Abstract
Although some rectal douches result in surface epithelium loss and potential increase of HIV transmission, men who have sex with men (MSM) continue to use them. We describe the prevalence of this practice among MSM engaging in unprotected receptive anal intercourse (URAI) in risky circumstances. A multiethnic sample with overrepresentation of HIV-negative MSM who had URAI in the previous year was recruited exclusively through the Internet. Participants were 105 MSM (78 HIV-negative, 27 HIV-positive). A total of 53% of HIV-negative and 96% of HIV-positive men douched in preparation for sex, most of them frequently or always, mainly for hygienic purposes. 27% of HIV-negative and 44% of HIV-positive douched after sex, partly believing douching protected from infections. Douching practices started around age 25. Regression analyses found the association between HIV status and douching occasions persisted after controlling for demographic characteristics and number of URAI occasions. Rectal douching in preparation for sex is common among men who practice URAI. This population could benefit from alternatives to condoms, such as rectal microbicides. Given the popularity of pre-coital douching and its frequency, a harmless rectal douche that could deliver a rectal microbicide could have great acceptability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the early days of the AIDS epidemic, scientists have found associations between the use of rectal enemas or douches and HIV as well as other sexually-transmitted infections (Bienzle et al. 1985; Deininger et al. 1990; Koziol et al. 1993; Moss et al. 1987; Ndimbie et al. 1996; Schreeder et al. 1982). Most of the studies were correlational, speculating that douching had deleterious effects on the rectum, but evidence was lacking until Schmelzer et al. (2004) published the results of their work. In a double-blind, repeated-measures study comparing three types of enema solutions (soapsuds, tap water, and polyethylene glycol-electrolyte solution—PEG-ES) in 24 healthy volunteers, rectal biopsies showed surface epithelium loss after soapsuds and tap water enemas, but not for PEG-ES enemas. Products that result in loss or damage to the epithelium may facilitate HIV transmission, one of the main reasons for which nonoxynol-9, a detergent that results in epithelial sloughing, was discarded as a possible rectal microbicide (Phillips et al. 2000). HIV-uninfected or infected men who have unprotected receptive anal intercourse (URAI) and douche in preparation for sex or following sex could unwittingly be increasing their chances of HIV transmission.
Topical microbicides, formulated as gels, foams, suppositories or films, are products currently under development for application inside the vagina or rectum before intercourse to prevent HIV transmission. Currently, it is believed that for a rectal microbicide to be efficacious, it should thoroughly cover the rectal and colon mucosa that may be susceptible to HIV exposure (Fuchs et al. 2007). Given that some douches disrupt the lining of the rectal mucosa, microbicides could see their potential effectiveness hampered if douching practices associated with intercourse are poorly understood. Insights on what rectal douching practices precede or follow anal intercourse may help inform strategies to maximize the adoption and effectiveness of microbicide use among men who have sex with men (MSM).
Studies of vaginal douching practices are illustrative at this point. Associations between vaginal douching and clamidial infection, pelvic inflammatory disease, and other STIs have been documented (Martino and Vermund 2002). Women report that they start douching typically during adolescence to feel “fresh” and “clean” and that the behavior is part of a number of other vaginal cleansing practices done during the time of menses or before sexual intercourse (Ness et al. 2003). The practice is more popular among African American women in the US than among Latinas or European Americans and appears to be more frequent among those with multiple sex partners (Koblin et al. 2002). Those who have studied vaginal douching from a behavioral perspective consider that people who engage in the practice are unlikely to change (Ness et al. 2003). The lack of willingness to change behavior, however, may rest on the absence of a product that could achieve similar desired effects to douching without its negative health consequences.
In this study, we interviewed men who use the Internet to meet other men for intentional condomless anal intercourse (“bareback”) (Carballo-Diéguez and Bauermeister 2004; Suarez and Miller 2001). This study had three objectives. First, to report the prevalence of douching behaviors in a sample of men at high risk for HIV transmission. Second, to analyze whether rectal douching behavior (e.g., age of onset, douching frequency, and number of pre-coital douching occasions) varied significantly by demographic characteristics (as had been reported for vaginal douching) and HIV status. Finally, to test whether pre-coital douching was associated with positive HIV status after controlling for unprotected receptive anal intercourse (URAI) occasions.
Method
Sample
As part of a larger study that explored reasons for “bareback” sex, we first identified the six most popular free Internet sites used by men in New York City to meet other men interested in this sexual practice (Carballo-Diéguez et al. 2006). Next, between April 2005 and March 2006, we recruited men who fulfilled the following eligibility criteria: (1) be at least 18 years old; (2) live in New York City or within commuting distance; (3) report using the Internet to meet men at least twice per month; (4) self-identify as a barebacker or as someone who practices barebacking; (5) have had intentional, condomless anal intercourse with a man met over the Internet; and (6) use at least one of the six most popular free Internet sites identified in the first phase of the study. By study design, respondents were recruited exclusively through the Internet and selected to include approximately equal numbers of European Americans, African Americans, Latinos, and Asian Pacific Islanders. We also stratified the sample to include about two thirds who reported both being HIV-negative and having had URAI in the previous year. We purposefully sampled men at higher risk for HIV infection by recruiting those who stated in their online profiles and/or during phone screening that they were HIV negative and had URAI in the previous year. On average, individuals meeting eligibility criteria were scheduled for a face-to-face interview three days after their initial screening.
Procedure
After giving consent to participate in this study, each respondent underwent an in-depth, face-to-face interview conducted by one of three clinical psychologists on our staff. This was followed by a structured assessment that used Computer Assisted Self-Interview (CASI) to collect information on demographic characteristics of the respondent, his sexual behavior in the previous two months, rectal douching, and HIV-testing information of self and last-two-months partners. The interviews lasted about two hours in total, at the end of which respondents were compensated with $50 for their time.
Measures
Demographic Characteristics
Respondents were asked to report their age, highest year of school completed, annual income (including money earned off the books), and ethnic and racial group membership. For ethnicity, respondents were asked to report if they considered themselves Latino or Hispanic. Those who did not identify as Hispanic or Latino were asked to report their race from the following categories: African American or Black, Asian or Pacific Islander, White or European American, Native American, and Other.
Sexual Behavior
Respondents were asked to report their sexual behavior with men and women during the previous two months. Questions were posed both in formal language and vernacular (in italics) to increase comprehension. Of relevance for the present report are three questions on sexual behavior with men in the past two months: (a) “How many times did a male partner put his penis in your rectum? (How many times did you get fucked in the ass?)”, (b) “How many times did a male partner put his penis in your rectum without a condom? (How many times did you get fucked in the ass without a condom?)”, and (c) “How many men put their penises in your rectum without a condom? (How many men fucked you in the ass without a condom?)”.
Douching Behavior
Respondents were asked about frequency, reasons for, timing, and age of onset of douching behavior. Questions that were not applicable were automatically skipped by the computer program (e.g., if the participant reported never douching, the rest of the questions on douching were skipped). The questions were: “How often did you douche or use rectal enemas in the past 6 (six) months?” “How many of those times did you douche in preparation for sex?” “At what age did you douche before sex for the first time?” “What made you douche before sex?” (possible answers were “To be clean,” “My sex partner suggested it,” “My friends talked about it,” and “Other [specify]”), “How frequently do you give yourself a rectal douche before sex? (possible answers were “Always,” “Frequently,” “Infrequently”), “At what age did you douche after sex for the first time?” “What made you douche after sex? (possible answers were “To be clean,” “To prevent getting any sexually transmitted infections, including HIV, from my sex partner,” “My sex partner suggested it,” “My friends talked about it,” and “Other [specify]),” and “How frequently do you give yourself a rectal douche after sex? (possible answers were “Always,” “Frequently,” and “Infrequently.”) Respondents who indicated that they had never douched were included into both douching frequency variables in a fourth category: “Never douched”.
HIV Status
Participants were asked whether they had been tested for HIV, if they had received their test result(s), and whether they were HIV infected or uninfected.
Data Analytic Strategy
We used univariate statistics to compare differences by HIV status across all study measures. After comparing different transformations based on how well they reduced the magnitude of the skewness statistic, a log-10 transformation was used to adjust for skewness in three variables (e.g., number of pre-coital douching occasions, number of URAI partners, and number of receptive anal intercourse occasions). We then used hierachical logistic regression to assess whether HIV status was associated with demographic characteristics (Model 1), number of pre-coital douching occasions (Model 2), and number of URAI occasions (Model 3). Number of URAI partners was not included in the model due to multicollinearity with number of URAI occasions (r = .90). Following a case-control study approach, we did not perform any adjustment for the oversampling of HIV-negative men and interpreted the odds ratio for model covariates without sample weights (Prentice and Pyke 1979).
Results
Sample Characteristics
One hundred twenty men were enrolled in the study. From these, we selected those participants (n = 105) who reported having receptive anal intercourse (RAI) in the previous two months, either exclusively (“bottoms”) or alternating with insertive anal intercourse (“versatiles”, see Table 1). Participants reported a mean age of 33 years (SD = 9.85 years), having some college education (M = 14.77; SD = 2.94), and an average income of $26,770 (SD = 23,790). Twenty-seven men (26%) reported being HIV-positive. HIV-positive men were older than HIV-negative men by an average of six years (t (103) = −2.61; P < .01), but did not differ in terms of education (t (103) = −0.01; ns), income (t (103) = 1.73; ns), or race/ethnicity (χ2 (1) = 6.44; ns).
Sexual Behavior
On average, participants reported having receptive anal intercourse on 11 (SD = 17.25) occasions over the past two months (see Table 2). Almost half of the sample (n = 49; 47%) reported having had one or more potentially serodiscordant partners in the past two months. HIV-positive men reported having greater number of URAI occasions (t (103) = −3.67; P < .001) and more partners with whom they had URAI (t (103) = −3.80; P < .001). HIV-positive men reported having more potentially serodiscordant partners than HIV-negative men (χ 2 (1) = 6.91; P < .01) and more URAI occasions with potentially serodiscordant partners than HIV-negative men (t (103) = −3.67; P < .001, not shown in table).
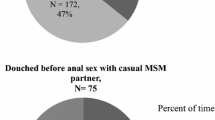
Douching Behavior
Rectal douching was a common practice among men who engaged in RAI (see Table 3). Almost two thirds of HIV negative men and all of HIV positive men reported douching in the prior six months. Most of the men who douched did it to prepare for anal intercourse, douching frequently or always when anal intercourse was expected. Douching after sex was less popular but present nonetheless, being practiced by slightly more than a quarter of HIV negative men and almost half of HIV positive men. However, only about half of them practiced post coital douching frequently or always, a smaller proportion than that of men who douched frequently or always before sex. Among the men who douched after sex, we found no differences by HIV status in post-sex douching behavior (χ2 (1) = 2.86; ns) or post-sex douching frequency (χ2 (1) = 1.37; ns).
Primary reasons for douching before sex among those who did it were wanting to be clean (n = 40; 60%), their sex partner had suggested it (n = 16; 24%), and their friends talked about it (n = 11; 16%). Three participants provided other reasons for douching before sex: “for better absorption of crystal-meth (booty bump)”, “read about it in a gay magazine”, and “to have more satisfaction”. The average age of onset for pre-coital douching was 25 years (SD = 8.22 years) and did not differ by HIV status (t (66) = 0.58; ns). We found no differences in pre-coital douching frequency by race (χ2 (5) = 5.64; ns), age (t (103) = −0.79; ns), education (t (103) = −0.05; ns), or income (t (103) = 1.44; ns).
Reasons for douching after sex among those who did it were that they wanted to be clean (n = 21; 64%), were trying to avoid sexually-transmitted infections (n = 8; 24%), were asked to do it by their sex partner (n = 3; 9%) and their friends were talking about it (n = 1; 3%). The average onset of post-sex douching was 27 years (SD = 9.73) and did not differ by HIV status (t (31) = .28; ns). The absence of differences, however, may be due to the smaller proportion of participants reporting douching after sex. Post-sex douching frequency did not differ by race (χ2 (5) = 5.64; ns), age (t (103) = −1.12; ns), education (t (103) = 0.77; ns), or income (t (103) = 1.37; ns).
Factors Associated with HIV Status
In our first model (see Table 4), we tested the association between demographic characteristics and HIV status. As shown in Table 4, older men (OR = 1.08; P < .01) in our sample were more likely to be HIV positive. We found only a trend association between lower income and HIV-positive status (OR = 0.98; P < .10), and no association between HIV status across race/ethnicity or years of education.
When we entered the number of pre-coital douching occasions into the regression (see Model 2 in Table 4), we found that greater number of pre-coital douching occasions over the past six months increased the likelihood of being HIV-positive (OR = 3.51; P < .01). In this model, the likelihood of being HIV-positive due to age (OR = 1.05; P < .10) and income (OR = 0.98; P < .10) became marginally significant. We found no association between HIV status across race/ethnicity or years of education.
We then entered the number of URAI occasions into our final model (see Model 3 in Table 4). The risk of being HIV-positive increased with greater number of URAI occasions (OR = 5.53; P < .05). The association between pre-coital douching occasions and HIV status decreased slightly (OR = 2.64; P < .05), yet remained statistically significant after accounting for all other covariates in the model. In addition, Asian Pacific Islander men were less likely to report being HIV-positive (OR = 0.12; P < .10) than their European American counterparts. No other race/ethnicity differences were found. Years of education, age, or income were not associated with the likelihood of being HIV-positive in the final model.
Discussion
Our study shows that rectal douching is a common practice among men who engage in URAI, being reported by more than two thirds of them across different ethnic groups. The behavior starts about age 25 with the main purpose of preparing for sex, and is done frequently or always. For HIV-negative men, douching may result in rectal mucosal damage that may facilitate the entry of HIV or other pathogens. In the case of HIV-positive men, whether rectal douching may exacerbate viral shedding needs to be investigated. Given that respondents practice rectal douching as a hygiene measure prior to sex, and considering the frequency with which the behavior takes place, it is likely to be quite resistant to change, as has been reported to be the case among women who use vaginal douches. Furthermore, the association between douching and HIV-positive status that persists after controlling for number of URAI occasions highlights the need to pay attention to rectal douching as a possible contributing factor to HIV transmission.
However, not all rectal douches may have harmful effects. Schmelzer et al. (2004) did not observe epithelium loss after PEG-ES enemas. Therefore, it may be possible to develop products that achieve the hygienic purpose pursued by users while avoiding harmful effects (Carballo-Diéguez et al. 1999). Furthermore, if a harmless rectal douche could be used as the vehicle to deliver an effective microbicidal agent, it could be possible to achieve wide coverage of the rectal mucosa with a protective agent prior to intercourse. A douche that were expelled or absorbed by the mucosa while leaving the microbicidal agent in any place that may become exposed to HIV during or after intercourse would probably be more acceptable than the current gel formulations of microbicides which may require a significant volume of gel to be present in the rectum during intercourse (Carballo-Diéguez et al. 2007).
Rectal douching after sex also merits attention, given that it is reported by a quarter of uninfected men and almost half of those infected. Would post-coital douching wash away a microbicide while ineffectively removing pathogens? Future research in microbicide development should consider the formulation of a multipurpose product that can be effectively used as a microbicidal and as a douche, not only before, but also after sex. Alternatively, future behavioral prevention interventions among MSM should consider incorporating cautionary information about the potential harms associated with douching after sex.
Rectal douching may increase the susceptibility to HIV and other sexually-transmitted infections by sloughing the anal epithelium (Fuchs et al. 2007). The prevalence of this behavior is consistent with findings from a small qualitative study among gay and bisexual men living in the Baltimore area (Hylton et al. 2004). Rectal douching was a common practice in our sample, with over two thirds of men reporting that they douched in preparation for sex in the past six months. From a prevention standpoint, this finding is somewhat troubling given that our sample consists of men who seek out sexual partners through the Internet for unprotected sex. As a prime population to benefit from the availability of HIV prevention alternatives to condoms, such as rectal microbicides, it is vital to decrease sexual hygene practices that may render the microbicide ineffective. For example, a potential harm reduction approach to minimize the sloughing of the anal epithelium may be to inform MSM on the risks of using soapsuds and water enemas and/or to increase the accessibility and marketing of PEG-ES enemas (Schmelzer et al. 2004).
Consistent with previous studies on rectal douching (Bienzle et al. 1985; Deininger et al. 1990; Koziol et al. 1993; Moss et al. 1987; Ndimbie et al. 1996; Schreeder et al. 1982), HIV-positive men in our sample were more likely to report having douched, before and after sex, than HIV-negative men. HIV-positive men were more likely to report greater number of douching occasions in the past 6 months than their HIV-negative counterparts. Taken together, these findings suggest that douching may increase opportunities for re-infection among HIV-positive men, particularly when they are the receptive partner (“bottom”). Nonetheless, our study’s cross-sectional design limits our ability to determine a causal association between douching and HIV infection. Furthermore, we requested information about douching in the prior six months, and HIV infection may have occurred much earlier than that. In order to determine the causal effect of douching on HIV infection, longitudinal studies would be necessary.
Most men in our sample reported that they wanted to be clean before and/or after having sex. This motivation is similar to previous findings among women using vaginal douches (Ness et al. 2003). In the case of vaginal microbicides, for example, it has become clear that hygienic practices such as vaginal douches, cleansing with fingers, or the introduction of vaginal dissectants in preparation for sex may affect the vaginal compartment in which the microbicide is expected to work (Koblin et al. 2002). Although findings from vaginal–penile microbicide trials should only be cautiously extrapolated to rectal–penile microbicides, rectal douching practices need to be carefully studied. The rectal compartment has a different physiology, morphology and function than the vaginal compartment and presents many challenges for the development of a microbicide that could be effective when used rectally. For example, it is anticipated that the volume of the microbicide to be used may have to be significantly larger for the rectum than for the vagina (Carballo-Diéguez et al. 2007). Future studies exploring what hygienic practices precede or follow anal intercourse and the effect that they may have on the action of a microbicide are necessary.
References
Bienzle, U., Guggenmoos-Holzmann, I., Zwingenberger, K., Thommsen, R., Ritter, K., & Uy, A., et al. (1985). Lymphadenopathy and antibodies to HTLV-III in homosexual men Clinical, laboratory and epidemiological features. Journal of Molecular Medicine, 63, 597–602.
Carballo-Diéguez, A., & Bauermeister, J. A. (2004). “Barebacking”: Intentional condomless anal sex in HIV-risk contexts: Reasons for and against it. Journal of Homosexuality, 47, 1–16.
Carballo-Diéguez, A., Dowsett, G. A., Ventuneac, A., Remien, R. H., Balan, I., Dolezal, C., Luciano, O., & Lin, P. (2006). Cybercartography of popular Internet sites used by New York City men who have sex with men interested in bareback sex. AIDS Education & Prevention, 18(6), 475–489.
Carballo-Diéguez, A., Exner, T., Dolezal, C., Pickard, R., Lin, P., & Mayer, K. H. (2007). Rectal microbicide acceptability: Results of a volume escalation trial. Sexually Transmitted Diseases, 34(4), 224–229.
Carballo-Diéguez, A., Stein, Z., Saez, H., Dolezal, C., Nieves-Rosa, L., & Diaz, F. (1999). Frequent use of lubricants for anal sex among men who have sex with men: the HIV prevention potential of a microbicidal gel. American Journal of Public Health, 90, 1117–1121.
Deininger, S., Müller, R., Guggenmoos-Holzmann, I., Laukamm-Josten, U., & Bienzle, U. (1990). Behavioral characteristics and laboratory parameters in homo- and bisexual men in West Berlin: An evaluation of five years of testing and counseling on AIDS. Journal of Molecular Medicine, 68, 906–913.
Fuchs, E. J., Lee, L. A., Torbenson, M. S., Parsons, T. L., Bakshi, R. P., & Guidos, A. M., et al. (2007). Hyperosmolar sexual lubricant causes epithelial damage in the distal colon: Potential implication for HIV transmission. Journal of Infectious Diseases, 195(5), 703–710.
Hylton, J., Hendrix, C., & Fuchs, E. (2004). An assessment of sexual practices affecting the feasibility of microbicide development among MSM. Oral Poster presented at Microbicides 2004, London.
Koblin, B. A., Mayer, K., Mwatha, A., Brown-Peterside, P., Holt, R., & Marmor, M., et al. (2002). Douching practices among women at high risk of HIV infection in the United States: Implications for microbicide testing and use. Sexually Transmitted Diseases, 29, 406–410.
Koziol, D. E., Saah, A. J., Odaka, N., & Munoz, A. (1993). A comparison of risk factors for human immunodeficiency virus and hepatitis B virus infections in homosexual men. Annals of Epidemiology, 3, 434–441.
Martino, J. L., & Vermund, S. H. (2002). Vaginal douching: Evidence for risks or benefits to women’s health. Epidemiologic Reviews, 24, 109–124.
Moss, A. R., Osmond, D., Bacchetti, P., Chermann, J. C., Barre-Sinoussi, F., & Carlson, J. (1987). Risk factors for AIDS and HIV seropositivity in homosexual men. American Journal of Epidemiology, 125, 1035–1047.
Ndimbie, O. K., Kingsley, L. A., Nedjar, S., & Rinaldo, C. R. (1996). Hepatitis C virus infection in male homosexual cohort: Risk factor analysis. Genitourinary Medicine, 72, 213–216.
Ness, R. B., Hillier, S. L., Richter, H. E., Soper, D. E., Stamm, C., & Bass, D. C., et al. (2003). Why women douche and why they may or may not stop. Sexually Transmitted Diseases, 30, 71–74.
Phillips, D., Taylor, C., Zacharopoulos, V., & Maguire, R. (2000). Nonoxynol-9 causes rapid exfoliation of sheets of rectal epithelium. Contraception, 62, 149–154.
Prentice, R. L., & Pyke, R. (1979). Logistic disease incidence models and case-control studies. Boimetrika, 66(3), 403–411.
Schmelzer, M., Schiller, L. R., Meyer, R., Rugari, S. M., & Case, P. (2004). Safety and effectiveness of large-volume enema solutions. Applied Nursing Research, 17, 265–274.
Schreeder, M. T., Thompson, S. E., Hadler, S. C., Berquist, K. R., Zaidi, A., & Maynard, J. E., et al. (1982). Hepatitis B in homosexual men: Prevalence of infection and factors related to transmission. Journal of Infectious Diseases, 146, 7–15.
Suarez, T., & Miller, J. (2001). Negotiating risks in context: A perspective on unprotected anal intercourse and barebacking among men who have sex with men—Where do we go from here? Archives of Sexual Behavior, 30, 287–300.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carballo-Diéguez, A., Bauermeister, J.A., Ventuneac, A. et al. The Use of Rectal Douches among HIV-uninfected and Infected Men who Have Unprotected Receptive Anal Intercourse: Implications for Rectal Microbicides. AIDS Behav 12, 860–866 (2008). https://doi.org/10.1007/s10461-007-9301-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-007-9301-0