Abstract
Peruvian men who have sex with men (MSM) and transwomen (TW) could benefit from a rectal microbicide (RM) formulated as a rectal douche to prevent HIV infection. However, little is known about rectal douching practices among Peruvian MSM and TW, information necessary to inform RM douche development and future uptake. Using a self-administered interview, we examined the prevalence of and factors associated with rectal douching among a convenience sample of 415 Peruvian MSM and 68 TW. In the previous 6 months, 18 % of participants reported rectal douching using pre-filled commercial kits or plastic bottles or enema bags filled with water, water/soap or saltwater. Multivariate logistic analysis found that “equally insertive and receptive” or “exclusively/mainly receptive” sex roles were associated with douche use. Rectal douching among Peruvian MSM and TW is similar to reports from other studies and supports the potential uptake of a douche-formulated RM in these populations.
Resumen
Los hombres que tienen sexo con otros hombres (HSH) y las mujeres transgénero (MT) peruanos podrían beneficiarse con microbicidas rectales (MR) formulados como una ducha rectal para prevenir la infección por VIH. Sin embargo, se conoce poco sobre las prácticas de duchas rectales entre HSH y MT en Perú, información necesaria para orientar el desarrollo de MR y su futura aceptación. Utilizando una entrevista auto-administrada, examinamos la prevalencia y los factores asociados con el uso de duchas rectales en una muestra por conveniencia de 415 HSH y 68 MT peruanos. En los seis meses recientes, 18% de los participantes reportaron haber usado duchas rectales comerciales pre-llenados o botellas de plástico o bolsas para enema llenas con agua, agua con jabón, o agua salada. El análisis multivariado encontró que los roles sexuales "igualmente insertivos o receptivos" o "exclusivamente/principalmente receptivos" estaban asociados con el uso de duchas rectales. El uso de duchas rectales entre HSH y MT es similar a lo reportado en otros estudios y da respaldo a la posible aceptación por parte de estas poblaciones de los MR formulados.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The efficacy and effectiveness of antiretroviral preexposure prophylaxis (PrEP) for the prevention of HIV acquisition in men who have sex with men (MSM) and transwomen (TW) has been unequivocally demonstrated when delivered orally in tablet form [1–4]. At the same time, products are under development that would deliver antiretrovirals locally, at the site of infection, rather than systemically as with oral PrEP. These “topical PrEP” products—microbicides—are introduced into the vagina or rectum prior to intercourse and could have a number of potential advantages over oral-PrEP in terms of cost, adherence and long-term safety as well as providing consumers more HIV prevention options according to personal preferences [5–7]. In view of the expanding global HIV epidemics in MSM and TW [8], there is an urgent, immediate need for novel HIV prevention options that can be readily incorporated into existing sexual practices, and rectal microbicides (RM) have the potential to play an important role in addressing this need.
The RM field was born out of the desire to develop an HIV prevention option specifically for the receptive partner during anal intercourse (AI). Gel-based RMs are attractive since they could integrate HIV prevention into a common preexisting behavior: anorectal lubrication prior to receptive AI. But like all HIV prevention interventions, future RMs will only work if used correctly and consistently. For this reason, a wealth of acceptability and adherence research has been conducted to identify the sociocultural and product related factors that may mediate their use [9–13]. Results from a Phase-II clinical trial on the safety and acceptability of a rectal gel are expected in 2016 [14], but irrespective of the results, one important issue will remain: lubricant use during AI by MSM and TW is not universal, and it cannot be assumed that a gel-based RM, regardless of its potential lubricating properties, will be adopted by those who do not already have the practice of applying rectal lubricants.
Research on sexual lubricant among MSM and TW are illustrative of the magnitude of the non-lube using population. For example, a 2010 global internet survey including 4554 men reporting receptive AI in the previous 6 months found that only 37.2 % of respondents reported “always” using lubricants during receptive AI [15]. A large survey among Peruvian MSM practicing receptive AI (N = 843) found that 48 % reported lubricant use during their last receptive AI [16]. The primary reasons for not using lubricants among men during receptive AI included “used saliva” (72.2 %) and “prefer dry sex” (19.1 %) for men in the global survey [15] and “uses condoms” (27 %) and “prefer dry sex” (20 %) in the Peruvian survey [16]. While no current or previous studies on RM have assessed its role as a lubricant (but rather have only assessed safety and acceptability as a rectally applied product), these data nonetheless fuel inquiry into alternatives to the RM gel delivery platform for non-lubricant users which could still leverage a preexisting practice to deliver the HIV prevention intervention.
Rectal douches (or enemas), as with sexual lubricants, are commonly used by MSM prior to receptive AI. Studies conducted mainly in US populations have begun to explore rectal douching practices among MSM in order to understand its potential as an HIV prevention delivery platform [17, 18]. Antiretroviral-based douches for HIV prevention may appeal not only to those who dislike gel-RMs (regardless of douching practices) but could attract non-douchers who may find a product that “cleans and protects” the rectum prior to receptive AI appealing [19]. The most comprehensive investigation on douching practices included 4992 MSM from 16 US cities, with half (52 %) of participants reporting a lifetime history of douching (35 % having done so in the past 3 months) and 88 % reporting the practice prior to receptive AI [20]. While water was the most commonly reported douching liquid (65 %), additives such as salt or soaps including antibacterial substances were reported by 24 % of the participants while 30 % reported commercially acquired products. Recent enema use was significantly associated with an HIV-positive status, being of color, having a sexually transmitted infection (STI) diagnosis, practicing both insertive and receptive AI and having condomless sex with more than two partners.
Javanbakht and colleagues examined rectal douching prevalence and practices in a worldwide sample comprising 1725 mostly male (88 %) respondents from 112 countries [21]. Among those reporting douching (66 % of the sample), the majority (83 %) said the practice occurred “always or almost always” before receptive AI. Homemade products were used by 93 % of douchers, water being reported 82 % of the time. Being infected with HIV, substance use during sex, and having an STI in the past year were all significantly associated with rectal douching. In multivariate analysis controlling for age, gender, region, condom and lubricant use, substance use, and HIV-status, those who douched had a 74 % increased odds of reporting a STI in the past year compared to non-douchers.
These studies highlight the potential utility of a douche-based HIV prevention intervention not only because of the high prevalence of the practice but also since it may well “target” persons with other practices that increase HIV/STI risks. An important next step, however, is the further expansion of this research into low and middle income countries, where the HIV prevalence among MSM and TW is generally much higher than in general populations [22, 23]. Peru exemplifies the global disparity in HIV rates between MSM, TW and the general population, [24] where the HIV prevalence is estimated at 12.4 % in MSM and 20.8 % in TW [25] compared to 0.40 % in the general population [26].
Two preliminary studies on rectal douching among MSM and TW have been conducted in Peru. In the first, among 824 MSM from three different cities (coastal Lima and the jungle cities of Iquitos and Pucallpa) practicing receptive AI, 27 % reported a history of rectal douching but 80 % of all respondents said they would use a rectal douche to protect against HIV if available [27]. In the second study, a qualitative analysis examined the thoughts and practices regarding rectal douching from a sample of 140 MSM and TW from Lima and Iquitos, Peru as well as Guayaquil, Ecuador. This study found that while an HIV-preventing douche was of interest to study participants and even perceived by some as having the potential to be more effective than a gel-based microbicide, questions regarding practicality and side-effects also emerged [19]. The types of douching solutions used led to the conclusion that current douching practices could be doing “more harm than good.” Nonetheless, while important, these initial studies were very limited in scope, inasmuch as they were designed primarily to establish if rectal douching occurred among Peruvian MSM and TW and what these populations knew and thought about the practice as it might relate to HIV prevention. Missing, however, is quantitative practice-specific data, including rectal douching frequency and timing (before or after AI); reasons for or not douching; and, douching apparatus and liquids used and liquid retention time. We conducted the present study to more formally characterize the prevalence, practices and factors associated with douching prior to AI among Peruvian MSM and TW, information which could inform RM douche development not only for Peru but for similar, Latino populations.
Methods
Participants and Procedures
This study was embedded in a cohort study examining the role of anogenital warts in HIV acquisition among 600 HIV-uninfected Peruvian MSM and TW in Lima, Peru, described elsewhere, where the recruitment plan is explained in detail [28]. Briefly, the study was conducted at the Gay Men’s health center Epicentro in Lima which provides free and low-cost health and social services for MSM and TW. During February 2012-February 2013, MSM and TW attending Epicentro for any reason were invited to be screened for study participation. Participants were also recruited at bars, clubs and volleyball courts where MSM and TW frequent, and via social media, where study banner-ads were posted describing the study and inviting MSM and TW to contact Epicentro for study screening. Recruitment venues were selected by convenience by the study staff which regularly recruits MSM and TW for a range of research studies, and where recruitment of study participants was reliably successful. Finally, all enrolled study participants were encouraged to refer other MSM and TW to the study. Eligibility criteria for study participation were: born anatomically male; at least 18 years old; reported any AI with a man during the previous 12 months; residing in Lima; tested HIV-uninfected at enrollment; and, had not previously participated in an HIV or HPV vaccine study. HIV status was determined using the Determine HIV-1/2 Combo Ag/Ab test (Alere Inc, Waltham, MA, USA) and confirmed by indirect immunofluorescence assay (in-house test, Peruvian National Institute of Health) and individuals testing positive were linked to the national HIV program for free care and treatment. After providing signed, voluntary informed consent for study participation (in which the study purpose, procedures, risks and benefits were discussed), the study procedures commenced. Enrolled participants completed a 20-min, computer-assisted self-interview and underwent a physical examination by the study clinician which included assessment of any STI symptoms (e.g., anogenital warts, other genital lesions and genital discharge); STI were treated empirically on-site following national guidelines and referrals were made to specialists as needed. Participants received the equivalent of USD $3 for transportation as well as condoms, lubricant and a small gift. Institutional Review Boards at the University of California, Los Angeles and the Asociación Civil Impacta Salud y Educación in Lima, Peru reviewed and approved all study materials prior to implementation.
Measures
The main study protocol stipulated follow-up clinic visits at months 6, 12, 18 and 24 post enrollment for repeated HIV testing and application of a computer-assisted, self-administered socio-behavioral interview lasting 20 min. Participants’ age and sexual identity were taken from the enrollment visit while all other data for the present study were collected at the first follow-up visit and based on a 6-month time frame (with the exception of sex under the influence of alcohol or drugs, see below) and included sexual behaviors and related practices, anal symptoms and douche/enema use. The sexual behaviors questions included: sex partners’ sex (male only, male and female, female only); transactional sex (i.e., the exchange of money or other items of value for sex, yes/no); sex role during AI with men (exclusively/mainly insertive, equally insertive and receptive, exclusively/mainly receptive); overall frequency of AI with men (number of episodes); frequency of condomless AI with men (based on overall frequency response, number of episodes); relationship status (are you currently in a relationship with a male, yes/no); and, sex with alcohol or drugs (two questions, past month time frame, yes/no). Anal symptoms were assessed by 4 questions for the presence of: anal pus or mucous (yes/no); blood (yes/no); pain or burning (yes/no); and, ulcers or lesions (yes/no).
The douche/enema use questions were adapted from the international survey on douching practices described above [21] and collected data on the use and reasons for douching or not douching; douching frequency; timing (before or after AI); liquids used; apparatus used; and, the duration that the liquid was retained before expelling. All questions, except for the liquid retention duration question (which asked participants to state the number of minutes liquid was retained inside the rectum/anus the last time a rectal douche was used) included a list of choices from which participants were asked to choose as well as an “other” option which allowed for free-text entry. For participants who did not douche during the previous 6 months, the choices for not douching were: Did not know that people use douche before anal sex; Unnecessary; Did not have time; Dislike; Did not have access to douche or enema; Only had insertive sex in the past 6 months. For those reporting rectal douching in the previous 6 months, the frequency was measured by asking 2 questions, one for douching prior to receptive AI and one for douching after receptive AI, which both used the following Likert scale response choices: Always (100 %); The majority of times (75–99 %); Usually (50–74 %); Sometimes (25–49 %); Rarely (1–24 %); and, Never. Participants responding with less than an “Always (100 %)” frequency were asked to state the reason(s) for not always douching using the same response choices as for those who stated that they never douched in the previous 6 months (see above). Reasons for douching were measured by 2 questions, one for douching prior to and the other after receptive AI, with the following choice options: Constipation; Hygiene/cleanliness; More pleasure; Partner wants. Douche/enema liquid choices were: Water; Water and salt; Water and soap; Drinking alcohol; Lemon juice; and, Commercial product. Finally, the douche/enema apparatus used was measured in a question with these choices: Commercial enema/douche kit; Plastic bottle (soda, shampoo bottle, etc.); Enema bag.
Data Analysis
A descriptive analysis was first performed comparing douchers and non-douchers by the sample characteristics (sociodemographic, sexual behavior, condom use, etc.). Next, logistic regression was used to assess the unadjusted and adjusted odds ratios (UOR/AOR) for the association between douching and all variables in the descriptive analysis (age, sex partners’ sex, transactional sex, sex role, frequency any AI, frequency any condomless AI, condom use last AI, relationship status, HIV result, current anal symptoms, sex with alcohol, sex with drugs) with 2 exceptions: “female only” (sex partners’ sex) was omitted from both UOR and AOR calculations due to collinearity and “transactional sex” was omitted from the AOR calculation due to a high non-response rate (89 %). The corresponding 95 % Confidence Intervals (95 % CI) were calculated and reported for each UOR and AOR.
All analyses were conducted using Stata Version 12.0 (Stata Corp., College Station, TX).
Results
Demographics and Sexual Behaviors
Of 600 MSM and TW enrolled into the main study, 483 completed the 6-month interview, comprising a sexually diverse sample of men identifying as gay (237 or 49 %), bisexual (121 or 25 %), heterosexual (43 or 9 %) and TW (68 or 14 %); 14 (3 %) of the sample sexually identified as “other.” Table 1 presents key demographic characteristics of douchers and non-douchers. Nearly half of participants (47 %) were aged 18–24 years (mean = 26 years, SD = 5.7 years, range 18–46 years). Most (82 %) reported only male sexual partners during the previous 6 months. Slightly more participants reported an exclusively/primarily receptive sex role during AI (36 %), compared to either an exclusively/primarily insertive sex role (29 %) or equally insertive/receptive (29 %). Over 82 % of participants reported AI with a male partner during the previous 6 months. Nearly half (49 %) of participants reported condomless AI with a male at least once in the previous 6 months, with 23 % reporting it with their most recent sex partner.
Sexually Transmitted Infections and Symptoms
Fifteen (3 %) participants tested positive for HIV at the 6 month visit. About 17 % of all participants (n = 84) reported current anal STI symptoms, including anal pus or mucous (2 %), bleeding (12 %), pain or burning (11 %) and ulcers or lesions (5 %).
Douche/Enema use Practices
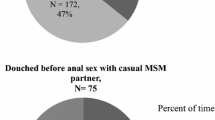
Rectal douching/enema use in the previous 6 months was reported by 18 % (88/483) of participants (Table 2). Among non-douche/enema users (395/483), 39 % said they thought it was unnecessary, 35 % said they were unaware people used douches before AI, and 16 % said they lacked access to a douche/enema. Among those reporting douche/enema use, approximately 40 % reported the practice prior to receptive AI “always or the majority of the time.” Reasons for douching/enema use prior to receptive AI were: hygiene (90 %); more pleasurable sex (21 %); constipation (14 %); and, partner request (10 %).
Water was the most commonly reported douche/enema liquid (59 %) followed by water with soap (27 %), commercial products (11 %) and saltwater (6 %). The most commonly reported apparatus used was a plastic bottle (such as a soda or shampoo bottle), with 47 participants (53 %) using this method. Other douching/enema apparatus included commercial, pre-filled kits (24 %); enema bags (6 %); and, other (13 %). Liquid retention inside of the body was on average 4.5 min (range 0–60 min; distribution: 1 min: 35 % of douche/enema users; 2–4 min: 33 %; 5–10 min: 17 %; and ≥10 min: 12 %).
Factors Associated with Douche/Enema Use (Table 3)
Variables associated with douche/enema use at the 6 month visit in the unadjusted model included sex partners’ sex (having male and female sex partners compared with having only male partners) (UOR = 0.21; 95 % CI 0.06–0.69; p < 0.01); sex role (equally insertive and receptive compared with exclusively/mainly insertive, UOR = 4.86; 95 % CI 2.03–11.63; p < 0.001) and exclusively/mainly receptive compared with exclusively/mainly insertive (UOR = 10.07; 95 % CI 4.43–22.92; p < 0.001); frequency of any AI with males (≥11 episodes compared with 1 episode; UOR = 4.64; 95 % CI 2.15–10.01; p < 0.001); frequency of any condomless AI with males (≥11 episodes compared with 0 episodes, UOR = 2.46, 95 % CI 1.08–5.58; p < 0.05); and current relationship status with another male (UOR = 1.83, 95 % CI 1.13–2.94; p < 0.05). In the adjusted model, only sex role was associated with douche use, with participants reporting an equally insertive and receptive sex role more likely to douche compared with those reporting an exclusively or mainly insertive sex role (AOR = 3.90, 95 % CI 1.44–10.61; p < 0.01) and participants reporting an exclusively or mainly receptive sex role more likely to douche than participants reporting an exclusively or mainly insertive sex role (AOR = 7.38, 95 % CI 2.24–19.90; p < 0.001). No independent association was found between self-reported STI symptoms, substance use during sex or sex with multiple sex partners and rectal douching in this study.
Discussion
We examined rectal douching practices in a sample of Peruvian MSM and TW, finding that nearly one in 5 participants used a douche or enema in the previous 6 months. Among those who used a rectal douche or enema, the practice was most frequently prior to receptive AI for hygiene/cleanliness using a (non-commercial) plastic bottle filled with water which was retained internally for less than 4 min. Our findings compliment the small body of literature on douche/enema practices of mainly US MSM and extend our previous work on this topic by providing detailed information on douching practices among Peruvian MSM and—importantly, and to our knowledge the first time—TW.
The results of our study also contrast in important ways with previous findings, including our own work in Peru, with regard to factors commonly associated with rectal douching and substances used during douching. Whereas a history of recent self-reported STI symptoms and substance use during sex were independently associated with douching when controlling for other variables in previous studies [20, 21], we found no such associations among douchers in our sample. Furthermore, while we previously reported a wide range of substances used by Peruvian MSM and TW during pre-coital rectal douching, including many that likely damage the rectal epithelia (e.g., lemon juice; tap water; soap and water; camphor; vinegar; a mixture of soap, bleach and isopropyl alcohol; chamomile water; detergent; shampoo; and, [consumable] alcohol) [19], in the present study only water, water and salt or water and soap were mentioned as non-commercial products used. In both cases, the discrepancies may be related to the relatively small sample size of douchers in the current study and the sample being limited to Lima and not including the jungle site Iquitos as in the previous study. It is possible, therefore, that douching practices differ between regions due to access issues (e.g., availability of commercial products, income differences), or differences in education levels, health and hygiene beliefs and practices or other sociocultural issues.
Differences in reported acceptability of rectal douches for HIV prevention have been previously noted between MSM in Lima and MSM from Iquitos [27], and a study exploring the acceptability of hypothetical RM found that MSM from Iquitos preferred a RM with a higher volume compared to MSM in Lima [13]. None of the studies in Peru, however, are able to explain the reasons for the detected discrepancies and, together with the present study, underscore the need for further, comprehensive research into the specific sexual practices and beliefs among geographically diverse samples of Peruvian MSM and TW. Future, longitudinal studies specifically designed to explore rectal douching and its acceptability as an HIV prevention intervention should incorporate a qualitative component akin to the work by Carballo-Diéguez [18] and Shilder [29] wherein not only the details of the practice are explored but the meaning the practice holds with regard to sexual pleasure, shame, and HIV transmission are included, as well. We further emphasize the need to prospectively include TW in all HIV prevention research, including future douche/enema studies, as their risks and behaviors differ from those of MSM, with whom they are often grouped [23]. While our study did include TW separately from MSM, their small number hindered comparisons between groups; this should be addressed by oversampling TW participants in future studies.
In addition to the need for additional epidemiological, behavioral and sociocultural data related to douching and enema use by MSM and TW in the context of future HIV prevention interventions, there remains a more pressing issue of developing interventions that address the likely harm the practice itself causes. The rectum’s single-cell epithelium makes it easily damaged by douches/enemas [30], and even tap water alone can lead to rectal epithelia sloughing [31] which could explain the association of the practice not only with HIV, but with various STIs including lymphogranuloma venereum proctitis [32], hepatitis B [33] and C infection [34] and neisseria gonorrhoeae [35]. Moreover, among HIV-infected MSM, a trend (p = 0.07) towards an increased risk of high grade anal intraepithelial neoplasia with enema use has been observed among those using >50 enemas in their lifetime [36].
Enema use has also been posited to possibly facilitate HPV transmission, perhaps by the sharing of enema equipment with others [36], or perhaps by its association with condomless anal intercourse and practicing both insertive and receptive anal intercourse [20]. In our study, there is evidence of a positive correlation between the frequency of AI and douche use (those who reported AI ≥ 11 or more times were more likely to report douche use than those reporting AI 1 time). This finding could be important in the development of usage guidelines for a RM douche since some target users may already be using douches daily or several times a week raising questions regarding dosing (could it be possible to “overdose” on a RM douche?). Moreover, though not reaching statistical significance, among those reporting douching, nearly a quarter (24 %) also reported current anal symptoms.
Based on the limited but growing body of literature on rectal douching/enema, the message is clear: safe douching/enema use information not only needs to be developed in the context of a douche-formulated RM, but should be incorporated into HIV, STI and sexual health interventions for MSM and TW now. Noor’s [20] four potential directions for research (the effects of douching on rectal mucosa; the development of non-damaging enemas for AI; inclusion of data collection of recent enema use in HIV/STI sexual risk outcomes studies; and the development of consistent messaging for use of water-based lubricants and enemas) would be a major step forward. Even the dissemination of information to the lay-pubic regarding the association of enema use with STI would be a significant first step, along with the recommendation to avoid adding substances to tap-water enemas, since they are the most commonly used.
There were limitations in our study which could be addressed in future studies designed specifically to examine douching/enema use with a greater overall sample size. We embedded a brief subset of questions into a much larger questionnaire designed to measure unrelated outcomes which prevented including many other variables of interest. The larger study enrolled a convenience sample of HIV-uninfected MSM and TW, therefore by month 6 relatively fewer participants were infected with HIV (3 %) than we would have encountered had the douche questions been asked at the initial screening visit 6 months prior when 21 % of all those screened were HIV-infected [37] and limits our ability to measure the association of HIV and rectal douching. Missing data, particularly for factors such as transactional sex and condomless anal intercourse, is noted as a potential source of bias (obscuring potential associations between douching and other variables) and we cannot be sure that non-response was a random occurrence. Lastly, we re-emphasize that our sample was drawn only from Lima, the capital of Peru, and would be strengthened by the inclusion of study samples drawn from rural areas including the jungle and mountain regions.
Rectal douching prior to receptive AI is a common practice among MSM globally, and we present the strongest evidence to date that Peruvian MSM and TW also douche/use enemas much in the same way in terms of intent, product and apparatus as has been found in other studies. Development of a douche-formulated RM is currently underway [38] and the results from this study build on a body of evidence supporting the plausibility of their use among populations most at risk for HIV in Peru.
Conclusions
MSM and TW are in need of expanded HIV prevention interventions. Oral PrEP is effective and available (though currently only formally available in the U.S.) and hopefully a gel-based RM will also be found to be safe, efficacious and eventually effective in near future trials. A douche-based rectal microbicide could play an important role by providing another HIV prevention option for these highly vulnerable populations.
References
Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
McCormack S, Dunn D. Pragmatic open-label randomised trial of preexposure prophylaxis: the proud study [abstract 22LB]. Abstract presented at: Conference on Retroviruses and Opportunistic Infections (CROI); February 23–26, 2015; Seattle, Washington.
Grant RM, Anderson PL, McMahan VM, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820–9.
Molina JM, Capitant C, Charreau I, Spire B et al. On demand PrEP With Oral TDF-FTC in MSM: results of the ANRS Ipergay trial [abstract 23LB]. Abstract presented at: Conference on Retroviruses and Opportunistic Infections (CROI); February 23–26, 2015; Seattle, Washington.
Krakower DS, Mayer KH. Pre-exposure prophylaxis to prevent HIV infection: current status, future opportunities and challenges. Drugs. 2015;75(3):243–51.
Peinado J, Lama JR, Galea JT, et al. Acceptability of oral versus rectal HIV preexposure prophylaxis among men who have sex with men and transgender women in Peru. J Int Assoc Provid AIDS Care. 2013;12(4):278–83.
Gomez GB, Borquez A, Caceres CF, et al. The potential impact of pre-exposure prophylaxis for HIV prevention among men who have sex with men and transwomen in Lima, Peru: a mathematical modelling study. PLoS Med. 2012;9(10):e1001323.
Beyrer C, Sullivan P, Millett G, Sanchez J, et al. The increase in global HIV epidemics MSM. AIDS. 2013;27(17):2665–78.
Galea JT, Kinsler JJ, Imrie J, et al. Preparing for rectal microbicides: sociocultural factors affecting product uptake among potential South American users. Am J Public Health. 2014;104(6):e113–20.
Newman PA, Roungprakhon S, Tepjan S. A social ecology of rectal microbicide acceptability among young men who have sex with men and transgender women in Thailand. J Int AIDS Soc. 2013;1(16):18476.
Pines HA, Gorbach PM, Weiss RE, et al. Acceptability of potential rectal microbicide delivery systems for HIV prevention: a randomized crossover trial. AIDS Behav. 2013;17(3):1002–15.
Carballo-Diéguez A, Exner T, Dolezal C, Pickard R, Lin P, Mayer KH. Rectal microbicide acceptability: results of a volume escalation trial. Sex Transm Dis. 2007;34(4):224–9.
Kinsler JJ, Cunningham WE, Nureña CR, et al. Using conjoint analysis to measure the acceptability of rectal microbicides among men who have sex with men in four South American cities. AIDS Behav. 2012;16(6):1436–47.
Microbicide Trials Network. MTN-017: phase II safety and acceptability study of tenofovir gel reformulated for rectal use. http://www.mtnstopshiv.org/news/studies/mtn017/backgrounder. Accessed 5 June 2015.
Javanbakht M, Murphy R, Gorbach P, LeBlanc MA, Pickett J. Preference and practices relating to lubricant use during anal intercourse: implications for rectal microbicides. Sex Health. 2010;7(2):193–8.
Kinsler JJ, Galea JT, Peinado J, Segura P, Montano SM, Sánchez J. Lubricant use among men who have sex with men reporting receptive anal intercourse in Peru: implications for rectal microbicides as an HIV prevention strategy. Int J STD AIDS. 2010;21(8):567–72.
Carballo-Diéguez A, Bauermeister JA, Ventuneac A, Dolezal C, Balan I, Remien RH. The use of rectal douches among HIV-uninfected and infected men who have unprotected receptive anal intercourse: implications for rectal microbicides. AIDS Behav. 2008;12(6):860–6.
Carballo-Diéguez A, Bauermeister J, Ventuneac A, Dolezal C, Mayer K. Why rectal douches may be acceptable rectal-microbicide delivery vehicles for men who have sex with men. Sex Trans Dis. 2010;37(4):228–33.
Galea JT, Kinsler JJ, Imrie J, Nureña CR, Sanchez J, Cunningham WE. Rectal douching and implications for rectal microbicides among populations vulnerable to HIV in South America: a qualitative study. Sex Transm Infect. 2014;90(1):33–5.
Noor SW, Rosser BR. Enema use among men who have sex with men: a behavioral epidemiologic study with implications for HIV/STI prevention. Arch Sex Behav. 2014;43(4):755–69.
Javanbakht M, Stahlman S, Pickett J, LeBlanc MA, Gorbach PM. Prevalence and types of rectal douches used for anal intercourse: results from an international survey. BMC Infect Dis. 2014;14:95.
Beyrer C, Baral SD, van Griensven F, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380(9839):367–77.
Baral SD, Poteat T, Stromdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(3):214–22.
Beyrer C, Baral SD, Walker D, Wirtz AL, Johns B, Sifakis F. The expanding epidemics of HIV type 1 among men who have sex with men in low- and middle-income countries: diversity and consistency. Epidemiol Rev. 2010;32(1):137–51.
MINSA [Peruvian Ministry of Health]. Informe nacional sobre los progresos realizados en el país [National report on progress made in the country]. http://www.unaids.org/sites/default/files/en/dataanalysis/knowyourresponse/countryprogressreports/2014countries/PER_narrative_report_2014.pdf. Accessed 5 June 2015.
UNAIDS Peru country report 2013. http://www.unaids.org/en/regionscountries/countries/peru. Accessed 5 June 2013.
Kinsler JJ, Galea JT, Lama JR, et al. Rectal douching among Peruvian men who have sex with men, and acceptability of a douche-formulated rectal microbicide to prevent HIV infection. Sex Transm Infect. 2013;89(1):62.
Brown B, Davtyan M, Leon SR, et al. A prospective cohort study characterising the role of anogenital warts in HIV acquisition among men who have sex with men: a study protocol. BMJ Open. 2014;4(9):e005687.
Schilder A, Orchard TR, Buchner CS, Strathdee SA, Hogg RS. Insert discourse: rectal douching among young HIV-positive and HIV-negative men who have sex with men in Vancouver. Can Sex Cult. 2010;14(4):327–43.
Anton P, Herold BC. HIV transmission: time for translational studies to bridge the gap. Sci Transl Med. 2011;3(77):77ps11.
Schmelzer M, Schiller LR, Meyer R, Rugari SM, Case P. Safety and effectiveness of large-volume enema solutions. Appl Nurs Res. 2004;17(4):265–74.
de Vries HJ, van der Bij AK, Fennema JS, et al. Lymphogranuloma venereum proctitis in men who have sex with men is associated with anal enema use and high-risk behavior. Sex Trans Dis. 2008;35(2):203–8.
Schreeder MT, Thompson SE, Hadler SC, et al. Hepatitis B in homosexual men: prevalence of infection and factors related to transmission. J Infect Dis. 1982;146(1):7–15.
Ndimbie OK, Kingsley LA, Nedjar S, Rinaldo CR. Hepatitis C virus infection in a male homosexual cohort: risk factor analysis. Genitourin Med. 1996;72(3):213–6.
Heiligenberg M, Rijnders B, van der Loeff MFs, et al. High prevalence of sexually transmitted infections in HIV-infected men during routine outpatient visits in The Netherlands. Sex Trans Dis. 2012;39(1):8–15.
Richel O, De Vries HJ, Dijkgraaf MG, Van Noesel CJ, Prins JM. Risk factors for the presence of anal intraepithelial neoplasia in HIV+ men who have sex with men. PLoS One. 2013;8(12):e84030.
Galea JT, Kinsler JJ, Galan DB, et al. Factors associated with visible anogenital warts among HIV-uninfected Peruvian men who have sex with men and transwomen: a cross-sectional study. Sex Trans Dis. 2015;42(4):202–7.
Development of rectal enema as microbicide (DREAM). http://grantome.com/grant/NIH/U19-AI113127-01. Accessed 5 June 2015.
Acknowledgments
We are grateful to the men and women who participated in this study as well as the staff at the community center Epicentro in Lima, Peru where the study was conducted. This work was supported in part by a research grant from the Merck Investigator-Initiated Studies Program of Merck & Co., Inc., NIH grant T32 MH080634 and the NIH Health Disparities Research Loan Repayment Program. The opinions expressed in this paper are those of the authors and do not necessarily represent those of Merck & Co., Inc. We also thank the International Rectal Microbicides Advocates (IRMA) who provided access to the global rectal douching survey and allowed its modification for use in the present study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Galea, J.T., Kinsler, J.J., McLean, S. et al. Rectal Douching Prevalence and Practices Among Peruvian Men Who have Sex with Men and Transwomen: Implications for Rectal Microbicides. AIDS Behav 20, 2555–2564 (2016). https://doi.org/10.1007/s10461-015-1221-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1221-9