Abstract
HIV continues to disproportionately affect men who have sex with men (MSM). Depression and substance use have been shown to be risk factors of partner violence among male same-sex couples. However, research exploring the risk factors for partner violence victimization after HIV disclosure among MSM is limited. The aim of this study was to determine the association between depressive symptoms, substance use, and disclosure-associated verbal and/or physical violence from a partner among MSM. Data were obtained from 340 HIV-positive MSM. Multivariable logistic regression was used to determine the associations between Center for Epidemiologic Studies-Depression and substance use scores, and disclosure-associated partner violence. After adjusting for age and income, every one-unit increase in substance use scores resulted in a 9 % (OR 1.09; 95 % CI 1.01–1.16) increase in the odds of disclosure-associated partner violence. HIV disclosure interventions for MSM populations should address substance use and potential violence from partners after disclosure.
Resumen
El VIH continúa afectando de una manera desproporcionada a los hombres que tienen sexo con hombres (HSH). Se ha demostrado que la depresión y el uso de drogas son factores de riesgo en la violencia de pareja (VP) de HSH. Sin embargo, las investigaciones que exploran los factores de riesgo en la VP después del revelamiento del seroestatus de VIH entre HSH es muy limitada. El objetivo de esta investigación fue explorar la asociación entre los síntomas de depresión, el uso de drogas, y la VP después del revelamiento del seroestatus entre HSH. Los datos fueron obtenidos de 340 hombres HSH VIH-positivos. Las asociaciones entre las puntaciones del CES-D (Center for Epidemiologic Studies-Depression Scale), y el uso de drogas y la VP después del revelamiento fueron exploradas con una regresión logística multivariante. Después de ajustar por la edad y el ingreso, cada puntuación del uso de drogas fue asociada con un aumento de 9 % (OR = 1.09; 95 % CI: 1.01–1.16) en la probabilidad de la VP después del revelamiento. Las intervenciones del revelamiento de seroestatus para HSH deberían abordar el uso de drogas y la prevención de la VP después del revelamiento.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
HIV continues to disproportionately affect men who have sex with men (MSM) compared to any other group globally [1] and in the US [2]. MSM populations represent about 2 % of the US population but account for approximately six in ten (63 %) of the estimated new infections in the US and close to eight in ten (78 %) of all men who have been newly diagnosed with HIV [2]. In 2011, the majority of persons living with HIV were MSM who were also injection-drug users [2]. With the high rates of HIV among MSM populations, disclosure of HIV status to partners becomes an integral factor in the prevention and treatment of HIV [3].
Disclosure of HIV status to partners may have numerous benefits. Increasing awareness of risk may help to motivate partners to seek HIV testing, reduce risky sexual behaviors, and decrease HIV transmission [4]. Benefits to the individual who discloses may include social, physical, psychological dividends [5] such as social support, better access to HIV treatment and care, and increased opportunities to discuss the reduction of HIV risk with partners [4]. Nevertheless, the decision to disclose HIV status to partners may have implications in all arenas of life [6]. The consequences theory of HIV disclosure states that people with HIV are likely to disclose their status to partners if the benefits or rewards for disclosing their status outweigh the costs or risks [5]. Costs may include valuable things that are given up for a reward of greater or equal value, or consequences that would be otherwise avoided [5], such as blame, abandonment, discrimination, disruption of relationships, and physical and/or emotional abuse [4].
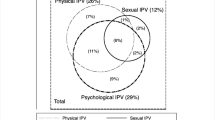
Partner violence continues to be a major public health problem in the US [7]. Violence between partners is not only a public health issue among heterosexual couples but also among same-sex couples [7, 8], and is sometimes found to be more prevalent among same-sex couples compared to heterosexual couples [9–11]. Among younger populations with same-sex partners, partner violence is also commonplace with one in four adolescents from a population-based sample reporting partner violence victimization, and approximately one in ten reporting physical partner violence [12]. Among a sample of MSM in the Chicago area, approximately 32 % reported partner violence, 21 % reported a history of verbal abuse, 19 % reported physical abuse and 19 % reported sexual abuse. The majority of men reporting any partner violence reported experiencing more than one type of partner violence [13], which highlights the interconnectivity of different forms of partner violence. Among a probability-based sample of MSM living in four US cities (Chicago, Los Angeles, New York, and San Francisco), 34 % reported psychological partner violence, 22 % reported physical partner violence and 5 % reported sexual partner violence [9]. Risky sexual behavior, such as unprotected anal sex [13], younger age [9], lower education level [9], being HIV-positive [9], experiencing depression [13] and substance abuse [13, 14] have been shown to be risk factors for partner violence among MSM populations.
The association between depressive symptoms, substance use and partner violence is complex. Several studies have shown a link between depression [15, 16], substance use and abuse [17–20], and other mental health disorders [21, 22] and partner violence among men and women. However, specifically among MSM couples, methamphetamine use, rock or crack cocaine use, and heavy drinking have been associated with partner violence victimization and aggression [14]. Alcohol intoxication, substance use problems including substance use with sex, hard drug use, and mental health diagnoses (including depression, bipolar disorder, and any psychiatric/emotional disorders) have also been associated with partner violence among MSM populations [13].
Theoretically, the psychoactive effects from the use of substances, such as impaired judgment, and having depressive symptoms may be related to partner violence victimization associated with HIV disclosure in a number of ways. Impairment from substance use may result in poorly timed or inappropriately delivered information on HIV serostatus to a partner based on poor judgement. For example, being under the influence of substances is likely to prohibit the accurate reading of a partner’s possible negative reaction to such sensitive information. It is equally likely that cognitive impairment may lead to the inability to leave a violent situation. Depressive symptoms may be associated with disclosure-associated partner violence due to the indifference a person may feel towards leaving a violent situation. For example, a history of depression may be associated with placing elevated focus on a maintenance of a relationship with a partner [23], albeit casual. As a result, an individual may be more willing to tolerate violence [23] from his partner.
As previously stated, one potential cost of disclosing HIV status to a partner is violence. Theoretically, among individuals with casual sex partners, the violence that may occur after disclosing their serostatus could be due to a reaction out of fear from their sex partners that they were put at risk of contracting HIV and even more so fearful that transmission of HIV may have occurred. Nevertheless, research focusing on HIV-disclosure associated partner violence tend to concentrate on women. These studies have shown that women experience abuse (sexual, physical and/or emotional) directly related to HIV disclosure or that occurred only after their HIV serostatus was disclosed [3, 24–27]. For example, Shamu and colleagues [3] explored disclosure-associated partner violence among pregnant women in Harare, Zimbabwe and showed that gender inequity, history of partner violence, risky sexual behaviors were associated with partner violence after HIV disclosure. Positive HIV status was linked to partner violence and negative reactions by male partners immediately after disclosing HIV status [3]. Among this population, the study showed the interconnectivity of partner violence, HIV status and HIV disclosure. Populations at risk for partner violence tend to be the same groups at risk for HIV infection [26]. However, studies examining risk factors for violence associated with disclosure of HIV status among sexual minority populations are lacking. Research exploring the interconnectivity between depressive symptoms, substance use and partner violence after HIV disclosure specifically among MSM populations is extremely limited. To our knowledge, no study has examined potential risk factors for partner violence associated with HIV disclosure among sexual minority populations. The objective of this study was to explore the association between depressive symptoms, substance use, and verbal and/or physical abuse by a partner associated with disclosure of HIV status among MSM. Determination of risk factors for violence associated with disclosure of HIV status to partners is crucial. As a result, public health practitioners, and health care providers of MSM populations living with HIV may be aware of these factors, and incorporate the necessary resources to address the interconnectivity of depressive symptoms, substance use and abuse associated with disclosure of status to partners, especially among MSM populations. We hypothesize that men who abuse substances and/or have depressive symptoms may be more likely to experience violence after disclosing their HIV status to their partners.
Methods
Data were obtained from 340 participants at the baseline assessment of a longitudinal randomized-controlled trial of an intervention designed to assist HIV-positive MSM in disclosing their serostatus to casual sex partners. This disclosure intervention study was conducted across two metropolitan statistical areas (MSA; Columbus, Ohio and Tampa, Florida) from December, 2009 through December, 2014 and consisted of participants who were HIV-positive, at least 18 years old, were sexually active, had two or more partners in the last 12 months (at least one of which was a man), and indicated an interest in learning more about disclosing their serostatus to sexual partners. In addition, men were English speaking and planned on living in the MSA for at least 1 year. Separate IRB approval was garnered for both recruitment locations and participants were treated in accordance with the “Ethical Principals of Psychologists and Code of Conduct” [28].
Study Participants and Recruitment
The average age of participants (n = 340) was 42.1 years (SD = 11.0 years). The average time since diagnosis was 13.6 years (SD = 8.3 years). Self-reported sexual orientation was mostly gay (n = 267, 78.5 %), and 74.4 % (n = 253) indicated that they had sex only with men. Most participants reported being single (n = 238, 70 %). Across study sites, there were statistically significant differences by age where the mean age of men from Tampa was 44.5 years (SD = 10.3 years) and from Columbus, 39.5 years (SD = 11.2 years). There were also statistically significant differences in substance use scores where the mean score among men from Tampa was 13.0 (SD = 5.7) and from Columbus, 14.9 (SD = 5.7). There were no statistically significant differences by income, race/ethnicity, educational level, employment status, mean Center for Epidemiologic Studies-Depression (CES-D) scores and partner violence status.
Participants were recruited in several ways. First, individuals were recruited through advertising efforts with local/state AIDS service organizations (ASOs). Caseworkers were informed about the study and handouts were made available to distribute to potential participants or through newsletters and direct mailings. ASOs also featured calls for participation on their websites, and sent materials to clients for recruitment efforts. Recruitment materials were also placed at HIV-related venues and forums held throughout the MSAs, and at local eating and drinking establishments. Finally, advertisements were placed in local daily newspapers.
Data Collection
Prior to randomization, participants completed a baseline questionnaire administered using audio-computer assisted self-interviewing (ACASI). Social desirability has been identified as a potential problem in the collection of reliable data on serostatus disclosure [29, 30]. However, ACASI has been demonstrated to be associated with more complete reporting of potentially stigmatized drug, sex and HIV risk behaviors [31, 32]. Additionally, ACASI has been both accepted and preferred as a method of data collection by participants in HIV risk-related studies [32]. Data were collected on person-level characteristics (i.e., items and scales asked only once for each participant) and encounter-level characteristics (i.e., repeated measures for each participant). Person-level items included measures of demographic characteristics, global sexual/disclosure activities (i.e., count measures of specific activities during the prior 30 days), and measures relevant to sexual activity/disclosure.
Measures
Verbal and/or Physical Abuse Associated with Disclosure
Verbal and/or physical abuse associated with disclosure was measured using a single item: “In the last 30 days, how many times were you verbally or physically abused by a partner after disclosing?” Approximately 99.4 % of participants (338/340) answered this item, with responses ranging from 0 to 10, with an average of 0.19 times.
Depressive Symptoms
Depressive symptoms were measured using the CES-D Mood [33] scale, which is a 20 item scale used to measure depressive symptoms in the general population. Items were scored using a 4-point Likert-type scale with values ranging from Rarely or None of the time (0) to Most or All of the time (3). Scores were summed to arrive at an overall score with values ranging from 0 to 60, with higher scores indicative of more depressive symptoms. The CES-D was chosen because of its good reported internal consistency (α = 0.85) and validity [33]. Depressive symptoms were also examined as a binary variable to determine participants who were at risk for clinical depression (CES-D ≥ 16) [34]. For the current study, the standardized Cronbach’s α for the CES-D was 0.94.
Substance Use
To assess substance use participants completed the substance use items of the Substance Abuse and Mental Illness Symptoms Screener (SAMISS) [35]. These seven items inquired about participants’ frequency, amount, and perceived problematic use of alcohol, illicit drugs, and prescription drugs and were summed to derive an overall substance abuse score. For most of the items, a Likert-type response scale ranging from Never (1) to 4 or more times a week (5) was used. Specific items were then summed to determine whether the participant was considered positive for substance use problems if their score exceeded a specified threshold [35]. For the current study, the standardized Cronbach’s α for the SAMISS was 0.77.
Potential Confounders
Confounders considered were shown to be associated with depression and substance use, and partner violence based on literature review a priori. Statistically significant differences in sociodemographic characteristics such as age [36–38] and income [37] are associated with depression. Substance use has also been shown to differ by age [39–44] and income [41, 43]. Previous studies have shown differences in age [45, 46] and income [45, 47] to be linked to partner violence. Therefore, the current study considered age (continuous) and monthly income ($0–$500, $501–$1000, ≥$1001) as potential confounders.
Analytic Approach
Participants were excluded if they were missing on all depressive symptoms, substance use, and partner violence questions (n = 2). The resultant sample size was 338.
Descriptive statistics were used to determine the distribution of sociodemographic characteristics among men reporting and not reporting partner violence after HIV disclosure. Two sets of multivariable logistic regression models were used to obtain adjusted odds ratios and 95 % confidence intervals depicting the association between depressive symptoms, substance use, and partner violence after disclosure of HIV status. Each confounder was placed in different models with depressive symptoms, and substance use as separate exposure variables, and partner violence victimization after disclosure as the outcome. However, no confounder changed the effect estimate between depressive symptoms, substance use and partner violence victimization >10 %. Nevertheless, adjusted models were still examined as recent research has recommended that potential confounding variables should not be discarded based on a lack of change in estimates but should still be included in the model based on theoretical evidence [48]. As a result, three nested models were used for each exposure measure: (1) an unadjusted model, (2) a model adjusted for age, and (3) a model adjusted for age and income. Exact logistic regression was used to assess the association between depressive symptoms and substance use as binary variables (where more information would be lost compared to analyzing them as continuous scores), and verbal and/or physical abuse associated with HIV disclosure. All analyses were performed with SAS software Version 9.4 (SAS Institute, Cary, NC).
Results
The distribution of sociodemographic characteristics, verbal and/or physical abuse by an intimate partner, depressive symptoms, and substance use among the study population overall, and by partner violence status are presented in Table 1. In the past 30 days, 6.2 % of the population reported partner violence victimization after disclosing their HIV serostatus to a partner. Approximately six in ten respondents were at risk for clinical depression (58.6 %) and seven in ten reported substance use (72.2 %). The mean score for depressive symptoms was 20.4 (SD = 13.3) and the mean substance use score was 13.9 (SD = 5.8). Seven in ten (71.4 %) respondents reporting verbal and/or physical abuse by a partner and close to six in ten (57.7 %) not reporting disclosure-associated partner violence in the past 30 days were at risk for clinical depression. Approximately 90.5 % of the sample reporting disclosure-associated partner violence and 71.0 % of the sample not reporting disclosure-associated partner violence met the Whetten criteria [34] for substance use. Mean CES-D scores were 27.6 (SD = 13.7) and 20.0 (SD = 13.1) for participants reporting disclosure-associated partner violence and not reporting disclosure-associated partner violence, respectively. Mean substance use scores were 17.5 (SD = 6.7) among victims of disclosure-associated partner violence in the past 30 days and 13.7 (SD = 5.7) among participants not reporting disclosure-associated partner violence.
Logistic regression analyses depicting the association between depressive symptoms and substance use sum scores, and verbal and/or physical abuse by a partner associated with disclosure in the past 30 days are shown in Table 2. Separate crude models show that for every one-unit increase in depressive symptoms and substance use scores, there was a 4 % increase (OR 1.04; 95 % CI 1.01–1.08) and 10 % increase (OR 1.10; 95 % CI 1.03–1.18) in the odds of reporting verbal and/or physical abuse by a partner after disclosing HIV serostatus, respectively. In other words, the more someone was depressed or increased their substance use, the likelihood of experiencing verbal and/or physical abuse by a partner after disclosing their HIV status increased 4 and 10 %, respectively. After adjusting for age and income, the relationship between depressive symptoms and disclosure-associated partner violence was attenuated so that the confidence intervals included unity (OR 1.03; 95 % CI 0.99–1.07). However, the association between substance use and disclosure-associated partner violence remained statistically significant (OR 1.09; 95 % CI 1.01–1.16).
Table 3 shows the results of exact logistic regression analyses depicting the association between being at risk for clinical depression, and substance use, and verbal and/or physical abuse by a partner after disclosing serostatus in the past 30 days. There were no statistically significant associations.
Discussion
This study is the first to demonstrate an association between depressive symptoms, substance use, and experiencing verbal and/or physical abuse associated with disclosure of HIV serostatus. In the full models, substance use scores were statistically significantly associated with disclosure-associated partner violence, but no statistically significant relationship was seen between depressive symptoms and disclosure-associated partner violence. Associations between binary representations of being at risk for clinical depression, substance use and disclosure-associated partner violence were not statistically significant.
The results from the current study depicting a relationship between substance use and disclosure-associated partner violence support findings from previous researchers examining the link between substance use and partner violence, and confirms part of our hypothesis. Wu et al. showed that substance use, specifically heavy drinking and methamphetamine use, was linked to partner violence among Black MSM throughout the relationship period and in the past month [14]. However, the same study found that cocaine use was statistically significantly associated with lifetime partner violence but not partner violence in the past month. Tran et al. found that substance use, including ecstasy, cocaine, and methamphetamine use, was also linked to partner violence among Asian/Pacific Islander MSM [49]. The lack of statistically significant associations between substance use as a binary variable and disclosure-associated partner violence could have been due to the small cell sizes as a result of the small number of participants reporting verbal and/or physical abuse associated with disclosure in the past 30 days. Categorizing continuous variables into binary variables may result in loss of information, which in this case, due to small numbers, may also contribute to failure to reject the null hypothesis.
Substance use may be associated with verbal and/or physical abuse by a partner after disclosure for a number of reasons. As previously theorized, substance use may be associated with disclosure-associated partner violence due to psychoactive effects of substance use and/or abuse leading to impaired judgment; and/or the inability to leave a violent situation. Therefore, men with substance use may be more likely to be vulnerable and more susceptible to verbal and/or physical abuse by a partner after disclosing their HIV serostatus compared to men who do not use substances.
Depressive symptoms were not statistically significantly associated with verbal and/or physical abuse by a partner after disclosure, which contradicts our hypothesis. This finding suggests that depressive symptoms might not play a role in disclosure-associated partner violence from casual partners among MSM. The current findings contradicts other studies, which have shown that depressive symptoms are associated with partner violence [13, 15, 16, 50]. Nevertheless, these studies examined depression and partner violence among women [50, 51], and heterosexual couples [16]. This difference in findings could be due to differences in study populations. Houston and McKirnan examined risk factors of intimate partner abuse among MSM and found that substance abuse and depression were associated with sexual and/or physical and/or verbal abuse [13]. However, their study examined sexual, physical and verbal abuse, not associated with disclosure of HIV status.
The findings of this study should be considered with some limitations. First, the total sample size was small with only 21 respondents responding to experiencing verbal and/or physical abuse by a partner after HIV disclosure in the past 30 days. As a result, large confidence intervals were obtained for analyses examining depressive symptoms and substance abuse as binary variables, and results implied that the null hypothesis could not be rejected. Also, due to the small sample size, the most parsimonious model (adjusting for age and income) was used and did not include other covariates in the model. We did not adjust for other sociodemographic characteristics, and for substance use when using depressive symptoms as an outcome, or for depressive symptoms when using substance use as the outcome. Indeed, adjusting for one factor, which is the outcome in another model with the same confounders may lead to circular analysis [52]. Second, verbal and/or physical abuse by a partner associated with HIV disclosure was only reported in the past 30 days. Disclosure-associated partner violence in the past month may not be representative of partner violence after disclosure at other time points. Varying relationships have been found between substance use and partner violence during the relationship period and partner violence in the past-month [14]. Third, it is possible that there may be shifts in the impact of variables or intervening variables over the study period (2009–2014). As a result, relationships among variables may change overtime. Therefore, longitudinal studies collecting data on depressive symptoms and substance use with follow-up data collection on partner violence are warranted to help to mitigate the shifts in variable impact that may change overtime in a cross-sectional study design, and to compare to findings seen in the current study. Fourth, the relationship between depressive symptoms, substance use, and partner violence may have differed across study sites. Indeed, substance use was statistically different across study sites. However, we were unable to determine differences and/or similarities in relationships across study sites due to the small number of participants reporting verbal and/or physical abuse from a partner. Fifth, the question asking study participants about disclosure-associated partner violence did not ask for information on sexual violence, which has been linked to alcohol and drug problems through posttraumatic stress symptom severity [53], and to depression through avoidance coping [54].
Nevertheless, the current study had several strengths. This study was the first to examine the association between depressive symptoms, substance use, and disclosure-associated violence among MSM. Depressive symptoms and substance use were operationalized as binary and continuous variables. These definitions allowed for analysis of binary variables based on previously defined thresholds, and of continuous variables so as not to lose any information in analysis. Next, nested models accounting for multiple potential confounders were used. The use of nested models helps to determine the change in effect estimates depending on what confounders were adjusted for at each stage. A final strength of this study was the use of exact logistic regression models. This technique accounted for the small cell sizes in models using the binary variables for depressive symptoms and substance use for analysis.
Conclusions
HIV disclosure interventions geared towards MSM populations should include resources to address substance use and partner violence victimization. Nevertheless, the findings also suggest that interventions for substance use should also address verbal and/or physical abuse by a partner associated with disclosure of HIV status among MSM populations. Health care providers, especially for populations living with HIV, should also be aware of the association between substance use and disclosure-associated violence so they may provide resources addressing not only substance use, but also violence prevention to persons who want to disclose their status to an intimate partner. Given the prevalence of substance use and depressive symptoms experienced by MSM (as demonstrated in this sample), the inclusion of these variables in future studies with this population is warranted. In light of the current study findings, future researchers should address the link between other mental health measures such as anxiety, PTSD, and disclosure-associated violence victimization among MSM populations. Future researchers may also wish to assess partner violence experienced over time, specifically include sexual violence as part of their measures, and use larger sample sizes when possible.
References
UNAIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. 2013. http://www.unaids.org/sites/default/files/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf. Accessed 29 May 2015.
Centers for Disease Control and Prevention (CDC). HIV among gay/bisexual men. 2015. http://www.cdc.gov/hiv/risk/gender/msm/facts/index.html. Accessed 24 Mar 2015.
Shamu S, Zarowsky C, Shefer T, Temmerman M, Abrahams N. Intimate partner violence after disclosure of HIV test results among pregnant women in Harare, Zimbabwe. PLoS One. 2014;9(10):e109447.
Maman S, Medley A. Gender dimensions of HIV status disclosure to sexual partners: rates, barriers and outcomes. A review paper. World Health Organization. 2004. http://www.who.int/gender/documents/en/genderdimensions.pdf. Accessed 25 Mar 2015.
Serovich JM. A test of two HIV disclosure theories. AIDS Educ Prev. 2001;13(4):355–64.
Serovich JM, Craft SM, Reed SJ. Women’s HIV disclosure to family and friends. AIDS Patient Care STDS. 2012;26(4):241–9.
Centers for Disease Control and Prevention (CDC). Injury prevention & control: divison of violence prevention: intimate partner violence. 2014. http://www.cdc.gov/violenceprevention/intimatepartnerviolence/. Accessed 24 Mar 2015.
Burke LK, Follingstad DR. Violence in lesbian and gay relationships: theory, prevalence, and correlational factors. Clin Psychol Rev. 1999;19(5):487–512.
Greenwood GL, Relf MV, Huang B, Pollack LM, Canchola JA, Catania JA. Battering victimization among a probability-based sample of men who have sex with men. Am J Public Health. 2002;92(12):1964–9.
Owen SS, Burke TW. An exploration of prevalence of domestic violence in same-sex relationships. Psychol Rep. 2004;95(1):129–32.
Tjaden P, Thoennes N, Allison CJ. Comparing violence over the life span in samples of same-sex and opposite-sex cohabitants. Violence Vict. 1999;14(4):413–25.
Halpern CT, Young ML, Waller MW, Martin SL, Kupper LL. Prevalence of partner violence in same-sex romantic and sexual relationships in a national sample of adolescents. J Adolesc Health. 2004;35(2):124–31.
Houston E, McKirnan DJ. Intimate partner abuse among gay and bisexual men: risk correlates and health outcomes. J Urban Health. 2007;84(5):681–90.
Wu E, El-Bassel N, McVinney LD, et al. The association between substance use and intimate partner violence within Black male same-sex relationships. J Interpers Violence. 2015;30(5):762–81.
Kim J, Lee J. Prospective study on the reciprocal relationship between intimate partner violence and depression among women in Korea. Soc Sci Med. 2013;99:42–8.
Vaeth PA, Ramisetty-Mikler S, Caetano R. Depression among couples in the United States in the context of intimate partner violence. J Interpers Violence. 2010;25(5):771–90.
Feingold A, Capaldi DM. Associations of women’s substance dependency symptoms with intimate partner violence. Partn Abuse. 2014;5(2):152–67.
Nowotny KM, Graves JL. Substance use and intimate partner violence victimization among White, African American, and Latina women. J Interpers Violence. 2013;28(17):3301–18.
Peters EN, Khondkaryan E, Sullivan TP. Associations between expectancies of alcohol and drug use, severity of partner violence, and posttraumatic stress among women. J Interpers Violence. 2012;27(11):2108–27.
Walton MA, Cunningham RM, Chermack ST, Maio R, Blow FC, Weber J. Correlates of violence history among injured patients in an urban emergency department: gender, substance use, and depression. J Addict Dis. 2007;26(3):61–75.
Iverson KM, McLaughlin KA, Gerber, et al. Exposure to interpersonal violence and its associations with psychiatric morbidity in a U.S. national sample: a gender comparison. Psychol Violence. 2013;3(3):273–87.
Schneider R, Burnette ML, Ilgen MA, Timko C. Prevalence and correlates of intimate partner violence victimization among men and women entering substance use disorder treatment. Violence Vict. 2009;24(6):744–56.
Barnett OW. Why battered women do not leave, Part 2: external inhibiting factors—social support and internal inhibiting factors. Trauma Violence Abuse. 2001;2(1):3–35.
Gielen AC, O’Campo P, Faden RR, Eke A. Women’s disclosure of HIV status: experiences of mistreatment and violence in an urban setting. Women’s Health. 1997;25(3):19–31.
Gielen AC, McDonnell KA, Burke JG, O’Campo P. Women’s lives after an HIV-positive diagnosis: disclosure and violence. Matern Child Health J. 2000;4(2):111–20.
Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, O’Campo P. HIV/AIDS and intimate partner violence: intersecting women’s health issues in the United States. Trauma Violence Abuse. 2007;8(2):178–98.
Koenig LJ, Whitaker DJ, Royce RA, et al. Violence during pregnancy among women with or at risk for HIV infection. Am J Public Health. 2002;92(3):367–70.
American Psychological Association. Ethical principles of psychologists and code of conduct. Am Psychol. 1992;47:1597–611.
Simoni JM, Pantalone DW. Secrets and safety in the age of AIDS: does HIV disclosure lead to safer sex? Top HIV Med. 2004;12(4):109–18.
Simoni JM, Pantalone DW. HIV disclosure and safer sex. In: Kalichman SC, editor. Positive prevention: reducing HIV transmission among people living with HIV/AIDS. New York: Kluwer Academic/Plenum; 2005.
Des Jarlais DC, Paone D, Milliken J, et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet. 1999;353(9165):1657–61.
Perlis TE, Des Jarlais DC, Friedman SR, et al. Audio-computerized self-interviewing versus face-to-face interviewing for research data collection at drug abuse treatment programs. Addiction. 2004;99(7):885–96.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Lewinson PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies-Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12:277–87.
Whetten K, Reif S, Swartz M, et al. A brief mental health and substance abuse screener for persons with HIV. AIDS Patient Care STDs. 2005;19(2):89–99.
Dipnall JF, Pasco JA, Meyer D, et al. The association between dietary patterns, diabetes and depression. J Affect Disord. 2015;174:215–24.
Do AN, Rosenberg ES, Sullivan PS, et al. Excess burden of depression among HIV-infected persons receiving medical care in the United States: data from the medical monitoring project and the behavioral risk factor surveillance system. PLoS One. 2014;9(3):e92842.
Khan AY, Carrithers J, Preskorn SH, et al. Clinical and demographic factors associated with DSM-IV melancholic depression. Ann Clin Psychiatry. 2006;18(2):91–8.
Barnes GM, Welte JW, Hoffman JH, Tidwell MC. Gambling, alcohol, and other substance use among youth in the United States. J Stud Alcohol Drugs. 2009;70(1):134–42.
Becerra BJ, Becerra MB, Gerdine MC, Banta JE. Religion, acculturation, and incarceration: determinants of substance use among Hispanic adults in the United States. J Environ Public Health. 2014;2014:459596.
Becker WC, Sullivan LE, Tetrault JM, Desai RA, Fiellin DA. Non-medical use, abuse and dependence on prescription opioids among U.S. adults: psychiatric, medical and substance use correlates. Drug Alcohol Depend. 2008;94(1–3):38–47.
Blazer DG, Wu LT. Patterns of tobacco use and tobacco-related psychiatric morbidity and substance use among middle-aged and older adults in the United States. Aging Ment Health. 2012;16(3):296–304.
Lemke S, Schaefer JA. VA nursing home residents with substance use disorders: mental health comorbidities, functioning, and problem behaviors. Aging Ment Health. 2010;14(5):593–602.
Webb, Vanable PA, Carey MP, Blair DC. Cigarette smoking among HIV+ men and women: examining health, substance use, and psychosocial correlates across the smoking spectrum. J Behav Med. 2007;30(5):371–83.
Brown MJ, Weitzen S, Lapane KL. Association between intimate partner violence and preventive screening among women. J Womens Health (Larchmt). 2013;22(11):947–52.
Palmetto N, Davidson LL, Breitbart V, Rickert VI. Predictors of physical intimate partner violence in the lives of young women: victimization, perpetration, and bidirectional violence. Violence Vict. 2013;28(1):103–21.
Cohen MM, Forte T, Du Mont J, Hyman I, Romans S. Adding insult to injury: intimate partner violence among women and men reporting activity limitations. Ann Epidemiol. 2006;16(8):644–51.
Lee PH. Should we adjust for a confounder if empirical and theoretical criteria yield contradictory results? A simulation study. Sci Rep. 2014;4:6085.
Tran A, Lin L, Nehl EJ, Talley CL, Dunkle KL, Wong FY. Prevalence of substance use and intimate partner violence in a sample of A/PI MSM. J Interpers Violence. 2014;29(11):2054–67.
de Fonseca-Machado MO, Alves LC, Monteiro JC, et al. Depressive disorder in pregnant Latin women: does intimate partner violence matter? J Clin Nurs. 2015;24(9–10):1289–99.
Kim-Godwin YS, Maume MO, Fox JA. Depression, stress, and intimate partner violence among Latino migrant and seasonal farmworkers in rural Southeastern North Carolina. J Immigr Minor Health. 2014;16(6):1217–24.
Kriegeskorte N, Simmons WK, Bellgowan PS, Baker CI. Circular analysis in systems neuroscience: the dangers of double dipping. Nat Neurosci. 2009;12(5):535–40.
Jaquier V, Flanagan JC, Sullivan TP. Anxiety and posttraumatic stress symptom pathways to substance use problems among community women experiencing intimate partner violence. Anxiety Stress Coping. 2015;28(4):445–55.
Flanagan JC, Jaquier V, Overstreet N, Swan SC, Sullivan TP. The mediating role of avoidance coping between intimate partner violence (IPV) victimization, mental health, and substance abuse among women experiencing bidirectional IPV. Psychiatry Res. 2014;220(1–2):391–6.
Acknowledgments
This study was supported by funding from the National Institute of Mental Health (R01MH082639). We would like to thank the men who participated in this study. We would also like to thank Ms. Milagro Porter for edits made to the Spanish version of the abstract.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brown, M.J., Serovich, J.M. & Kimberly, J.A. Depressive Symptoms, Substance Use and Partner Violence Victimization Associated with HIV Disclosure Among Men Who have Sex with Men. AIDS Behav 20, 184–192 (2016). https://doi.org/10.1007/s10461-015-1122-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1122-y