Abstract
Internalized stigma and disclosure concerns are key elements for the study of mental health in people living with HIV. Since no measures of these constructs were available for Spanish population, this study sought to develop such instruments, to analyze their reliability and validity and to provide a short version. A heterogeneous sample of 458 adults from different Spanish-speaking countries completed the HIV-Internalized Stigma Scale and the HIV-Disclosure Concerns Scale, along with the Hospital Anxiety and Depression Scale, Rosenberg’s Self-esteem Scale and other socio-demographic variables. Reliability and correlation analyses, exploratory factor analyses, path analyses with latent variables, and ANOVAs were conducted to test the scales’ psychometric properties. The scales showed good reliability in terms of internal consistency and temporal stability, as well as good sensitivity and factorial and criterion validity. The HIV-Internalized Stigma Scale and the HIV-Disclosure Concerns Scale are reliable and valid means to assess these variables in several contexts.
Resumen
El Estigma Internalizado y el Miedo a Comunicar el Diagnóstico son clave para el estudio de la salud mental en personas con VIH. Dado que no existían herramientas para evaluarlos en población española, el propósito de este estudio fue desarrollar tales escalas, analizar su fiabilidad y validez y proporcionar una versión abreviada. Una muestra heterogénea de 458 adultos de diferentes países hispanoparlantes completaron la Escala de Estigma Internalizado-VIH y la Escala de Miedo a Comunicar el Diagnóstico-VIH, junto con la Hospital Anxiety and Depression Scale, la Escala de Autoestima de Rosenberg y otras variables socio-demográficas. Para evaluar las propiedades psicométricas de las escalas desarrolladas, se realizaron análisis de fiabilidad, correlacionales y factoriales exploratorios, así como modelos de rutas con variables latentes y ANOVAs. Las escalas mostraron buena fiabilidad en términos de consistencia interna y estabilidad temporal, así como buena sensibilidad y validez factorial y referida a criterio. La Escala de Estigma Internalizado-VIH y la Escala de Miedo a Comunicar el Diagnóstico-VIH constituyen medios fiables y válidos para evaluar estas variables en diferentes contextos.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although HIV infection is now conceptualized as a manageable chronic condition rather than a death sentence [1–3], People Living with HIV (PLH) are still more likely to experience depression, suicidal ideation, stress, stigma, isolation, and marginalization [4]. Furthermore, they are more likely to experience discrimination than those with other chronic conditions [5]. Social stigma and fear of HIV disclosure are often key challenges for PLH [6–10], thus it is necessary to have adequate assessment procedures to measure these constructs and prevent their effects. Since there were no assessment instruments for the measurement of HIV internalized stigma and disclosure concerns available for the Spanish population, the main objective of this study was to develop and validate such assessment instruments. First, however, we will clarify the meaning and importance of these constructs and review the availability and adequacy of existing instruments.
HIV Stigma Constructs
HIV stigma refers to the socially constructed and shared knowledge about the devalued status of PLH, who as a result are subject to prejudice, discounting, discrediting, and discrimination [11]. It is based on the view that the individual is responsible for contracting the virus, which is regarded as fatal, highly contagious and eventually leading to significant physical decline and sometimes death [12]. HIV stigma can manifest itself at the structural, the societal and the individual levels; the latter level is where explicit biases have decreased but more subtle forms of stigma persist [13].
HIV stigma has recently been conceptualized as a fundamental cause of health inequalities [9], as it influences the resources, conditions, social relationships, coping strategies and self-esteem of PLH, which in turn can lead to poorer health outcomes. Studies show a relationship between high HIV stigma and less involvement in HIV counseling, delayed health care seeking, lower treatment adherence, faster disease progression and poorer mental health (e.g., depression, lower satisfaction with life) [14–20]. There are mixed results regarding gender differences in stigma [11, 22], and a tendency to decrease has been found as the years living with HIV, the years on antiretroviral therapy (ART) and age increase; similarly, lower levels in stigma are associated with having a high school graduation or greater and being currently employed [21].
The construct of stigma is complex, and a variety of types of stigma are defined in the literature [19, 22]. From the perspective of the HIV-negative person, stigma can be either perceived or enacted, whereas from the PLH perspective it can be internalized, perceived and experienced [23]. Although our study will focus on internalized stigma, we will first define experienced and perceived stigma for clarification.
Experienced stigma (ES) refers to the personal experience of stigma (i.e., experiences of prejudice, stereotyping, and discrimination) and thus involves interpersonal actions. Perceived or felt stigma (FS) concerns the subjective awareness of stigma in the society or local community [11, 24, 25]. Logically, PLH experiencing a high degree of FS would be more likely to protect themselves against possible ES by means of disclosure avoidance [11]. It is not surprising, then, that although FS is widely commonplace, ES is considerably less prevalent [3, 13].
Internalized Stigma
Internalized HIV stigma (IS), also called self-stigma, represents the devaluation and discredit of oneself based on one’s stigma [14]. It is regarded as a process “in which stigmatized persons accept the negative views that others in society hold about them and incorporate those views into their self-concept” [19]. IS is characterized by negative feelings about the self, identity transformation and maladaptive behavior, which stem from the person’s experiences, perceptions or anticipation of negative social reactions [26]. A higher degree of IS indicates a tendency to feel guilty, accept stigmatization from others and justify their discriminatory behaviors [13]. Although IS is theoretically closely related to FS, the correlation between them is only moderate, suggesting they are different aspects or dimensions of stigma [19].
It has been claimed that IS may have even more severe consequences than FS or ES [19, 27, 28], as depression is related to IS but not to actual experienced discrimination [22] and those who experienced ES have a good quality of life, as opposed to those with a higher IS [13]. Additionally, IS is associated with anxiety, guilt, shame, worthlessness, hopelessness, embarrassment, suicidal thoughts and low self-esteem, as well as with substance abuse, poor social support, social isolation, poorer adherence to treatment, low psychological, physical, social and environmental quality of life, faster disease progression and risky sexual behavior [3, 12, 17, 18, 20, 27, 29–32]. Moreover, IS tends to be higher among men in general [11], the recently diagnosed and those who have not attended an HIV-related support group or activities [12], since support groups help deal with stigma in a multidimensional way, decrease social isolation and feelings of shame and provide opportunities for disclosure rehearsal [28]. These findings highlight the importance of considering IS both in research and in clinical settings.
Disclosure Concerns
Disclosure concerns (DC) are highly related to stigma in general [1, 33], and more specifically have been theorized to constitute the basis of FS and IS [11]; thus, receiving support after disclosure of serostatus plays a key role in the reduction of stigma. Another approach [22] suggests that FS is likely to internalize if there is a lack of social support, implying that a higher level of social support reduces social isolation, which in turn decreases DC. A third approach suggests that IS hinders disclosure, which in turn reduces received support [3]. To our understanding, it is possible that all the aforementioned processes occur, perhaps in different phases or stages. For example, it could be that felt normative stigma is learned in the form of vicarious stigma (e.g., listening to other people’s comments, jokes or stories) [11], establishing the basis for IS and DC. Depending on the person’s experiences and personality characteristics, a higher internalization of stigma may happen, leading to higher DC. Also, positive disclosure experiences (e.g., no rejection, receiving support) may reduce levels of FS, IS and DC. This model involves a complex flux of influences that work in several directions.
It is important to note that DC, although related to stigma, are not limited only to those who have experienced ES, but constitute a protective response for PLH regardless of their actual experiences of stigma [13], are related to treatment adherence [32] and can accelerate the pace of HIV/AIDS [28]. Not only are DC related to IS and depression [34], but they also fully mediate the relationship between FS and depression, and partially mediate the association between IS and depression [11]; the same work highlights the fact that providing support to PLH for disclosure of their serostatus is essential to reduce stigma. Reducing DC and stigma, in turn, would lead to improved physical and mental health outcomes for PLH, an essential objective in the field of Health Psychology.
HIV Stigma Measures
Valid and reliable instruments for measuring HIV stigma and DC are needed in order to develop interventions for stigma reduction and to evaluate the effects of such interventions [35]. A review of the HIV literature during the past 15 years reveals studies in which some effort has been made regarding definition and differentiation of IS and DC constructs [11, 13, 19], but a lack of clarity remains, and measures often include items which refer to related but different stigma concepts. For example, Kingori et al.’s Felt Stigma Scale [22] was intended to measure FS but the content of its items also resembles ES, as two of the factors that emerged show: Ostracizing and Discrimination. The Van Rie HIV/AIDS-related Stigma Scales are another example: comprising 20 items and validated in Thailand [36] and the USA [37], they do not take into account the different stigma types and fail to represent IS and DC. Although the authors included content related to shame, guilt and disclosure, the phrasing of the items provided two FS subscales: one for the community perspective and one for AIDS patients’ perspective.
Something similar happens in stigma measures specifically designed to measure IS and DC. For instance, Sayles et al.’s 28-item IS scale includes items that refer to general stereotypes held by society (FS), DC, and experienced discrimination (ES). The only domain that measures IS as defined here was an unexpected dimension labeled self-acceptance, and most of those items referred to DC and the degree to which one’s family is comfortable talking about HIV [38].
The HIV Stigma Scale, which has been validated in the USA [25, 39], the Netherlands [40], Canada [21] and Sweden [35], is another example. It includes an eight-item DC subscale and a seven-item negative self-image (IS) subscale, both with item content we deem appropriate. However, it was supposed to measure perceived stigma (FS). Indeed, when adapted for Spanish-speaking Latino populations in Peru [41], Dominican Republic [42] and Puerto Rico [43], it was renamed the HIV Felt-Stigma Scale, although it still comprised factors related to ES, DC and IS. We aim to clarify the extant confusion and elucidate specific factors of stigma in our own scale development.
Kalichman et al.’s Internalized AIDS-Related Stigma Scale [29] constitutes a good and important effort towards IS assessment, as the construct is well defined and delimited. It is a six-item measure initially validated with populations in South Africa, Swaziland and the USA, and was later validated with populations in Uganda [44] and Ireland [45]. Four of its items clearly measure IS, but the other two (“It is difficult to tell people about my HIV infection”, “I hide my HIV status from others”) could be assessing DC or FS, as difficulty to disclose or disclosure avoidance can stem from a high degree of FS. That is, a person could live in a highly stigmatizing environment and therefore have a high level of FS and try not to disclose, despite their actual degree of IS. The Internalized Stigma of AIDS Tool (ISAT) consists of 10 items and was validated in the USA [19]. This scale also includes items that do not necessarily measure IS (e.g., “I feel like I have to hide my illness”, “I try to hide that I have HIV”), but could be measuring DC or FS.
Other measures have more accurately clarified the IS construct. For example, the HIV/AIDS Stigma Instrument-PLWA (HASPI-P), validated in African settings [33], includes a 5-item subscale named ‘negative self-perception’ that we believe represents IS with clarity, as does Steward’s et al. 10-item Internalized stigma scale [11], designed for an Indian population.
Apart from the widespread lack of construct clarity, there are other problems with some of these stigma measures. A recent review of IS measures by Stevelink et al. [46] found problems regarding internal consistency, reliability, construct and criterion validity, interpretability, responsiveness, and floor and ceiling effects. When scale authors have addressed these matters, either the results have not been good (e.g., low reliability coefficients) or the procedures have not been appropriate (e.g., sample not large enough for factor analysis) (see the review for specific information).
Only the HIV Stigma Scale has been adapted for a Spanish-speaking population in three Latino contexts—Peru [41], Dominican Republic [42], and Puerto Rico [43]—, and we have mentioned the limitations of this scale. To our knowledge, there are no IS and DC scales available for Spanish-speaking populations in Spain and Latin America. Thus the objective of this study was to develop and ascertain the psychometric properties of two measures, one for IS and one for DC, in Spanish and Latin American populations.
Study Objectives and Hypotheses
In developing this study, we considered a few key issues. The first issue is that the experience of HIV stigma can vary across cultures [11]. Thus cultural adaptation of the scales was important to ensure content validity [22, 46]. Secondly, consideration was given with regard to the research and clinical contexts in which this scale might be given. Thus efforts, were made to minimize participant/patient burden [40]. Thirdly, since different types of stigma have different consequences for PLH [11] it is important to distinguish between them in research [22]. We resolved to design two different measures but, resulting from the lack of construct clarity present in the literature, we decided to initially treat them as one with regard to factor analyses. We then planned to ascertain if, as we think, they are different but related constructs or if, conversely, they are one construct. Lastly, we followed the recommendation to use measures of related constructs to ascertain construct validity [22], and thus we included anxiety, depression and self-esteem measures in our study, all of which have been widely used for validation purposes (e.g., [24, 30, 32, 35]).
From the previous objectives and considerations, the following hypotheses are derived:
H1
The IS and DC scales will be shown to be different constructs, although positively related. We expect a moderate Pearson correlation between IS and DC of r = .40–.60 [25, 38, 39, 41, 43].
H2
The IS and DC scales will be positively related to depression and anxiety and negatively related to self-esteem. We expect a higher correlation of depression to IS (around r = .30–60) than to DC (around r = .0–25), as previously found in literature [11, 19, 29, 41–44], and we predict a similar correlation will occur with anxiety. Self-esteem will similarly have a higher negative correlation to IS (around r = .40–.60) than to DC (expected to be non-significant or below r = .25) [25, 39, 42].
H3
The IS and DC scales will be sensitive to gender, age, time since diagnosis, educational level, nationality, connection to an HIV-related NPO, treatment status (i.e., on ART treatment or not) and treatment adherence. Much like the extant literature, we expect that the IS and DC scales will correlate negatively with age and time since diagnosis, and that those with secondary education or higher, who have a connection to an Non-Profit Organization (NPO), who are on treatment and who have good treatment adherence will have a lower degree of IS and DC. We expect cultural differences to emerge [32] but since they have not been explored among these cultures, we cannot be more specific.
Methods
Participants
A total of 458 participants were assessed during this validation study. The sample was obtained by a snowball approach. Eighty-four local and national associations and groups from Spanish-speaking countries were contacted online and asked to distribute information about the study and a link for participation through their online social networks. In order to complete the questionnaire, the participants first had to read the information page (in which they were provided information about the research and the confidentiality of their answers) and click on the acceptance button.
The descriptive statistics of the sample can be found in Table 1. Most of the participants were male, homosexual, Spanish, single, with a University degree, employed and reported little economic difficulty in coping with HIV. The majority had acquired the virus by means of sexual activity, were taking HIV medication, and did not have any connection to a NPO. The mean age was 36.6 years (SD = 10.3; range 18–75 years) and the mean time since HIV diagnosis was 78.9 months (SD = 87.21; range 1–360).
Instruments
HIV Internalized Stigma Scale (HIV-ISS)
This scale, developed for this study, is a self-report instrument in Spanish language that evaluates the level of internalized stigma related to HIV during the last month, and consists of 10 items with a 5-point response scale (1 = never or nearly ever, 2 = seldom, 3 = sometimes, 4 = frequently, 5 = all or almost all the time). The total score of the HIV-ISS is obtained by adding the 10 item scores, and ranges from 10 to 50. A higher score indicates a higher level of perceived internalized stigma. An English translation of the HIV-ISS scale is presented in Appendix 1, and the original Spanish scale is available from the authors upon request.
HIV Disclosure Concerns Scale (HIV-DCS)
This measure, developed for this study, is a self-report instrument in Spanish language designed to assess the level of HIV-related disclosure concerns, and consists of 10 items with a 5-point response scale (1 = very little, 2 = a little, 3 = somewhat, 4 = much, 5 = a great deal). The total score is obtained by adding the 10 item scores, and ranges from 10 to 50. A higher score indicates a higher level of disclosure concerns. An English translation of the HIV-DCS is presented in Appendix 2, and the original Spanish scale is available from the authors upon request.
Hospital Anxiety and Depression Scale (HADS; [47])
This self-report measure is comprised of 14 items with a 4-point Likert-type scale (0–3), which form two 7-item subscales, one for anxiety (HADS-A) and one for depression (HADS-D). The scores of the Spanish version [48] have shown adequate psychometric properties in different Spanish populations [49–52], such as fibromyalgia patients [49, 52] and has proven to be a good screening instrument to assess anxiety and depression [50]. Cronbach’s alpha in the current sample was .88 for the HADS-A and .87 for the HADS-D.
Rosenberg Self-Esteem Scale (RSE; [53])
This measure contains 10 items related to feelings of self-respect and self-acceptance with a Likert-type scale response format from 1 to 4. Half of the items are negatively worded. It has been validated in Spanish in a variety of clinical samples [54] and in University students [55], showing adequate psychometric properties. Cronbach’s alpha in the current sample was .86.
Sociodemographic Variables
Participants provided information on gender (male/female/other), age, nationality, time since HIV diagnosis (years and months), sexual orientation (homosexual/bisexual/heterosexual/other), educational level, employment status (and if unemployed, the reason), occupation, relationship status (living with partner was considered equal to married) and economic difficulty in coping with HIV infection. Participants were also asked about means of HIV transmission (sexual/syringe or similar/blood transfusion or mother-to-child/other or don’t know) and if they had connections with an HIV+ NPO. Lastly, participants indicated whether they were taking HIV medication and, if so, daily dosage and doses skipped in the last month, so as to measure treatment adherence.
Procedures
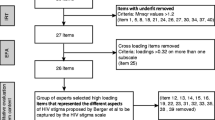
We designed a correlational transversal study that was approved by the authors’ University ethical committee. In order to develop the two initial instruments and to ensure their content validity, we reviewed the current literature on IS and DC, focusing on items that encompass these constructs in existing scales [11, 19, 21, 22, 25, 29, 33, 35–45]. We made an effort to select, combine, divide and create items that reflect the different aspects of IS and DC, resulting in the development of two draft instruments: the HIV Internalized Stigma Scale (HIV-ISS) and the HIV Disclosure Concerns Scale (HIV-DCS).
Each scale comprised 11 items with a 5-point Likert-type response format. Next, to improve the content validity and cultural appropriateness of the scales, scale items were subjected to critical analysis by an advisory committee composed of two clinical psychologists who worked in an HIV-related NPO in Madrid (Spain) and four HIV+ patients (two males and to females) who attended NPO activities. The advisory committee members were asked to read the scales and respond to the following questions: Do you find any item to be irrelevant? Do you think there are items that are very similar and should be combined? Is there any item that you would deem important to separate into several? Would you change the way of expressing anything? Can you think of any important aspects not taken into account that should be included? The committee members then presented their comments and suggested item revisions. As established by mutual agreement at the beginning of the meeting, the clinical psychologists provided their judgments last, in order to avoid biasing the patients’ opinion. A final agreement regarding item revisions was achieved by the committee members.
As a result of the critical analysis, 1 item was eliminated from the HIV-ISS and 2 items from the HIV-DCS; 2 items were combined and subsequently separated in the HIV-ISS; 1 item was separated into two in the HIV-DCS; 1 item in each scale was re-written to improve its content; and 1 item of the HIV-DCS was modified to include an important aspect not taken into account in the original scale. The final scales were composed of 10 items each.
The revised scales, along with the HADS and the RSE, were administered to a sample of 458 HIV-positive adults. Upon completion, respondents were thanked and invited to collaborate further by completing the HIV-ISS and the HIV-DCS again in 4 weeks. Those willing (N = 291) provided their email and were assigned a code to allow merging of the test/retest data. After 4 weeks, respondents were emailed a message which included the link for the retest questionnaire and a reminder of their code. A total of 125 participants completed the retest assessment.
Statistical Analyses
Factorial validity was assessed by means of an exploratory factor analysis (EFA) conducted on both scales to test if the items of each scale loaded differentially on two factors. Initial suitability of the data for performing EFAs was assessed via the Kaiser–Meyer–Olkin (KMO) measure and Bartlett’s test that one or more latent factors are required to explain the correlations among the items. The distributions of scores were asymmetric, so we used the unweighted least squares (ULS) method for extraction, given that it requires no distributional conditions, it usually yields less biased estimates and it is quite robust [56]. We used direct Oblimin method for rotation to allow factor correlation. The criterion for retaining a factor was that it had an eigenvalue higher than 1. Only items with factor loadings higher than .40 were retained, guaranteeing the factors only included moderately to strongly-related items [57, 58].
The reliability related to internal consistency was measured by Cronbach’s alpha coefficient, and test–retest was assessed using a two-way mixed, absolute agreement, single-measures Intra-class Correlation Coefficient (ICC) [59]. The ICC was chosen because it addresses both agreement and correspondence between scores, and the repetition can be regarded as a random factor [60].
Criterion validity of HIV-ISS and HIV-DCS scores was assessed by Pearson’s correlation with HADS-A, HADS-D and RSE scores. Additionally, the model fit of a predictive Path Analysis with Latent Variables (PALV) was tested. This model considered HIV-ISS and HIV-DCS scores as predictors and HADS-A, HADS-D and RSE scores as criteria. Thus, Unweighted Least Squares was used as the estimation method. In order to assess model fit, we used absolute measures of fit (GFI, AGFI and SRMR) and incremental ones (NFI and RFI). For GFI, AGFI, NFI and RFI, values between .90 and .95 are considered acceptable, and above .95 are good—the fit is better as it approaches to 1 [61–63]. For SRMR, values <.08 are indicative of a good fit [64]. All of these indices are valid for the ULS method.
Finally, sensitivity of the scales was assessed by addressing gender, age, time since diagnosis, nationality, educational level, connection with NPOs, treatment status and treatment adherence effects on IS and DC (Pearson correlations, ANOVAs and T tests were conducted). Significant omnibus F-test results for ANOVAs were followed up with post hoc paired comparison tests with multiplicity-adjusted p-values obtained using the Games-Howell post hoc test. An adherence of 90 % or higher was considered good adherence. Only males and females were included in the gender differences analyses, as there were only four participants who reported “other” gender. Data analyses were performed using SPSS v22.0 and AMOS v22.0.
Results
Factorial Validity
We began by conducting an EFA. The KMO (KMO = .95) and Bartlett’s test (χ2 = 6634.28, df = 190, p < .001) indicated good sampling adequacy for factor analysis. The analysis yielded a two-factor solution that accounted for 63.07 % of the variance—the first factor explained 47.48 % and the second 15.59 %. As for the shared variance in the data, 59.15 % was explained by the solution, 45.54 % by the first factor and 13.62 % by the second. The left side of Table 2 shows the factors loadings for the rotated solution (factor pattern matrix). Since an oblique rotation was applied, we provide the factor structure matrix in the right side of Table 2, which shows the correlation between each item and the factors of the rotated solution. The correlation between the two factors was r = .51.
As can be seen in Table 2, all items loaded highly on only one factor and there were no cross-loadings. In fact, all of the HIV-ISS items loaded on Factor 1 and all items from the HIV-DCS scale loaded on Factor 2, which suggests that Factor 1 represents Internalized Stigma due to HIV+ condition and Factor 2 refers to Disclosure Concerns.
Reliability (Internal Consistency and Test–Retest Reliability) and Descriptive Results
For the complete sample, Cronbach’s alphas for the HIV-ISS and the HIV-DCS were α = .94 and α = .93, respectively. These values did not increase with the removal of any items. Reliability tests were run within those nationality subsamples with 50 participants or more (Spain, Mexico, Colombia and other Latin American countries), with alphas ranging from α = .91–.95 for the HIV-ISS and α = .91–.94 for the HIV-DCS.
The mean score on the HIV-ISS for the whole sample was 23.33 (SD = 11.14; range 10–50), and the mean score for the HIV-DCS was 35.36 (SD = 11.17; range 10–50). Table 3 shows the Mean, SD and Corrected Item-Total Correlation of each item. The test–retest correlation assessed with ICC was .79 (p < .001; 95 % CI .71–.85) for the HIV-ISS, and .86 (p < .001; 95 % CI .81–.90) for the HIV-DCS. Within the subsamples of participants from Spain, Mexico, Colombia and other Latin American countries, the ICC ranges were .74–.86 (all p < .001) for the HIV-ISS and .84–.92 (all p < .001) for the HIV-DCS.
Criterion Validity
To assess criterion validity, indicated by the correlation among HIV-ISS and HIV-DCS scores and other instruments that measure similar constructs, the HADS-A (anxiety), HADS-D (depression) and RSE (self-esteem) scores were employed. Results of the Pearson correlations are presented in Table 4. As expected, all measures were correlated in the anticipated direction. HIV-ISS was more related to HADS-A (r = .63), HADS-D (r = .56) and RSE (r = −.60) than HIV-DCS (r = .35, r = .35 and r = −.30, respectively; all correlations p < .01), although both scales showed high and significant correlations.
The regression model tested by means of the PALV is presented in Fig. 1. The obtained fit values were the following: GFI = .98, AGFI = .98, SRMR = .07, NFI = .98 and RFI = .98. All of them were well inside limits for acceptance of the model. As can be seen in Fig. 1, the amounts of explained variance are high (HADS-A = .65, HADS-D = .59, and RSE = .59). Also, the regression weights of HIV-ISS on the dependent variables were high and significant in all cases and in the expected direction: .87 on HADS-A, .83 on HADS-D and −.85 on RSE. The regression weights of HIV-DCS on HADS-A, HADS-D and RSE were almost null (−.11, −.12 and .15, respectively).
Sensitivity of the Scales
To address possible age and time since diagnosis relation with Internalized Stigma and Disclosure Concerns, Pearson correlations were obtained. The results were significant for both scales: HIV-ISS had a high, significant negative correlation with age (r = −.35, p < .01) and with time since diagnosis (r = −.32, p < .01), as HIV-DCS did (respectively, r = −.27, p < .01 and r = −.31, p < .01).
We also tested for HIV-ISS and HIV-DCS differences by nationality, educational level, connection with an NPO, being on HIV treatment or not and treatment adherence. The ANOVA showed that the differences by nationality were significant for HIV-DCS (F[4, 453] = 4.64; p = .001, η 2 = .04), but not for HIV-ISS (F[4, 453] = 1.58; p = .179). A Games-Howell post hoc test showed that HIV-DCS scores were significantly lower for Mexicans (M = 31.86) compared to Spaniards (M = 36.45, p = .018) and Colombians (M = 38.93) (p = .002). There were no significant differences among educational levels (F HIV-ISS[5, 452] = 1.16, p = .328; F HIV-DCS[5, 452] = 1.07, p = .376).
The t-tests showed that those in connection with an NPO had lower HIV-ISS and HIV-DCS scores (M HIV-ISS = 20.47, M HIV-DCS = 29.17) than those who were not (M HIV-ISS = 24.48, M HIV-DCS = 37.84; t HIV-ISS(456) = 3.52, p < .001; t HIV-DCS(202.47) = 7.33, p < .001). Also, those on treatment had lower HIV-ISS and HIV-DCS scores (M HIV-ISS = 22.11, M HIV-DCS = 34.57) than those who were not (M HIV-ISS = 29.14, M HIV-DCS = 39.08; t HIV-ISS(103.28) = −4.68, p < .001; t HIV-DCS(456) = −3.31, p = .001). No differences on HIV-ISS and HIV-DCS were found between those who had good adherence and those who did not (t HIV-ISS(376) = −.88, p = .381; t HIV-DCS(376) = −1.30, p = .196), or between males and females (t HIV-ISS(452) = .62, p = .533; t HIV-DCS(452) = .37, p = .716).
HIV-ISS and HIV-DCS Short Forms
Since there are circumstances where it would not be practical to administer the complete scales, we sought to provide short tools for assessing IS and DC. To achieve this, we retained three items from each scale basing our decision on the factor loadings and the Cronbach alphas when items were deleted.
Items 1, 2 and 5 remained for the HIV-ISS, showing an alpha of α = .87, a test–retest ICC of .70 (95 % CI .59–.78) and a correlation with the whole scale of r = .93. The HIV-ISS Short Form (HIV-ISS-SF) was significantly related to HADS-A, HADS-D and RSE (Pearson correlations were, respectively, r = .64, r = .56 and r = −.55, all of them p < .001). Items 2, 6 and 7 remained for the HIV-DCS, with an alpha of α = .90, a test–retest ICC of .84 (95 % CI .77–.88) and a correlation with the whole scale of r = .94. The HIV-DCS Short Form (HIV-DCS-SF) was significantly related to HIV-ISS-SF, HADS-A, HADS-D and RSE (Pearson correlations were, respectively, r = .42, r = .29, r = .30 and r = −.25, all of them p < .001).
Another EFA was conducted (KMO = .78 and Bartlett’s test: χ2 = 1681.20, df = 15, p < .001) with the six items and it yielded a two factor solution in which HIV-DCS-SF formed the first factor that explained 57.53 % of the variance, and HIV-ISS-SF items formed the second factor that accounted for an additional 23.45 % of the variance. The two factors were correlated (r = .47), and Table 5 shows the Pattern Matrix for this EFA. These data suggest that the short versions of both scales provide reliable and valid measures of internalized stigma and disclosure concerns for use in situations where a short scale is necessary.
Discussion
We sought to develop and ascertain the psychometric properties of an Internalized Stigma (IS) scale and a Disclosure Concerns (DC) scale in HIV+ populations from several Spanish-speaking countries. The results suggest that both scales show adequate psychometric properties in terms of validity, reliability and sensitivity.
Regarding factorial validity, our data support our first hypothesis that IS and DC would be different, although related, constructs. The EFA yielded a clear two factor solution both for the whole scales and the short forms, in which one factor comprised the IS items and the other the DC items, resulting in a IS scale and a DC scale that were moderately correlated, as found in previous research [25, 38, 39, 41, 43]. With respect to criterion validity, our results showed that our measures (both the whole scales and the short forms) are significantly related to depression, anxiety and self-esteem, which supports our second hypothesis. The correlations followed the expected direction, with IS correlations being higher than DC correlations, as found in other studies [11, 19, 25, 29, 39, 41–44]. The PALV, which showed an excellent fit to data, demonstrated that high percentages of the variance of HADS-A, HADS-D and RSE can be explained from HIV-ISS. In this case, the relations between IS and the criteria were, again, stronger than that of DC, the latter being non-significant in all cases. This result is congruous with what was found in Bunn et al. and Jimenez et al.’s work [25, 43].
Regarding reliability, we found that both measures in both forms (the whole scales and the short forms) demonstrated good internal consistency and test–retest reliability, data that speak in favor of the psychometric solidity of these measures.
With regard to sensitivity analyses, IS and DC were in our sample negatively related to age, time since diagnosis, connection to an NPO, and being on treatment, as previously found [12, 21, 38]. Our study also revealed potential national differences on DC that had not been previously explored among these populations, showing that Mexicans have lower DC than Spaniards and Colombians. These results provide partial support for our third hypothesis, and open paths to future research.
There were hypothesized relations for which our results did not provide support. First, there were no gender differences in relation to IS or DC. This result is congruous with Sayle et al.’s results [38], and could reflect national differences, since the study on which we based our hypothesis [11] was conducted in India. Second, a previous study found that those with secondary education or higher had a lower degree of general stigma and IS [21, 38], but no differences emerged in our sample. We think this might be due to the small number of participants who had an educational level lower than secondary—only 18 out of the 458 of the total sample. Third, there were no differences in IS or DC by treatment adherence, which other studies had found [17, 32]. This result, although congruous with Tzemis et al.’s work [21], could be explained if we again consider the small number of participants who reported suboptimal adherence—only 22 out of 378 who were on ART. Nevertheless, this lack of conclusiveness suggests the need for further research in these areas.
Our study has several implications. With regard to research, it provides the Spanish and Spanish-speaking research community with reliable and valid tools to assess the critical variables of IS and DC, as well as with short forms more convenient for situations with a tight timetable. The scales have been validated in a large and culturally heterogeneous sample and, thus, can be used for research in several populations. Our study has also contributed knowledge to the field of stigma by showing DC and IS are different constructs and that their measurement, especially that of IS, is able to predict the existence of psychopathological symptoms such as anxiety, depression and self-esteem. This is of paramount importance to the field of Health Psychology, where our study could also have clinical implications. The IS and DC scales could be used in clinical settings as screening methods to detect people at risk that would benefit from a psychological intervention, although we believe more research would be necessary in this regard, especially with populations in Latin American countries. Possible interventions derived from our results might include the suggestion that passive waiting for IS and DC to fade over the years may not the only option; we could encourage newly diagnosed patients to engage with an NPO (e.g., attend talks or workshops, join a support group, attend other events) and to begin ART, although the direction of this relations remains to be explored.
There were several limitations to our study, especially with respect to self-selection bias and convenience sampling strategy. Our advisory committee only included HIV+ people affiliated with an NPO, which makes them less likely to report IS and DC. It is true that it is difficult to approach and engage people outside NPOs for this kind of activity, but this issue could have impacted the scale refinement procedures. It is also possible that only highly motivated individuals completed the scales, which would imply a bias in our results, as the men and women who participated may differ in significant ways from those who chose not to participate. Additionally, those individuals not using online social networks had limited opportunity to be recruited into the study, so the sample may be biased toward people associated with some kind of (virtual) community, and our tools may not have been validated by the most stigmatized and isolated PLH.
Also, some of the subsamples (i.e., those without secondary education and those with suboptimal adherence) were small, which limited the possibility of accurately testing some of our hypotheses regarding the sensitivity of the scales. Likewise, the fact that our sample was highly educated may limit the generalizability of our findings to Spanish-speaking populations with a lower educational level. Moreover, all Spanish-speaking individuals were considered as one sample for some analyses (e.g., criterion validity analyses), not taking into account the nationality of the participants, which constitutes another limitation of this study. Future research should address these issues, and we also recommend in depth exploration of the national differences that emerged in our study, as well as the reasons for those differences.
Finally, further research should test if our scales are sensitive to change, for instance with a pre-post design that compares scale scores before and after attending a support group or a stigma reduction intervention.
In conclusion, the HIV-ISS and HIV-DCS are reliable means of assessing HIV internalized stigma and disclosure concerns as separate constructs, both for clinical and research purposes and in a variety of Spanish-speaking populations.
References
Prado G, Lightfoot M, Brown CH. Macro-level approaches to HIV prevention among ethnic minority youth: state of the science, opportunities, and challenges. Am Psychol. 2013;68(4):286–99.
Bletzer KV. Identity and resilience among persons with HIV: a rural African American experience. Qual Health Res. 2007;17(2):162–75.
Feigin R, Sapir Y, Patinkin N, Turner D. Breaking through the silence: the experience of living with HIV-positive serostatus, and its implications on disclosure. Soc Work Health Care. 2013;52(9):826–45.
Wu L, Li X. Community-based HIV/AIDS interventions to promote psychosocial well-being among people living with HIV/AIDS: a literature review. Health Psychol Behav Med. 2013;1(1):31–46.
Su X, Lau JTF, Mak WWS, et al. Perceived discrimination, social support, and perceived stress among people living with HIV/AIDS in China. AIDS Care. 2013;25(2):239–48.
Clucas C, Sibley E, Harding R, Liu L, Catalan J, Sherr L. A systematic review of Interventions for anxiety in people with HIV. Psychol Health Med. 2011;16(5):528–47.
Teva I, de la Paz Bermúdez Sánchez M, Hernández-Quero J, Buela-Casal G. Evaluación de la depresión, ansiedad e ira en pacientes con VIH/SIDA. Salud Ment. 2005;28(5):40–9.
DeGenova MK, Patton DM, Jurich JA, MacDermid SM. Ways of coping among HIV-infected individuals. J Soc Psychol. 1994;134(5):655–63.
Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–21.
De Santis JP, Florom-Smith A, Vermeesch A, Barroso S, DeLeon DA. Motivation, management, and mastery a theory of resilience in the context of HIV infection. J Am Psychiatr Nurses Assoc. 2013;19(1):36–46.
Steward WT, Herek GM, Ramakrishna J, et al. HIV-related stigma: adapting a theoretical framework for use in India. Soc Sci Med. 2008;67(8):1225–35.
Lee RS, Kochman A, Sikkema KJ. Internalized stigma among people living with HIV-AIDS. AIDS Behav. 2002;6(4):309–19.
Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol. 2013;68(4):225.
Bharat S. A systematic review of HIV/AIDS-related stigma and discrimination in India: current understanding and future needs. SAHARA J. 2011;8(3):138–49.
Pellowski JA, Kalichman SC, Matthews KA, Adler N. A pandemic of the poor: social disadvantage and the U.S. HIV epidemic. Am Psychol. 2013;68(4):197–209.
Rao D, Kekwaletswe TC, Hosek S, Martinez J, Rodriguez F. Stigma and social barriers to medication adherence with urban youth living with HIV. AIDS Care. 2007;19(1):28–33.
Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009;24(10):1101–8.
Leserman J. Role of depression, stress, and trauma in HIV disease progression. Psychosom Med. 2008;70(5):539–45.
Phillips KD, Moneyham L, Tavakoli A. Development of an instrument to measure internalized stigma in those with HIV/AIDS. Issues Ment Health Nurs. 2011;32(6):359–66.
Yi S, Chhoun P, Suong S, Thin K, Brody C, Tuot S. AIDS-related stigma and mental disorders among people living with HIV: a cross-sectional study in Cambodia. PLoS One. 2015;10(3):e0121461.
Tzemis D, Forrest JI, Puskas CM, et al. Identifying self-perceived HIV-related stigma in a population accessing antiretroviral therapy. AIDS Care. 2013;25(1):95–102.
Kingori C, Reece M, Obeng S, et al. Psychometric evaluation of a cross-culturally adapted felt stigma questionnaire among people living with HIV in Kenya. AIDS Patient Care STDS. 2013;27(8):481–8.
Rensen C, Bandyopadhyay S, Gopal PK, Van Brakel WH. Measuring leprosy-related stigma—a pilot study to validate a toolkit of instruments. Disabil Rehabil. 2011;33(9):711–9.
Scambler G. Epilepsy. London: Tavistock; 1989.
Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV: a reexamination of the HIV stigma scale. AIDS Educ Prev. 2007;19(3):198–208.
Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71(12):2150–61.
Singh D, Kumar B, Mukhopadhyay A, Singh A. Internalised stigma and quality of life in people living with HIV. J Indian Health Psychol. 2014;9(1):1–9.
Paudel V, Baral KP. Women living with HIV/AIDS (WLHA), battling stigma, discrimination and denial and the role of support groups as a coping strategy: a review of literature. Reprod Health. 2015;12(1):53.
Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the internalized AIDS-related stigma scale. AIDS Care. 2009;21(1):87–93.
Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64(9):1823–31.
Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–77.
Li MJ, Murray JK, Suwanteerangkul J, Wiwatanadate P. Stigma, social support, and treatment adherence among HIV-positive patients in Chiang Mai, Thailand. AIDS Educ Prev. 2014;26(5):471–83.
Holzemer WL, Uys LR, Chirwa ML, et al. Validation of the HIV/AIDS stigma instrument-PLWA (HASI-p). AIDS Care. 2007;19(8):1002–12.
Okello ES, Wagner GJ, Ghosh-Dastidar B, et al. Depression, internalized HIV stigma and HIV disclosure. World J AIDS. 2015;5(01):30.
Lindberg MH, Wettergren L, Wiklander M, Svedhem-Johansson V, Eriksson LE. Psychometric evaluation of the HIV stigma scale in a Swedish context. PLoS One. 2014;9(12):e114867.
Van Rie A, Sengupta S, Pungrassami P, et al. Measuring stigma associated with tuberculosis and HIV/AIDS in southern Thailand: exploratory and confirmatory factor analyses of two new scales. Trop Med Int Health. 2008;13(1):21–30.
Kipp AM, Audet CM, Earnshaw VA, Owens J, McGowan CC, Wallston KA. Re-validation of the Van Rie HIV/AIDS-related stigma scale for use with people living with HIV in the United States. PLoS One. 2015;10(3):e0118836.
Sayles JN, Hays RD, Sarkisian CA, Mahajan AP, Spritzer KL, Cunningham WE. Development and psychometric assessment of a multidimensional measure of internalized HIV stigma in a sample of HIV-positive adults. AIDS Behav. 2008;12(5):748–58.
Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–29.
Sumari-de Boer IM, Nellen JFB, Sprangers MAG, Prins JM, Nieuwkerk PT. Personalized stigma and disclosure concerns among HIV-infected immigrant and indigenous HIV-infected persons in the Netherlands. J HIV AIDS Soc Serv. 2012;11(1):42–56.
Franke MF, Muñoz M, Finnegan K, et al. Validation and abbreviation of an HIV stigma scale in an adult spanish-speaking population in urban Peru. AIDS Behav. 2010;14(1):189–99.
Miric M. Escala para la evaluación del estigma sentido entre las personas VIH positivas en la República Dominicana. Paradigmas. 2004;4:70–101.
Jimenez JC, Puig M, Ramos JC, et al. Measuring HIV felt stigma: a culturally adapted scale targeting PLWHA in Puerto Rico. AIDS Care. 2010;22(11):1314–22.
Tsai AC, Weiser SD, Steward WT, et al. Evidence for the reliability and validity of the internalized AIDS-related stigma scale in rural Uganda. AIDS Behav. 2013;17(1):427–33.
Murphy PJ, Hevey D. The relationship between internalised HIV-related stigma and posttraumatic growth. AIDS Behav. 2013;17(5):1809–18.
Stevelink SAM, Wu IC, Voorend CGN, van Brakel WH. The psychometric assessment of internalized stigma instruments: a systematic review. Stigma Res Action. 2012;2(2):100–18.
Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–70.
Quintana JM, Padierna A, Esteban C, Arostegui I, Bilbao A, Ruiz I. Evaluation of the psychometric characteristics of the Spanish version of the Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 2003;107(3):216–21.
Luciano JV, Barrada JR, Aguado J, Osma J, García-Campayo J. Bifactor analysis and construct validity of the HADS: a cross-sectional and longitudinal study in fibromyalgia patients. Psychol Assess. 2014;26(2):395–406.
Terol-Cantero M, Cabrera-Perona V. Hospital Anxiety and Depression Scale (HADS) review in Spanish samples. An Psicol. 2015;31(2):494–503.
Herrero MJ, Blanch J, Peri JM, De Pablo J, Pintor L, Bulbena A. A validation study of the hospital anxiety and depression scale (HADS) in a Spanish population. Gen Hosp Psychiatry. 2003;25(4):277–83.
Vallejo MA, Rivera J, Esteve-Vives J, Rodríguez-Muñoz MF. Uso del cuestionario Hospital Anxiety and Depression Scale (HADS) para evaluar la ansiedad y la depresión en pacientes con fibromialgia. Rev Psiquiatr Salud Ment. 2012;05(02):107–14.
Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965.
Morejón AJV, García-Bóveda RJ, Jiménez RV-M. Escala de autoestima de Rosenberg: fiabilidad y validez en población clínica española. Apunt Psicol. 2004;22(2):247–55.
Martín-Albo J, Núñez JL, Navarro JG, Grijalvo F. The Rosenberg Self-Esteem Scale: translation and validation in university students. Span J Psychol. 2007;10(02):458–67.
Briggs NE, MacCallum RC. Recovery of weak common factors by maximum likelihood and ordinary least squares estimation. Multivar Behav Res. 2003;38(1):25–56.
Stevens JP. Applied multivariate statistics for the social sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1992.
Floyd FJ, Widaman KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychol Assess. 1995;7(3):286–99.
Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19(1):231–40.
Kim H-Y. Statistical notes for clinical researchers: evaluation of measurement error 1: using intraclass correlation coefficients. Restor Dent Endod. 2013;38(2):98.
Byrne BM. Structural equation modeling with AMOS: basic concepts, applications, and programming. Mahwah, NJ: Lawrence Erlbaum; 2001.
Bollen KA. Sample size and Bentler and Bonett’s non-normed fit index. Psychometrika. 1986;51:375–7.
Bentler PM, Bonett DG. Significance tests and goodness-of-fit in the analysis of covariance structures. Psychol Bull. 1980;88:588–600.
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model A Multidiscip J. 1999;6(1):1–55.
Acknowledgments
The authors would like to acknowledge the HIV associations in Spain and Latin America for their help with the data collection, being especially grateful to Apoyo Positivo, whose help was fundamental both for the focus group and the data collection. The authors would also like to acknowledge Manuel Martín-Fernandez for his statistics-related advice, Rocío Rodríguez-Rey for the review of the first draft, and Joey Taylor, Mallory Johnson and Torsten Neilands for their comments on the manuscript. Finally, the first author would like to acknowledge the financial support given by the Spanish Ministerio de Educación, Cultura y Deporte through a FPU fellowship.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1: English Translation of the HIV Internalized Stigma Scale
Please indicate the degree in which you felt in the following ways during the last month because of having HIV:
Never or hardly ever | Rarely | Sometimes | Very often | All or almost all the time | |
|---|---|---|---|---|---|
1. I felt dirty or stained | 1 | 2 | 3 | 4 | 5 |
2. I felt guilty | 1 | 2 | 3 | 4 | 5 |
3. I felt embarrassed | 1 | 2 | 3 | 4 | 5 |
4. I felt flawed or incomplete | 1 | 2 | 3 | 4 | 5 |
5. I felt disappointed with myself | 1 | 2 | 3 | 4 | 5 |
6. I thought I was promiscuous | 1 | 2 | 3 | 4 | 5 |
7. I thought I don’t deserve to be loved | 1 | 2 | 3 | 4 | 5 |
8. I thought I have HIV because I did things that aren’t good | 1 | 2 | 3 | 4 | 5 |
9. I felt repulsion for myself | 1 | 2 | 3 | 4 | 5 |
10. I thought I’m being punished for having done immoral things | 1 | 2 | 3 | 4 | 5 |
Appendix 2: English Translation of the HIV Disclosure Concerns Scale
Please indicate the degree in which the following sentences describe what you think or feel:
Very little | Little | Somewhat | Much | A great deal | |
|---|---|---|---|---|---|
1. It’s difficult to tell people that I have HIV | 1 | 2 | 3 | 4 | 5 |
2. I’d do almost anything to avoid that people know that I have HIV | 1 | 2 | 3 | 4 | 5 |
3. I’m very careful with whom I tell I have HIV | 1 | 2 | 3 | 4 | 5 |
4. I’m worried that if my appearance changes because of HIV or the treatment, someone may find out that I have it | 1 | 2 | 3 | 4 | 5 |
5. I’m worried that if I attend or participate in an HIV group, someone may see me and be suspicious | 1 | 2 | 3 | 4 | 5 |
6. I’m worried about someone seeing my medical reports and finding out about my HIV | 1 | 2 | 3 | 4 | 5 |
7. I’m worried that if I go to the doctor or I get ill, someone close to me might find that I have HIV | 1 | 2 | 3 | 4 | 5 |
I’m worried about how they would react if they knew I have HIV | |||||
8. The most important people for me | 1 | 2 | 3 | 4 | 5 |
9. People from work | 1 | 2 | 3 | 4 | 5 |
10. Other people I interact with | 1 | 2 | 3 | 4 | 5 |
Rights and permissions
About this article
Cite this article
Hernansaiz-Garrido, H., Alonso-Tapia, J. Internalized HIV Stigma and Disclosure Concerns: Development and Validation of Two Scales in Spanish-Speaking Populations. AIDS Behav 21, 93–105 (2017). https://doi.org/10.1007/s10461-016-1305-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1305-1