Abstract
Concerns that standard didactic adherence counselling may be inadequate to maximise antiretroviral therapy (ART) adherence led us to evaluate more intensive individualised motivational adherence counselling. We randomised 297 HIV-positive ART-naïve patients in Durban, South Africa, to receive either didactic counselling, prior to ART initiation (n = 150), or an intensive motivational adherence intervention after initiating ART (n = 147). Study arms were similar for age (mean 35.8 years), sex (43.1 % male), CD4+ cell count (median 121.5 cells/μl) and viral load (median 119,000 copies/ml). Virologic suppression at 9 months was achieved in 89.8 % of didactic and 87.9 % of motivational counselling participants (risk ratio [RR] 0.98, 95 % confidence interval [CI] 0.90–1.07, p = 0.62). 82.9 % of didactic and 79.5 % of motivational counselling participants achieved >95 % adherence by pill count at 6 months (RR 0.96, 95 % CI 0.85–1.09, p = 0.51). Participants receiving intensive motivational counselling did not achieve higher treatment adherence or virological suppression than those receiving routinely provided didactic adherence counselling. These data are reassuring that less resource intensive didactic counselling was adequate for excellent treatment outcomes in this setting.
Resumen
La inquietud de que la terapia didáctica de adherencia estándar pudiera ser inadecuada para maximizar la adherencia al tratamiento antiretroviral (ART), nos llevó a evaluar la terapia motivacional individualizada. Aleatorizamos 297 pacientes HIV-positivos sin ART previo en Durban, Sudáfrica, para recibir, ya sea terapia didáctica antes del inicio del ART (n = 150), o terapia motivacional intensiva después de iniciado el ART (n = 147). Los brazos del estudio fueron similares en edad (promedio 35.8 años), sexo (43.1 % hombres), recuento de células CD4+ (mediana 121.5 células/μl) y carga viral (mediana 119,000 copias/ml). La supresión virológica a los nueves meses se logró en el 89.8 % de los participantes que recibieron terapia didáctica y en 87.9 % de aquellos en terapia motivacional (riesgo relativo [RR] 0.98, 95 % intervalo de confianza [CI] 0.90–1.07, p = 0.62). 82.9 % de los participantes bajo terapia didáctica y 79.5 % de los tratados con terapia motivacional alcanzaron >95 % de adherencia por cuenta de píldoras a los seis meses (RR 0.96, 95 % CI 0.85–1.09, p = 0.51). Los participantes que recibieron terapia motivacional intensiva no mostraron una mayor adherencia al tratamiento o supresión virológica que aquellos bajo terapia didáctica rutinaria. Estos resultados son tranquilizadores ya que muestran que la menos costosa terapia didáctica es adecuada en este escenario.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2007, at the start of this study, it was estimated that South Africa had 5.7 million human immunodeficiency virus (HIV)-infected people [1] with approximately 1,700 new infections daily [2] highlighting the growing importance of determining the best way to optimise HIV treatment. Since the introduction of combination antiretroviral therapy (ART), HIV disease has changed from being a predictor of a certain death, to a manageable chronic illness if the treatment is taken as prescribed [3, 4]. This means ensuring the highest levels of treatment adherence, usually at least 95 % of medication taken as prescribed [5–7].
Due to the high burden of both tuberculosis (TB) and HIV in South Africa, the development of active TB is often the first sign of underlying HIV infection and an important trigger for HIV testing and possible ART initiation [8]. This was thought to be an efficient patient identification strategy at a time when the voluntary HIV testing rate among otherwise healthy people was very low [9]. There were concerns that integrating HIV and TB treatment, with higher pill burden and potential for side effects, might require additional adherence support, and require tailored adherence motivation counselling as TB treatment is for a defined period of time whereas HIV requires life-long therapy. In the light of this, the Centre for the AIDS Programme of Research in South Africa (CAPRISA) established a programme of research into integrating TB and HIV treatment and care in 2002 in Durban, South Africa.
Interventions to Enhance Adherence to ART
Early reviews were key in the conceptualisation of the current study. An initial overview of published adherence research indicated that adherence was inconsistently measured, and that most studies were conducted without control groups which resulted in inconclusive evidence [10]. A further review of 21 intervention studies up to the end of January 2003, concluded that only four studies were randomised controlled trials (RCTs), and that most were underpowered but that some studies suggested positive outcomes, which justified additional research [11]. A research synthesis of 24 intervention trials between 1996 and 2004 [12] confirmed that interventions that targeted participants with known adherence problems had a larger effect than those that did not.
A major review of RCTs published between 1996 and 2005 identified 19 studies that looked at behavioural interventions to enhancing adherence to ART [7]. In terms of interventions, 55 % used one-on-one counselling, and 16 % used group counselling, mostly delivered by health practitioners such as doctors or nurses (47 %) and mental health professionals (26 %), and 53 % of the studies used trial staff rather than routine clinical staff. Data from 14 RCTs included were analysed assessing the effect of adherence interventions on viral load between 2 weeks and 6 months post-intervention. It was found that 62 % of the intervention arm participants controlled their virus, versus 55 % of the participants in the control arm. This gives a fairly weak aggregate effect size (OR = 1.25, 95 % CI 0.99–1.59, N = 1247). Although the evidence against the null was not conclusive, the percentage of participants in the intervention arm that had undetectable viral load versus those in the control arm could translate into significant financial and health-systems benefits.
This review also reported 18 trials where the outcome was expressed as effect on adherence (the majority of studies measured adherence by self report, between 2 weeks and 6 months post-intervention), and in this case 62 % of participants in the intervention arm and 50 % of participants in the control arm achieved at least 95 % adherence [7]. This resulted in stronger evidence against the null and a stronger aggregated effect size (OR = 1.5, 95 % CI 1.16–1.94, N = 1633). This larger effect for adherence is not likely to be due to unreliable measurement by self-report, as effect sizes were actually larger in studies that used more objective measures (e.g. electronic monitoring). Thus, participants in the intervention arm were 1.5 times more likely to be 95 % or more adherent, and 1.25 times more likely to achieve suppressed viral load than participants in the control arm. This effect tended to be greater in studies that provided information on ART and interactive discussions regarding the cognitions, motivation, and participant expectations. Although it is inherently problematic to combine the diverse outcomes from studies with very different interventions and designs, this was the first attempt to synthesise the RCT outcome data and it was cautiously optimistic about the ability of behavioural interventions to enhance ART and strongly in favour of additional, rigorous assessment of adherence interventions by RCT, especially in Africa [13].
During the development of the intervention for the current study, we made a site visit to Harlem Hospital, and the ‘medication manager’ adherence intervention developed and being tested there was observed, and the approach modified and assimilated into the intervention being developed for our study [14]. The medication manager provided personalised adherence support to participants, using a standard assessment protocol to identify and address any deficits in adherence information, motivation and behavioural skills. The primary endpoint was time to first virologic failure, defined as the first plasma viral load above 2,000 copies/ml on or after the 4th monthly follow-up visit. In the main intention to treat analysis, the medication manager group had 13 % lower rate of first virological failure, but this was not statistically significant. Participants in the medication manager arm also had significantly raised CD4 counts (mean difference of 22.5 cells/μl higher), and better long-term adherence by self-report. This study provided some evidence that the approach of using a theory-based model to identify and correct specific deficits in information, motivation and behavioural skills with counselling techniques based on motivational interviewing (MI) was feasible, and showed promise in enhancing adherence and treatment outcomes on ART.
In summary, the literature indicated that counselling interventions, based on models of behaviour change, that provided participant-specific problem-solving and interactive sessions, seemed to be most likely to have an effect on improving ART adherence [7, 10, 11, 15, 16]. The motivation, information and behavioural skills model tied to MI had been used and evaluated in the USA in ART adherence, with some preliminary indications that this may be a fruitful avenue for further research [14, 17–19]. ART adherence in the context of TB treatment was identified as a key data gap that needed to be addressed, as integrated treatment was not the recommended standard of care.
To address our concerns about the adequacy of standard didactic counselling in our setting, we conducted a RCT to assess whether intensive individualised motivational adherence counselling led to better adherence and treatment outcomes than standard didactic counselling in newly diagnosed HIV infected patients initiating antiretroviral therapy.
Methods
Study Design and Setting
The study was a parallel group (1:1 ratio), open-label randomised controlled trial, with concealment of allocation from the person conducting the enrolment. It was conducted at the CAPRISA eThekwini HIV-TB clinic, in Durban, South Africa. This research facility adjoins to the Prince Cyril Zulu Communicable Diseases Centre, one of the biggest TB outpatient treatment clinics in South Africa.
Participants
Between August 2007 and February 2009, we recruited participants 18 years of age or older and eligible to initiate ART (at the time, a CD4 T cell count of 350 or less). The majority of these participants were also included in a study of the optimal time to initiate ART in patients who were receiving TB treatment [20, 21]. Just over 53 % of participants were receiving TB treatment at the time of their participation in this study, and a further 25.6 % had completed TB treatment within 4 weeks previous to initiation on ART (described further in Table 1 of the results).
ART Regimen
The ART regimen used was selected to be compatible with TB treatment [21]. The first line regimen offered, free of charge, was a once-a-day regimen consisting of enteric-coated didanosine (250 mg if <60 kg, 400 mg if >60 kg), lamivudine 300 mg, and efavirenz 600 mg (or, nevirapine (200 mg twice a day) in the case of pregnancy).
Adherence Counselling
Tuberculosis treatment adherence support was provided separately from the HIV treatment programme. This TB treatment service was provided by the Department of Health, according to the provincial standard of care, and was not under the control or provision of study staff, although completion of the required number of TB drug doses and outcomes of TB treatment were assessed as part of the TB and HIV treatment integration studies underway at the clinic.
The standard HIV treatment adherence support counselling for this programme was delivered by a nongovernmental organisation, consistent with the requirements in the initial South African national guidelines for treatment provision for adolescents and adults [22], the World Health Organization (WHO) guidelines for scaling up ART in resource-constrained settings [23], and with the US Department of Health and Human Services guidelines [24]. The counselling focussed on treatment literacy, and was delivered in an educational, or didactic, style. The counselling was seen as essential for treatment readiness, and so focussed on preparation prior to ART initiation. No formal counselling post-initiation of ART was specified, although on-going monitoring of adherence was recommended. We were concerned that this approach to adherence support may become less effective over time, as counselling group size increased, and the didactic approach might be prone to rote repetition of information with inadequate engagement with the individual issues faced by patients.Footnote 1
Procedures
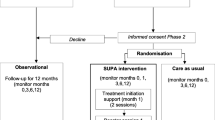
On determination of ART eligibility, all patients received two pre-initiation 20-45 min didactic counselling sessions as standard at the clinic. At the time of the ART initiation visit, patients were consented, enrolled and randomised. The randomisation was set up by a statistician using a random number generator in SAS, and the randomisation codes contained in sequentially numbered, sealed opaque envelopes, stratified in blocks of four or six relative to time of TB treatment (described in the baseline characteristics table of the results). The didactic arm participants received the final 20–45 min didactic counselling session only. The motivational counselling arm participants instead received the first 30–40 min individualised motivational counselling session, and then the additional four individualised motivational counselling sessions at intervals up to 6 months after initiation of therapy (Fig. 1). All participants were followed up to at least 9 months on treatment. Participants still in care had viral load measures taken at 12 months. Adherence was assessed by clinic-based pill count at 6 months post-initiation of therapy.
Content and Delivery of the Standard Didactic Counselling
The standard didactic counselling consisted of three sessions. The first session covered stigma and discrimination, nutrition and taking control of the treatment regimen. The second session focused on HIV pathogenesis, routes of infection, HIV testing techniques, and a basic introduction to ART. The final session focused on information relating to ART, the drug regimen, the importance of adherence, side effects, and the importance of monitoring and the development of resistance. Due to the large numbers of participants expected to be enrolled into the treatment programme, with increasing pressure to meet the high treatment initiation targets, this counselling was designed to be delivered in groups if necessary. Two sessions could be provided on the same day, but not all three.
Content and Delivery of the Individualised Motivational Counselling
An individualised intensive motivational adherence counselling intervention was developed, using content based on the information, motivation and behavioural skills model (IMB) of adherence to ART [25–27], using counselling delivery techniques from MI [28, 29]. The counselling was designed to be provided exclusively on a one-to-one basis, using a client-centred rather than didactic approach. Counselling could be tailored to specific participant needs, promoting an experience that was supportive of individualised care.
Motivational interviewing was developed initially to treat alcohol abuse, and it is amenable to brief counselling sessions [30]. MI is directive in the sense that the counsellor pursues the goal of examining and resolving ambivalence about behaviour change, but also client-centred in that it was designed to elicit statements in favour of behaviour change from the clients themselves [29, 30]. A review of trials of MI-based interventions in diverse settings, concluded that this approach was more effective than traditional advice giving [31]. Although MI was not formally used in our study, the motivational counselling did use techniques based on this approach. For example, instead of informing participants about potential barriers to adherence, and associated solutions, the counsellors encouraged them to think about potential barriers to adherence in their own experience and encouraged participants to talk about, and opt for, solutions that they felt they could implement in their own lives. As the statements about barriers requiring potential behaviour change were made by the participants, and the solutions also suggested by them, these counselling sessions were expected to be self-motivating. Participants were more likely to take ownership of their adherence challenges and successfully enact solutions they had suggested.
According to the IMB model of HIV prevention, initiating and maintaining patterns of HIV preventative behaviour depends on individuals being well informed, highly motivated and in possession of effective behavioural skills, rather than solely on the possession of knowledge. Content for the individualised motivational counselling was identified from this model, specifically a version modified for ART adherence [27], a literature review of adherence barriers, reasons for non-adherence from our clinic patients, and interviews with adherence counsellors and pharmacy staff.
Information was provided on the regimen, correct dosing, identifying and coping with side effects, as well as key information on non-adherence and resistance. Personal motivation was enhanced through MI-based techniques. Social motivation was encouraged through managed disclosure, designed to bring about gradual and safe disclosure over the first 6 months of treatment. Specific behavioural skills were encouraged, including skills to ensure clinic visits were kept, integrating dosing into the routine of daily life, and for identifying and coping with side effects. Moderating factors like general psychological well being, unstable living conditions, and substance or alcohol abuse were address through referrals to appropriate services.
The content of the motivational counselling was displayed on table top flipchart folders in English and isiZulu, the main local language, with locally relevant imagery like a three legged cooking pot to aid understanding and retention, facing the participants. Counselling scripts, based on MI techniques, faced the counsellors. The slogans summarised key principles like “The Power of Three” (the regimen of three drugs) and “The System of Three” (three important strategies for taking the drugs correctly). Additional support materials included wall posters for summarising counselling content, symptom solution cards that included key slogans and side effect management strategies, ‘prescriptions’ for adherence that were participant-agreed commitments to behaviours necessary to adhere optimally, as well as a treatment plan card that included pictures of the drugs in the regimen and space for a concrete plan for integrating dosing into daily routine. The ‘prescriptions’ and treatment plan cards were prepared at the first counselling visit, and reviewed and amended over the course of the intervention.
Two health educators from the existing nursing staff were trained to administer motivational counselling. On the day of treatment initiation participants were counselled on preparing to take ART, especially identifying managing side effects, and this was followed up at week two with a session on adjusting to ART medications. At 2 and 3 months, sessions were conducted dealing with on-going treatment issues and managed disclosure. At month six, participants were counselled on lifelong therapy concerns.
In accordance with standard clinic practice, and essential to adequate standard of care, once initiated on treatment all participants could receive additional ad hoc counselling support, on the basis of increasing viral load, decreasing CD4 count, missing doses (either by self-report or pill count), or when the participants account of their treatment behaviour did not make sense. To provide this, the standard didactic counselling session three was repeated as required in both study arms.
Study Outcomes
The primary outcome was the proportion of participants with suppressed viral load (plasma viral load of <400 copies/ml, HIV-1 RNA-PCR—Roche diagnostics) at 9 months (range of 8–10 months) post-initiation of ART. A secondary outcome looked at adherence by pill count over the previous inter-visit period at 6 months post-initiation of therapy. Pill count was expressed as a percentage of the pills taken as prescribed over the study visit interval (usually the previous 28 days), by assuming that all non-returned pills had been taken over the study visit interval. These data were verified from the clinic records based on previous study visit and drugs dispensed by the pharmacy. This measure was recorded at 6 months, as this was part of the counselling intervention study follow-up. Suppressed viral load at 12 months was assessed as an additional secondary outcome.
As early mortality is common in treatment programmes in this region [32, 33], deaths prior to 3 months were not considered as contributing to the primary outcome as they occurred too early for treatment adherence to have an impact, and these participants were excluded from all analyses. Participants who died after 3 months, but prior to 9 months, were considered to have unsuppressed viral load in the analysis.
Sample Size and Statistical Analysis
The individualised motivational counselling was hypothesised to be superior as it was more intensive, and provided individually in a client-centred and participatory way. From data available during planning, we estimated that we would need at least 150 evaluable outcomes in each arm at 9 months, for the study to have 80 % power to detect an absolute difference of at least 15 % in suppressed viral load, estimating 65 % suppressed in the didactic counselling arm, with a type 1 error of 5 %.
As odds ratios exaggerate the magnitude of association for common events [34], and as viral load suppression was high in this study, the primary outcome was assessed using risk ratios with 95 % confidence intervals (CIs). As no adjustment was necessary for the outcomes, no regression model was needed to estimate the risk ratios. All analyses were performed using the STATA 11.0 statistical analysis program (College Station, Texas 77845, USA).
Restricted and Whole Cohort Analysis
In the first instance, each analysis was restricted to all participants with outcome data at 6, 9 and 12 months respectively, including those who died after 3 months who were considered to have unsuppressed viral load. To determine the impact of the lost, withdrawn from the treatment programme, or relocated participants, and those otherwise with missing data, whole cohort analysis was performed where those with no outcome data were assumed not to have confirmed suppressed viral load or adherence greater than 95 %.
Ethics
This study was approved by the Biomedical Research Ethics committees of the University of KwaZulu-Natal, Durban (E326/05), The London School of Hygiene and Tropical Medicine, London (5114), and, Columbia University, New York (IRB-AAAC0202). The trial was registered Clinicaltrials.gov (NCT00408642) on the South African National Health Research Ethics Council (NHREC) trials register (DOH-27-0807-2004).
Results
297 ART naïve patients were eligible and all consented to be enrolled, 150 randomised to the didactic and 147 in the individualised motivational counselling arm (Fig. 2). All participants were followed up and analysed in the arms into which they were randomised. Baseline demographic and clinical characteristics were similar in both groups (Table 1).
Follow-up to 9 Months
Ten (3.4 %) of the 297 participants died prior to 3 months and were excluded from all outcome analyses (Fig. 2). Of the remaining 287, eight (2.7 %) were lost to follow-up, three (1.0 %) had withdrawn from the treatment programme, six (2.0 %) had defaulted treatment, seven (2.4 %) were known to have relocated and 11 (3.7 %) were missing viral loads or had missed their visit. 250 (84.2 %) had viral load measures, and two (0.7 %) had died between 3 and 9 months. 229 (77.1 %) participants, 117 in the didactic and 112 in the motivational counselling arm, had recorded adherence measures at 6 months.
Intervention Coverage
All participants in the didactic counselling arm had to have documented evidence of having completed the standard adherence support programme as this was a requirement prior to initiation on ART. Of the 131 participants from the individualised motivational counselling arm in follow-up for at least 6 months and, therefore, expected to have completed five sessions, 97.7 % (128/131) completed at least three and 88.5 % (116/131) completed all five sessions.
Ad hoc Counselling Support
During the course of the study there were 101 recorded instances of ad hoc adherence counselling for 49 study participants. 71 of these instances occurred in the 31 didactic counselling participants, versus only 30 sessions in 18 of the motivational counselling participants (Mann–Whitney p = 0.04). One participant in the didactic counselling arm accounted for five of these sessions, and another for eight.
Reasons for repeat adherence counselling referral were captured in 99 of cases (Table 2). The most frequent reason given for referring a participant for ad hoc counselling was that the incorrect number of pills was returned at the study visit, slightly more frequent in the didactic counselling arm. Participants in the didactic counselling arm were also more than twice as likely to have been referred for poor knowledge of drug dosing instructions. However, there is no evidence that reasons for referral differed by counselling type (Fisher’s exact p = 0.89).
Primary Outcome: Suppressed Viral Load at 9 Months
A total of 252 participants were included in the restricted analysis; 250 with viral load measures at 9 months, and two participants (one in each arm) who died between 3 and 9 months. By 9 months, suppressed viral load was achieved in 89.8 % (115/128) of the participants in the didactic counselling arm and in 87.9 % (109/124) of participants in the motivational counselling arm (RR = 0.98; 95 % CI 0.90–1.07, p = 0.62) (Table 3). In the whole cohort analysis, suppressed viral load was achieved in 78.8 % (115/146) of the participants in the didactic, and in 77.3 % (109/141) of the motivational counselling arm (RR = 0.98; 95 % CI 0.87–1.11, p = 0.76).
In predetermined exploratory analysis (not shown here), adjustment for gender, age, employment status, education level, relationship status, point of HIV treatment initiation in relation to TB treatment, viral load and CD4 count by log binomial regression [35] had no major impact on the primary outcome of the trial.
Secondary Outcome 1: ≥95 % Adherence by Pill Count at 6 Months
In the restricted analysis, 82.9 % (97/117) of those in the didactic and 79.5 % (89/112) of the individualised motivational counselling arm participants had a pill count greater than 95 % (RR = 0.96; 95 % CI 0.85–1.09, p = 0.51). In the whole cohort analysis, 66.4 % (97/146) in the didactic arm versus 63.1 % (89/141) of those in motivational arm had adherence ≥95 % (RR = 0.95; 95 % CI 0.80–1.13, p = 0.56).
Secondary Outcome 2: Suppressed Viraemia at 12 Months
As part of clinical follow-up of all retained participants, viral load data were available for 247 participants at 12 months post-initiation of therapy. Of those who provided data, 91.1 % (112/123) in the didactic and 87.9 % (109/124) in the motivational counselling arm had suppressed viral load (RR = 0.97; 95 % CI 0.89–1.05, p = 0.42). In the whole cohort analysis, 76.7 % (112/146) in the didactic versus 77.3 % (109/141) in the motivational arm had suppressed viral load (RR = 1.0; 95 % CI 0.89–1.14, p = 0.91).
Discussion
In our trial, ART-naïve participants who received intensive individualised motivational counselling did not have improved viral suppression or adherence outcomes. Exposure to the motivational counselling was high, and poor coverage was not likely to be a factor. Viral suppression was high in both groups. While the 252 participants with treatment outcome at 9 months assessed in the restricted analysis was below the target of 300 evaluable participants, the whole cohort analysis of all 297 participants did not lead to materially different trial outcomes.
Treatment outcome data from the southern Africa region at the time of this study help to contextualise the results (Table 4). These data, mostly from other well-resourced treatment trials, seem to also show good outcomes. However, significant losses to follow up and early mortality are masked as most results are given for ‘on treatment’ participants. Where an intention to treat estimate is given, the result is much poorer [36], highlighting the good outcome in our current study. Including data from other southern African countries, which also includes real-world clinic data, indicate much lower estimates, especially in adolescent patients [37]. One study from a rural setting in KwaZulu-Natal indicates that suppression rates have increased significantly from 2005, to 2007, most probably due to improved service provision and patient tracking procedures [38].
Factors other than the counselling are likely to have contributed to the good outcomes observed in the current study. It is possible that the repeated adherence assessments functioned as an adherence intervention in both arms by reminding participants of the importance of adherence. The tracking and tracing in place at the clinic required for trial follow-up reduced the likelihood of missed study visits and losses to follow-up. Tracking is key as it is a reminder for visits, ensures good refill rates, and also communicates to each participant that they are important. In this setting where access to treatment is difficult, the threat of losing access to treatment may have exerted a powerful motivational influence, as would direct experiences of morbidity and mortality in the community.
The clinic also provides a selection of other supportive activities, not formally considered to be part of the standard of care at the start of the study, but would have improved outcomes beyond what would be expected with didactic counselling alone. These include pillboxes to aid remembering to take pills, pill packet illustrations for illiterate participants and dosing instructions provided in the local language. Ad hoc counselling was provided to any participants who had clinical problems or adherence measures that concerned staff, as previously indicated. These sessions were significantly more likely to occur in the didactic counselling arm participants, which is not surprising as the motivational counselling participants were more likely to be scheduled for an individualised counselling session within which they would have dealt with any issues relating to poor adherence. Although it is possible that the ad hoc counselling meant that the control arm might be biased towards the null, this ad hoc counselling was part of the standard of care against which the intervention counselling would need to be an improvement, and so this was not unexpected, or avoidable. In addition to this, these sessions were only conducted in a relatively small number of cases and participants, and the content remained didactic rather than motivational.
All of these factors are implementable in other settings, and would be amenable to study as adherence interventions in their own right. It is also possible that once the Hawthorne effect of being intensively followed up in this study wore off [39], that differences between the adherence strategies between the two arms might, over time, lead to greater sustained adherence and viral suppression in one of the arms, but this was not feasible to assess within the time frames of the current study.
Finally, the majority of participants were co-enrolled on a TB/HIV treatment study or were previous TB treatment patients. They remained a selected group of participants who had experience of, and likely success with, TB treatment adherence. It was considered probable during the conceptualisation of this trial that the burden of concurrent or sequential TB treatment and ART would negatively impact on treatment adherence. That the participants in this study have done so well is very promising in relation to the increased calls to integrate HIV and TB treatment, and the very large proportion of HIV patients this specific population represents in South Africa. These results support closer integration of HIV and TB treatment.
Major strengths of our study include the randomised controlled trial design, use of a theory-based intervention, the use of viral load as the primary outcome, and the trial setting of a TB clinic, which is a common entry point for HIV treatment in Africa. While adherence intervention studies report adherence and treatment outcomes for relatively short periods of time, often only for up to immediately after the completion of the intervention being tested [7, 40], this study assessed treatment outcomes up to 12 months post-initiation of treatment.
A limitation of this trial was that the high viral suppression rate following standard didactic counselling was not anticipated, the sample size calculation assumed only 65 % suppression in the didactic arm, and the study was not powered for small incremental benefits of motivational counselling since substantial benefits would be needed from this intensive and more costly approach to warrant its implementation. A further limitation is that the setting of this trial in a TB clinic may reduce its generalizability.
Although this study showed that it is feasible to roll out this more intensive individualised motivational counselling in a resource-constrained setting, the counselling was designed to target issues with specific skills deficits at the individual level that may not have been appropriate for this setting. This intensive individualised motivational counselling approach is more likely to be necessary and effective where barriers to adherence are personal and motivational rather than structural, and in populations who experience many of these barriers. Identification of a population at high risk for non-adherence, or of participants who are experiencing difficulties, may be a more appropriate target for testing this intervention. This is likely to be even more important now that treatment provision has expanded so much outside of clinical research settings.
In summary, we conclude that the standard of care didactic counselling was adequate in the setting of our TB clinic, and that intensive personalised one-on-one motivational counselling did not significantly improve adherence and treatment outcomes in this study. The finding that motivational counselling had no benefit over traditional didactic counselling in this setting is an important contribution to the literature on HIV treatment adherence counselling, as it does warn against implementing intensive individualised motivational counselling in settings where less resource intensive didactic counselling may be adequate. These study results empower health educators, nurses or community health workers to provide efficacious adherence support in a limited and structured counselling intervention.
Notes
We refer to patients in the treatment programme, and to participants when enrolled onto this study.
References
UNAIDS. AIDS epidemic update : november 2009. Geneva: WHO; 2009.
Nachega JB, Hislop M, Dowdy DW, Lo M, Omer SB, Regensberg L, et al. Adherence to highly active antiretroviral therapy assessed by pharmacy claims predicts survival in HIV-infected South African adults. J Acquir Immune Defic Syndr. 2006;43(1):78–84.
Broder S. The development of antiretroviral therapy and its impact on the HIV-1/AIDS pandemic. Antivir Res. 2010;85(1):1–18.
Jones R, Gazzard B. The cost of antiretroviral drugs and influence on prescribing policies. Int J STD AIDS. 2006;17(8):499–506.
Orrell C. Antiretroviral adherence in a resource-poor setting. Curr HIV/AIDS Rep. 2005;2(4):171–6.
Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21–30.
Simoni JM, Pearson CR, Pantalone DW, Marks G, Crepaz N. Efficacy of interventions in improving highly active antiretroviral therapy adherence and HIV-1 RNA viral load. A meta-analytic review of randomized controlled trials. J Acquir Immune Defic Syndr. 2006;43(1):S23–35.
Abdool Karim SS, Abdool Karim Q, Friedland G, Lalloo U, El-Sadr WM. Implementing antiretroviral therapy in resource-constrained settings: opportunities and challenges in integrating HIV and tuberculosis care. AIDS. 2004;18(7):975–9.
Shisana O, Simbayi L, editors. Nelson Mandela/HSRC Study of HIV/AIDS. South African national HIV prevalence, behavioural risks and mass media. Household survey 2002. Cape Town: Human Sciences Research Council; 2002.
Ammassari A, Trotta MP, Murri R, Castelli F, Narciso P, Noto P, et al. Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. J Acquir Immune Defic Syndr. 2002;31(3):S123–7.
Simoni JM, Frick PA, Pantalone DW, Turner BJ. Antiretroviral adherence interventions: a review of current literature and ongoing studies. Top HIV Med. 2003;11(6):185–98.
Amico KR, Harman JJ, Johnson BT. Efficacy of antiretroviral therapy adherence interventions: a research synthesis of trials, 1996 to 2004. J Acquir Immune Defic Syndr. 2006;41(3):285–97.
Gordon CM. Commentary on meta-analysis of randomized controlled trials for HIV treatment adherence interventions: research directions and implications for practice. J Acquir Immune Defic Syndr. 2006;43(1):S36–40.
Mannheimer SB, Morse E, Matts JP, Andrews L, Child C, Schmetter B, et al. Sustained benefit from a long-term antiretroviral adherence intervention: results of a large randomized clinical trial. J Acquir Immune Defic Syndr. 2006;43(1):S41–7.
Cote JK, Godin G. Efficacy of interventions in improving adherence to antiretroviral therapy. Int J STD AIDS. 2005;16(5):335–43.
Simoni JM, Amico KR, Pearson CR, Malow R. Strategies for promoting adherence to antiretroviral therapy: a review of the literature. Curr Infect Dis Rep. 2008;10(6):515–21.
DiIorio C, McCarty F, Resnicow K, McDonnell Holstad M, Soet J, Yeager K, et al. Using motivational interviewing to promote adherence to antiretroviral medications: a randomized controlled study. AIDS Care. 2008;20(3):273–83.
Davies G, Koenig LJ, Stratford D, Palmore M, Bush T, Golde M, et al. Overview and implementation of an intervention to prevent adherence failure among HIV-infected adults initiating antiretroviral therapy: lessons learned from Project HEART. AIDS Care. 2006;18(8):895–903.
Koenig LJ, Pals SL, Bush T, Pratt Palmore M, Stratford D, Ellerbrock TV. Randomized controlled trial of an intervention to prevent adherence failure among HIV-infected patients initiating antiretroviral therapy. Health Psychol. 2008;27(2):159–69.
Abdool Karim SS, Naidoo K, Grobler A, Padayatchi N, Baxter C, Gray A, et al. Timing of initiation of antiretroviral drugs during tuberculosis therapy. N Engl J Med. 2010;362(8):697–706.
Abdool Karim SS, Naidoo K, Grobler A, Padayatchi N, Baxter C, Gray AL, et al. Integration of antiretroviral therapy with tuberculosis treatment. N Engl J med. 2011;365(16):1492–501.
Department of Health. National antiretroviral treatment guideliness. Pretoria: National Department of Health; 2004.
WHO. Scaling up antiretroviral therapy in resource-limited settings: treatment guidelines for a public health approach (2003 revision). Geneva: World Health Organization; 2004.
DHHS. Guidelines for the use of antiretroviral agents in hiv-1-infected adults and adolescents. Washington: DHHS; 2004.
Fisher J, Fisher W, Bryan A, Misovich S. Information-motivation-behavioural skills model-based HIV risk behaviour change interventions for inner city high school youth. Health Psychol. 2002;21(2):177–86.
Fisher JD, Fisher WA. The information-motivation-behavioural skills model. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging theories in health promotion practice and research. San Francisco: Jossey-Bass; 2002. p. 40–70.
Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychol. 2006;25(4):462–73.
Fisher JD, Fisher WA, Cornman DH, Amico RK, Bryan A, Friedland GH. Clinician-delivered intervention during routine clinical care reduces unprotected sexual behavior among HIV-infected patients. J Acquir Immune Defic Syndr. 2006;41(1):44–52.
Rollnick S, Butler CC, McCambridge J, Kinnersley P, Elwyn G, Resnicow K. Consultations about changing behaviour. BMJ. 2005;331(7522):961–3.
Emmons KM, Rollnick S. Motivational interviewing in health care settings. Opportunities and limitations. Am J Prev Med. 2001;20(1):68–74.
Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305–12.
Lawn SD, Harries AD, Anglaret X, Myer L, Wood R. Early mortality among adults accessing antiretroviral treatment programmes in sub-Saharan Africa. AIDS. 2008;22(15):1897–908.
Lawn SD, Little F, Bekker LG, Kaplan R, Campbel E, Orrell C, et al. Changing mortality risk associated with CD4 cell response to antiretroviral therapy in South Africa. AIDS. 2009;23(3):335–42.
Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280(19):1690–1.
Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6.
Barth RE, van der Meer JT, Hoepelman AI, Schrooders PA, van de Vijver DA, Geelen SP, et al. Effectiveness of highly active antiretroviral therapy administered by general practitioners in rural South Africa. Eur J Clin Microbiol Infect Dis. 2008;27(10):977–84.
Nachega JB, Hislop M, Nguyen H, Dowdy DW, Chaisson RE, Regensberg L, et al. Antiretroviral therapy adherence, virologic and immunologic outcomes in adolescents compared with adults in southern Africa. J Acquir Immune Defic Syndr. 2009;51(1):65–71.
Mutevedzi PC, Lessells RJ, Heller T, Barnighausen T, Cooke GS, Newell ML. Scale-up of a decentralized HIV treatment programme in rural KwaZulu-Natal, South Africa: does rapid expansion affect patient outcomes? Bull World Health Organ. 2010;88(8):593–600.
McCarney R, Warner J, Iliffe S, van Haselen R, Griffin M, Fisher P. The Hawthorne Effect: a randomised, controlled trial. BMC Med Res Methodol. 2007;7:30.
Simoni JM, Amico KR, Smith L, Nelson K. Antiretroviral adherence interventions: translating research findings to the real world clinic. Curr HIV/AIDS Rep. 2010;7(1):44–51.
Acknowledgements
This research was supported by the Doris Duke Charitable Foundation-funded Operations Research on AIDS Care and Treatment in Africa (ORACTA) Programme (Grant # 2005058). The Association of Commonwealth Universities funded PhD study for Francois van Loggerenberg at London School of Hygiene and Tropical Medicine. He was also supported by the Columbia University-Southern African Fogarty AIDS International Training and Research Programme (AITRP) funded by the Fogarty International Center, National Institutes of Health (Grant #D43TW00231). The National Institute of Allergy and infectious Disease (NIAID), National Institutes of Health (NIH) (Grant# AI51794) funded the infrastructure for this research. Alison Grant was supported by a Public Health Career Scientist award from the UK Department of Health. We would like to thank the clinic research support staff who provided the data collection, nursing services, as well as the administrative and counselling support for CAPRISA 058 study, Senzo Hlathi, Goodness Gumede, and Thandi Shezi. Dr Leila Mansoor provided advice and assisted with the training of the clinic counselling staff. Lise Werner, Anneke Grobler and Nonhlanhla Yende provided additional statistical guidance and support. Jayraj Ramota was the data manager, and data were entered and validated by Mfanafuthi Mthambela. Clive Govender provided data quality control. Members of the Center for Health, Intervention, and Prevention (CHIP), University of Connecticut, who developed the IMB model, were very helpful in the conceptualisation, conduct and analysis of this trial. Specifically, Paul Shuper and K. Rivet Amico provided on-going support and guidance. Katherine Fielding and Simon Lewin provided support as members of the PhD advisory committee. The intervention was based on one developed by Gerald Friedland (Yale University, USA), Marita Murrman, Patricia Torro, and Wafaa El-Sadr (all Columbia University, USA) in earlier work, and was generously shared; their support and guidance during the conceptualisation of this study conducted is acknowledged. We would like to especially acknowledge the participants who took part in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Loggerenberg, F., Grant, A.D., Naidoo, K. et al. Individualised Motivational Counselling to Enhance Adherence to Antiretroviral Therapy is not Superior to Didactic Counselling in South African Patients: Findings of the CAPRISA 058 Randomised Controlled Trial. AIDS Behav 19, 145–156 (2015). https://doi.org/10.1007/s10461-014-0763-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-014-0763-6