 5.53), respectively. Alcohol use (> 2 drinks) in the past month was reported by 10% of women. At 12 months, 6% [95% CI 1.4, 11.8] (n = 4) of infants (M age = 12.85 months; SD = 2.09) tested positive for HIV using DBS. Further detail of demographic and psychosocial characteristics is in Table 1.
One infant could not complete the expressive communication subscale, and another could not complete the fine motor subscale, resulting in a sample size of 68 infants for these two subscales. Two infants could not complete the gross motor subscale, resulting in a sample size of n = 67 for gross motor functioning. Falling asleep was the primary reason for not completing the full measure.
Prevalence of Maternal Depression and Infant Developmental Delay
At baseline, 45% (n = 31) of women met the criteria for possible prenatal depression. Post-partum, 35% (n = 24) met criteria for possible postpartum depression. At 12 months, 46% (n = 32) of infants were at emerging risk or at risk for cognitive delay, 39% (n = 27) for delayed receptive communication, and 38% (n = 26) for delayed expressive communication. Fine motor skills were delayed in 43% (n = 30) of infants and gross motor functioning was delayed in 51% (n = 35) of infants. A total of n = 19 (28%) infants were delayed on all domains.
Bivariate Associations with Infant Developmental Delay
In bivariate analyses, nondisclosure of HIV serostatus to partner at baseline was associated with risk for cognitive delay at 12-months (p = 0.048). Decreased male involvement during pregnancy was associated with delayed fine motor functioning at 12-months (p = 0.034). Decreased male involvement was associated with delayed gross motor development (p = 0.002). No other bivariate associations were found. Specifically, there were no bivariate associations between pre- and postnatal depression and any of the domains of infant development.
Multivariable Associations with Infant Developmental Delay
In multivariable logistic regression models, after controlling for prenatal depression and infant HIV serostatus, not cohabiting with their male partners (p = 0.028), nondisclosure of HIV serostatus (p = 0.016) at baseline predicted infant cognitive delay, and postnatal depression (p = 0.038) was associated with infant cognitive delay at 12 months. Controlling for relationship status, prenatal depression, and infant HIV serostatus, decreased male involvement during pregnancy predicted gross motor developmental delay at 12-months (p = 0.003). No associations were found for receptive and expressive communication. Additive interactions between pre- and postnatal depression were tested to examine whether excess risk was conferred by the presence of both pre- and postnatal depression, though all interaction terms were non-significant (ps > 0.180). Multivariable model summaries can be found in Table 2.
Discussion
This pilot study evaluated the effect of maternal depression on infant development at 12 months of age, and assessed cognitive functioning, expressive and receptive communication, and fine and gross motor skills among infant-mother dyads living in rural South Africa. Overall, lack of male involvement during pregnancy and not cohabiting with partners predicted delays in infant cognitive functioning, gross motor development and receptive communication; there was also an association between postnatal depression and delayed cognitive development. Contrary to our hypothesis, the combined effect of pre- and post-natal depression did not appear to confer additional risk for developmental delays beyond that of pre- or post-natal depression alone.
One-third of women participating reported depression post-partum, which was associated with cognitive delay in infants, supplementing previous research among HIV uninfected women [21,22,23]. The impact of parental psychopathology on child developmental outcomes has been widely documented [42]. Prenatal depression, though more prevalent than postnatal depression (45%) in this sample, did not appear to influence cognitive development. Though previous studies in sub-Saharan Africa have not assessed the impact of prenatal depression on infant development [43,44,45,46], studies in Greece [59], United States, and United Kingdom [60] have found associations between prenatal depression and developmental delays, whereas other studies have not found an association [61, 62]. Because recruitment was conducted at an antenatal clinic, nearly half of the women were diagnosed with HIV at the time of recruitment and assessment of prenatal depression, which may explain the greater prevalence of depression prenatally; rates of depression are the highest immediately following diagnosis [63]. As such, symptoms of depression for some women may have subsided by the 12-month assessment, given that there was a gap of more than one year between the pre- and post-natal assessment. Furthermore, while most women reported having disclosed their HIV status to their partners, partner participation in pregnancy was modest. In this sample, decreased male involvement during pregnancy predicted gross motor developmental delay at 12-months—the beneficial effect of male involvement has been reported in other settings and contexts [64]. In a systematic review of the literature, frequent, active paternal engagement predicted a variety of positive infant incomes, including enhanced cognitive development, as well as decreased rates of externalizing disorders later in life [64].
Limitations
A number of limitations must be considered when interpreting these findings. The small sample size limits generalizability to other populations and does not allow us to assess more complex causal patterns using more advanced statistical techniques, such as structural equation modeling. A small sample may also be subject to finite sample bias. There may be other important predictors, moderators, and mediators affecting infant development not assessed that could have unveiled more complex relationships and pathways between depression and infant development. All infants were exposed to HIV, and as such, were all at risk for developmental delays, which may account for the high prevalence of delays in this sample [28]. Finally, depression was assessed via self-report and may have been underreported, although a computerized system was used to reduce bias in self-report [65].
Future Research and Recommendations
As the biological mechanisms associated with prenatal depression, e.g., dysregulation of dopamine, serotonin, cortisol, norepinephrine [24], as well as lifestyle factors, e.g., smoking, alcohol use, diet [66] have previously been associated with cognitive delays, future research should also address reducing the impact of prenatal depression, targeting its intensity and duration [66] in HIV-infected women. Given the greater prevalence of prenatal depression compared to postnatal depression (45 vs. 35%), research should also examine the relative impact of HIV and depression and the longitudinal course of infant development among depressed HIV-infected and uninfected mothers [67], as well as the role of tailored clinical interventions for post-partum depression.
Public health initiatives to increase the cultural acceptability of male involvement in pregnancy may be an important step in reducing the vulnerability of infants to suboptimal developmental outcomes. Promotion of male involvement in antenatal care programs should be maintained, and strategies to integrate “men friendly” antenatal and postnatal services may thereby improve neonatal development outcomes. Interventions to decrease depression in pregnant HIV-infected women, such as cognitive behavioral therapy [4] and increase male partner involvement [67] could also be applied to enhance infant developmental outcomes.
Conclusions
This pilot study highlighted the high prevalence of maternal depression among women living in rural South Africa and the risk of infant developmental delays. The importance of training healthcare providers to assess ante- and post-natal depression in HIV-infected women is apparent [48, 68], and the need for tailored pedagogical approaches to manage developmental delay that may arise among infants merits intervention. Programs to support the mental health of HIV-infected women pre-and post-partum represent an important opportunity to optimize infant health outcomes in rural South Africa.
References
Yonkers KA, Wisner KL, Stewart DE, Oberlander TF, Dell DL, Stotland N, et al. The management of depression during pregnancy: a report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Gen Hosp Psychiatry. 2009;31(5):403–13.
Roehr B. American Psychiatric Association explains DSM-5. BMJ. 2013;346:f3591.
Natamba B, Achan J, Arbach A, Oyok T, Ghosh S, Mehta S, et al. Reliability and validity of the center for epidemiologic studies-depression scale in screening for depression among HIV-infected and-uninfected pregnant women attending antenatal services in northern Uganda: a cross-sectional study. BMC psychiatry. 2014;14(1):1.
Stringer EM, Meltzer-Brody S, Kasaro M, Stuebe AM, Wiegand S, Paul R, et al. Depression, pregnancy, and HIV: the case to strengthen mental health services for pregnant and post-partum women in sub-Saharan Africa. Lancet Psychiatry. 2014;1(2):159–62.
Dow A, Dube Q, Pence BW, Van Rie A. Postpartum depression and HIV infection among women in Malawi. Jaids-J Acq Imm Def. 2014;65(3):359–65.
Sawyer A, Ayers S, Smith H. Pre- and postnatal psychological wellbeing in Africa: a systematic review. J Affect Disorders. 2010;123(1–3):17–29.
Peltzer K, Rodriguez VJ, Jones D. Prevalence of prenatal depression and associated factors among HIV-positive women in primary care in Mpumalanga province, South Africa. Sahara J-J Soc Asp H. 2016;13(1):60–7.
O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psycho. 2013;9:379–407.
Ammassari A, Antinori A, Aloisi MS, Trotta MP, Murri R, Bartoli L, et al. Depressive symptoms, neurocognitive impairment, and adherence to highly active antiretroviral therapy among HIV-infected persons. Psychosomatics. 2004;45(5):394–402.
French AL, Gawel SH, Hershow R, Benning L, Hessol NA, Levine AM, et al. Trends in mortality and causes of death among women with HIV in the US: a ten-year study. J Acquir Immune Defic Syndr. 2009;51(4):399–406.
Ickovics JR, Reed E, Magriples U, Westdahl C, Schindler Rising S, Kershaw TS. Effects of group prenatal care on psychosocial risk in pregnancy: results from a randomised controlled trial. Psychol Health. 2011;26(2):235–50.
Kapetanovic S, Christensen S, Karim R, Lin F, Mack WJ, Operskalski E, et al. Correlates of perinatal depression in HIV-infected women. AIDS Patient Care STDS. 2009;23(2):101–8.
Nachega JB, Mutamba B, Basangwa D, Nguyen H, Dowdy DW, Mills EJ, et al. Severe mental illness at ART initiation is associated with worse retention in care among HIV-infected Ugandan adults. Trop Med Int Health. 2013;18(1):53–7.
Turner BJ, Hecht FM. Improving on a coin toss to predict patient adherence to medications. Ann Intern Med. 2001;134(10):1004–6.
Levine AB, Aaron EZ, Criniti SM. Screening for depression in pregnant women with HIV infection. J Reprod Med. 2008;53(5):352–6.
Blaney NT, Fernandez MI, Ethier KA, Wilson TE, Walter E, Koenig LJ, et al. Psychosocial and behavioral correlates of depression among HIV-infected pregnant women. Aids Patient Care St. 2004;18(7):405–15.
Bonacquisti A, Geller PA, Aaron E. Rates and predictors of prenatal depression in women living with and without HIV. Aids Care. 2014;26(1):100–6.
Casale M, Wild L, Cluver L, Kuo C. Social support as a protective factor for depression among women caring for children in HIV-endemic South Africa. J Behav Med. 2015;38(1):17–27.
Davies T, Schneider M, Nyatsanza M, Lund C. “The sun has set even though it is morning”: experiences and explanations of perinatal depression in an urban township, Cape Town. Transcult Psychiatry. 2016;53(3):286–312.
Van den Bergh BR, Mulder EJ, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: links and possible mechanisms, A review. Neurosci Biobehav Rev. 2005;29(2):237–58.
Kingston D, McDonald S, Austin MP, Tough S. Association between prenatal and postnatal psychological distress and toddler cognitive development: a systematic review. PLoS ONE. 2015;. doi:10.1371/journal.pone.0126929.
Murray L, Fiori-Cowley A, Hooper R, Cooper P. The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Dev. 1996;67(5):2512–26.
Murray L, Kempton C, Woolgar M, Hooper R. Depressed mothers speech to their infants and its relation to infant gender and cognitive-development. J Child Psychol Psyc. 1993;34(7):1083–101.
Field T. Prenatal depression effects on early development: a review. Infant Behav Dev. 2011;34(1):1–14.
Sinclair D, Murray L. Effects of postnatal depression on children’s adjustment to school—teacher’s reports. Brit J Psychiat. 1998;172:58–63.
O’Hara MW. Postpartum depression: what we know. J Clin Psychol. 2009;65(12):1258–69.
Goodman S, Brand S, Hammen C. Maternal depression and infant mental health. Handbook of depression and its treatment. 2nd ed. New York: Guilford; 2008. p. 249–76.
Dobrova-Krol NA, van IJzendoorn MH, Bakermans-Kranenburg MJ, Juffer F. Effects of perinatal HIV infection and early institutional rearing on physical and cognitive development of children in Ukraine. Child Dev. 2010;81(1):237–51.
Le Doare K, Bland R, Newell ML. Neurodevelopment in children born to HIV-infected mothers by infection and treatment status. Pediatrics. 2012;130(5):E1326–44.
Whitehead N, Potterton J, Coovadia A. The neurodevelopment of HIV-infected infants on HAART compared to HIV-exposed but uninfected infants. Aids Care. 2014;26(4):497–504.
O’Connor TG, Heron J, Glover V, Team AS. Antenatal anxiety predicts child behavioral/emotional problems independently of postnatal depression. J Am Acad Child Psy. 2002;41(12):1470–7.
Buss C, Davis EP, Hobel CJ, Sandman CA. Maternal pregnancy-specific anxiety is associated with child executive function at 6–9 years age. Stress. 2011;14(6):665–76.
van den Berg S, Shapiro DA, Bickerstaffe D, Cavanagh K. Computerized cognitive-behaviour therapy for anxiety and depression: a practical solution to the shortage of trained therapists. J Psychiatr Ment Health Nurs. 2004;11(5):508–13.
Mellins CA, Kang E, Leu CS, Havens JF, Chesney MA. Longitudinal study of mental health and psychosocial predictors of medical treatment adherence in mothers living with HIV disease. AIDS Patient Care STDS. 2003;17(8):407–16.
Talge NM, Neal C, Glover V, Early Stress TR, Prevention Science Network F Neonatal Experience on C, et al. Antenatal maternal stress and long-term effects on child neurodevelopment: how and why? J Child Psychol Psychiatry. 2007;48(3–4):245–61.
Emerson E, Einfeld S. Emotional and behavioural difficulties in young children with and without developmental delay: a bi-national perspective. J Child Psychol Psychiatry. 2010;51(5):583–93.
Feldman M, Hancock C, Rielly N, Minnes P, Cairns C. Behavior problems in young children with or at risk for developmental delay. J Child Fam Stud. 2000;9(2):247–61.
Sheeber L, Davis B, Hops H. Gender-specific vulnerability to depression in children of depressed mothers. Children of depressed parents: Mechanisms of risk and implications for treatment. 2002:253–74.
Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. 2011;14(1):1–27.
Hauser-Cram P, Woodman AC. Trajectories of internalizing and externalizing behavior problems in children with developmental disabilities. J Abnorm Child Psychol. 2016;44(4):811–21.
Lowe K, Allen D, Jones E, Brophy S, Moore K, James W. Challenging behaviours: prevalence and topographies. J Intellect Disabil Res. 2007;51(Pt 8):625–36.
Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800–19.
Hartley C, Pretorius K, Mohamed A, Laughton B, Madhi S, Cotton MF, et al. Maternal postpartum depression and infant social withdrawal among human immunodeficiency virus (HIV) positive mother-infant dyads. Psychol Health Med. 2010;15(3):278–87.
Avan B, Richter LM, Ramchandani PG, Norris SA, Stein A. Maternal postnatal depression and children’s growth and behaviour during the early years of life: exploring the interaction between physical and mental health. Arch Dis Child. 2010;95(9):690–5.
Tomlinson M, Cooper P, Murray L. The mother-infant relationship and infant attachment in a south African peri-urban settlement. Child Dev. 2005;76(5):1044–54.
Hadley C, Tegegn A, Tessema F, Asefa M, Galea S. Parental symptoms of common mental disorders and children’s social, motor, and language development in sub-Saharan Africa. Ann Hum Biol. 2008;35(3):259–75.
Jones D, Peltzer K, Weiss SM, Sifunda S, Dwane N, Ramlagan S, et al. Implementing comprehensive prevention of mother-to-child transmission and HIV prevention for South African couples: study protocol for a randomized controlled trial. Trials. 2014;15:417.
Kershaw TS, Magriples U, Westdahl C, Rising SS, Ickovics J. Pregnancy as a window of opportunity for HIV prevention: effects of an HIV intervention delivered within prenatal care. Am J Public Health. 2009;99(11):2079–86.
Metzger DS, Koblin B, Turner C, Navaline H, Valenti F, Holte S, et al. Randomized controlled trial of audio computer-assisted self-interviewing: utility and acceptability in longitudinal studies. HIVNET Vaccine Preparedness Study Protocol Team. Am J Epidemiol. 2000;152(2):99–106.
Bayley N, Reuner G. Bayley scales of infant and toddler development: Bayley-III: Harcourt Assessment. Tex: Psych. Corporation San Antonio; 2006.
Rademeyer V, Jacklin L. A study to evaluate the performance of black South African urban infants on the Bayley Scales of Infant Development III. S. Afr. J Child Health. 2013;7(2):54–9.
Ferguson G, Jelsma J. The prevalence of motor delay among HIV infected children living in Cape Town, South Africa. Int J Rehabil Res. 2009;32(2):108–14.
Marlow N. Measuring neurodevelopmental outcome in neonatal trials: a continuing and increasing challenge. Arch Dis Child Fetal Neonatal Ed. 2013;98:F554–8.
Hutchings J, Potterton J. Developmental delay in HIV-exposed infants in Harare, Zimbabwe. Vulnerable Children Youth Stud. 2014;9(1):43–55.
Van Rie A, Mupuala A, Dow A. Impact of the HIV/AIDS epidemic on the neurodevelopment of preschool-aged children in Kinshasa, Democratic Republic of the Congo. Pediatrics. 2008;122(1):e123–8.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression—development of the 10-Item Edinburgh postnatal depression scale. Brit J Psychiat. 1987;150:782–6.
Lawrie TA, Hofmeyr GJ, de Jager M, Berk M. Validation of the Edinburgh postnatal depression scale on a cohort of South African women. S Afr Med J. 1998;88(10):1340–4.
Byamugisha R, Tumwine JK, Semiyaga N, Tylleskar T. Determinants of male involvement in the prevention of mother-to-child transmission of HIV programme in Eastern Uganda: a cross-sectional survey. Reprod Health. 2010;7.
Koutra K, Chatzi L, Bagkeris M, Vassilaki M, Bitsios P, Kogevinas M. Antenatal and postnatal maternal mental health as determinants of infant neurodevelopment at 18 months of age in a mother-child cohort (Rhea Study) in Crete, Greece. Soc Psych Psych Epid. 2013;48(8):1335–45.
Barker ED, Jaffee SR, Uher R, Maughan B. The Contribution of prenatal and postnatal maternal anxiety and depression to child mal adjustment. Depress Anxiety. 2011;28(8):696–702.
Korhonen M, Luoma I, Salmelin R, Tamminen T. A longitudinal study of maternal prenatal, postnatal and concurrent depressive symptoms and adolescent well-being. J Affect Disorders. 2012;136(3):680–92.
Peltzer, K., Mlambo, M., Matseke, M. G., Shikwane, E., Louw, J., & Kekana, Q. (2011). Report on PMTCT comprehensive community intervention package including male involvement, infant follow-up, peer support, partner violence and infant feeding in Nkangala District, Mpumalanga province.
Olley BO, Seedat S, Nei DG, Stein DJ. Predictors of major depression in recently diagnosed patients with HIV/AIDS in South Africa. AIDS Patient Care STDS. 2004;18(8):481–7.
Sarkadi A, Kristiansson R, Oberklaid F, Bremberg S. Fathers’ involvement and children’s developmental outcomes: a systematic review of longitudinal studies. Acta Paediatr. 2008;97(2):153–8.
Rhodes KV, Lauderdale DS, He T, Howes DS, Levinson W. “Between me and the computer”: increased detection of intimate partner violence using a computer questionnaire. Ann Emerg Med. 2002;40(5):476–84.
Lewis AJ, Austin E, Knapp R, Vaiano T, Galbally M. Perinatal maternal mental health, fetal programming and child development. Healthcare (Basel). 2015;3(4):1212–27.
Aluisio AR, Bosire R, Bourke B, Gatuguta A, Kiarie JN, Nduati R, et al. Male partner participation in antenatal clinic services is associated with improved HIV-free survival among infants in Nairobi, Kenya: a Prospective Cohort Study. Jaids-J Acq Imm Def. 2016;73(2):169–76.
Crozier SR, Robinson SM, Borland SE, Godfrey KM, Cooper C, Inskip HM, et al. Do women change their health behaviours in pregnancy? Findings from the Southampton Women’s Survey. Paediatr Perinat Epidemiol. 2009;23(5):446–53.
Acknowledgements
This study was funded by a collaborative NIH/PEPFAR grant, R01HD078187-S. Activities were conducted with the support of the University of Miami Miller School of Medicine Center for AIDS Research, funded by an NIH grant, P30AI073961.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Rodriguez, V.J., Matseke, G., Cook, R. et al. Infant Development and Pre- and Post-partum Depression in Rural South African HIV-Infected Women. AIDS Behav 22, 1766–1774 (2018). https://doi.org/10.1007/s10461-017-1925-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1925-0