Abstract
Behavioral interventions to prevent HIV or assist HIV-positive persons often incorporate peers, yet empirical support for their efficacy is only recently accumulating. We describe the results of a review of the global literature, identifying 117 studies evaluating the efficacy of peer-based interventions in the area of HIV/AIDS. About half were conducted in the developing world and half in Western nations. Across a range of populations and intervention modalities, the majority of studies provided some support for peer interventions according to outcome indicators in the domains of sexual risk behavior, attitudes and cognitions, HIV knowledge, and substance use. However, outcomes assessed using biomarkers and other non-self-report variables were less likely to indicate intervention efficacy. Overall, findings suggest that we can have some confidence in peer interventions, yet more data are needed demonstrating an effect in the most rigorous study designs and with outcomes that are not potentially affected by respondent bias.
Resumen
Las intervenciones que pretenden cambiar el comportamiento para prevenir el VIH o para aydar a las personas infectadas por el VIH frecuentemente incluyen a los trabajadores no profesionales como promotores de salud, o “pares”. Sin embargo, los datos sobre la eficacia de las intervenciones que utilizan pares apenas están acumulando recientemente. Esta revisión sistemática describe los resultados de una revista de la literatura global, la cual identificó 117 estudios que evalúan la eficacia de las intervenciones basadas en pares relacionadas con el VIH. Aproximadamente la mitad de los estudios fueran llevados a cabo en los países en desarrollo y la mitad en los países desarrollados. Representando diversas poblaciones y tipos de intervenciones, la mayor parte de los estudios demuestra apoyo para el uso de pares, según resultados relacionados con comportamiento sexual riesgoso, las actitudes y la cognición, los conocimientos relacionados con el VIH, y el uso de sustancias. Sin embargo, los resultados medidos por datos biológicos y otros datos objetivos mostraron menos tendencia a indicar una intervención eficaz. En general, los resultados parcialmente apoyan el uso de las intervenciones basadas en pares pero todavía se precisan mas datos demostrando efectos en estudios de diseño riguroso y con resultados que no son limitados por un sesgo potencial de respuesta.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An estimated 33.4 million people are living with HIV infection throughout the world [1]. In the United States (US) alone, there are thought to be about 1.1 million people living with HIV/AIDS (PLWHA) [2]. Despite efforts to prevent new infections, transmission of HIV continues, with an estimated 2.7 million new infections worldwide in 2008 [1].
Appropriate use of antiretroviral therapy can radically improve the prognosis of PLWHA and has been shown to be cost effective in both low- and high-income countries [3]. Moreover, early comprehensive use of ART in high-prevalence populations has been suggested as a possible strategy to reduce transmission of HIV [4]. The magnitude of the epidemic and the complexity of chronic HIV care, however, represent major challenges to healthcare delivery systems in both resource-rich and resource-limited settings.
Indeed, the World Health Organization and UNAIDS have identified human resource limitations as a major barrier to scaling up HIV service delivery [5–7]. Efforts to build human resource capacity in HIV services include the shifting of healthcare tasks typically performed by highly trained medical specialists to workers who are in more abundant supply or who can be more quickly and inexpensively recruited, trained, and deployed [8, 9]. Community-based, non-professional care providers have become an important component of task-shifting strategies: in several high HIV-prevalence countries, community health workers are being integrated into HIV health care services [10]. In addition to health care tasks, community members also can provide to PLWHA valuable ancillary services, such as individual and group education and social support [11].
PLWHA are uniquely qualified to perform some of these tasks, especially supportive services, since they can complement task-oriented training with direct experience of disease management in the specific context of their communities’ strengths and challenges. Indeed, since the onset of the HIV epidemic, PLWHA or those who are otherwise directly affected by HIV/AIDS (e.g. parents or caregivers of PLWHA) have contributed to HIV prevention, care, and treatment in a wide range of paid and unpaid peer provider roles [12].
As we described elsewhere, peers may be distinguished from other community health workers by several qualities [13]. First, peers share with their patients or clients key personal characteristics, circumstances, or experiences (i.e., “peerness”). Thus peers may be selected because they are from certain communities (e.g., African-American men who have sex with men [MSM]) or belong to targeted subgroups (e.g., former injection drug users). Second, their shared characteristics, circumstances, and experiences influence the particular ways in which peers provide services and are received by patients or clients, so that their status as peers is thought to add value to the health services they provide. Third, like other community health workers, peers generally complete short-term, competency-based training rather than a discipline-based or clinical curriculum [10]. Finally, peer roles are highly specified as part of formal HIV prevention and treatment efforts. Although peers may share social networks with their clients and their work may overlap with their social activities, peer services are intentionally provided according to standard protocols for health-related interventions, rather than being the natural result of engagement in social networks [13].
Peer interventions for HIV prevention and care have been promoted by international funding agencies and policy makers [14, 15]. Support for the use of peers in a wide variety of HIV care settings is likely based in part on their perceived availability, accessibility, and low cost in comparison to professional healthcare providers. Common characteristics, circumstances, and experiences are thought to facilitate their acceptability to target populations and increase their influence and legitimacy [16].
In contrast to the popularity and widespread implementation of peer interventions in HIV, researchers have only recently begun to more rigorously evaluate the efficacy of peer support. In general, the heterogeneity of outcomes and assessment methods used to measure them limit the ability to compare results across studies and the dearth of rigorous study designs restricts the ability to make conclusions about their efficacy. Recent systematic and qualitative reviews of peer interventions also have found a relatively weak evidence base and methodological diversity in reporting of results that limit the ability to draw strong conclusions from published studies [17–19].
One exception to the lack of systematic analysis of peer-related HIV interventions is a recent meta-analysis and systematic review that located 30 studies of peer education for HIV prevention in developing countries published between January 1990 and November 2006. Meta-analysis indicated that peer education interventions were significantly associated with increased HIV knowledge, reduced equipment sharing among injection drug users, and increased condom use, but not sexually transmitted infections (STIs). The authors concluded that peer education programs in developing countries had moderate effects on behavioral outcomes but no demonstrated significant impact on biological outcomes [16].
Given the considerable resources committed to developing and disseminating peer-based programs, evidence of their effect is warranted. Policy makers and public health officials could clearly benefit from research on the effect of peers, including an updated investigation to determine whether there are differential outcomes for US-based interventions versus those in the developing world and specific areas in which peers are more likely to show an effect.
The present paper describes the results of a systematic review of the global literature on peer interventions to promote health in the area of HIV/AIDS. The heterogeneity in the outcomes precluded a meta-analysis [20]. Our primary aims were to describe the state of the research literature evaluating peer interventions and to summarize in a systematic fashion the evidence for the efficacy of peer work in HIV across multiple HIV-related health domains.
Methods
Literature Review
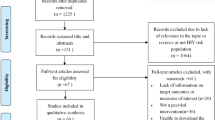
A search of published literature was conducted using PubMed and PsychInfo. Only articles published before November 1, 2010 were considered. Searches were limited to English-language reports, using combinations of the terms: HIV, peer, intervention(s). We also consulted with colleagues and scanned the reference lists of relevant publications. Articles were restricted to those that: (1) involved peers as the only or one of the main modes of intervention, with peers defined as those who were (a) from similar socio-demographic or other relevant backgrounds as participants in the study, (b) non-professionally trained, and (c) introduced to operate according to specified protocols; (2) addressed an HIV-related health concern as one of the main aims; (3) conducted a statistical evaluation of the effect of the peer intervention on at least one HIV-related outcome; and (4) were original reports of the results.
A multi-stage process was adopted to select relevant papers. The first and second authors first examined the titles and abstracts for their applicability according to the inclusion criteria. All papers that appeared eligible were distributed among the authors and two research associates who independently examined each according to the selection criteria. All studies were subject to further examination during the coding process as well. All discrepancies regarding eligibility were discussed until a consensus was reached among the authors.
Study Coding
Selected papers were classified independently by the authors into one of the following predetermined categories: randomized controlled trials (RCT), quasi-experimental designs (non-randomized comparison), and cross-sectional or other less rigorous designs (no comparison group). Authors extracted data in the following categories: study location (US, other developed country, developing country); population (MSM, school-based youth, non-school based youth, sex workers, substance users, PLWHA, other at-risk women, other); intervention type (formal meeting/structured groups, formal one-on-one interactions, peer opinion leader, outreach, other); and extent of follow-up. We also extracted type of outcome reported (sexual risk behavior; substance use; HIV knowledge, attitudes and cognitions; biomarkers; other non-self-reported outcome); number of results per outcome domain; and the number of supportive results (defined as statistically significant results, P < 0.05, that supported the intervention’s efficacy for a specified outcome). Any disagreements were discussed by all authors until a consensus was reached.
Analysis
Study characteristics were tabulated by summing the number of studies per category and then stratifying by study design. Efficacy of peer interventions was assessed by summing the number of studies with a supportive result for at least one of the variables in the specified domain. Note this is a liberal estimate of efficacy: if a study assessed six substance use variables and only one demonstrated a supportive effect for the peer intervention, the study would be considered as indicating support. We then divided the number of supportive interventions by the total number of studies to create an overall percentage of studies with supportive results. These were stratified by study design, with Pearson’s χ2 tests and Fisher’s exact tests, as appropriate, used to compare the percentage of studies with supportive results across study designs and individual study characteristics (i.e. year of publication, study location, intervention modality, and population studied).
Results
Description of Studies
Overall, 518 manuscripts were identified in the preliminary search; 330 were excluded during the abstract review process; and an additional 71 were excluded during the data extraction process. An on-line appendix listing the final 117 studies selected, their ratings, and full citations is provided; a summary of the studies is presented in Table 1.
As seen in the table, the number of publications in this area is growing steadily, from only 10 in the first 4-year period (1990–1994) to 65 in 2005–2010. However, only a minority of studies (n = 28) employed a rigorous randomized controlled design; most were quasi-experimental (n = 54) or used some other cross-sectional approach (n = 35). The US is vastly overrepresented among study locations (n = 51), but new studies have led to a greater representation of work in the developing world (n = 54). The modalities varied considerably, though in over half of the studies (n = 68) peers operated through formal meetings or structured groups. Outreach activities were also common (n = 40), with formal one-on-one (n = 24) and popular opinion leader [21] (n = 15) strategies used less frequently. Finally, the peer interventions targeted a wide range of populations, most commonly school-based youth (n = 28), substance users (n = 18), sex workers (n = 18), and MSM (n = 17).
In terms of intervention outcomes, most studies examined multiple domains; note that 92 of the 117 studies (79%) assessed variables that fell into more then one of the 6 domains. Seventy-eight studies assessed sexual risk behaviors, including unprotected anal intercourse and condom use. Seventy-three studies analyzed various attitudes and cognitions around HIV acquisition and transmission, including perceived risk for HIV, perceived importance of not getting HIV, belief that a healthy person cannot be infected, and intentions to practice only safe sex. HIV knowledge, variously operationalized, was assessed as an outcome in 52 studies. Substance use, including reported behaviors such as needle sharing, cleaning needles, and methamphetamine use, was assessed in 27 studies. Least frequently included as outcomes were biological makers such as HIV tests, CD4 counts, tests for STIs, and viral load (n = 16 studies) and outcomes measured by means other than self-report (e.g., electronically monitored HIV medication adherence, condom sales; n = 9 studies).
Additionally, studies varied greatly in the number of variables they assessed, with an average of 7 different variables assessed per study (range = 1–48). Per domain, studies assessed attitudes and cognitions (Mean (M) = 5.1 outcomes, range = 1–34); sexual risk behaviors (M = 3.4, range = 1–24); substance use (M = 3.3, range = 1–14); biological outcomes (M = 2.8, range = 1–11); HIV knowledge (M = 2.1, range = 1–20); and other non-self-reported outcomes (M = 2.1, range = 1–8).
Efficacy of Peer Interventions
The percentage of outcomes that supported the efficacy of peer-based interventions is reported for each outcome domain by study design in Table 2. As seen in column 1, descriptive findings indicate that, overall, peer interventions were efficacious, although the likelihood of a supportive result varied according to outcome domain. Attitudes and cognitions, HIV knowledge, and sexual risk behaviors were the domains most widely assessed and were most likely to indicate the efficacy of the peer interventions, with 89.0% of the 73 studies assessing attitudes and cognitions, 84.6% of the 52 studies assessing HIV knowledge, and 76.9% of the 78 studies assessing sexual risk behaviors indicating at least one supportive result in the domain. Variables in the substance use domain, used as outcome indicators in 27 studies, also generally pointed to the efficacy of the peer interventions being tested, with at least one supportive result in 70.4% of studies using them. Biological makers (n = 16 studies) and other outcomes that did not rely on self-report (n = 9 studies) were seldom used and much less likely to offer evidence that the peer intervention was successful (at least one supportive result was reported in 37.5% of studies examining biological markers and 55.6% of studies of other non-self report outcomes).
Moderators of Intervention Efficacy
Finally, we examined whether the rigor of the study design or any individual study characteristic moderated findings of intervention efficacy. χ2 analyses indicated that the likelihood of a supportive result—in 5 of the 6 domains—did not differ according to the rigor of the study design (see columns 2–5 in Table 2). For instance, for sexual risk behavior, 64.7% of the RCTs that evaluated variables in this domain demonstrated a supportive result for at least one of them, as did 78.1% of the quasi-experimental designs and 85.0% of the other, less rigorous designs. These percentages were not significantly different, χ2(2) = 2.2, P = 0.14. The exception was biological outcomes, for which 12.5% of the RCTs, 40.0% of the quasi-experimental design, and all of the other, less rigorous design demonstrated support for the peer intervention under study, χ2(2) = 7.1, P = 0.03.
With respect to individual study characteristics that might moderate the likelihood of a supportive result, we examined year of publication, study location, intervention modality, and population studied. Study location, intervention modality, and population studied were shown to moderate the findings of some of the outcome domains. Specifically, of the 73 studies that assessed attitudes and cognitions, 6 (66.7%) of the 9 studies conducted in developed countries compared to 59 (92.2%) of the 64 studies conducted in the US or developing countries had supportive results in this domain, χ2(1) = 5.3, P = 0.02. For intervention modality, of the 27 studies that assessed substance use, 9 (100%) of the studies that used outreach compared to 10 (55.6%) of the 18 studies that did not use outreach methods had supportive results, Fisher’s exact test, P = 0.02. Finally, study population moderated the results in two different domains, sexual risk behavior and attitudes and cognitions. Of the 78 studies that assessed sexual risk behavior, only 1 (20.0%) of the 5 studies targeting PLWHA had supportive results, whereas 59 (80.8%) of the 73 studies that did not target PLWHA had supportive results, χ2(1) = 9.8, P < 0.01. For the 73 studies that assessed attitudes and cognitions, 5 (62.5%) of the 8 studies targeting MSM had supportive results, compared to 60 (92.3%) of the 65 studies that did not target MSM, χ2(1) = 6.5, P = 0.01.
Discussion
Peer interventions for HIV prevention or care are widespread and widely endorsed, yet only recently have researchers begun to examine them empirically. We reviewed the literature, casting a wide net in order to get a sense of the field overall. We identified 117 studies evaluating the efficacy of peer-based interventions in the area of HIV/AIDS. About half were conducted in the developing world and half in the US and other Western nations. Across a range of populations studied and intervention modalities employed, the majority of studies provided some support for the peer interventions they assessed according to outcome indicators in the domains of attitudes and cognitions, HIV knowledge, sexual risk behavior, and substance use. However, outcomes assessed in terms of biomarkers and other variables not self-reported—perhaps capable of offering a less subjective, more rigorous test of efficacy—were less likely to indicate intervention efficacy. Analyses of the potentially moderating impact of study rigor failed to indicate any significant findings except for the biological outcomes: positive findings were more likely in interventions tested in other, less rigorous designs than in RCTs or in quasi-experimental studies. Analyses of individual study characteristics as moderators of intervention effect revealed multiple potential moderators, including study location, intervention modality, and population studied. Studies conducted in developed countries (vs. not in developed countries) were less likely to have supportive results in the domain of attitudes and cognitions. Further, studies that used outreach methods compared to those that did not use outreach methods were more likely to have supportive results in the substance use domain. Finally, studies that targeted (vs. did not target) PLWHA were less likely to have supportive results in the domain of sexual risk behavior and studies that targeted MSM (vs. did not target) were less likely to have supportive results in the domain of attitudes and cognitions.
The current review is consistent with a prior meta-analytic review of peer interventions for HIV in the developing countries [16], which demonstrated effects on HIV knowledge, less equipment sharing among injection drug users, and condom use, but not STIs. Overall, the findings suggest we can have some confidence in peer interventions, but more data are needed demonstrating an effect in the most rigorous study designs and with outcomes that are not potentially affected by respondent bias. Nonetheless, we acknowledge there may be some situations in which the more subjective measures are the only options or are more appropriate; for instance, in studies which are under-powered for biological outcomes or in which rich, qualitative data on potential explanatory factors or contextual information would be useful.
There were some limitations to our study; most notably that we could not use meta-analytic techniques because of the heterogeneity of the 861 variables assessed across the 6 outcome domains in the 117 studies [20]. Also, publication bias might affect our conclusions: if studies indicating positive effects are more likely to be published, this would bias the body of research. Also, in our analyses we considered a study as providing support for peer interventions if any one of multiple indicators in a single domain were significant. This is a liberal definition of efficacy, more likely to show support than a stricter criterion requiring, for example, support across a majority or even all results evaluated in a given domain. At the risk of reporting false positives, we wanted to describe the upper limit of intervention efficacy.
Despite the limitations, our findings provide some support and encouragement to those pursing peer interventions in the area of HIV. The lack of findings for individual study moderators means, unfortunately, that we can offer few guidelines as to what types of interventions are most helpful. The moderator analyses did reveal that work with MSM may be most challenging in terms of attempting to show efficacy at least in the domain of attitudes and cognitions. Future work on peer interventions would benefit the field by using more rigorous evaluation methods. If possible, researchers should employ RCTs, providing full details about the research in accordance with Consolidated Standards of Reporting Trials (CONSORT) guidelines. If ethical considerations, resource constraints, or community dissent preclude RCTs, research might consider alternative approaches such as a wait-list control design, which would still provide rigorous support. Minimally, researchers should clearly describe primary and secondary outcomes a priori and report results for all outcomes, both a priori and post hoc. Also, they should provide greater specification of the measures and procedures. For example, the provision of details about how the peers were selected and trained and the scope and specifics of their duties could guide further research and those hoping to apply the interventions to real-world settings. Collecting and reporting process data on the feasibility and implementation of the intervention would further guide interpretation of the findings and assist in implementation efforts. For instance, if a large proportion of individuals approached declined to participate or, once enrolled, failed to complete the intervention, this might suggest the findings for such as study should not be as widely generalized.
Future research on the moderators of the effect of peer-led interventions also is needed. As one example, Cornish et al. systematically compared the context and the implementation of two sex-worker peer education interventions run, one in India and the other in South Africa. They found that the greater success of the Indian project was in part attributed to its (1) more stable and supportive social, material and political context and (2) community commitment to sex workers’ involvement, ownership and empowerment, as opposed to a more biomedical approach that marginalized sex workers’ concerns [22].
Future work on mediators also is needed to elucidate the processes by which peer interventions facilitate HIV-related outcomes. In earlier work, we provided a working definition of peer support and a 2-step framework for designing theory-based interventions [13]. Incorporating a clear theoretical conceptualization for an intervention before testing it allows for the examination of constructs that might explain its effect, such as self-efficacy, empowerment, improved knowledge, or skills acquisition.
Conclusions
In summary, this review and systematic analysis suggests that peer interventions to promote the health and well-being of persons living with or at risk for HIV/AIDS are widespread but that only more recently have researchers begun to systematically evaluate their efficacy. There are many reports of effective interventions, but many of these are undermined by methodology that limits the extent to which causality can be inferred. Future work, in carefully designed studies, could help demonstrate the actual effectiveness of peers and under what conditions and for which outcomes they can be maximally successful. The dire state of the HIV epidemic, coupled with decreasing global financial commitment, argue for the urgent need for such research.
References
World Health Organization. AIDS epidemic update: Nov 2009. Geneva: WHO; 2009.
Hall H, Song R, Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520–9.
Walensky R. Cost-effectiveness of HIV interventions: from cohort studies and clinical trials to policy. Top HIV Med. 2009;17(4):130–4.
Blower S, Gershengorn H, Grant R. A tale of two futures: HIV and antiretroviral therapy in San Francisco. Science. 2000;287(5453):650–4.
United Nations General Assembly. Towards universal access: assessment by the Joint United Nations Programme on HIV/AIDS on scaling up HIV prevention, treatment, care and support. New York: United Nations; 2006.
U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). Report on work force capacity and HIV/AIDS. Washington: Office of the US Global AIDS Coordinator, U.S. Department of State; 2006.
World Health Organization. Scaling up HIV/AIDS care: service delivery and human resources perspectives. Geneva: WHO; 2004.
World Health Organization. Task shifting: rational redistribution of tasks among health workforce teams: global recommendations and guidelines. Geneva: WHO; 2008.
World Health Organization. International conference on task shifting. Addis Ababa Declaration, 10 Jan 2008. Addis Ababa: WHO; 2008.
Celletti F, Wright A, Palen J, et al. Can the deployment of community health workers for the delivery of HIV services represent an effective and sustainable response to health workforce shortages? Results of a multicountry study. AIDS (Lond, Engl). 2010;24(Suppl 1):S45–57.
Wouters E. Mobilising the community in the fight against HIV/AIDS. Lancet. 2009;374(9700):1501.
Health Resources and Services Administration. Service delivery and HIV-positive peers. U.S. Department of Health and Human Services, Health Resources and Services Administration, HIV/AIDS Bureau; 2005. http://hab.hrsa.gov/publications/june5/. Accessed on 26 Jun 2009.
Simoni JM, Franks J, Lehavot K, Yard SS. Peer interventions to promote health: conceptual considerations. J Orthopsychiatry (in press).
UNAIDS. Peer education and HIV/AIDS: concepts, uses, and challenges. Geneva: UNAIDS; 1999.
U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). Prevention of sexual transmission for people engaged in high risk activity. Washington; 2009.
Medley A, Kennedy C, O’Reilly K, Sweat M. Effectiveness of peer education interventions for HIV prevention in developing countries: a systematic review and meta-analysis. AIDS Educ Prev. 2009;21(3):181–206.
Maticka-Tyndale E, Barnett JP. Peer-led interventions to reduce HIV risk of youth: a review. Evaluation and Program Planning. 2010;33(2):98–112.
Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: A Qualitative Systematic Review. Am J Prev Med. 2007;33(5):418–27.
Webel AR, Okonsky J, Trompeta J, Holzemer WL. A systematic review of the effectiveness of peer-based interventions on health-related behaviors in adults. Am J Public Health. 2010;100(2):247–53.
Deeks JJ, Higgins JP, Altman DG. Chapter 9: analysing data and undertaking meta-analyses. In: Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions: Cochrane Book Series. Chichester, UK: John Wiley & Sons, Ltd; 2008.
Kelly JA. Popular opinion leaders and HIV prevention peer education: resolving discrepant findings, and implications for the development of effective community programmes. AIDS Care. 2004;16(2):139–50.
Cornish F, Campbell C. The social conditions for successful peer education: a comparison of two HIV prevention programs run by sex workers in India and South Africa. Am J Community Psychol. 2009;44(1–2):123–35.
Acknowledgments
The authors would like to thank David Huh and Joyce Yang for their help with study selection and coding.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Simoni, J.M., Nelson, K.M., Franks, J.C. et al. Are Peer Interventions for HIV Efficacious? A Systematic Review. AIDS Behav 15, 1589–1595 (2011). https://doi.org/10.1007/s10461-011-9963-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-011-9963-5