Abstract
Men who have sex with men (MSM) are the largest risk group in the US HIV epidemic and African American MSM (AA MSM) are disproportionately affected. Substance-abusing sexual minorities warrant attention as they are at elevated risk for HIV, yet are not a homogeneous risk group. The purpose of this study was to use latent class analysis to identify patterns of drug and alcohol use in a sample of 359 AA MSM and examine associations with sexual risk. Three classes were identified: Individuals who used multiple substances (poly-users) (18 %), alcohol/marijuana users (33 %) and individuals who had low probability of reporting drug or problematic alcohol use (50 %). Results from multivariate analysis indicate that poly-users were older and more likely to report sex exchange and recent sexually transmitted infection compared to the other classes. Alcohol and poly-users were more likely to report sex under the influence. Identifying and defining substance use patterns can improve specification of risk groups and allocation of prevention resources.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
African American men who have sex with men (AA MSM) are disproportionately affected by HIV, representing over one-third of new infections in the United States [1]. Drug and alcohol use is associated with poor HIV medical adherence and clinical outcomes [2, 3]. Substance- abusing sexual minorities are more likely to be untreated or under-utilize treatment [4] and may be a bridge to non-drug using populations [5]. However, substance-using MSM are not a homogeneous risk group [6]. For example, one study of young MSM in Chicago report three patterns of alcohol and substance use: individuals who used multiple substances including marijuana, alcohol and other drugs, individuals who used alcohol and marijuana only, and individuals who used low levels of marijuana only [7]. In a sample of Malaysian men, three patterns were also identified: negligible substance use, use of alcohol, poppers and ecstasy before sex and amphetamine-type stimulant use [8]. In samples of MSM, variability in drug use has been associated with sexual risk such as number of sex partners, unprotected sex and sexually transmitted infections [9, 10]. The majority of the studies focused on drug and alcohol use among MSM are focused on club drugs or prescription drug use and therefore are not generalizable to settings where use of these drugs are not prevalent.
Latent class analysis (LCA) [11] is a well-established statistical methodology which identifies subgroups with distinct behavioral or clinical characteristics in a population. A growing number of studies have applied LCA to elucidate classes in various public health related areas, including mental health [12] and substance use [13–19]. This technique has been used to examine drug use patterns in national epidemiologic samples of drug users [18]. LCA has the potential to identify types of substance-using MSM who have the greatest risk behaviors and therefore would benefit most from interventions. With limited funding and resources for providing treatment and interventions, LCA offers an empirical approach for maximizing intervention cost-effectiveness.
There are few studies that have addressed the heterogeneity of alcohol and drug use within the population of AA MSM and associations with sexual risk. The aims of this study were to (1) use LCA to empirically define and characterize drug and alcohol use patterns of a sample of AA MSM and (2) to examine differences in sexual risk by pattern of use.
Methods
Sample
Data for the current study comes from two convenience samples of AA MSM who were recruited and assessed using similar procedures. The Unity in Diversity study (UND) was a pilot HIV prevention intervention conducted in Baltimore from August 2007–August 2008 with a sample of high-risk AA MSM [20]. Social Geographies (SG) was an observational study conducted from March 2012–July 2012 that focused on examining the socio-spatial context of HIV risk among AA MSM in Baltimore [21]. For both studies, inclusion criteria were: (1) aged 18–55, (2) self-report African American/black ethnicity/race, and (3) self-report sex with another male in the prior 90 days. For the UND study addition inclusion criteria was self-report unprotected anal sex with a male partner in the prior 90 days and being willing to take an HIV test. Substance use, demographic and health data were collected in face-to face interviews by trained research staff. To maximize validity in reporting of stigmatized behaviors, sexual risk data was collected using audio-computer assisted self-interview technology. Data was missing on substance use for n = 10 participants, therefore the final sample for this study is 359. Table 1 presents a comparison between the two samples on demographic, substance use and sexual risk variables. Differences between the two samples were observed, therefore, study membership was included as a covariate in the multivariate model.
Measures
Substance Use Class
To conduct the LCA, six binary variables were included: self-reported heavy use of alcohol, binge drinking, crack, heroin, cocaine and marijuana in the prior 90 days. These were chosen based on the prevalence and variability of the responses in the substance use assessment. In both samples, use of methamphetamines was low (2 %). We did not assess club drug use in the SG study however, zero participants in the UND study reported club drug use.
Heavy alcohol use was assessed using the question, “How many drinks containing alcohol did you have when you were drinking in the past 90 days?” Heavy use was operationalized as drinking three or more alcoholic beverages in a typical day.
Binge drinking was operationalized as self-report of six or more alcoholic beverages in one sitting in the past 90 days.
Crack and heroin use was operationalized as using at least once weekly or more frequently in the past 90 days versus less often or no use.
Powdered cocaine and marijuana use was operationalized as any use in the prior 90 days.
Sexual Risk was assessed using items from the National Behavior Surveillance Survey [22]. Participants reported the total number of male sexual partners in the prior 90 days. Participants were then asked “Now I want you to think about the man you most recently had anal sex”. After answering questions about the most recent male partner, questions preceded to the next man the participant had recently had anal sex. This continued up to the third most recent partner, if that was applicable. For each male partner, participants indicated whether they considered the individual a main partner (yes or no). Participants were allowed to indicate that more than one individual was a main partner. Condom use during sex with each male partner was assessed for both insertive and receptive anal sex. First participants indicated the numbers of times they had insertive and receptive anal sex with each partner and then how many of those times a condom was used. Based on literature, that indicates condom use varies by main versus non-main partner, unprotected anal sex was operationalized based on partner-type separately for insertive and receptive sex (unprotected yes or no). Participants also reported whether money or drugs were exchanged during most recent anal sex (yes/no) with each male partner and a construct was created to indicate that they had exchanged with any of the male partners. Sex under the influence of alcohol or drugs was determined by asking two separate questions: “The last time you had sex with[partner] were you buzzed or drunk from alcohol?” and “had you used any drugs prior to anal sex?” An affirmative response to either question was coded as yes for the indicator variable: sex under the influence. Participants who reported more than three male partners were asked global questions on condom use (i.e. frequency of condom use across all remaining partners). This analysis only includes partner specific risk data.
Sexually Transmitted Infections
Participants indicated whether they had been “told by a doctor or other healthcare professional in the prior 90 days that they had any sexually transmitted infection, other than HIV” (yes or no).
Sexual identity was assessed with the question “Do you consider yourself to be heterosexual or straight; bisexual; queer; homosexual, gay or same-gender loving; not sure or questioning; or other?” Based on distribution of the responses a three-category construct was created where 0 = homosexual, gay, queer, same gender loving, 1 = bisexual and 2 = other (e.g. heterosexual, questioning/not sure).
HIV status was self-reported by participants in the Social Geographies study (positive, negative or unknown). Participants in the UNDwho reported negative or unknown status were tested using the Oraquick testing kit and those who reported HIV positive status provided documentation in the form of clinical lab results or medications.
Socio-demographics included self-reported age, highest educational attainment and annual income were self-reported. Employment status was categorized as not working, on disability, or working (full or part-time). Participants reported whether they currently had any health insurance.
Statistical Analysis
Latent Class Modeling
Latent class analysis [11] was used to empirically define subgroups based on individual substance use. LCA was performed using MPlus version 7.3 (Muthén & Muthén, 1998–2014). For all LCA models considered, the six binary substance use variables were included (heavy alcohol use, binge drinking, cocaine, crack, heroin, marijuana). An iterative modeling process was used to produce 2- through 5-class models. For each model, the analysis estimated (a) the percent of the total sample in each subgroup/class and (b) the conditional probability for each class that an individual in that particular class will give a positive response to each of the five items. We determined the number of classes that exist in the sample by [1] performing the analysis repeatedly, specifying an additional class each time, and [2] comparing the models with varying numbers of classes on measures of fit and interpretability of the results. Specifically, Bayesian information criteria (BIC), sample-size adjusted bayesian information criteria, and Akaike’s information criteria (AIC) were used to evaluate model fit. The best-fitting model is considered the one where BIC, sample size adjusted BIC, and AIC values are minimized [23]. Based on the LCA results, a three-categorical variable on class membership was created for further bivariate and multivariate analysis.
Comparisons by Substance Use Class
To compare variables by the LCA identified substance use classes, ANOVA was used for continuous variables and the Fisher’s Chi square for dichotomous variables. Two multinomial logistic regressions were then conducted to examine independent effects of variables that were statistically associated with substance use class from bivariate analysis, with statistical significance determined at the p < 0.05 level. The first regression model used the LCA identified light user class as the reference group and the second regression used the LCA identified alcohol/marijuana class as the reference group. Results are presented as relative risk ratios (RRR), estimating the risk (odds ratio) of class membership to one of the other LCA identified classes compared to the reference group. We conducted a sub-analysis of the 275 individuals who reported having insertive anal sex with a non-main partner to examine associations with unprotected insertive anal sex and LCA identified substance use class. In the multivariate model this risk variable was not statistically associated with substance use class and therefore not presented in the Table.
Results
Socio-demographics and Drug use Characteristics of the Samples
Table 1 presents comparisons of the UND and SG study samples by socio-demographic and drug use characteristics. Participants in the SG study were on average older (40.3 vs. 39.7 years) compared to the UND individuals. A greater proportion of the SG participants had health insurance (p = 0.03), were HIV negative (p < 0.01), identified as homosexual, gay or queer (p < 0.01) and reported heavy (p < 0.01) and binge alcohol use (p < 0.01) compared to UND. A greater proportion of UND reported any marijuana use compared to SG (p = 0.02). Based on these differences, study membership was included as a covariate in the multivariate model.
Latent Class Analysis
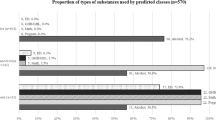
We estimated models of sub-groups of substance use classes among the men in the sample for one, two, and three classes. While the BIC was minimized in the two-class model, the AIC and sample size adjusted BIC were minimized in the three-class model. The three-class model also provided improved interpretation and therefore a three-class model was selected for the subsequent analysis. Based on the estimated model, class 1 made up 50 % (n = 175) of the sample, class 2—18 % (n = 65), and class 3—32 % (n = 119) of the sample (Fig. 1). In our study, the three-class LCA model yielded high entropy (0.81), and all the three latent classes have high correct classification rates (0.948, 0.858 and 0.811), suggesting modal class regression is appropriate.
No individuals in the sample reported zero use of both alcohol and marijuana. Membership to class one was composed of individuals who had 46 % probability of reporting any marijuana use, 18 % probability of heavy alcohol use and 8 % probability of binge drinking (herein class 1 will be referred to as light users). Class 2 consisted of individuals with high probabilities of heavy alcohol use (83 %) binge drinking (>92 %), crack (67 %) and marijuana (81 %), 28 % probability of heroin use and 48 % cocaine use (herein class 2 will be referred to as poly-users). Membership to class three was defined by high probability of heavy alcohol use (87 %), binge drinking (100 %) and marijuana use (68 %) and low probabilities of cocaine (11 %), crack (4 %) or heroin (1 %) (herein class 3 will be referred to as alcohol/marijuana).
Bivariate Analysis
Table 2 presents descriptive data on the pooled sample and bivariate comparisons of demographic and health variables by class. The majority of the sample had at least 12 years of education (61 %). Less than one-third was employed (28 %) and approximately one-third was not working due to disability (32 %). HIV status did not vary by class membership; 41 % of the sample was HIV positive. Overall, unprotected insertive anal sex with both main and non-main partners was prevalent (47 and 44 % respectively). Poly-users were on average older and a higher proportion of this class reported incarceration compared to light user and the alcohol/marijuana class. A smaller proportion of light users had health insurance compared to the other classes. There were no differences in sexual identity between classes.
Table 3 presents descriptive data and bivariate comparisons of sex risk variables by class. The majority reported two or more sexual partners in the prior 90 days. In unadjusted analyses several risk variables were significantly associated with class. A greater proportion of poly-users had exchanged sex for money or drugs with their most recent three male sex partners, had been diagnosed with an STI in the prior 90 days, reported sex while intoxicated and unprotected insertive anal sex with a non-main male partner, compared to the other two classes.
Comparisons Between the Alcohol/Marijuana Class Versus Light User Class
Controlling for study membership, the alcohol/marijuana class was younger (RRR = 0.97; 0.94–0.99) and had lower relative risk of having health insurance (RRR = 0.52; 0.30–0.92) compared to the light user class. However, the alcohol/marijuana class had higher relative risk having sex under the influence (RRR = 2.87; 1.27–11.5).
Comparisons Between the Poly-User Class and Other Classes
Controlling for study membership, compared to both light user and alcohol/marijuana class, poly-users had higher relative risk of being older, exchanging sex for money or drugs and having an STI in the prior 90 days. Additionally, when compared to light users, poly-users had high relative risk of recent incarceration (RRR = 2.26; 1.04–4.90) and sex under the influence (RRR = 4.45; 1.90–10.4). Compared to alcohol/marijuana class there were no statistical associations with having sex under the influence.
Discussion
In this study we sought to use latent class analysis to examine patterns of drug and alcohol use in a sample of sexually active AA MSM and to examine whether the patterns were associated with sexual risk behavior. Three distinct classes were derived lending support to other studies that have demonstrated heterogeneity of substance use within populations [24, 25]. By recognizing that there are different patterns of use, research can be more precise in identifying sub-groups who may be more vulnerable to poor health or treatment outcomes or at risk of transitioning to more severe/problematic use.
The second aim of this study was to examine whether sexual risk varied by substance use class. We were surprised that the number of total male sex partners and main male sex partners was not associated with substance use class. The majority of the men reported at least two partners in the prior 90 days. In part, this may be due to the inclusion criteria for Unity in Diversity (sex with at least two people, one of which must be a male) and therefore this may not be generalizable to all substance using AA MSM populations. However, unprotected anal sex rates were high for the entire sample for both main partner and non-main partner types. The literature is inconsistent on whether substance use is associated with having multiple sex partners and unprotected anal intercourse [24, 26–29]. Results from the present study suggest that substance use is not a determinant of these sexual specific risk factors.
Compared to light and alcohol/marijuana class, members of the poly-user class were older and had increased relative risk of exchanging sex for money or drugs and a recent STI. Having an STI is established as one of the key factors driving the disparity in HIV among AA MSM compared to other racial groups [30, 31]. Additionally, sex exchange for money or drugs has been found to play a unique role in both HIV and STI disease transmission to individuals who may be part of lower risk sexual networks [32–34]. Furthermore, when you compare poly-user class to light use class, the poly-user class had higher relative risk of incarceration and anal sex under the influence. It should be noted that this was the smallest of the three classes in this sample. Yet these findings underscore the need to integrate HIV prevention programs, and STI screening and clinical care, with substance abuse treatment programming [35, 36] and incarceration facilities to address their distinctive needs.
The class characterized by high probability of heavy and binge alcohol use and marijuana use accounted for one-third of this sample. Compared to light users variables associated with alcohol/marijuana class were lack of health insurance, younger age and greater odds of anal sex under the influence. The finding that both alcohol/marijuana and poly-user classes were significantly more likely to engage in sex under the influence is consistent with literature on the association between heavy and binge alcohol use and unprotected sex [26, 27]. The reduced rate of health insurance among this group may provide insight into the low rates of substance abuse treatment access and utilization, previously observed in this population [37, 38]. Interventions tailored for this group should focus on reducing episodes of heavy and binge drinking as an approach to reduce sex under the influence. There are a number of evidence-based approaches for alcohol use that could be integrated with HIV prevention [39].
The largest class of this sample, accounting for half, was characterized by their low probability of heavy or binge alcohol use and very low probability of crack, heroin or cocaine use. Individuals in this group had a 47 % probability of marijuana use. While this group of men is not characterized by risky or hazardous substance abuse, half of the men in this class reported sex under the influence with at least one of their most recent three male sex partners. The role of marijuana use as a risk factor for sexual risk has not received much attention. Given the prevalence of marijuana use [40], especially in younger populations, further research is needed. Moreover, over one-third of this group reported unprotected receptive anal sex with main partners and a quarter reported unprotected receptive anal sex with non-main partners. This is consistent with other studies that report greater condom use with casual partners compared to main [41, 42]. Feelings of trust and reliance on monogamy and therefore lower risk have been described as possible reasons for lower condom use in main partnerships [43, 44]. While interventions tailored to this group may not focus on reducing their overall level of substance use, our findings underscore the importance of addressing risks associated with sex under the influence and promoting frequent HIV and STI testing and behavioral skills to increase condom use for receptive anal sex
Limitations of this study should be noted. First, this study uses data from two samples that were recruited at two different time periods. Though they were assessed using similar methods, the samples differed in their drug and alcohol use and sexual risk. However, this diversity of substance use may improve the generalizability of the findings. On the other hand, the this study was conducted in a specific geographic location where rates of methamphetamine and club drug use is low and limits generalizability to areas that may have a different epidemiology of substance use [45]. The average age of this sample is 39 years and therefore may not generalize to younger MSM and the strict inclusion criteria may have excluded low frequency user. Further, this study asked men to identify “main” versus “non-main” partners. Research suggests that the personal meaning of this classification may differ widely among individuals, referring to a wide range of sexual partnerships potentially leading to mis-classification bias. Despite these limitations, this study offers a perspective of how HIV risk and substance use intersect, which has important implications for maximizing intervention cost-effectiveness by targeting specific substance using MSM groups. Additional research is needed to examine interactions among these three groups (via sex and drug and alcohol behaviors), as well as the overlap in their social networks and the stability of their sexual networks.
References
Centers for Disease Control and Prevention (CDC). Estimated HIV incidence among adults and adolescents in the United States, 2007–2010. HIV Surveillance Supplemental Report 2012;0017(No. 4).
Kader R, Govender R, Seedat S, Koch JR, Parry C. Understanding the impact of hazardous and harmful use of alcohol and/or other drugs on ARV adherence and disease progression. PLoS One. 2015;10(5):e0125088.
Parsons JT, Starks TJ, Millar BM, Boonrai K, Marcotte D. Patterns of substance use among HIV-positive adults over 50: implications for treatment and medication adherence. Drug Alcohol Depend. 2014;139:33–40.
McCabe SE, West BT, Hughes TL, Boyd CJ. Sexual orientation and substance abuse treatment utilization in the United States: results from a national survey. J Subst Abuse Treat. 2013;44:4.
Lambert E, Normand J, Stall R, Aral S, Vlahov D. Introduction: new dynamics of HIV risk among drug-using men who have sex with men. J Urban Health. 2005;82(1 Suppl 1):i1–8.
Finlayson T, Le B, Smith A, Bowles K, Cribbin M, Miles I, et al. HIV risk, prevention, and testing behaviors among men who have sex with men-National HIV Behavioral Surveillance System, 21 U.S. Cities, United States, 2008. MMWR Surveill Summ. 2011;60(14):1–38.
Newcomb ME, Ryan DT, Greene GJ, Garofalo R, Mustanski B. Prevalence and patterns of smoking, alcohol use, and illicit drug use in young men who have sex with men. Drug Alcohol Depend. 2014;1(141):65–71.
Lim SH, Cheung DH, Guadamuz TE, Wei C, Koe S, Altice FL. Latent class analysis of substance use among men who have sex with men in Malaysia: findings from the Asian internet MSM sex survey. Drug Alcohol Depend. 2015;151:31–7.
Colfax G, Coates TJ, Husnik MJ, Huang Y, Buchbinder S, Koblin B, et al. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. J Urban Health. 2005;82(1 Suppl 1):i62–70.
Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, et al. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr. 2007;45(1):85–92.
McCutcheon A. Latent class analysis. Newbury Park: Sage; 1987.
Olino TM, Klein DN, Lewinsohn PM, Rohde P, Seeley JR. Latent trajectory classes of depressive and anxiety disorders from adolescence to adulthood: descriptions of classes and associations with risk factors. Compr Psychiatry. 2010;51(3):224–35.
Monga N, Rehm J, Fischer B, Brissette S, Bruneau J, El-Guebaly N, et al. Using latent class analysis (LCA) to analyze patterns of drug use in a population of illegal opioid users. Drug Alcohol Depend. 2007;88(1):1–8.
Kuramoto SJ, Bohnert AS, Latkin CA. Understanding subtypes of inner-city drug users with a latent class approach. Drug Alcohol Depend. 2011;118(2–3):237–43.
Ko JY, Martins SS, Kuramoto SJ, Chilcoat HD. Patterns of alcohol-dependence symptoms using a latent empirical approach: associations with treatment usage and other correlates. J Stud Alcohol Drugs. 2010;71(6):870–8.
Wittchen HU, Behrendt S, Hofler M, Perkonigg A, Rehm J, Lieb R, et al. A typology of cannabis-related problems among individuals with repeated illegal drug use in the first three decades of life: evidence for heterogeneity and different treatment needs. Drug Alcohol Depend. 2009;102(1–3):151–7.
Sherman SG, Sutcliffe CG, German D, Sirirojn B, Aramrattana A, Celentano DD. Patterns of risky behaviors associated with methamphetamine use among young Thai adults: a latent class analysis. J Adolesc Health. 2009;44(2):169–75.
Agrawal A, Lynskey MT, Madden PAF, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: results from the national epidemiological survey on alcohol and related conditions. Addiction. 2007;102(1):94–104.
Carlson RG, Wang J, Falck RS, Siegal HA. Drug use practices among MDMA/ecstasy users in Ohio: a latent class analysis. Drug Alcohol Depend. 2005;79(2):167–79.
Tobin KE, Kuramoto SJ, German D, Fields E, Spikes P, Patterson J, et al. Unity in Diversity: results of a randomized clinical culturally tailored pilot HIV prevention intervention trial in Baltimore, MD, for African American men who have sex with men. Health Educ Behav. 2012;40:286.
Tobin KE, Takahashi LM, Cutchin M, Holtgrave D, Latkin C. Exploring the Social Geographies of African American Men who have Sex with Men, Baltimore, Maryland. Programs and abstracts of the National HIV Prevention Conference; August 14–17 Atlanta, GA: The National HIV Prevention Conference; 2011.
Pollack LM, Osmond DH, Paul JP, Catania JA. Evaluation of the center for disease control and prevention’s HIV behavioral surveillance of men who have sex with men: sampling issues. Sex Transm Dis. 2005;32(9):581–9.
Schwartz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–4.
Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16:1–17.
Santos GM, Coffin PO, Das M, Matheson T, DeMicco E, Raiford JL, et al. Dose-response associations between number and frequency of substance use and high-risk sexual behaviors among HIV-negative substance-using men who have sex with men (SUMSM) in San Francisco. J Acquir Immune Defic Syndr. 2013;63(4):540–4.
Boone MR, Cook SH, Wilson P. Substance use and sexual risk behavior in HIV-positive men who have sex with men: an episode-level analysis. AIDS Behav. 2013;17(5):1883–7.
Kahler CW, Wray TB, Pantalone DW, Kruis RD, Mastroleo NR, Monti PM, et al. Daily associations between alcohol use and unprotected anal sex among heavy drinking HIV-positive men who have sex with men. AIDS Behav. 2014;19:422.
Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48(2–3):218–53.
Mustanski B. Moderating effects of age on the alcohol and sexual risk taking association: an online daily diary study of men who have sex with men. AIDS Behav. 2008;12(1):118–26.
Sexton J, Garnett G, Rottingen JA. Metaanalysis and metaregression in interpreting study variability in the impact of sexually transmitted diseases on susceptibility to HIV infection. Sex Transm Dis. 2005;32(6):351–7.
Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999;75(1):3–17.
Jeffries WL 4th. Beyond the bisexual bridge: sexual health among U.S. men who have sex with men and women. Am J Prev Med. 2014;47(3):320–9.
Gorbach PM, Murphy R, Weiss RE, Hucks-Ortiz C, Shoptaw S. Bridging sexual boundaries: men who have sex with men and women in a street-based sample in Los Angeles. J Urban Health. 2009;86(Suppl 1):63–76.
Tobin KE, Latkin CA. An examination of social network characteristics of men who have sex with men who use drugs. Sex Transm Infect. 2008;84(6):420–4.
Kurtz SP, Stall RD, Buttram ME, Surratt HL, Chen M. A randomized trial of a behavioral intervention for high risk substance-using MSM. AIDS Behav. 2013;17(9):2914–26.
Higa DH, Crepaz N, Marshall KJ, Kay L, Vosburgh HW, Spikes P, et al. A systematic review to identify challenges of demonstrating efficacy of HIV behavioral interventions for gay, bisexual, and other men who have sex with men (MSM). AIDS Behav. 2013;17(4):1231–44.
Morgan O, Kuramoto F, Emmet W, Stange JL, Nobunaga E. The impact of the affordable care act on behavioral health care for individuals from racial and ethnic communities. J Soc Work Disabil Rehabil. 2014;13(1–2):139–61.
Lo CC, Cheng TC. Racial/ethnic differences in access to substance abuse treatment. J Health Care Poor Underserved. 2011;22(2):621–37.
Santos GM, Coffin PO, Vittinghoff E, DeMicco E, Das M, Matheson T, et al. Substance use and drinking outcomes in personalized cognitive counseling randomized trial for episodic substance-using men who have sex with men. Drug Alcohol Depend. 2014;1(138):234–9.
Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use: 1975-2014: overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; 2015.
Hensel DJ, Rosenberger JG, Novak DS, Reece M. Sexual event-level characteristics of condom use during anal intercourse among HIV-negative men who have sex with men. Sex Transm Dis. 2012;39(7):550–5.
Mimiaga MJ, Reisner SL, Cranston K, Isenberg D, Bright D, Daffin G, et al. Sexual mixing patterns and partner characteristics of black MSM in Massachusetts at increased risk for HIV infection and transmission. J Urban Health. 2009;86(4):602–23.
Adams J, Neville S. Men who have sex with men account for nonuse of condoms. Qual Health Res. 2009;19(12):1669–77.
Bauermeister JA, Carballo-Dieguez A, Ventuneac A, Dolezal C. Assessing motivations to engage in intentional condomless anal intercourse in HIV risk contexts (“Bareback Sex”) among men who have sex with men. AIDS Educ Prev. 2009;21(2):156–68.
Young SD, Shoptaw S. Stimulant use among African American and Latino MSM social networking users. J Addict Dis. 2013;32(1):39–45.
Acknowledgments
This research was supported by funding from the National Institute on Drug Abuse (1R03DA035696) and the National Institute on Alcohol Abuse and Alcoholism (R00AA020782). The authors thank Sharif Braxton for his assistance with references and manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is not being considered elsewhere for publication, nor has it been previously published. This manuscript has been read and approved by all the authors.
Rights and permissions
About this article
Cite this article
Tobin, K.E., Yang, C., King, K. et al. Associations Between Drug and Alcohol Use Patterns and Sexual Risk in a Sample of African American Men Who Have Sex with Men. AIDS Behav 20, 590–599 (2016). https://doi.org/10.1007/s10461-015-1214-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1214-8