Abstract
The purpose of this study was to examine neurological impairment in combination with information–motivation–behavioral skills (IMB) variables. The study tests the role of IMB variables as mediators of antecedent variables of demographics, life stress, social support, and neurological impairment with outcome measures of HIV preventive and risk behaviors in a sample of HIV-positive, alcohol-using adults (n = 250) with a history of alcohol abuse/dependence. Neurological impairment was measured with the Color Trails Test (CTT). Average performance on the CTT by the sample was substantially worse than established norms. In a directional latent variable model, neurological impairment directly predicted lower transmission knowledge scores and poorer performance on an observational condom skills assessment. Greater neurological impairment was significantly associated with greater age. Future interventions geared toward HIV+ adults who use alcohol should take into consideration HIV-related and age-related neurological functioning which may impede the facilitation of safe sex behaviors.
Resumen
El propósito de este estudio fue de investigar la interrelación del deterioro neurológico con las variables de (IMB) las cuales son Información, Motivación y Habilidad de Conducta. El estudio investigo como las variables de IMB actúan como mediadores y anteceden las variables demográficas, estrés, apoyo social, y deterioro neurológico las cuales miden el resultado de la conducta preventiva del VIH y conducta de riesgo en una grupo de personas adultas que consumen alcohol y son VIH-positivo, (no = 250) con un historial de abuso o dependencia de alcohol. El deterioro neurológico se midió con la medida llamada Examen de Rastro de Colores (CTT). El rendimiento de promedio medio de esta prueba (CTT) en este grupo de personas fue sustancialmente más bajo que las normas normales de otros grupos. En un modelo direccional latente de variables, la afección neurológica predijo directamente más baja transmisión de conocimiento y un peor rendimiento en la evaluación de observación de habilidades de cómo usar el condón. Mayor deterioro neurológico fue asociado significativamente con mayor edad. Por lo cual, proponemos que las intervenciones en el futuro que sean orientadas a adultos VIH + que consumen alcohol deben de tomar en consideración la relación con el VIH al igual que la relación con la edad y su interrelación con el funcionamiento neurológico lo cual puede impedir la facilitación de conductas de sexo seguro.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
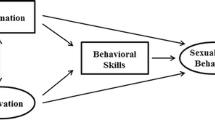
Several models of health behavior change have been developed to better understand the bio-psychosocial factors that influence HIV transmission. One theoretical framework that has effectively predicted HIV risk and preventive behavior in diverse samples and conditions is the information–motivation–behavioral skills (IMB) model [1]. According to the IMB model, there are three fundamental determinants of HIV risk reduction: knowledge of HIV/AIDS transmission and information concerning specific methods for the prevention of the transmission; motivation to change HIV/AIDS risk behavior; and behavioral skills for performing the specific preventive behaviors. This model proposes that HIV prevention information and motivation efforts, through preventive behavioral skills, will influence health behaviors such as condom use during sexual intercourse [2]. However, a biological indicator, such as neurological functioning, might be an effective component to add to a test of the IMB model in order to enhance the explanatory power of the model.
The IMB model has shown particular strength in predicting condom skills, knowledge, intention and self-efficacy [3]. It is common in studies using IMB model skills to use measures of self-efficacy for performing behavior and to use single or multiple indicators to define motivation. For example, Kalichman et al. [4] combined pro-condom social norms, condom attitudes, and perceived risk for HIV as independent markers of motivation within the IMB framework. In another study, the motivational component was determined by measuring attitudes toward condom use, perceived social norms supportive of condom use, and behavioral intentions to use condoms [5].
The IMB model has been tested in a broad range of populations including college students, [2] heroin injectors (6), severely mentally ill adults [4], and adolescents [7]. However, it is suggested that the constructs of the model are most generalizable when applied to a well-defined population [7]. This study will examine neurological functioning, life stress, and social support, along with IMB model constructs—knowledge about HIV and STD transmission, prosocial peer attitudes about condom use, and condom self-efficacy in alcohol-using, HIV-positive adults, a high risk population for spreading HIV.
It is important to study the effects of neurological impairment on risk behaviors. With HIV-positive individuals living longer due to increased availability and accessibility of HIV treatments in the U.S., new neurologic syndromes often associated with one’s HIV status are emerging with greater frequency over the life span [8–11]. HIV-associated neuropathology affects the loss of specific neuron subpopulations involved in cognition and motor function such as impaired hippocampal-dependent memory and delirium [11].
HIV associated neurocognitive disorders (HAND) are divided into minor cognitive motor disorder (MCMD) and HIV-associated dementia (HAD) [10]. MCMD is further subdivided to include asymptomatic neurocognitive impairment (ANI) and mild neurocognitive disorder (MND). MND is accompanied by mild interference in daily functioning, whereas ANI-associated cognitive impairment does not interfere with activities of daily living [12, 13]. ANI and MND are both identified by performance scores at least 1 standard deviation (SD) below the mean of normative scores in at least two cognitive domains: attention-information, processing, language, abstraction-executive, complex perceptual motor skills, memory, including learning and recall, simple motor skills or sensory perceptual abilities [10, 14]. On the other hand, HAD is characterized by marked neurocognitive impairment with 2 SD or greater below the means of normative scores in at least two cognitive domains and cognitive impairment produces marked interference with activities of daily living [10, 14].
The types of impairments exhibited by persons with these neurologic syndromes can affect functioning at work or in everyday activities of daily living [12]. Even though HAND has become less frequent, HIV-positive individuals are still at risk for these neurological complications. It is estimated that around 2–5 % of HIV-positive individuals may develop HIV-associated dementia and up to 37 % suffer a less severe ANI or MND [15]. Several of the neurocognitive deficits seen in patients with HAND are believed to contribute to HIV risk behavior, affecting impulse control [16] and episodic memory functions that may impair the ability to plan and execute intentions [17]. Alcohol use is also associated with neurological impairment. Studies examining 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) data have reported that more than 50 % of HIV-infected clinic patients reported heavy alcohol use [18, 19]. Among individuals with HIV infection and drug and alcohol use disorders, impaired verbal working memory [20], impaired auditory working memory, and enhanced cognitive impulsivity have been observed [21]. Additionally, synergistic negative effects of HIV and heavy alcohol use together have been observed in motor and visual spatial tasks [22].
Social contextual variables such as social support and life stress are also associated with risk and protective health behaviors. According to a 2010 CDC white paper on social determinants of HIV/AIDS in the U.S. [23], environmental conditions such as housing and social support; social and physical environments; and availability, cost of, and access to health services are affected by distribution of power and resources and contribute as pathways or barriers to HIV infection and overall health. High levels of perceived stress among HIV-infected people have been associated with having lower income [24]. Financial difficulty has been one of the most frequently reported stressful events among people with HIV [25]. Other stressful life events are exceedingly common in the lives of people living with HIV and are negatively associated with antiretroviral medication adherence and treatment outcomes. McMahon et al. [26] found that higher levels of stress predicted less frequent condom use during a 6-month drug abuse treatment follow-up. Additionally, studies examining the relationship between social support and risk behaviors have been mixed: some have demonstrated that lower levels of support are associated with increased sexual risk behavior [27–31] where others have found no relationship between social support and risk [32].
The current study employs structural equation modeling to more clearly delineate the complex relationships among and between constructs from Fisher and Fisher’s IMB model [1, 2], along with measures of life stress, social support, and neurological impairment, in predicting outcomes associated with HIV risk: alcohol use, condom skills, and high risk sexual activity. The hypothesized structural equation model positions background demographics, neurological impairment, and psychosocial variables representing life stress and social support as predictors of the IMB components of transmission knowledge, prosocial peer attitudes about condom use, and condom self-efficacy. In turn, the Information and Motivational mediators are used as predictors of Behavioral outcomes including objective condom skills, risky sexual behaviors, and quantity and frequency of alcohol use. A further specific hypothesis posits a negative influence of neurological impairment on both Information (transmission knowledge) and behavioral skills.
Methods
Participants
The baseline sample was culturally diverse, predominantly minority, low income, and sexually active (N = 250; 35 % female; 71 % Black/African American, 16 % Hispanic, 7 % White, 2 % American Indian/Native/Hawaiian/Pacific Islander, 2 % mixed, 2 % unreported). Seven percent had less than an 8th grade education, 35 % had some high school, 34 % had a high school diploma or GED, and 24 % percent had attended college or had a college degree. Nine percent were currently employed. The recruitment sites primarily serve a heterosexual population (68.9 %; n = 173); however, some of our enrolled participants reported sexual orientation as homosexual (17.9 %; n = 45) and bisexual (10.8 %; n = 27) or none or unsure (1.6 %; n = 4); refused to answer (0.8 %; n = 2).
Recruitment
The recruitment sites were primarily located in densely populated, multicultural, low income, urban areas of Miami with high rates of alcohol and other drug abuse, HIV, violence and poverty, with the vast majority of the population uninsured and suffering from multiple health disparities. Thirteen Community-Based Organizations (CBOs) that were in contact with the target population agreed to act as recruitment sites. These CBO programs are among the largest in the local area providing outpatient alcohol and drug abuse treatment programs and mental health services to HIV-positive alcohol and drug abusing men and women. The agencies providing outpatient mental health, alcohol and drug abuse treatment share several attributes: first, programs are not-for-profit, accredited by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), and licensed by the State of Florida Department of Health and Rehabilitative Services; second, each program is designed to promote progression from preliminary screening and biopsychosocial assessment to individually tailored addiction treatment; and third, the goal of each program is strongly focused on helping patients achieve and maintain abstinence from alcohol, drugs, and sexual behaviors through case management and therapeutic activities.
In addition to advantages in size and the diversity of populations served by the recruitment sites, all of the CBO programs possess further desirable characteristics: (a) a history of working cooperatively with our research team in prior studies; (b) a demonstrated commitment by program leadership and staff to research as a primary method of improving treatment knowledge and ultimately improving treatment outcomes; and (c) active involvement in assisting our research staff in refining treatment protocols to assure validity while maintaining treatment integrity. The CBOs vary on several key dimensions important to the study: seropositivity rates vary among their clients; the programs embrace different philosophical approaches to HIV/AIDS services, ranging from faith-based to medical models; and, although the majority of the clients served by these agencies are from minority groups, the clients vary in the proportions that are African American, Caribbean Islander and Hispanic. The vast majority of clients are from families who are in the lowest socioeconomic class and receive Medicaid benefits, with the exception of those who are ineligible due to immigration status.
Participants meeting inclusion/exclusion criteria were recruited from these sites. The inclusion criteria were being older than 18 years and less than 60 years; being HIV-positive and willing to present documentation to confirm their serostatus; having consumed any alcohol in the last 3 months; having a history of alcohol abuse or dependence within the past 2 years; and having at least one episode of unprotected vaginal or anal sex in the past 90 days. Further criteria included facility in English, understanding the informed consent, ability to provide contact information to be located for more interviews, willingness to be randomized to treatment or a control group and to be contacted for follow-up assessments, planning to be in the area for the next 12 months, not facing immediate incarceration or residence in a restricted environment, and currently not showing symptoms of a major psychiatric disorder including psychosis, or suicidality. Based on these entry criteria, our recruiter and research team screened and identified 2,634 potential participants, 261 of whom met study criteria. Data analyses were completed on 250 participants of which ten participants did not have recorded data due to computer or assessor error, and one study participant did not meet criteria based on the information that was gathered.
Trained staff members recruited and screened clients. The recruiter contacted the facilities that had agreed to support the study and made presentations about the study to facility clients. All potentially eligible study participants at the recruitment sites were informed of the study by research staff, posters, flyers, site staff, and by word of mouth. Those clients who were interested in participating in the study were offered a pre-screening interview. Staff explained the inclusion criteria to the potential participants, screened them for eligibility, and conducted informed consent. Human subjects’ approval was obtained from Florida International University’s Institutional Review Board (IRB; approval number: 102607-01).
Recruitment staff met with participants in private to explain the study procedures including intervention and assessment protocols, follow-up periods, confidentiality, and incentive structure. Attention was given to ensuring that clients understood that participation was strictly voluntary and that participation in any other outside treatment activities was not contingent on study participation. The client was specifically informed about the informed consent documentation. The nature of the confidentiality that surrounds research studies was also discussed with the participant, explaining that confidentiality is assured to the extent allowed by law. After the study was explained, clients were asked to repeat back the critical elements of informed consent, including what it means to consent voluntarily, procedures for withdrawal, confidentiality, and assessment procedures.
Assessment
The assessments were conducted in a variety of ways depending on the nature of what was being assessed and covered a wide range of information. Assessment methods included: (1) CAPI (computer assisted personal interview); (2) ACASI (audio computer assisted self-interview for subjective sensitive topics); (3) paper and pen as specified for neurological measures; and (4) TLFB (time-line follow-back); e.g., alcohol/drug use and # of sex partners.
Variables in the Model
Indicators of the latent variables representing the psychosocial and IMB constructs of the model are described below. Some items are single-item demographics and sum scores.
Demographics and Background Characteristics (CAPI) Demographics included Hispanic ethnicity (“Do you consider yourself to be Hispanic or Latino(a)?” 1 = yes/2 = no); gender (1 = male, 2 = female); and age in years.
Neurological Impairment was assessed with the Color Trails Tests 1 and 2 (CTT-1 and CTT-2) [33] using paper and pen. CTT-1 requires the participant to connect encircled numbers one through 25, randomly arranged on a page, in proper order. Odd numbered circles have a pink background and even-numbered circles have a yellow background. CTT-2 shows all numbers twice. The participant must connect the numbers from 1 to 25 alternating between pink and yellow circles and must disregard the numbers in circles of the alternate color. Times are recorded in seconds; the two scores were used as indicators of a latent variable representing neurological impairment. The CTT is sensitive to a variety of neurological impairments and processes [34] and, because the test requires no language skills (entirely numeric), it is considered culturally fair [35]. Mean scores for CTT-1 among normative samples of men and women are 28.5 (SD 10.2) and 28.7 (SD 10.7) respectively. Mean scores for CTT-2 among normative samples of men and women are 70.6 (SD 35.5) and 70.3 (SD 29.2) respectively [36].
Life Stress was measured with six items modified from the Life Event Survey (LES) [37] to assess perception of life events in the past 3 months that may have bothered or caused distress (coefficient alpha = 0.77) using ACASI. Sample items included “your illness bothered you in the past 3 months”, “your alcohol use bothered you in the past 3 months”. Items were rated on a 1–5 scale ranging from “not at all” to “extremely”; thus, higher scores indicate more stress. To avoid too many indicators for the size of the sample, items were combined randomly into three parcels. This is a commonly utilized procedure and is acceptable when coefficient alpha is high among the items [38].
Social Support was assessed with the 19-item Medical Outcomes Study (MOS) Social Support Survey [39] using ACASI. A higher score indicates more support; item response categories range from 1 to 5 and choices include: none of the time, a little of the time, some of the time, most of the time, and all of the time. Coefficient alpha for the 19 items was 0.96. Principal component analysis indicated there were three factors. The means of these three subfactors were used and labeled “instrumental support,” “illness-specific support,” and “love and affection.” Higher scores indicate more support.
Intermediate IMB Construct: Knowledge about HIV and STD transmission was assessed using ACASI with the Sexually Transmitted Disease Knowledge Questionnaire (STD-KQ) [40], a 28 item (one item added for this study) questionnaire which measures awareness of HIV/STD transmission routes, safe and risky behaviors, myths about HIV and other STDs, and behavior-specific prevention information. During validation, the STD-KQ demonstrated internal consistency (alpha = 0.86) and test–retest reliability (r = 0.88) over a brief period [40]. A single score was used as an indicator of knowledge about transmission.
Intermediate IMB Construct: Prosocial Peer Attitudes about condom use were assessed with six items from the Sexual Risks Scale—Norms [41] (coefficient alpha = 0.82) using ACASI. This was considered to be part of the motivational aspect of the model. For example, “My friends and I encourage each other before dates to practice ‘safer’ sex.” Items were rated on a 1–5 scale ranging from “strongly disagree” to “strongly agree.” Items were randomly combined into three parcels as described above due to the large coefficient alpha and concerns about sample size.
Intermediate IMB Construct: Condom Self-Efficacy was assessed with ACASI using the Condom Use Self Efficacy Scale Revised. [42, 43] This scale consists of 28 items such as “I feel confident in my ability to discuss condom usage with any partner I might have,” and “I feel confident in my ability to suggest using condoms with a new partner.” Items were rated on a 1–5 scale ranging from “strongly disagree” to “strongly agree.” Coefficient alpha for the scale was 0.87. The items were combined into three parcels, again due to concerns about sample size.
Outcome Measures
Condom Skills were quantified using a “direct” skill performance measure, Condom Use Skills [44, 45] in which an assessor rates a participant’s observed use of male condoms on a wooden penile model. Scores reflect the total number of correct steps as well as possible errors. One overall score was given ranging from 0 to 7. The assessors/evaluators are trained in a group setting using guidance, modeling, and role-play. They receive instant feedback in order to assure and demonstrate accurate assessment skills. Then, they are observed in vivo by a supervisor until the assessor demonstrates consistent and accurate scoring.
Risky Sex Behavior was assessed with four items: three items were from an adapted version of the Risk Behavior Assessment (RBA) [46], using ACASI, and one item assessed the number of sex partners in the past 3 months using the TLFB measure [47–49]. The TLFB and the RBA is a structured interview designed specifically for a substance abusing population that assesses a number of sexual risk behaviors. The RBA’s three risk items asked, “In the last 3 months how many times have you (1) traded sex for shelter or food?; (2) traded sex for drugs?; and (3) traded sex for money?”
Recent Alcohol Use was assessed by a TLFB measure [47–49] using pen and paper. The TLFB procedure uses a calendar format to enhance accurate recall and to provide a continuous history for alcohol intensity variables: (1) total number of days used alcohol in the past 3 months; (2) total number of standard drinks consumed in the past 3 months.
Analysis
The analytic method used in this current paper is structural equation modeling (SEM) using latent variables. The initial confirmatory and hypothesized predictive analyses were performed using the EQS structural equations program, version 6.1 [50]. Latent variable analysis allows one to evaluate a hypothesized model with correlated non-experimental data. Goodness-of-fit of the models was assessed with the maximum likelihood χ2, the Comparative Fit Index (CFI), and the root mean squared error of approximation (RMSEA) [50, 51]. The CFI ranges from 0 to 1 and reflects the improvement in fit of a hypothesized model over a model of complete independence among the measured variables. CFI values at 0.95 or greater are desirable, indicating that the hypothesized model reproduces 95 % or more of the covariation in the data. The RMSEA is a measure of lack of fit per degrees of freedom, controlling for sample size. Values less than 0.06 indicate a relatively good fit between the hypothesized model and the observed data.
An initial confirmatory factor analysis (CFA) assessed the adequacy of the hypothesized measurement model and the associations among the latent variables and the single item variables in the model which included the demographics, the knowledge score, and the condom skills score. Correlations between error residuals were considered for addition to the model for fit improvement and were based on results of the LaGrange multiplier test (LM Test) [52] which suggests significant paths or covariances that can improve the fit of the model. Then a directional latent variable model positioned background variables of neurological impairment, gender, age, ethnicity, life stress and social support as predictors of the intermediate IMB constructs of knowledge, prosocial peer attitudes, and condom self-efficacy. In turn, the IMB constructs predicted condom skills, risky sex behavior, and recent alcohol use. As mentioned previously, we hypothesized a priori that neurological impairment would directly impact condom skills and included that pathway in the initial path model. Additional paths from the background items were also allowed if suggested by the LM test.
Results
Neurological Impairment
As reported in Table 1, mean scores on the CTT-1 and CTT-2 were substantially greater than the established norms for those tests. As reported above, normative scores for men and women are 28.5 (SD 10.2) and 28.7 (SD 10.7) respectively for the CTT-1 [36]. In this current sample which has an age range similar to that of Bornstein [36], the average score was 57.76 (SD 31.54). Normative scores for CTT-2 among men and women are 70.6 (SD 35.5) and 70.3 (SD 29.2) respectively [36]. This sample had an average score of 118.65 (SD 54.80). Gender was not associated with the scores (see Table 2).
Confirmatory Factor Analysis
Table 1 reports summary statistics of the measured variables and the factor loadings of the hypothesized factor structure for the latent variables. All factor loadings were significant (p < 0.001). Fit indexes for the final CFA model were excellent: M-L χ2 = 272.13, 213 df; CFI = 0.97; RMSEA = 0.033, Confidence Interval (CI) for RMSEA = 0.020 to 0.045. Only one correlated error residual was added. This was an association between “sex for money” and “sex for drugs” on the risky sex behavior latent variable which appears logical and is a reasonable addition to the model. Fit statistics were also acceptable without the additional correlated error residual.
Table 2 reports the bivariate correlations among the variables in the model before the directional hypothesized structural equation model was tested. Focusing on the most significant findings, neurological impairment was more likely among older participants (0.21, p < 0.001), and was associated with a lower knowledge score (−0.28, p < 0.001) and poorer condom skills (–0.30, p < 0.001). Females reported more social support (0.18, p < 0.01). Older participants were less like to be Hispanic (−0.17, p < 0.01), and reported both worse condom skills (−0.18, p < 0.01) and fewer risky sex behaviors (−0.18, p < 0.01). Greater life stress was associated with less social support (−0.17, p < 0.05), better condom skills (0.24, p < 0.001) and more risky sex behaviors (0.21, p < 0.001). Social support and a higher knowledge score was associated with better condom skills (0.18, p < 0.01 and 0.20, p < 0.001 respectively).
Structural Equation Analysis
The final model after dropping nonsignificant regression paths is presented in Fig. 1. Rectangles represent single-item measured variables and circles represent multiply-indicated latent variables. Regression paths were trimmed gradually following the procedure in which the most minimal nonsignificant paths and correlations are dropped sequentially until none remain in the model [53]. Fit indexes were very good: M-L χ2 = 289.21, 261 df; CFI = 0.99; RMSEA = 0.021, CI = 0.000–0.034. As hypothesized, greater neurological impairment negatively predicted both the knowledge score and condom skills. A better knowledge score and greater condom self-efficacy predicted better condom skills. IMB constructs did not directly predict any of the risky sex behaviors, but prosocial peer attitudes were associated with less recent alcohol use. Based on suggestions from the LM Test, a few additional regression paths from the baseline items were added to the outcome variables including a negative association between age and risky sex behavior (−0.16), and an association between life stress and risky sex behavior (0.26). Social support directly predicted better condom skills (0.17). These supplementary paths were not necessary for a good fit but were added to expand the information in the study. There was a significant negative correlation between better condom skills and recent alcohol use (−0.14).
Discussion
Outcomes from the present study are informative in guiding the development and enhancement of risk reduction interventions in HIV-positive populations. Findings based upon IMB model associations and the direct impact of neurological impairment on both knowledge and safe sex behaviors such as proper condom use may contribute most in directing future research.
While it is of utmost importance to build research upon sound psychosocial theory such as the IMB model, the use of structural equation modeling in testing relationships between numerous factors including a biological predictor yielded a great deal of useful and novel information. Because IMB has been applied to HIV more than any other health issue, our findings are of importance in understanding the additional and synergistic effects that neurological impairment has upon HIV knowledge, risk, and protection. In addition to finding that neurological impairment was associated with older age, our study revealed a strong negative association between impairment and HIV transmission knowledge and condom skills. Although most research has shown that highly active antiretroviral therapy has resulted in prolonged life and even reduced the incidence of HAD, recent studies are indicating that long term toxicity may still contribute to impaired neurological function [54–57]. An in vitro study was recently able to elaborate a possible mechanism of toxicity with the net effect of elevating amyloid beta (Aβ) plaques in the brain [58]. However, the authors note a number of factors remain unsettled on the pathological contributions of HIV infection, ART, aging, and co-morbid conditions, including the way newer medications, so-called neuroHAART with more central nervous system penetration, may behave [58, 59]. Based on the findings in the present study, it is recommended that future interventions seeking to elucidate issues of treatment response be designed with participants’ levels of HIV- and/or age-related neurological functioning in mind.
In addition to the association between HIV transmission knowledge and condom skills with HIV-related neurological impairment, it has been shown that HIV or its treatments could also impair the cognitive functions associated with impulsivity and decision-making, personality characteristics associated with higher levels of HIV-related risk-taking [60]. A pattern of deficits in mental operations such as response inhibition and working memory has been demonstrated in several studies [20, 61]. Additionally, Martin et al. [21] found that HIV-positive subjects performed significantly worse on the Iowa gambling tasks test (a measure of impulsivity) suggesting that risk-taking could possibly be attributed to neurologic deficits. Whether or not the same prefrontal operations are affected by alcohol use that are affected by HIV or its treatments, a greater level of impulsive decision making has been observed in alcohol abusing populations [62]. Although impulsivity was not examined in this study, it is recommended that future research explore the effects of both alcohol and HIV-related neuropathology on the myriad brain operations associated with knowledge, skills and impulsivity related to risk-taking and risk-reducing behaviors.
As shown in Fig. 1, we identified several significant predictive paths between psychosocial variables and risk and protective outcomes in this study. A predictive relationship was found between prosocial peer attitudes about condom use and alcohol use. It is possible that these phenomena are concurrent and that the same social group that drinks less frequently consists of health-minded people who also express pro-condom norms. Whereas many studies have confirmed the close association of alcohol use with risky sexual behavior [63], little information is available on the actual health-related attitudes of people who use alcohol heavily. Further, it should be noted that when questioning participants on peer attitudes, we are collecting information on their perceptions of their peers. A study by Carey et al. [64] found that their sample inaccurately believed others were more approving of risk behavior and less approving of condom use as compared with their peers’ actual attitudes. The same study reported that participants’ perceptions of norms in fact predicted their reported risk behavior suggesting that the mere perception of norms might be powerful in steering risk-taking or protective behavior. In the current study, if a participant were embedded in a network of peers who use alcohol in excess and were to believe this same group to hold anti-condom attitudes, that participant may also be engaging in higher risk behaviors. It would be valuable to conduct further research in order to better understand the strength of alcohol use versus perceived social norms in predicting risk behaviors.
Also within the realm of social contextual variables, we found a relationship between positive social support and better condom skills. Social support can increase one’s sense of well-being and stability in life situations. Integration into a health-minded social network may also reduce exposure to experiences and environments linked to risky sexual practices. Not surprisingly, several studies have shown that higher levels of social support predicted using condoms more frequently [65, 66]. Alternatively, life stress was identified as an important predictor of sexual risk behavior. Stressful events can strain coping resources and the accumulation of multiple stressors may overwhelm the problem-solving capacity of the individual, leading to diminished self-care [67].
It is important to acknowledge a few possible study limitations. There may be a lack of generalizability to other HIV-positive individuals and findings from this study may be most applicable to the people who volunteered to participate. This investigation relied upon participant self-reports for some of the variables which can be biased intentionally or unintentionally due to inaccurate recall and the sensitive nature of the personality, problem behavior, and sex risk questions posed in the study assessments. Such questions are prone to triggering issues of shame and stigma, known to cause participants to conceal or amend responses erring on the side of social desirability [68]. Although self-report can yield biased data from participants, we employed several strategies to minimize recall bias and to encourage honest reporting, including Time-line Follow-back and recall of no more than 90 days for participants. Up to 3 months recall of alcohol and other drug use has proven to provide reliable data [69]. Also, data from the Color Trails Test are objective measures of neurological impairment.
In addition, this study examined certain constructs that may be difficult to define. For example, the true construct validity of motivation within the IMB model remains in question [5]. Kalichman [7] also found that measures of condom self-efficacy were equivalent to objective measures of condom skills. In this study, we measured both condom self-efficacy and skills as separate factors rather than one as-proxy-for another. However, the correlation between them was not so great as to indicate a tautological association between them so they appear to be measuring separate constructs. Thus, the application of IMB in predicting condom use skills and HIV risk behaviors remains a theoretical framework of good fit in many populations and settings. Our finding that HIV risk knowledge and self-efficacy both significantly predicted condom skills supports previous assertions. However, unlike the present study, prior research has revealed positive correlations between IMB constructs and risk behaviors using a different set of construct definitions and measurements [70].
Outcomes from this study can contribute to the growing body of knowledge concerning HIV-related neurocognitive impairment and, more specifically, to IMB-driven interventions aimed at reducing HIV risk. Impairment of information processing and memory seen in HIV-infected individuals may prevent acquisition and retention of behavioral content often delivered in risk-reduction programs. Additionally, cognitive impairment has been found to affect motivation, an important behavioral predictor of intervention effectiveness [71, 72]. Research suggests that cognitive rehabilitation strategies should be incorporated into treatment, particularly to improve of executive function [73]. Using IMB risk reduction interventions that incorporate role playing and detailed risk information have shown sustained reduction in unprotected sex [74]. Studies suggest that interventions incorporating cognitive remediation strategies, diverse presentation of information, and a strong focus on practical applications (e.g., motivation and role-play) are the most successful at reducing risk among cognitively impaired populations [75].
References
Fisher J, Fisher W. Changing AIDS-risk behavior. Psychol Bull. 1992;111:455–74.
Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychol. 1994;13:238–50.
Malow RM, Stein JA, McMahon RC, Dévieux JG, Rosenberg R, Jean-Gilles M. Effects of a culturally adapted HIV prevention intervention in Haitian youth. J Assoc Nurses AIDS Care. 2009;20(2):110–21.
Kalichman S, Malow R, Devieux J, Stein JA, Piedman F. HIV risk reduction for substance using seriously mentally ill adults: test of the information-motivation-behavior skills (IMB) model. Commun Ment Health J. 2005;41(3):277–89.
Kalichman SC, Picciano JF, Roffman RA. Motivation to reduce HIV risk behaviors in the context of the information, motivation and behavioral skills (IMB) model of HIV prevention. J Health Psychol. 2008;13(5):680–9.
Bryan A, Fisher J, Fisher W, Murray D. Understanding condom use among heroin addicts in methadone maintenance using the information–motivation–behavioral skills model. Subs Abuse Misuse. 2000;35(1):451–47.
Kalichman S, Stein J, Malow R, Averhart C, Dévieux J, Jennings T, et al. Predicting protected sexual behaviour using the information–motivation–behaviour skills model among adolescent substance abusers in court-ordered treatment. Psychol Health Med. 2002;7(3):327–39.
Norman LR, Basso M, Kumar A, Malow R. Neuropsychological consequences of HIV and substance abuse: a literature review and implications for treatment and future research. Curr Drug Abuse Rev. 2009;2(2):143–56.
Durvasula R, Norman L, Malow R. Current perspectives on the neuropsychology of HIV. In: Pope C, White R, Malow R, editors. HIV/AIDS: global frontiers in prevention/intervention. New York: Routledge; 2009. p. 177–90.
Antinori A, Arendt G, Becker J, Brew B, Byrd D, Cherner M, et al. Updated research nosology for HIV associated neurocognitive disorders. Neurology. 2007;69:1789–99.
del Palacio M, Álvarez S, Muñoz-Fernández MÁ. HIV-1 infection and neurocognitive impairment in the current era. Rev Med Virol. 2011;85(21):11468–78.
Gandhi NS, Skolasky RL, Peters KB, Moxley RT 4th, Creighton J, Roosa HV, Selnes OA, McArthur J, Sacktor N. A comparison of performance-based measures of function in HIV-associated neurocognitive disorders. J Neurovirol. 2011;17:159–65.
Foley JM, Wright MJ, Gooding AL, Ettenhofer M, Kim M, Choi M, Castellon SA, Sadek J, Heaton RK, van Gorp WG, Marcotte TD, Hinkin CH. Operationalization of the updated diagnostic alogarithm for classifying HIV-related cognitive impairment and dementia. Int Psychogeriatr. 2011;23(5):835–43.
Gisslén M, Price RW, Nilsson S. The definition of HIV-associated neurocognitive disorders: are we overestimating the real prevalence? BMC Infect Dis. 2011;11:356.
Sacktor N. The epidemiology of human immunodeficiency virus-associated neurological disease in the era of highly active antiretroviral therapy. J Neurovirol. 2002;8(2):115–21.
Lopez OL, Smith G, Meltzer CC, Becker JT. Dopamine systems in human immunodeficiency virus-associated dementia. Neuropsychiatry Neuropsychol Behav Neurol. 1999;12(3):184–92.
Woods S, Moore D, Weber E, Grant I. Cognitive neuropsychology of HIV-associated neurocognitive disorders. Neuropsychol Rev. 2009;19(2):152–68.
Samet JH, Phillips SJ, Horton NJ, Traphagen ET, Freedberg KA. Detecting alcohol problems in HIV-infected patients: use of the CAGE questionnaire. AIDS Res Hum Retrovir. 2004;20(2):151–5.
Conigliaro J, Justice AC, Gordon AJ, Bryant K, VACS Alcohol and Behavior Change Research Group. Role of alcohol in determining human immunodeficiency virus (HIV)-relevant outcomes: a conceptual model to guide the implementation of evidence-based interventions into practice. Med Care. 2006;44(8 Supl. 2):S1–S6.
Farinpour R, Martin EM, Seidenberg M, Pitrak DL, Pursell KJ, Mullane KM, Novak RM, Harrow M. Verbal working memory in HIV-seropositive drug users. J Int Neuropsychol Soc. 2000;6:548–55.
Martin EM, Pitrak DL, Weddington W, Rains NA, Nunnally G, Nixon H, Grbesic S, Vassileva J, Bechara A. Cognitive impulsivity and HIV serostatus in substance dependent males. J Int Neuropsychol Soc. 2004;10(7):931–8.
Rothlind JC, Greenfield TM, Bruce AV, Meyerhoff DJ, Flenniken DL, Lindgren JA, Weiner MW. Heavy alcohol consumption in individuals with HIV infection: effects on neuropsychological performance. J Int Neuropsychol Soc. 2005;11(1):70–83.
Centers for Disease Control and Prevention. Establishing a holistic framework to reduce inequities in HIV, viral hepatitis, STDS, and tuberculosis in the United States. Atlanta: Department of Health and Human Services; 2010.
Koopman C, Gore-Felton C, Marouf F, Butler LD, Field N, Gill M, Chen XH, Israelski D, Spiegel D. Relationships of perceived stress to coping, attachment and social support among HIV-positive persons. AIDS Care. 2000;12(5):663–72.
Reif S, Mugavero M, Raper J, Thielman N, Leserman J, Whetten K, Pence BW. Highly stressed: stressful and traumatic experiences among individuals with HIV/AIDS in the Deep South. AIDS Care. 2011;23(2):152–62.
McMahon RC, Penedo FJ, Loewinger L, Jennings TE. Stress, social support and HIV risk among drug dependent men. Am Psychol. 1998;53(8):882–939.
Pence BW, Raper JL, Reif S, Thielman NM, Leserman J, Mugavero MJ. Incident stressful and traumatic life events and human immunodeficiency virus sexual transmission risk behaviors in a longitudinal, multisite cohort study. Psychosom Med. 2010;72(7):720–6.
Miller GE, Cole SW. Social relationships and the progression of human immunodeficiency virus infection: a review of evidence and possible underlying mechanisms. Ann Behav Med. 1998;20(3):181–9.
Adib SM, Joseph JG, Ostrow DG, James SA. Predictors of relapse in sexual practices among homosexual men. AIDS Educ Prev. 1991;3:293–304.
Kimberly JA, Serovich JM. The role of family and friend social support in reducing risk behaviors among HIV-positive gay men. AIDS Educ Prev. 1999;11(6):465–75.
St. Lawrence JS, Brasfield TL, Jefferson KW, Allyene E, Shirley A. Social support as a factor in African–American adolescents’ sexual risk behavior. J Adolesc Res. 1994;9(3):292–10.
McMahon RC, Malow RM, Jennings TE. Personality, stress, and social support in HIV risk prediction. AIDS Behav. 2000;4(4):399–410.
D’Elia L, Satz P, Uchiyama C, White T. Color Trails Test. Odessa: Psychological Assessment Resources; 1996.
Tombaugh T. Trail making test A and B: normative data stratified by age and education. Archiv Clin Neuropsychol. 2004;19:203–14.
Maj M, Satz P, Janssen R, Zaudig M, Starace F, D’Elia L, Sughondhabirom B, Mussa M, Naber D, Ndetei D, et al. WHO neuropsychiatric AIDS study, cross-sectional phase II. Neuropsychological and neurological findings. Arch Gen Psychiatry. 1994;51(1):51–61.
Bornstein R. Normative data on selected neuropsychological measures from a nonclinical sample. J Clin Psychol. 1985;41(5):651–9.
Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the life experiences survey. J Consult Clin Psychol. 1978;46:932–46.
Yuan KH, Bentler PM, Kano Y. On averaging variables in a confirmatory factor analysis model. Behaviormetrika. 1997;24:71–83.
Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–14.
Jaworski BC, Carey MP. Development and psychometric evaluation of a self-administered questionnaire to measure knowledge of sexually transmitted diseases. AIDS Behav. 2007;11:557–74.
DeHart DD, Birkimer JC. Trying to practice safer sex: development of the sexual risks scale. J Sex Res. 1997;34:11–25.
Brien TM, Thombs DL, Mahoney CA, Wallnau L. Dimensions of self-efficacy among three distinct groups of condom users. J Am Coll Health. 1994;42:167–74.
Brafford LJ, Beck KH. Development and validation of a condom self-efficacy scale for college students. J Am Coll Health. 1991;39:219–25.
Malow R, Dévieux JG, Rosenberg R, Capp L, Schneiderman N. A cognitive-behavioral intervention for HIV+ recovering drug abusers: the 2000–2005 NIDA-funded AIDS prevention center study. Psychol AIDS Exch. 2001;30:23–6.
Sorensen JL, London J, Morales E. Group counseling to prevent AIDS. In: Sorensen J, Wermuth L, Gibson D, Choi K, Guydish J, Batki S, editors. Preventing AIDS in drug users and their sexual partners. New York: Guilford; 1991. p. 99–115.
National Institute on Drug Abuse (NIDA). NIDA risk behavior assessment. Rockville: NIDA; 1991.
Carey MP, Carey KB, Maisto SA, Gordon CM, Weinhardt LS. Assessing sexual risk behaviour with the timeline followback (TLFB) approach: continued development and psychometric evaluation with psychiatric outpatients. Int J STD AIDS. 2001;12:365–75.
Weinhardt LS, Carey MP, Maisto SA, Carey KB, Cohen MM, Wickramasinghe SM. Reliability of the timeline followback sexual behavior interview. Ann Behav Med. 1998;20:25–30.
Weinhardt LS, Otto-Salaj LL, Brondino MJ, Norberg MM, Kalichman S. Sex-related alcohol expectancies predict sexual risk behavior among severely and persistently mentally ill adults. Psychol Addict Behav. 2002;16:64–7.
Bentler PM. EQS structural equations program manual. Encino: Multivariate Software; 2006.
Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6:1–55.
Chou CP, Bentler PM. Model modification in covariance structure modeling: a comparison among likelihood ratio, Lagrange Multiplier, and Wald tests. Multivar Behav Res. 1990;25:115–36.
MacCallum RC. Specification searches in covariance structure modeling. Psychol Bull. 1986;100:107–20.
Mothobi NZ, Brew BJ. Neurocognitive dysfunction in the highly active antiretroviral therapy era. Curr Opin Infect Dis. 2011;24(5):503–8.
Joska JA, Gouse H, Paul RH, Stein DJ, Flisher AJ. Does highly active antiretroviral therapy improve neurocognitive function? A systematic review. J Neurovirol. 2010;16(2):101–14.
Robinson-Papp J, Elliott KJ, Simpson DM. HIV-related neurocognitive impairment in the HAART era. Curr HIV/AIDS Rep. 2009;6(3):146–52.
Heaton RK, Franklin DR, Ellis RJ, et al. HIV-associated neurocognitive disorders before and during the era of combination antiretroviral therapy: differences in rates, nature, and predictors. J Neurovirol. 2011;17(1):3–16.
Giunta B, Ehrhart J, Obregon DF, Lam L, Le L, Jin JJ, et al. Antiretroviral medications disrupt microglial phagocytosis of β-amyloid and increase its production by neurons: implications for HIV-associated neurocognitive disorders. Mol Brain. 2011;4:23.
Cysique LA, Waters EK, Brew BJ. Central nervous system antiretroviral efficacy in HIV infection: a qualitative and quantitative review and implications for future research. BMC Neurol. 2011;11:148.
Dévieux J, Malow R, Stein JA, Jennings TE, Lucenko BA, Averhart C, et al. Impulsivity and HIV risk among adjudicated alcohol and other drug-abusing adolescent offenders. AIDS Educ Prevent. 2002;14(Supplement B):24–3.
Martin EM, Sullivan TS, Reed RA, Fletcher TA, Pitrak DL, Weddington W, Harrow M. Auditory working memory in HIV-1 infection. J Int Neuropsychol Soc. 2001;7(1):20–6.
Courtney KE, Arellano R, Barkley-Levenson E, Gálvan A, Poldrack RA, Mackillop J, David Jentsch J, Ray LA. The relationship between measures of impulsivity and alcohol misuse: an integrative structural equation modeling approach. Alcohol Clin Experim Res. 2011. doi:10.1111/j.1530-0277.2011.01635.x.
MacDonald TK, Zanna MP, Fong GT. Why common sense goes out the window: Effects of alcohol on intentions to use condoms. Personal Soc Psychol Bull. 1996;22:763–75.
Carey K, Scott-Sheldon L, Carey M, Cain D, Mlobeli R, Vermaak R, et al. Community norms for HIV risk behaviors among men in a South African township. J Behav Med. 2011;34(1):32–40.
Catania JA, Coates TJ, Stall R. Changes in condom use among homosexual men in San Francisco. Health Psychol. 1991;10:190–9.
Sobo EJ. Finance, romance, social support, and condoms: use among impoverished inner-city women. Hum Organ. 1995;54:115–28.
Cohen S, Wills TA. Stress, social support and the buffering hypothesis. Psychol Bull. 1985;98:310–57.
Malow RM, Gustman S, Ziskind D, McMahon R, Lawence J. Evaluating HIV prevention interventions among drug abusers: validity issues. J HIV/AIDS Prevent Educ Adolesc Child. 1998;2:21–40.
Schroder K, Carey MP, Vanable P. Methodological challenges in research on sexual risk behavior: I accuracy of self-reports. Ann Behav Med. 2003;26:104–23.
Huy NV, Dunne MP, Debattista J, Hien NT, An DTM. Association of human immunodeficiency virus (HIV) preventive information, motivation, self-efficacy and depression with sexual risk behaviors among male freelance laborers. J AIDS HIV Res. 2011;3(1):20–9.
Blume A, Davis J, Schmaling K. Neurocognitive dysfunction in dually-diagnosed patients: a potential roadblock to motivating behavior change. J Psychoact Drugs. 1999;31(2):111–5.
Morgenstern J, Bates ME. Effects of executive function impairment on change processes and substance use outcomes in 12-step treatment. J Stud Alcohol. 1999;60(6):846–55.
Blume AW, Marlatt GA. The role of executive cognitive functions in changing substance use: what we know and what we need to know. Ann Behav Med. 2009;37(2):117–25.
Calsyn D, Hatch-Maillette M, Tross S, Doyle S, Crits-Christoph P, Song Y, et al. Motivational and skills training HIV/sexually transmitted infection sexual risk reduction groups for men. J Subst Abuse Treat. 2009;37(2):138–50.
Anand P, Springer S, Copenhaver M, Altice F. Neurocognitive impairment and HIV risk factors: a reciprocal relationship. AIDS Behav. 2010;14(6):1213–26.
Acknowledgments
This research was supported by Grant R01AA017405 from National Institute on Alcohol Abuse and Alcoholism (NIAAA) and Grant DA 01070-38 from the National Institute on Drug Abuse.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Malow, R.M., Dévieux, J.G., Stein, J.A. et al. Neurological Function, Information–Motivation–Behavioral Skills Factors, and Risk Behaviors Among HIV-Positive Alcohol Users. AIDS Behav 16, 2297–2308 (2012). https://doi.org/10.1007/s10461-012-0246-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-012-0246-6