Abstract
This article discusses ethnoveterinary medical pluralism in Western Kenya. Qualitative methods of data collection such as key informant interviews, open-ended in-depth interviews, focus group discussions (FGDs), narratives, and participant and direct observations were applied. The study shows that farmers in Nyang’oma seek both curative and preventive medical services for their animals from the broad range of health care providers available to them within a pluralistic medical system. Kleinman’s model of medical pluralism, which describes the professional, folk, and popular sectors, informs this discussion because of its relevance and appropriateness to the study. It is, however, important to note the overlap in the three sectors and to point out that livestock farmers engage in multiple “consultations” based on a combination of their own characteristics and the cost, availability and specialization of health care providers. The study concludes by recognizing the complexity of ethnoveterinary medical pluralism and calls for the integration of a pluralistic perspective into the planning and implementation of animal health care interventions and services.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In Kenya, as in many other developing countries, current veterinary practices involve several categories of practitioners and techniques. Very often, livestock farmers access animal health care services through the use of traditional techniques, modern pharmaceutical drugs, untrained animal health care dispensers, and private or government veterinarians. Decisions regarding health care choices for livestock are based on the perceptions of the cause of the health problem, belief in the efficacy of a given approach as well as the cost implications, particularly in resource poor households (Nyamwaya 1982; Cohen and Odhiambo 1989; Sindiga 1995; Martin and Mathias 1999).
This study draws upon the structural model of health care systems that was developed by Arthur Kleinman in 1980. Kleinman points out that individuals seek help with health problems within a local cultural system composed of three overlapping parts: the professional, folk, and popular sectors (Kleinman 1980, p. 50). The professional sector consists of the organized, healing professions. In most societies, this sector refers to the modern scientific medicine (Kleinman 1980, p. 53) also known as allopathic medicine or biomedicine. The folk sector, on the other hand, is the “non-professional, non-bureaucratic, specialist sector which shades into the other two sectors of the local health care system” (Kleinman 1980, p. 59) and which is either sacred or secular or a mixture of both. The popular sector is the lay, non-professional, non-specialist domain of society where illness is first detected and the first line of treatment offered, mainly at the household level. The popular sector “can be thought of as a matrix containing several levels: individual, family, social network, and community beliefs and activities” (Kleinman 1980, p. 50). “When people resort to folk or professional practitioners, their choices are anchored in the cognitive and value orientations of the popular culture. After patients receive treatment, they return to the popular sector to evaluate it, and decide what to do next” (Kleinman 1980, pp. 50–51). As Janzen (1978, p. xviii) notes, medical pluralism refers to the existence in a single society of differently designed and conceived medical systems. Such systems exist together and may compete with one another (Fabrega 1982, pp. 241–242) while Leslie (1976, p. 9) sees “medical systems as pluralistic structures of different kinds of practitioners and institutional norms.”
According to Martin et al. (2001, p. vii), ethnoveterinary medicine (EVM) refers to a holistic approach towards the provision of animal healthcare. Ethnoveterinary studies, they say, provide useful insights into animal (and also often human) healthcare and are equally useful into how animals and their diseases are perceived and managed in different societies. Thus, ethnoveterinary research and development encompasses social as well as biomedical sciences. It also links science and ethnoscience, or bodies of local (or indigenous or traditional) knowledge. It is not simply another topic in the broadening arena of non-conventional animal medicine. Rather, it recasts veterinary medicine in a more holistic perspective. Martin et al. (2001) insist that, while for millennia people have used home-grown veterinary skills and techniques to keep their animals healthy, it is only in the last decade that people’s local knowledge and skills received much scientific attention, under the rubric of EVM. This perspective they say was lost in many western societies, where for the past 50 years veterinarians have been taught that disease is purely a structural or physiological dysfunction. Whether in animals or humans, however, ordinary people see health and illness as far more comprehensive issues, often involving religion, environment, intra- and inter-species social relations, and more.
This paper seeks to show the complex interaction between the Kleinman’s three sectors in ethnoveterinary medical pluralism within a local socio-cultural context. In Kenya, Kleinman’s model has been used by Nyamongo (1998) to explain lay people’s response to illness among the Abagusi people of southwestern Kenya with great success. The same has however not been done with respect to animal healthcare. This paper also seeks to underscore the practical implications and appropriateness of this pluralism in a resource poor rural farming community in western Kenya and shows how it impacts on conventional veterinary health care services.
The research questions therefore are: What are the various local perceptions and practices concerning animal healthcare in Nyang’oma? How do these perceptions and practices interact with conventional veterinary perceptions and practices? Are conventional veterinarians aware of the local perceptions and practices and how do they take into account such perceptions and practices in their day-to-day programs and policy formulation? Additionally the paper seeks to show that by giving special attention to these perceptions and practices they stand to be exposed to more scientific scrutiny, which can lead to their validation and eventually to better animal healthcare provision and enhanced living standards of the rural poor.
Methods and procedures
Research site
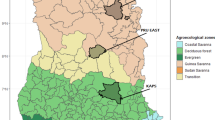
The study was conducted in Nyang’oma sub-location within Bondo district in Western Kenya along the shores of Lake Victoria (see Map 1 below). Nyang’oma sub-location is a rural community with a total population of about 5,000 people who are mainly Dholuo speaking. The Luo are a polygynous, exogamous, Nilotic and virilocal group with a patrilineal kinship structure (Hauge 1974, p. 11). The dominant religions are Anglican and Roman Catholic although Christian syncretic sects are also becoming common in the area.
The local economy is a mixture of livestock, crop production, fishing, petty trade, and small-scale gold mining. In the agricultural sub-sector, the major crops include sorghum, millet, maize, beans, cassava, potatoes, and vegetables. Most of these crops are grown for subsistence with a small surplus sold to provide income.
On livestock farming it was identified that the farmers in Nyang’oma categorize their animals into “large” and “small” stock. Poultry is categorized as “small stock,” while goats, sheep and cattle are in the “large stock” category. Two systems of farming have been identified. The majority are indigenous livestock farmers who keep such animals as the Zebu (Boran) cattle, sheep, goats, poultry, donkeys, dogs, and cats. Indigenous goats, cattle, and sheep are herded or kept under a tethering system while poultry are kept under a free range system. Dogs and cats survive from the food leftovers from their keepers. However, there are also a few farmers who practice commercial livestock farming and keep grade or crossbred cattle, goats, sheep, and poultry. Most farmers who keep grade or cross bred animals are relatively wealthy and do so mainly for commercial rather than subsistence purposes. However, in the contemporary setting the majority are indigenous livestock farmers who keep cattle for subsistence purposes and as a source of liquid capital. Traditionally cattle were also considered the main source of wealth and status and were used for payment of bride wealth.
Based on their knowledge of the vulnerability of the commercially bred animals to the harsh environmental conditions prevailing in Nyang’oma, many commercial farmers tended to provide better care to these animals than their indigenous counterparts. Many farmers who own grade and crossbred animals have planted Napier grass for feeding their animals. Napier grass is also planted for sale. Many farmers have acquired crossbred and grade animals for economic and social reasons. These animals are considered to be more productive than the traditional type and confer more prestige.
According to the traditional patterns of household resource allocation and division of labor any woman or young person can own an animal, but in a de jure sense these animals belong to the husband who is the “owner” of the home or head of the household. In polygynous homesteads, men allocate cows to their wives so that every wife can get milk. This also ensures that each can be responsible for taking care of the animals allocated to her. Even where a “herdsman” is employed to look after the animals, it is still the woman who is in charge of the day-to-day management of her animals.
Children are mainly responsible for looking after poultry, which many of them own. They can either buy or get them as presents from relatives and friends. The children play an important role in feeding and safeguarding the health of the family poultry. One common practice for feeding these poultry involve trapping white ants by digging shallow holes on the ground then placing dry sticks and grasses. These attract the ants that can easily be collected into containers. This is considered a special food for poultry. Local poultry consist of indigenous birds raised as scavengers in the backyard under a free range management system.
Both men and women provide animal health care services in Nyang’oma. However, most female practitioners tend to use herbal medications while men are the main practitioners in surgical treatments such as bone-setting, dehorning, castration, removal of false teeth, ear notching, venipuncture, and docking. Although most practitioners tend to be elderly people, children also have some knowledge, which they use in treatment. Docking is especially done by boys and many children are also aware of the herbal concoctions for poultry illnesses. Despite this intergenerational role sharing, the flow of information on animal health and husbandry is dependent on the subject. Some knowledge is common to the public while some, especially those related to the use of herbal medicine, are special and remain the preserve of a few families. Such specialized knowledge can only be given under special arrangements such as payment or apprenticeship.
Study design and data collection methods
Data collection was conducted from December 2002 to July 2004. Qualitative methods of data collection such as key informant interviews, open-ended in-depth interviews, focus group discussions (FGDs), narratives, and participant- and direct observations were used. The study participants were purposively selected from the population within the sub-location based on their expert indigenous knowledge on livestock health care. It is important to note that all the interviewees including the professionals were members of the Luo community with good command of the language. The interviewer himself was also a member of the community who had good comprehension of both Dholuo (the local language) and English. Thus, interviews were mainly conducted in the vernacular, Dholuo, and recorded in English. Where the informants were proficient in English, interviews were mainly done in English though some short interludes in Dholuo helped to ascertain differences in terminologies and perceptions. The data were subsequently analyzed based on identification of main themes, coding, and linking. All names used in the article are pseudonyms.
The characteristics of practitioners who provided information through key informant interviews are summarized in the Table 1. Their ages have been deliberately left out to avoid obvious identification as the study promised anonymity of the participants. Some practices such as docking and ear notching had no specific practitioners and so farmers were relied upon to give information. On the other hand supernatural practitioners interviewed on this topic were not readily available, so again farmers were relied upon. All informants gave verbal informed consent.
Findings
A wide range of practitioners is consulted whenever an animal illness is detected and decisions are made regarding treatment (see Table 1).
Animal health care within the professional sector
Trained veterinarians in Nyang’oma are rare. Such practitioners include university graduates and diploma and certificate holders in animal health. Some of them work as government employees while others practice privately and, often, illegally without licenses. Among the unlicensed private professional practitioners are retired government veterinary personnel. The government veterinary personnel who have a contact office at the divisional headquarters attend to livestock diseases. However, these veterinarians are rarely found in their offices, so livestock farmers usually travel long distances to the district veterinary office for services.
Government officials are consulted especially in situations of disease outbreaks for which livestock farmers have no previous or specialized knowledge. According to one cattle keeper who is also a retired driver with the veterinary department, “the government veterinary departments have more special facilities and equipment and so are better placed to take samples for testing then advise farmers on which drugs to use.” Farmers who own cattle also consult government veterinary officers because they consider these animals to be more vulnerable to the harsh environmental conditions in Nyang’oma. One informant captured this when he said, “these grade animals need special treatment. They are not like our indigenous ones. If they do not get better treatment they can not perform well here.” Those who own grade and crossbred animals are therefore the major consumers of government veterinary services.
The government veterinary staff usually organizes field days to vaccinate animals and to teach farmers about new husbandry techniques. Such field days are rarely attended by the indigenous livestock farmers. Commercial livestock farmers, however, attend these sessions in large numbers, and vaccination is frequently carried out in these settings. Some of them call the veterinary staff to their homes to provide the service. This is mainly based on farmers’ knowledge of the vulnerability of the commercially bred animals to the harsh environmental conditions prevailing in Nyang’oma as opposed to their indigenous counterparts which are known to be hardy and better adapted to those conditions. However, values are changing with many farmers appreciating modern therapeutic, preventive, and promotive interventions.
Animal health care within the folk sector
Apart from the professionally trained practitioners, farmers also consult “traditionalists” who provide different types of ethnoveterinary health care services. As Kleinman (1980) puts it, this is the domain where practitioners draw from local knowledge and specialize in different forms of healing which are either sacred, secular, or both. The web of community social relationships is a major determinant of service provision in this domain. In Nyang’oma the practitioners consist of both adult males and females. Most livestock farmers consulted them because their charges are relatively cheaper and can sometimes be provided on credit, free of charge, or paid for in kind. The practitioners live within the community and are therefore readily accessible.
Herbal specialists
Herbalists who are locally known as joyadh nyaluo (jayadh nyaluo, sing.) are the main group of ethnoveterinary practitioners. In Nyang’oma, these practitioners are considered more effective in dealing with certain types of animal illnesses. Such illnesses include biero momoko (“retained placenta”) and yamo (an illness that leads to swellings and wounds). Most farmers believe that several animal health problems originate from the stomach and then spread to different parts of the body where they manifest themselves in various forms such as small swellings, boils or general dullness of the affected animals. Herbal medicine is administered to animals as a drench in order to trigger diarrhea that expels the “bad things” believed to cause illness. Herbal medicine is also considered the most appropriate in treating udder and teat problems. The illness is believed to be caused by dhoho (“evil eye”).
An important point is that herbal medications are mainly administered to indigenous animals and rarely to grade and crossbred animals. This also goes with the same reasoning on the vulnerability of commercially kept livestock. They are expensive to obtain and nobody would want to gamble with their health. Provision of the most effective treatment as fast as possible is recommended.
It should also be noted that herbal drugs are sometimes used as prophylaxes. Thus, a combination of herbs such as pilipili (Capsicum frutescens, Solanaceae), ogaka (Aloe spp. Aloeaceae) and minya (Cissus quadrangularis, Vitaceae) can be crushed, mixed with water, and given to poultry as a drench to prevent any form of illness. (For botanical names see Kokwaro and Timothy 1999).
In terms of sequencing, herbal therapy is often given in combination with or after modern therapy, because it is believed that herbal medicine has some purifying quality and can therefore clear any residual maladies after modern therapy. Nyang’oma farmers believe that modern veterinary medicine is effective in combating illness faster because it strikes directly at the location of the illness. However, they believe that modern drugs lack certain purifying qualities associated with herbal medicine and that therefore it is necessary to administer a dose of herbal medicine alongside the modern therapy. In the treatment of poultry, for example, a combination of the concoction sited above is mixed with other conventional drugs such as aspirin (conventional painkiller), tetracycline capsules (commercially manufactured antibiotics), and even anti-malarial tablets.
Very often, there are differences and convergences in perceptions between the folk practitioners and their professional counterparts. Professional practitioners often concur with their folk counterparts especially on the naming and perceptions concerning yamo. This was confirmed by one veterinary doctor in private practice who maintained that “yamo was real and that indeed there were several different kinds of yamo. These came as boils (buche, pl., bur, sing.) and swellings in the body or legs.” However, with regards to the efficacy of herbal medicine in the treatment of illnesses there are some differences. For example, one herbalist insisted that “traditional medicine is still much better in the treatment of yamo. Modern medicine does not completely rid the body of yamo the same way traditional medicine does.” The veterinarian, however, objected to herbal treatment. She maintained that it is difficult to know the ingredients and the right dosage of an herbal concoction. Instead she preferred injections with pen and strip (a conventional antibiotic) for the yamo cases.
There are also marked differences of opinion with respect to the illness resulting from the evil eye or dhoho. The professional veterinarians maintain that the illness is a natural phenomenon which is caused by bacterial infection. They call it mastitis and treat it with commercially manufactured pharmaceuticals.
Orthopaedic specialists
Traditional bonesetters are known locally as jochomo (jachomo, sing.). They deal with cases of chogo motur (broken bone) and fuoni mowil (dislocated joints). There are many such practitioners in Nyang’oma. They often fix broken bones by applying certain types of herbal medicine as well as splints. Once herbal medicine has been applied on the area with a broken bone and dislocated joints, the bone is held in position by osembo (a string of sticks that are tied around the affected areas). The sticks are not removed until the animal heals. However, they may occasionally be removed and replaced if the healing process seems to be taking long and there is need to start the herbal treatment afresh. Although this study did not establish how cases of broken limbs of grade animals are handled, it was reported that in cases of indigenous animals farmers believe in jochomo whom they regularly consult. In some cases sick animals are not treated but left to heal on their own but if their health continues to deteriorate they may be slaughtered and eaten. Because of the high value attached to them, cattle, sheep, and goats are commonly attended to by jochomo in cases of broken bones. The less valued dogs and donkeys on the other hand were left to heal on their own while poultry would simply be slaughtered and eaten.
Bone setting by the professional practitioners was not observed during fieldwork. However, one veterinarian reported that broken bones are often put in place by wrapping plasters along the straight bones and left there for some time to let the bones heal. However, the veterinarian conceded that the practice was not as effective as that of the traditional setters as the bones often did not heal properly and the animals would continue to limp. According to him, the traditional orthopaedic specialists tend to be more effective than their professional counterparts.
Obstetric specialists
Biero momoko (retained placenta) is considered to be a serious animal health problem. Traditional removers of retained placenta, jogol biero momoko (jagol biero momoko, sing.), are common in Nyang’oma and deal with these birth complications. Retention of the placenta is reported to be more common among cattle than goats, sheep, donkeys, cats, and dogs. Retained placenta is removed with the use of local herbal medicines such as odagua (Ricinus communis, Euphorbiaceae), olusia (Vernonia amygdalina, Ateraceae compositae), and nyang’liech (Sateganotaenia arahacea, Umbeliferae), which are crushed, mixed with water, and administered orally as a drench to the affected cow (for botanical names see Kokwaro and Timothy 1999). An elderly woman who specializes in removing retained placenta spoke about what she usually does, “I remove biero momoko by inserting my hands into the uterus then pull it out. There are herbal medicines that I apply on my hands to help remove the placenta faster.” Immediately after a cow gives birth, the owners of the cow begin to monitor the animal to see if the placenta will come out by itself. This is partly done to prevent the cow from eating its own placenta as this is considered a bad habit that leads to poor health and to low milk output. Retained placenta may as well lead to poor health and even death of the affected animal. If it takes two to 3 h before the placenta comes out then it is considered risky and experts are consulted.
This herbal therapy is generally considered to be very effective and mainly applied on indigenous zebu cows. Fieldwork did not establish any cases where it was done to grade cows. Birth complications affecting grade cows are dealt with by government veterinary personnel. A veterinarian reports that he also removes retained placenta by physically (gloved) inserting hands into the vagina of the cow and pulling out the placenta. According to him the placenta has tentacles which they hold to pull it out. After the removal of the placenta, they apply some antibiotics to prevent infection. The risky period starts 6 h after delivery according to the veterinary professionals.
Dental specialists
Among the farmers in Nyang’oma there is a strong belief that jimo (“false teeth”) can sprout on the jaws of heifers between the ages of four to five years. According to the local ethnoveterinary dentists, these teeth are known to be thin, long, and pointed and only sprout on top of the gum. It is believed that their roots do not penetrate deep into the jaw. This means that when a young heifer feeds, the roots of the teeth can knock against the jaw and the heifer feels pain which makes it difficult to feed normally. Such a heifer would have poor health. Diarrhea is considered one of the indicators of the existence of such teeth in an animal. The therapy is to remove the teeth. A specialist who removes false teeth reports that a heifer with these teeth will not be able to conceive and give birth. However, once the teeth have been removed, there will be no more fertility problems. In Nyang’oma there are several specialists, or jomuk jimo (jamuk jimo, sing.), who know how to remove false teeth. It was reported that an ox could have as many as eight to ten of such deformed teeth. They are traditionally removed using pointed objects such as the hind side of a file. A little salt is applied after their removal to disinfect the wound. After removal, the animal can eat normally and grow big, fat, and healthy.
According to the veterinary personnel in Nyang’oma, an animal’s teeth can also be deformed as a result of the wear and tear of feeding. Some teeth also sprout besides the jaw line, making them abnormal and thereby interfering with normal feeding of an ox. In their view, these are also jimo. They maintain that there are no other special teeth. Another veterinary practitioner who partly agreed with the traditionalists added that, “even in the traditional practice the animals that are commonly identified with the problem are young and may still have the milk teeth.” She pointed out that these teeth are weak and can easily be knocked out using a strong implement such as pliers and secateurs.
Surgical specialists
According to the Nyang’oma farmers, animal husbandry often involves surgical operations for purposes of illness prevention, treatment or health promotion. Some of these surgical procedures involve special knowledge and skills to perform and require specific specialists while others are simple procedures which farmers can do themselves. Venipuncture, castration, and dehorning are examples of surgical procedures that require special knowledge.
Venipuncturists
In Nyang’oma venipuncture is a therapy for an illness called aremo. Aremo is a condition in which the affected animal is perceived to have too much blood in its body. An ox about to contract the illness shows signs of abnormal agility. In the case of a serious attack, limping, rough and dark hair coat as well as dullness are some of the symptoms of the illness. Blood letting is recommended to reduce the blood volume in the body. This is done through venipuncture where the great neck vein of an affected animal is impaled to let some blood flow out of its body. This practice, which is locally called boro, consists of tying a rope tightly around an ox’s neck so that the great neck vein can be seen and be impaled. The impaling is done on the head side of the vein. The practitioners, locally referred to as joboro (jaboro, sing.) use a bow and a special type of arrow (atung’) whose blade has an obstructing cloth tied at its base so that only a small part of the blade can pierce the vein. The practice is mainly a male responsibility. It was reported that the practice has undergone some changes. Some venipuncturists now use a sharp knife to stab the vein while others draw blood from the vein using a needle and syringe.
After trapping the blood some dung or ash is smeared on the wound. It is reported that the number of venipuncturists is going down in the community because the practice is considered outdated and also due to the perception that modern veterinary therapy tends to address aremo illness more effectively. However, some livestock farmers still apply both approaches, with venipuncture being used as first aid whenever modern medication is not immediately available.
Professional veterinarians have conflicting views concerning bloodletting as a treatment for aremo illness. One veterinary officer in Nyang’oma states that: “A sick animal needs blood to fight illness using white and red blood cells. A sick animal should not be made to lose blood. Aremo is just a bacterial infection and is not caused by too much blood in the animal’s body.” Another veterinarian, however, felt that bloodletting as first aid can be effective. According to him the practice can lead to reduced parasites in the blood of the affected animals, thus allowing the white cells to effectively fight the residual parasites and thereby restoring the animal’s health.
Thus, while the conventional veterinarians share the same terminology, aremo, with the local farmers and have some general agreement about treatment, they hold different opinions concerning the pathogenesis of the illness. Interestingly, though, both the local farmers and the veterinarian often refer to the same illness using modern veterinary terminology, “black quarter.”
Castrators
Some ethnoveterinary practices are carried out not only for therapeutic purposes, but also because of other expected benefits. Castration is believed to make a bull grow faster and gain more body mass. It is also done to tame a bull and make it easier to handle. Castrated bulls can be used in ploughing. Castration also reduces incidences of contagious disease because the bulls do not roam around once they have been castrated. The procedure is also carried out to reduce incidences of in-breeding which is considered “sinful” and dangerous. It is believed that in-breeding may make animals infertile or give birth to abnormal offspring. Given this belief, only a few bulls with desired qualities are not castrated.
Several traditional castrators practice in Nyang’oma. They are locally known as jopuoto (japuoto, sing.). The act of puoto involves hitting the sperm ducts of a bull using such objects as a hammer or a log. Two sticks are placed at the scrotum on either side of the sperm ducts and hit to cut the sperm ducts. However, some practitioners admit that when aiming at the sperm duct it is possible to accidentally hit the testicles thereby causing serious harm to the animal. Some farmers therefore prefer modern castration techniques that employ the burdizzo (a pliers-like tool with sharp jaws for cutting the sperm ducts) and they consider this to be a safer method although it also carries some risks, particularly when a bull jerks. Commercial livestock farmers mainly rely on trained personnel to castrate their animals. However, some jopuoto have learned how to use the modern technique alongside the traditional puoto. Most farmers who own indigenous bulls depend largely on the traditional practitioners who are mainly male adults. While the practitioners are capable of using both techniques, there was only one person in the village who owned the burdizzo that the other practitioners would borrow. Whenever practitioners are unable to access the burdizzo they rely on their traditional skills. Some livestock farmers, however, believe that the traditional technique is better than the burdizzo technique because “it makes a bull grow fat and more healthy,” according to one expert.
Dehorners
Dehorning is mainly done to goats and cattle. With respect to goats, there is a belief that the first horns are not strong enough and should be removed to let the goat develop stronger ones and have better health. It is believed that if the first horns are not removed they make a goat to lose weight and become stunted. They also believe that these horns can cause the thinning illness (achiya) in goats. Once they have been removed it is believed that a goat gains weight and becomes more attractive. Dehorning is usually done to a goat at the age of two years. Specialists who dehorn goats, jomuk tung’ (jamuk tung’, sing.) traditionally pulled out the horns using their teeth but pliers and other implements can also be used.
Many farmers with traditional cattle breeds tend to rely on the traditional technique of dehorning which involves cutting off the tips of an ox’s horn using a hack saw or a hot panga (machete). Cattle are mainly dehorned to prevent injury to handlers and other animals. Thus, length and sharpness of the horn as well as aggressiveness of the animal determine if and when dehorning is to be done.
Conventional veterinarians perform “debudding,” or, the removal of the horn buds in calves to prevent the growth of horns. Professionally this is done by applying a caustic compound during a calf’s first week of life. In Nyang’oma a veterinarian reported that whenever there is lack of the caustic compound they alternatively disbud calves horns using a hot iron implement, which cauterizes the place from where the horns are expected to sprout. This prevents the horns from sprouting and is believed to make an ox fat and docile. However, in Nyang’oma this practice is only common with commercial livestock farmers who can afford the services. Because it is done before calves’ horns sprout many people have often thought that grade and crossbred cattle are naturally hornless.
Injection specialists
Several practitioners offer veterinary services without having been trained in animal health care. In Nyang’oma these practitioners are called jobilek (jabilek, sing.) or quacks, or simply “injectors,” locally josandan or jochuopo (pl.), jasandan or jachuopo (sing.). These terms for the injectors are not very specific and can be used broadly to refer to qualified practitioners as well. The jobilek combine both conventional and traditional medicine in treating animals. They inject animals using modern drugs bought from veterinary shops, yet their perceptions of illnesses tend to concur with those of other farmers who treat animals using traditional herbs. One jabilek explained that, “aginga is an illness caused by a lot of blood in the body. Letting that blood flow out through ear slitting is necessary to make the animal healthy. But for a faster and more effective treatment animals should be given Adamycine (a commercially manufactured antibiotic common in veterinary shops around Nyang’oma) injections.”
Some community members consider the treatment offered by jobilek to be dangerous, as they are not trained. Commercial livestock owners prefer trained veterinarians to avoid any complications that could arise from the work of quacks. One of them reported that there were several instances where the jobilek were found to have under- or overdosed the animals. Despite the risk, the quacks are still consulted by most livestock farmers because their services are cheaper and can sometimes be provided on credit, free of charge or paid for in kind. The other advantage is that the quacks live within the community and are readily accessible.
Supernatural specialists
Some animal illnesses are attributed to ndagla (“witchcraft”). Some key informants reported that jandagla can place magical substances in the cowshed or sheep pen in order “to make the animals sick.” If this happens, a specialist in ndagla (jandagla) is called to undo the harmful magic. In a case where such witchcraft paraphernalia is the suspected cause of an animal’s illness, the remedy is to seek counter magic to neutralize the effects of the one “planted” in the home. Those who perform the cleansing act are referred to as jothieth (jathieth, sing.), a term that carries a positive connotation. Jothieth are widely perceived as “good people” who help victims of witchcraft. It is also a term which is used broadly to refer to different types of magicians. In Nyang’oma community several magicians are consulted secretly because magical practices are viewed as backward and sinful. People tend to be suspicious of individuals who practice magic. Sometimes joroho (jaroho, sing.)—religious persons with the power to “see” (divine) the planted magical paraphernalia may also be invited to come and remove the harmful paraphernalia or deactivate them so as to restore the health of the affected animals. There is a large membership of the syncretic Roho churches in Nyang’oma and it is believed that they have the power to “see” and “remove” what jandagla has placed in cowshed. The causes of witchcraft were given as jealousy and competition among family friends and neighbours. Given the secretive nature of their operations, the study could not determine the specific consumers of their services because of the stigma attached to this practice.
Animal health care within the popular sector
The popular sector involves the use of simple remedies that are administered by the livestock farmers themselves, their neighbors or relatives at home whenever an animal is ill. Such remedies are often applied as first aid measures. Most livestock farmers have comprehensive knowledge of various animal illnesses and also know how to prevent or treat them. Some farmers massage their animals as first aid, especially against aremo illness. Under this technique, aching muscles, joints, and limbs are massaged using either plain warm water or warm water mixed with salt and herbal medicine such as crushed leaves of dwele (Melia azedarach, Meliaceae). It is believed that the herbal drug enters the body through the skin and relaxes the muscles and also removes any blood clot.
Other surgical operations are simple and can be performed by the farmers themselves for purposes of health promotion, illness prevention or treatment. They include docking and ear slitting.
Docking
This is surgical operation which involves amputating a lamb’s tail and serves several purposes. A bigger portion of a female lamb’s tail is amputated to allow for mating while only a small portion of the male lamb’s tail is amputated. The practice is believed to be aesthetic as the docked sheep becomes more beautiful than the non-docked one. Other informants said that docking helps in distributing fat evenly throughout the body of a sheep. Amputation is done to lambs at about the age of 2 months. The sheep’s tail is amputated using a hot machete (panga) or knife. The resulting wound is then cauterized using a hot object such as a panga or potsherds. The wound is disinfected by applying a little salt. Even though adult males usually dock the animals, young boys prefer to do it and the piece of meat that comes from the tail is considered a delicacy when roasted.
Docking is considered a simple procedure and is therefore performed by the farmers themselves without consulting professional veterinarians. However, a professional veterinarian who was interviewed on this issue supported the farmers and emphasized the importance of docking in order to facilitate mating, distribution of body fat, and beautification of the wool.
Ear notching
Ear notching or slitting is the practice of amputating a small part of an animal’s ear or simply slitting the ear in order to let out blood. This bloodletting is done as a treatment for aginga, an illness common among calves. A calf suffering from this condition shows symptoms such as swelling under the ears. The perception is that the swelling results from “bad blood” that clots in these regions. The farmers believe that too much milk left for the calf to suckle causes this illness. It is also believed that a calf will develop aginga when it swallows hair while suckling its mother. A preventive strategy is therefore to leave only a little milk for the calf to suckle after milking a cow. The treatment involves slitting or notching the ears of the affected calf to allow the “bad blood” to flow out, thereby leading to recovery. The practice does not require special skills and many livestock farmers know how to do it. It is mainly done by male farmers and therefore lacks a specific title for its practitioners.
This practice is often criticized by professional veterinary practitioners who see it as a cruel act that causes pain and leads to loss of vital blood. According to the critics, aginga is simply East Coast Fever (ECF), an illness transmitted by ticks and can be treated with commercially manufactured antibiotics such as Butalex or Adamycine injections. However, one professional veterinarian argued that farmers must have benefited accidentally from the fact that bloodletting helped reduce parasites in the blood and allows the white blood corpuscles to fight the residual parasites.
In many other cases, ear slitting/notching is done to identify the animals. Slitting for purposes of identification is common with donkeys because they resemble each other. Professional veterinarians reported that identification is the main reason for ear slitting. Sometimes ear slitting is done for aesthetic purposes. Livestock farmers who own fat and big bulls often slit their ears to make them “beautiful” and “warrior-like.”
Most livestock farmers in Nyang’oma have learned how to inject their own animals and administer several non-injectable drugs that they buy over the counter. Friends often offer advice or treatment for free or charge less than the other service providers with scientific knowledge. The livestock farmers have established several animal health networks among themselves. Thus, it is not only economic forces that determine health care choices for animals, but social relations also play a major role in the provision of animal health care services.
Farmers neither stick to one particular healer nor to one particular method of treatment, but oscillate between several treatment techniques and specialists so long as a cure has not been found. In most cases, they alternate between the private and government veterinary personnel. A conversation between three livestock farmers one evening at Nyang’oma shopping center illustrates the practical reality of ethnoveterinary medical pluralism in Western Kenya.
-
Owilli:
Yes, the illness attacked the bull when I was away. I traveled to Kisumu and only young children were left at home. When I came back my children told me that the bull first appeared dull then after some time it started trembling after which it fell down and just died like that.
-
Joram:
Oh! There should have been an elderly person at home during your absence. The bull simply needed proper massage. You just warm water and using a cloth you massage the fatigued parts thoroughly. You can add leaves of dwele [Melia azedarach-Meliaceae] to this water and continue with the massage. At least after this massage you will obviously see that the bull can stand up and walk normally. You know aremo is just due to the blood that clots around the joints. So if you massage with hot water, this clotting blood will flow normally. Dwele leaves are especially good when put in that boiled water. If you still suspect any problems then you can call a jasandan [injection specialist] to give more treatment. You can also contact Maria Nyaseda who knows several types of herbal medicine that can treat such animal illnesses.
-
Owilli:
In fact after thorough massage, if God allows, the ox will be fine.
-
Joram:
Yes, from there you just pray and leave everything to God.
-
Hosea:
In fact Odingo [a trained private veterinarian who also sells veterinary drugs at a nearby market center] really knows how to administer injections in such cases. He also has good drugs that he can sell to you and you just administer personally to sick animals. He also charges cheaply for the drugs and services rendered.
-
Joram:
But aremo is not a real problem these days. Even Opiyo Molla [a jabilek] or Osumu Otunga [a retired vet clinician] treats it quite well.
It is evident from this conversation that the illness was first detected at home (the popular sector) where the response could involve several home remedies. Some of these could be offered as first aid, for example, in the case of massage or ear notching while at the same time drugs could be bought over the counter and individually administered by the farmers to their animals. From here treatment could be taken over by specialists either in the professional or the folk sectors. In the professional sector trained practitioners such as a private veterinarian could be consulted. In the folk sector an herbalist could offer therapy while sometimes the farmers could consult jobilek. Prayers were also considered as an integral part of animal health care delivery service.
There are cases when the treatment of an animal is not carried out immediately an animal illness is detected. Farmers tend to wait to see if the animal can recover on its own without any treatment. A livestock farmer explained, “you have to look at the ox for some time. Maybe the illness is just passing. It is only when you realize that the illness is becoming worse that you start looking for ways of treating it. An ox has a lot of strength. Simple illnesses may not affect it.” Sometimes the waiting has to do with lack of resources needed for the treatment. As was reported by an informant, “sometimes an animal may fall sick when you don’t have money for treatment and you have to wait until you get money. That is when you seek treatment.” The waiting can also be due to the ease with which domestic animals are disposed of. Sick or dead animals are often slaughtered and eaten by people in Nyang’oma.
Discussion and conclusion
The study has shown that the structural model comprising three sectors of human health care developed by Kleinman in 1980 is also applicable to animal health care in Western Kenya. Among the Nyang’oma farmers these sectors—the professional sector, the folk sector and the popular sector—are identifiable. The first category is composed of individuals trained in modern techniques of animal health care. Kleinman calls it the professional sector, or the domain where we find the organized, legally sanctioned healing professions such as modern western scientific medicine. In the animal health care setting, the practitioners in this sector include professionals who have been trained in veterinary or animal health sciences. Most of the practitioners are government employed and privately practicing trained veterinarians.
The second category includes the traditional experts who are classified by Kleinman under the folk sector. Among the Nyang’oma animal health care providers these traditionalists who offer various ethnoveterinary services practice without any formal training and do not have any formal authorization from the government. The category includes healers such as herbal specialists, orthopaedic specialists, obstetric specialists, dental specialists, venipuncturists, castrators and dehorning specialists. Supernatural specialists and the injection specialists also fall into this category. These experts rely on traditional and/or modern biomedical diagnostic and treatment techniques. In this sector some illnesses are considered special and can only respond to herbal medicine and other traditional approaches. Examples include yamo, biero momoko, and dhoho. In a separate study in Bondo district, Geissler et al. (2002) found similar perceptions concerning yamo in human illness. (See also Nyamanga et al. 2006a). It is quite important for veterinary practitioners to be aware of these specialists, their perceptions, and practices in order to design effective intervention programs that would include training as well as incorporation of practices and perceptions that have undergone validation and been found acceptable.
Third, Kleinman’s popular sector corresponds to the use of home-based remedies in animal health care. This is the sector where illness is first detected and the first line of treatment offered. As Kleinman puts it, this “is the lay, non-professional, non-specialist, popular culture arena in which illness is first defined and health care activities initiated” (1980, p. 50). Treatments are often done as first aid measures before other experts are consulted. Some of the remedies in this sector include massage, docking, ear notching or treatment with over-the-counter drugs. It is also in this domain where decisions on which practitioners to consult are made. Home based training to farmers may be considered by interventionists to enhance their capacity.
Although there are important differences between the sectors, they also overlap. Some illness concepts are shared between the professional and folk practitioners even if the perceptions about pathogenesis are different. This was identified in illnesses such as achany, aremo, aginga, and jimo where the professionals and traditional practitioners use the same terms. Very often, scientific terms are also shared. For example, terms like foot and mouth disease (to refer to achany), mastitis (to refer to dhoho) and black quarter (to refer to aremo) or ECF (to refer to aginga) are used by many jobilek and other traditional practitioners as well as the livestock farmers themselves. In many cases, however, the pathogenesis differed so that mastitis (dhoho) was seen by the livestock farmers as being caused by the “evil eye,” whereas in the professional sector this was an illness caused by bacterial infection. Such differences in perception also lead to different treatment approaches. For the folk practitioner, mastitis responds well to herbal therapy, whereas the professional veterinarian often recommends commercially produced antibiotic therapy. In many surgical and manipulative operations, there are similarities between all the three sectors and the differences are relatively few. Such similarities are discernible in dehorning, bone setting, removal of retained placenta, docking, and castration. The operations are similar although the conventional veterinarians sometimes criticize the traditionalists of clumsiness in the way they handle these surgical operations. These findings point to the practical importance of coming up with an ethnoveterinary dictionary explaining local people’s perceptions about animal illnesses and how they respond to it and containing a subsection on the position of conventional veterinary on the same.
There are several areas where perceptions tend to be unclear given the fact that most of the professional veterinarians interviewed come from the local community and tend to share the farmers’ worldview. For example, while some professional practitioners reject bloodletting (venipuncture and ear slitting) as treatments for aremo or aginga conditions, others feel that these practices may have some minimal therapeutic value—reduced parasitic load leads to recovery. This observation has been made by Nyamanga et al. (2006b). It points to the possible convergence between ethnoveterinary perceptions and practices with those of conventional veterinary, which needs to be strengthened through validation tests and training. It should, however, be emphasized that many of these practices have been used elsewhere and explained in EVM literature as making good practical sense in veterinary medicine and husbandry wherever other more sophisticated options are unavailable (Mathias et al. 1996; Martin et al. 2001). For example, a rather similar practice of bone setting which involves lancing the affected area to make blood flow and then splinting the leg with rawhide wrapped in sticks has been observed in the treatment of horses among North American Indians (Lawrence 1996). As was noted in Nyang’oma, African bonesetters’ skills have been widely verified in the literature as being effective and sometimes even superior to western—trained professionals (McCorkle, personal communication). Even disinfection using materials such as cow dung, ash or salt have been identified (Martin et al. 2001, p. 8) to be effective in some situations.
While many of the traditional practices still play an important role, some of them are declining. For example, modern therapies are becoming more popular compared to traditional practices such as boro (venipuncture) because the former are perceived to be more effective in the treatment of illnesses such as aremo. Modernization has also glorified the conventional veterinary practice and relegated some of the traditional approaches to inferior positions where the practices and beliefs are perceived as backward, primitive, non-progressive, and sometimes harmful. In addition, population growth and the increased need for land has led to the increasing scarcity of many herbal plants as large tracts of land are cleared for farming and human settlement. This observation has also been made by Saimo et al. (2003) in Uganda. This finding calls for greater efforts geared towards environmental conservation, for example through the planting of herbal plants in home gardens.
The government of Kenya has recognized that the ethnoveterinary practitioners form an important part of animal health service delivery at the community level. In some parts of Kenya, they have been identified and offered training to improve their capacity. This has been done mainly in the arid and semi-arid parts of Kenya, particularly among the Turkana and Samburu communities where ethnoveterinary knowledge has been analyzed for possible effect and partial integration of the two animal health care systems at the community level has been implemented (IIRR (International Institute of Rural Reconstruction) 1996; ITDG 2002a, b, 2006). This initiative is essential for the preservation and improvement of indigenous animal health care knowledge. As is noted by Martin et al. (2001, p. 6), some non-western knowledge medical traditions are as highly formalized as Western medicine while others have had the benefit of a writing system and/or a recognized profession of healer-husbandmen—as in Sri Lankans’ 400-year-old palm leaf records of veterinary treatments and their still existing cadre of traditional specialists.
The Luo livestock farmers in Nyang’oma oscillate between the three sectors and practitioners depending on various factors. Kleinman noted such alternation between the three sectors in human health care. This is in accordance with an earlier study among the Luo, where Sindiga (1995) noted the movement between various practitioners in case of human illnesses. The same has also been reported by Nyamwaya (1982) among the Pokot of Marakwet district and Nyamongo (1998) among the Abagusi in Kenya regarding human health.
When illnesses persist, the perceptions of causality can also shift and remedial action changed. An illness may first be perceived as “natural,” but as it persists the perceptions may change in such a way that it becomes linked to witchcraft. Magicians (jothieth) and religious practitioners will then be consulted to neutralize the effect of harmful magic (ndagla). However, these practitioners are consulted only when other treatment options have proved ineffective and the animal’s health continues to deteriorate or when several animals die within short intervals. These supernatural practices and perceptions have also been documented by Martin et al. (2001, p. 16) where they refer to them as medico-religious acts and note that from an “emic” (cultural insider’s) point of view these are just another part of veterinary treatment and good husbandry.
Among the Nyang’oma farmers such movements between different animal health providers are influenced by factors such as perceived causality, belief in the efficacy of alternative remedies, cost, perceptions of value and vulnerability of animals, availability of this service, the farmer’s social networks, relationship to the practitioner, and distance to a practitioner’s place as well as the characteristics of the owner.
The nature of the farming system also influences the kind of treatment given to animals. In the eyes of the community, grade and crossbred animals are more valued than the traditional animal variety. It is considered “modern” and “progressive” to own such animals instead of the indigenous types that are perceived to be of lower value. Cattle, goats, and sheep are more valued than poultry. Donkeys may be expensive to purchase but are still assigned the lowest value mainly because the Luo do not eat them but only use them as beasts of burden. This perception influences treatment where the more valued animals receive better attention than the less valued ones.
Some animals are also considered as better adapted to the tropical environmental conditions and are immune to sickness. Even if they get sick they may not receive immediate treatment because their body is capable of fighting illness and heal without any remedial action. Indigenous livestock and donkeys in particular are considered to have such immunity.
Ownership also influences treatment. Generally, it is the responsibility of the head of the homestead to ensure that animals in the home are kept healthy. Because the “big stock” animals (i.e. cattle, sheep, and goats) are mainly controlled by men, these animals tend to receive better health care. However, ownership was not so rigidly restricted and everybody can acquire and own any kind of animal except in some special circumstances. For example, a woman or child is not allowed to own a mating bull or cock if the head of the homestead (the man) is still alive.
Professionally trained veterinarians are few in Nyang’oma and this partly explains why farmers consult injection specialists and other traditional practitioners. Thus, distance is a key factor influencing choice of service and practitioner. Several livestock folk practitioners have neither the licenses, nor the training in the services they provide but are in high demand for animal health care services because they are more available. In addition, friendship and other kin based ties also influence relationships with these practitioners. Such observations have also been made by Mugunieri et al. (2003).
The belief in the efficacy of a given therapy is also an important factor. Farmers tend to rely on government personnel because they believe that the government has better infrastructure for prevention, detection, and management of animal illnesses. The high cost of treatment, however, often deters farmers from making these consultations. Government personnel are therefore not consulted first, because in addition to treatment costs they also charge for their transportation to and from the client, and this makes them expensive. It is convenient to consult private practitioners most of whom live in the community and only charge for treatment. Owing to the scarcity of trained veterinarians in Nyang’oma, several community-based animal health care dispensers have filled the gaps in veterinary health care services and charge lower fees which poor peasant farmers can afford. Usually farmers purchase drugs from veterinary shops and invite the injection specialists (jobilek) to come and inject the sick animal and negotiate the charges. According to Mathias (1996), EVM provides low-cost alternatives in situations where western-type drugs and veterinary services are not available or too expensive. The question of efficacy has been the subject of debate. Martin et al. (2001) note, for example, that mixing supernatural and natural approaches in health care is one of the major reasons for outsiders’ denigration of local health care systems. That scientists and developers are prone to view medico-religious beliefs as dangerous superstitions to be eradicated—even though these same scientists and developers may perceive no such contradictions when they themselves light votive candles in church, hold masses, and offer up prayers for ailing loved ones (Martin et al. 2001, pp. 16–17). Martin et al. (2001) emphasise the need for recognition and appreciation of ethnoveterinary health care techniques especially in resource poor communities where farmers may not have adequate access to commercially manufactured modern drugs and treatment procedures.
Nyang’oma farmers attach value to their animals and this influences their treatment decisions. Highly valued animals tend to receive prompt and better treatment while the less valued ones may be left to heal on their own. Milk cows and oxen for plough receive better attention than the other animals. Chicken is a delicacy and poultry will be slaughtered for a meal rather than let them lose weight due to an illness. Fielding (2002) also notes the cost factor in animal treatment when he says that if the cost of a treatment is a significant proportion of the value of the animal that is being treated then the animal may be left untreated or a low cost EVM may be used. This finding points to an important interesting consideration regarding cost-effectiveness. Animals are considered “disposable” as they can be slaughtered and eaten rather than heavily invested in for their health.
This study therefore has important implications for conventional veterinary services. First, it is important to know farmers’ perceptions and practices so that interventions can be adapted to their conceptual framework and the socio-cultural context in which they live and work (see also Schwabe and Makuet Kuojok 1981). It is also important to recognize that the western biomedical services provided to the farmers are often sought alongside many other treatment options and this has direct influence in the farmers’ resource allocation. The study points towards the bottom-up approach in animal health intervention programs. Understanding animal health dynamics at the community level is necessary for an intervention to be effective. Perceptions and practices concerning animal health differ from one community to another. However they are important in animal health and husbandry and therefore understanding and incorporating what is valid by interventionists is necessary to improve animal health, especially in rural poor households.
Overall, the study has shown that anthropological research on ethnoveterinary practices can provide an important basis for the planning, implementation, and evaluation of conventional, veterinary programs. Medical anthropology encourages the incorporation of indigenous perceptions and practices as well as structures in improving lifestyles of a people.
References
Cohen, D.W., and E.S.A. Odhiambo. 1989. Siaya. The historical anthropology of an African landscape. Nairobi: Heinemann Kenya.
Fielding, D. 2002. Ethnoveterinary medicine in the tropics – key issues and the way forward?. Edinburgh: Center for Tropical Veterinary Medicine, Royal (Dick) School of Veterinary Studies, University of Edinburgh.
Fabrega, H. 1982. A commentary on African systems of medicine. In African health and healing systems: Proceedings of a symposium, ed. P.S. Yoder, 237–252. Los Angeles: Crossroads Press.
Geissler, P.W., S.A. Harris, R.J. Prince, A. Olsen, R.A. Odhiambo, H. Oketch-Rabah, P.A. Madiega, A. Andersen, and P. Mølgaard. 2002. Medicinal plants used by Luo mothers and children in Bondo district, Kenya. Journal of Ethnopharmacology 83: 39–54.
Hauge, H.E. 1974. Luo religion and folklore. Oslo: Scandinavian University Books.
IIRR (International Institute of Rural Reconstruction). 1996. Ethnoveterinary medicine in Kenya. A field manual of traditional animal health care practices. Nairobi: International Institute of Rural Reconstruction.
ITDG (Intermediate Technology and Development Group). 2002a. Ethnoveterinary knowledge merges with community-based animal healthcare. http://practicalaction.org/?id = region_east_africa_kit_jun_03_animal_health. Accessed 17 May 2005.
ITDG (Intermediate Technology and Development Group). 2002b. Trials on EVK remedies get underway. http://practicalaction.org/?id = region_east_africa_kit_dec_02_4_vets. Accessed 23 May 2005.
ITDG (Intermediate Technology and Development Group). 2006. Rural Agriculture and Pastoralism Programme. http://practicalaction.org/?id = region_east_africa_rural_agriculture. Accessed 1 November 2007.
Janzen, J. 1978. The quest for therapy: Medical pluralism in lower Zaire. Berkeley: University of California Press.
Kleinman, A. 1980. Patients and healers in the context of culture. Berkeley: University of California Press.
Kokwaro, J.O., and J. Timothy. 1999. Luo biological dictionary. Nairobi: East African Educational Publishers.
Lawrence, E.A. 1996. I stand for my horse: Equine husbandry and health care among some North American Indians. In Ethnoveterinary research and development, ed. C.M. McCorkle, E. Mathias, and Schillhorn Van Veen, 116–120. London: Intermediate Technology and Development Group Publications.
Leslie, C. 1976. Introduction. In Asian medical system. A comparative study, ed. C. Leslie, 9. Berkeley: University of California Press.
Martin, M., and E. Mathias. 1999. Ethnoveterinary medicine as part of an integrated approach to animal health care. http://www.new-agri.co.uk/99-1/perspect.html. Accessed 23 May 2005.
Martin, M., E. Mathias, and M. McCorkle. 2001. Ethnoveterinary medicine. An annotated bibliography of community animal health care. London: Intermediate Technology and Development Group Publishing.
Mathias, E. 1996. How can ethnoveterinary knowledge be used in field projects? Indigenous Knowledge and Development Monitor 4 (2): 6–7.
Mathias, E., C.M. McCorkle, and Schillhorn Van Veen. 1996. Introduction: Ethnoveterinary research and development. In Ethnoveterinary research and development, ed. C.M. McCorkle, E. Mathias, and S. Van Veen, 1–23. London: Intermediate Technology and Development Group Publications.
Mugunieri, L., J. Omiti, and P. Irungu. 2003. Policy requirements to accommodate community-based animal health workers in Kenya. Institute of Policy Analysis and Research (IPAR): Nairobi. Policy Brief 9: 2.
Nyamanga, P.A., C. Suda, and J. Aagaard-Hansen. 2006a. Similarities between human and livestock illnesses among the Luo in Western Kenya. Anthropology and Medicine 13 (1): 13–24.
Nyamanga, P.A., C. Suda, and J. Aagaard-Hansen. 2006b. Ethnoveterinary perceptions of cattle illnesses in Western Kenya. Mila (N.S), The Journal of the Institute of African Studies 7: 1–7.
Nyamongo, I.K. 1998. Lay people’s response to illness: an ethnographic study of Anti-Malaria behavior among the Abagusi of southwestern Kenya. PhD dissertation, University of Florida.
Nyamwaya, D. 1982. The management of illness in an East African society: a study of choice and constraint in health care among the Pokot. PhD dissertation, Faculty of Archaeology and Anthropology, Cambridge.
Saimo, M.K., E.S. Bizimenyera, A. Bwanika, F. Ssebuguzi, G. Weny, and G.W. Lubega. 2003. Ethnoveterinary practices in Uganda: use of medicinal plants in treating helminthosis and coccidiosis in rural poultry and goats in Uganda. Bulletin of Animal Health and Production in Africa 51 (3): 133–138.
Schwabe, C.W., and I. Makuet Kuojok. 1981. Practices and beliefs of the traditional Dinka healer in relation to provision of modern medical and veterinary services for the southern Sudan. Human Organization 40 (3): 231–238.
Sindiga, I. 1995. Managing illness among the Luo. In Traditional medicine in Africa, ed. I. Sindiga, C. Nyaigotti-Chacha, and M.P. Kanunah, 64–79. Nairobi: East African Educational Publishers.
Acknowledgements
The authors are extremely grateful to the Institute of African studies, University of Nairobi for the co-operation and support given during the period of proposal development and data collection. We owe thanks to the DBL – Centre for Health Research and Development, University of Copenhagen for the financial support that made this work possible. Special thanks go to our informants, the custodians of the knowledge presented in this article and which they willfully provided so that this work could become a reality. The authors express their sincere gratitude to Nyang’oma Research Training Site (NRTS) for providing the field staff and logistical and practical support that were very instrumental in the success of the article. Last but not least we are very grateful to the editors of the journal as well as Dr. Constance McCorkle for extraordinary and constructive support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nyamanga, P.A., Suda, C. & Aagaard-Hansen, J. The socio-cultural context and practical implications of ethnoveterinary medical pluralism in western Kenya. Agric Hum Values 25, 513–527 (2008). https://doi.org/10.1007/s10460-008-9141-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10460-008-9141-1