Abstract
Self-regulated learning is essential for professional development and lifelong learning. As self-regulated learning has many inaccuracies, the need to support self-regulated learning has been recommended. Supervisors can provide such support. In a prior study trainees reported on the variation in received supervisor support. This study aims at exploring supervisors’ perspectives. The aim is to explore how supervisors experience self-regulated learning of postgraduate general practitioners (GP) trainees and their role in this, and what helps and hinders them in supervising. In a qualitative study using a phenomenological approach, we interviewed 20 supervisors of first- and third-year postgraduate GP trainees. Supervisors recognised trainee activity in self-regulated learning and adapted their coaching style to trainee needs, occasionally causing conflicting emotions. Supervisors’ beliefs regarding their role, trainees’ role and the usefulness of educational interventions influenced their support. Supervisors experienced a relation between patient safety, self-regulated learning and trainee capability to learn. Supervisor training was helpful to exchange experience and obtain advice. Supervisors found colleagues helpful in sharing supervision tasks or in calibrating judgments of trainees. Busy practice occasionally hindered the supervisory process. In conclusion, supervisors adapt their coaching to trainees’ self-regulated learning, sometimes causing conflicting emotions. Patient safety and entrustment are key aspects of the supervisory process. Supervisors’ beliefs about their role and trainees’ role influence their support. Supervisor training is important to increase awareness of these beliefs and the influence on their behaviour, and to improve the use of educational instruments. The results align with findings from other (medical) education, thereby illustrating its relevance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Self-regulated learning (SRL) is important to the professional development of medical trainees and their lifelong learning (Boekaerts 1997; Puustinen and Pulkkinen 2001; Regehr and Eva 2006; Sandars and Cleary 2011; Veloski et al. 2006; Zimmerman 2000). Before defining SRL we shortly describe perspectives from learning theories. Medical education has been influenced by cognitive as well as socio-cultural theories of learning (Mann 2011; Swanwick 2005; Taylor and Hamdy 2013). Cognitive learning perspectives focus on how learning takes place within a person, independently of its social context. Among others these perspectives contain experiential learning (Kolb 1984) and learning through reflection (Schön 1984). Socio-cultural learning perspectives explicitly involve the context and the community in learning. How individuals interact with their environment and how experience is shaped by context and community is described by situativity theories (Durning and Artino 2011). Important concepts are distributed cognition and affordances. Distributed cognition means that cognition in a context is distributed over actors, places, artefacts and time, and individuals depend on all of these elements to act effectively (Durning and Artino 2011; Hutchins and Klausen 1996; Pimmer et al. 2013). Affordances refer to the possibilities a workplace offers for individuals to participate and to learn from the workplace with its activities and interactions. Learning then also depends from individuals’ agency to use these affordances (Billett 2004; Durning and Artino 2011; Withagen et al. 2012). Lave and Wenger described how individuals learn by participating in communities of practice, and transit from legitimate peripheral participation to full participation (Lave and Wenger 1991; Wenger 2002).
The view on SRL depends on theoretical perspectives on learning. Cognitive views will focus on reflection on individual performance and learning, while socio-cultural views also will stress reflection on the social context as a whole and on opportunities the context offers for individual and collective learning. A well known definition of SRL comes from Zimmerman, who has defined self-regulated learning as ‘self-generated thoughts, feelings, and actions that are planned and cyclically adapted to the attainment of personal goals’ (Zimmerman 2000). Stemming from a socio-cognitive perspective self-regulation according to Zimmerman is viewed as an individual’s interaction of personal, behavioural and environmental processes (Artino and Jones 2013; Puustinen and Pulkkinen 2001; Sandars and Cleary 2011; Zimmerman 2000). The learner uses feedback from prior performance to make adjustments during current learning and performance. Zimmerman distinguishes three self-oriented feedback loops. Behavioural self-regulation refers to self-observing and adjusting performance, environmental self-regulation refers to observing and adjusting environmental conditions, and covert self-regulation refers to monitoring and adjusting cognitive and affective states. Self-regulation contains activities like goal setting, planning learning activities, regulating self-motivation, performing the task, monitoring the performance and self-assessing goal-attainment. So, Zimmerman refers to self-regulatory activities on cognitive and behavioural as well as environmental processes.
Clinical practice can be characterized as a community of practice with a variety of social relationships through which learning occurs (Wallenburg 2012; Wenger 2002). Simply by participating in this community of practice trainees will learn. However, self-regulation may promote deeper learning and understanding because it is a more conscious and deliberate process. Therefore, self-regulation may help medical trainees to adequately handle clinical questions and integrate new knowledge, skills and competences. However, they seem to use strategies that insufficiently enhance their learning (Bjork et al. 2013; Brydges et al. 2010). Trainees can regulate their cognition, motivation and behaviour to achieve their learning goals but tend to do this suboptimally (Bjork et al. 2013; Brydges et al. 2010). They also can identify and prioritise learning goals. However, these priorities can change in the face of time pressure (Brydges et al. 2010). Moreover, in maintaining a positive self-concept, they tend to avoid situations in which they might commit an error despite the positive consequences, such as obtaining feedback, the error would provide (Bjork et al. 2013; Brydges et al. 2010; Schumacher et al. 2013). Finally, self-assessment alone, as an essential part of SRL, is ineffective because learners tend to under- or overestimate their performance (Bjork et al. 2013; Davis et al. 2006; Eva and Regehr 2008; Gordon 1991; Hodges et al. 2001; Kramer et al. 2007; Kruger and Dunning 1999; Regehr and Eva 2006; Schumacher et al. 2013; Tracey et al. 1997). Because self-regulation is central to optimize the learning process, it is important to improve its role. The literature reveals that informed self-assessment, facilitated reflection and directed self-guided learning can support SRL (Brydges and Butler 2012; Brydges et al. 2010; Butler and Brydges 2013; Sargeant et al. 2008; Schumacher et al. 2013). Also, in postgraduate training supervisors can have a supportive role (Boendermaker et al. 2000; Brydges et al. 2010; Kilminster et al. 2007; Mann et al. 2001; Sagasser et al. 2012; Sandars and Cleary 2011; Sutkin et al. 2008; Wearne et al. 2012). Supervisors, who are experienced clinicians and trained in their supervisory tasks, can help identify trainee skill levels and set an appropriate level of challenge, occasionally in ways trainees would not attempt themselves. Additionally, they can aid by assisting, supervising or assessing the task to be mastered. To get a deeper understanding of how SRL works out in practice we performed a study into postgraduate trainees’ experience with self-regulated learning (Sagasser et al. 2012). Trainees reported that supervisors may encourage their self-regulated learning. However, we found that trainees’ learning was not visible to the supervisors in situations where the trainees did not involve them. Thus, in those cases, the supervisors could not support the trainees, and the learning of the trainees was subject to their own guidance. We also found that the trainees experienced variation in supervisor support. This reported variation in supervisor support raised questions on supervisor’s role in self-regulated learning. Therefore we are interested in how supervisors experience the self-regulated learning of trainees and their own role in that learning. This may contribute to adjusting the support by supervisors of the self-regulated learning of trainees. We wanted to explore how the supervisors experience the self-regulated learning of trainees and how they experience their supportive role. Our main questions were:
-
1.
What is supervisors’ experience with how trainees regulate their learning?
-
2.
How do supervisors experience their own role in supporting trainee self-regulated learning?
-
3.
What helps and hinders supervisors in supporting trainee self-regulated learning?
Methods
We designed a qualitative study using a phenomenological approach. We invited supervisors from a postgraduate training programme for general practitioners (GP) to participate.
Context
The study was performed on supervisors of the three-year postgraduate training programme for general practice in the Netherlands (Van Berkestijn 2002). Patient care in general practice is based on the principles of continuous, integrated and personal care (Van Weel et al. 2012). General practitioners act as gatekeeper and coordinate access to specialised care. As a consequence GP trainees are confronted with patients conveying a variety of symptoms and problems, ranging from acute to chronic and from singular to complex. During their training GP trainees provide patient care independently under clinical supervision of their supervisor. Postgraduate GP training has a long tradition of learning in the workplace under supervision of an experienced GP. Each of the eight University Medical Centres in the Netherlands offers GP training in their department of general practice/primary care. In years 1 and 3 of the programme, the trainees work in a general practice where they are coached and instructed by a single supervisor. Year 2 consists of rotating duty in hospitals, nursing homes and psychiatric outpatient clinics under different supervisors. During years 1 and 3, the trainees work 4 days a week in general practice. On the fifth day, they attend a day-release programme at the university’s training institute in groups of twelve to fifteen trainees facilitated by two mentors. Thus, GP training primarily consists of workplace-based learning aimed at connecting clinical experience with theoretical background. Reflection and feedback on experience, assessment and personal development are important aspects of GP training. Trainees are encouraged to write learning plans and reflections for inclusion in their learning portfolio. In the course of the training programme, trainees participate in several mandatory assessments. The communication skills are assessed from video-recorded consultations by the trainees (communication assessment). Knowledge in medical domains is assessed by multiple choice tests (progress knowledge test) (Van Leeuwen et al. 1997). Three progress meetings are held every year, in which trainees discuss their development with mentors and their supervisor using the Competency Assessment List (Compass) (Tromp et al. 2012). All of the supervisors are experienced GPs and provide clinical and educational supervision in the context of general practice. Supervisors attend a longitudinal training programme at the university’s training institute, which focuses on didactic and coaching skills, assessment and exchanging experience.
Design
Because our aim was to discover, describe and interpret the experience of the supervisors, we performed a qualitative study using a phenomenological approach (Creswell 1998; Dowling 2007; Giorgi 2006) based on a constructivist research paradigm (Bergman et al. 2012; Bunniss and Kelly 2010). Our phenomenological approach is known as new or American phenomenology because this allows for including interpretations and context (Dowling 2007). While traditional phenomenology seeks for a universal meaning of the experience, new phenomenology focuses on describing lived experiences of the participants and includes thoughts, interpretations and context related to the experiences in data-gathering and data-analysis. The analytic steps, like dividing into meaning units and constructing descriptions, are the same in both approaches of phenomenology. Reductionism is an important concept in phenomenology. In traditional phenomenology this refers to reducing an experience until a universal meaning appears. In new phenomenology reductionism refers to reducing an experience to the essence taking thoughts, interpretations and context into account. Traditional phenomenology is descriptive and the researcher sets aside all prejudgments by bracketing. However, as new phenomenology is rather interpretative, researchers need to critically review their potential influence on the data-gathering and data-analysis and adhere reflexivity.
The phenomenon under study is the experience of the supervisors with the process of self-regulated learning by GP trainees in clinical practice. Using stratified purposeful sampling, we selected our participants based on supervisor gender, and the gender and year of training (1 or 3) of their trainees (Gibson and Brown 2009; Miles and Huberman 1994). The inclusion criteria were that trainees should have started their training year for a minimum of 4 months ago. To make the findings applicable to similar training situations, supervisors from two universities (Nijmegen and Maastricht) were included. We conducted semi-structured interviews with individual supervisors (Gibson and Brown 2009). Written informed consent was obtained before the interview. Firstly, the supervisors described the characteristics of their practice. Next, the interviewer asked the supervisors to describe how their current trainee regulates her/his learning. The interviewer asked on the current trainee, because this referred to recent experience allowing for detailed description. The interviewer also encouraged the supervisors to reflect on differing supervisory experience with prior trainees. Then, the interviewer asked the supervisors to reflect on their support of self-regulated learning by introducing topics such as the role of learning goals, learning plans, observations, learning activities, debriefing patients, assessments and progress meetings. Furthermore, the supervisors were encouraged to reflect on hindering or helpful elements in supporting their trainees. To promote credibility we applied member checking by sending supervisors a summary of the interview for comments or corrections (Frambach et al. 2013; Tavakol and Sandars 2014). Supervisors received a gift coupon for their participation.
Our research team included one educationalist/PhD student (MS) and three experienced researchers and educators with differing backgrounds: two general practitioners (AK, CvW) and one psychologist (CvdV). During analysis, a research assistant (NE) was added to the research team.
Ethical approval
The study was approved by the Ethical Review Board of the Dutch Association for Medical Education (nr 172). Anonymity was guaranteed and participation was voluntary.
Data analysis
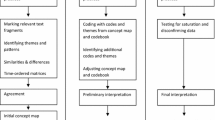
The interviews were audio-recorded and transcribed. The data were analysed in accordance with a phenomenological approach using the following steps: (1) reading for a sense of the whole, (2) dividing into meaning units, (3) transforming the data and (4) synthesising the transformed meaning units to generate a general description of the experience (Giorgi 2006). To integrate thematic codes derived from theory and the open codes derived from the data, we used template analysis (King 2004, 2012; King et al. 2002). The initial codebook was developed through reading and coding the first five transcripts (AK and MS). MS coded all of the transcripts. AK or NE also coded 13 transcripts. During this analytical process, MS took notes and used a logbook to document the coding and analysis. Reflexivity within the research team was practiced by critically questioning and discussing views of the researchers on data and analysis (Barry et al. 1999). Atlas-ti 6.2 software was used to organise the data.
Results
Twenty supervisors participated in the study: 12 male and 8 female. The average age was 51 years. The number of supervised trainees was 20 (9 first-year and 11 third-year trainees of whom 6 were male and 14 female). The practices of the supervisors were geographically spread out around the two universities in cities as well as larger and smaller villages. The number of GPs per practice varied. Most worked in group practices. A minority practiced in multidisciplinary health centres with physician assistants, physical therapists, pharmacists or psychologists. All of the practices had one or more physician assistants, who were responsible for protocolized chronic care (diabetics, COPD, CVD risk management, mental health care). Table 1 provides an overview of participants’ characteristics.
Between August 2012 and January 2013, one researcher (MS) conducted all of the interviews. The interviewer did not know the interviewees before the interviews. The average interview time was 59 min. The interviews were conducted at the practices of the supervisors. The order of the questions and the depth of the discussion depended on the input of the interviewees. Saturation was reached after 16 interviews. The remaining interviews were used to confirm the emergent topics. Regarding member checking, all but one supervisors responded to the invitation to check, and stated that they agreed with the summary presented. One supervisor did not respond to this invitation even after repeated requests. We present the results by describing what supervisors see from trainees’ self-regulated learning, what they do to support self-regulated learning, and what helpful and hindering elements they experience.
What do supervisors see from the self-regulated learning by trainees?
Trainee activity
The supervisors identified the trainees as active or passive self-regulating learners. Active learners actively identified learning goals and pursued relevant educational opportunities within or outside the practice, they involved their supervisors in their learning and made their progress visible in documents and coaching sessions. The supervisors described them as critically reviewing their activities and taking responsibility for their learning: “…How he directs his learning…that’s something he’s dealing with himself. Um, that’s what this trainee wants. He has very clear ideas about what he wants to learn and not wants to learn and is able to learn (…) and how he directs his learning? Um, by self-tuition (…) he is very active with his individual learning plan, so, formulating, adjusting, discussing, yeah, such a cycle, you know?” (Supervisor 8, female). By contrast passive learners had difficulty identifying learning goals, taking the initiative in learning activities, reflecting on experience and learning, structuring learning or making learning visible to others: “…not that he was not willing to learn, but to actually um, think like gosh, I should find it out, I should do this or um, studying guidelines and discuss these together, well yeah, one can think of 101 things to do (…) that yeah, that he needed some, needed…it did not happen all by itself.” (Supervisor 18, female).
Generally, all of the supervisors knew the learning goals of their trainees and could describe the learning activities trainees employed to attain these goals, such as studying, consulting their supervisor, following courses, preparing meetings or working with other healthcare workers within or outside the practice. The trainees acted on their own initiative and as a result of discussion with their supervisors. The trainees varied in the formulation of their learning goals, the documentation of their learning and their use of learning portfolios. This ranged from global to specific formulation and documentation, and from incidental to systematic use. The supervisors related personal features of the trainees to self-regulated learning, such as being hardworking, structured, a perfectionist, (in)secure, precise, timid or enthusiastic.
Patient safety, self-regulated learning and trainee capability to learn
The supervisors described a relation between patient safety, self-regulated learning and trainees’ capability to learn. From the beginning of the training year, the supervisors regularly used various ways to inform themselves on trainees’ medical knowledge, skills and competence. The supervisors were alert to their trainees’ way of coping with uncertainty and their lack of medical expertise from the viewpoint of patient safety: ‘Can I trust this trainee with my patients?’ In addition, the supervisors estimated how their trainees handled a lack of medical knowledge, formulated and prioritised learning questions, pursued learning and made their learning visible. These processes gave supervisors insight into trainees’ self-regulated learning skills as well as into trainees’ capability to acquire knowledge, skills and competences. Estimating trainee capability to learn and guarding patient safety were intertwined, particularly at the beginning of the year, as one supervisor stated: “I also notice that she needs to learn a lot about medical knowledge, but in general she doesn’t do unexpected things. She doesn’t act riskily.” (Supervisor 19, female). Experience with prior trainees who performed inadequately, stressed the need to safeguard patient safety, as this supervisor described: “I expected that a graduate can perform a pelvic exam. I was startled, so now I always think (…) I just want to know how, when you examine lungs or ears, in the beginning, yes, I just want to watch along.” (Supervisor 20, female). To judge their performance, the supervisors observed their trainees in the practice, during visits and out of office hours. When trainees debriefed their patients, the supervisors critically queried the professional performance of the trainees, mostly guided by the patient record system. In the beginning, most supervisors daily discussed all the patients of their trainees. The supervisors of first-year trainees discussed all the patients for a longer period of time than the supervisors of third-year trainees. Later on, the supervisors primarily discussed the patients whom the trainees wanted to discuss. When the trainees were entrusted to patients, the supervisors continued to inform themselves on trainees’ performance to a varying extent, also to detect potential misconceptions. Ways of this informing were randomly questioning trainees’ patient treatments, and observing and discussing skills and performance. Within this entire process, the supervisors were continuously alert if the trainees could identify alarming symptoms and avoided the risk of discharging a patient mistakenly. An important sign for adequate performance was whether the trainees consulted their supervisors when necessary (and when unnecessary).
What do supervisors do to support trainee self-regulated learning?
We found an adaptive process between supervisors and trainees. Firstly, we describe this adaptation and then present how the beliefs and experience of the supervisors accounted for variation between supervisors.
Adaptation to trainee needs
All of the supervisors were highly committed to trainee self-regulated learning. Generally, they adapted their supportive activities to trainee needs and used directive and non-directive coaching styles, taking trainee self-regulated learning activity and patient safety into account (see Fig. 1). Because most trainees directed their learning more or less actively, most supervisors employed a non-directive coaching style. This non-directive coaching style aimed to facilitate trainee learning by scheduling learning activities and coaching sessions, ‘thinking along with’ trainee learning (e.g. identifying learning goals that the trainees did not notice themselves or proposing learning activities) and estimating trainee progress. Non-directive coaching provided the trainees substantial liberty to regulate their learning: “This is a very accurate trainee who’s doing everything quite independently, actually. (…) You only incidentally need to ask her ‘did you do this, did you do that?” (Supervisor 2, male). Occasionally, supervisors had to direct their trainees to regulate their learning: “Sometimes you have to pull a bit, um, like “When will it come? When do I hear it?”, that there’s not much coming out of her independently in the beginning”. (Supervisor 6, female). However, few supervisors adopted a directive and controlling style because their trainees were unable to undertake self-regulated learning. Moreover, few supervisors had doubts about the professional development of their trainees. This directive style involved making strict appointments on learning goals, on learning activities and on the documentation of learning: “I’ve been a sergeant-major for a year, or at least for half a year, I’ve drilled.(…) At a certain point, I’ve let loose that self-directed learning” (Supervisor 3, female).
The supervision of trainees with strong, active self-regulating learning capacities was experienced as pleasant: “Yes, she is doing it quite transparently, I’ve never had someone like her. She’s doing great. (…) that’s the best trainee I’ve had up till now. So this is a treat to supervise”. (Supervisor 10, male). Supervising with a directive coaching style against one’s preference was experienced as a struggle: “Then, I really noticed I’m getting tired now, I’ve had it. It’s a bit like flogging a dead horse, well, not quite, because she is making enough progress, but I’m tired. I’m just too tired to continuously push and stimulate, so I find that very hindering, such an attitude, someone who’s that dependent”. (Supervisor 19, female).
All of the supervisors adjusted their supportive activities taking into account trainee’s competence, year of training, prior medical experience or interest in specific topics. When trainees were insecure or had difficulty to take responsibility, the supervisors adapted their supportive activities by frequently reassuring them in their development.
Beliefs and experience influencing adaptation
The supervisors described that beliefs and experience with respect to their role, the role of the trainees and the usefulness of learning activities and educational instruments influenced their supportive activities. As supervisors varied in their beliefs this accounted for variations between supervisors’ adaptation.
All of the supervisors found the trainees responsible for their own learning and expected them to actively direct their learning and to use learning opportunities. This belief made that some supervisors sometimes did not direct their trainee: “I, I put it, put it back to her a bit, like ‘listen, if you want that, you should negotiate with the medical receptionists. If you want that and indicate that, then the medical receptionists will do it. They really do their best’. But she (=the trainee) has to do that”. (Supervisor 16, male). However, other supervisors described situations in which they balanced their role with that of a trainee, by pushing a bit but not too much: “…but I just find that she should think of it, and what I sometimes do, I write in her schedule ‘mini-CEX for this (=patient)? That reminds her (…) and then sometimes it happens, but sometimes it doesn’t…” (Supervisor 4, female). While all of the supervisors found themselves responsible to well educate the trainee, some mentioned the reach of their responsibility: “So, on that point I think it’s not my responsibility as supervisor anymore. I deliver her as..I do my best. A few things really are not in order, the training institute knows this as well. I’ll hand her over to the training institute. I think from there they should…well, I don’t know how they take it up again, but that’s where my responsibility as supervisor ends, I think…” (Supervisor 19, female).
Supervisors to some extent varied in their beliefs on the usefulness of learning activities and educational instruments. All of the supervisors found it important to observe the trainees, to provide feedback, to assess and to discuss their progress. This belief influenced their supportive activities like organizing educational moments: “We have observations on Wednesday. First patient you fill in a mini-CEX, so in any case you have a fixed observational moment throughout the year”. (Supervisor 12, male) or providing in relevant patients “In the beginning, I find it important to visit elder, possibly chronic patients together, to get acquainted so the trainee can monitor these chronic patients further”. (Supervisor 12, male). However, some supervisors explained not to stimulate learning activities that they did not favour themselves, such as EBM-exercises: “She won’t do an EBM-exercise. We did it a few times, but we’re not enthusiastic about it (…) I don’t like it. I’m not so handy with computers (…) So, I don’t stimulate it”. (Supervisor 10, male) or extensively discussing medical guidelines: “Yes, so I…what I do is that I…I don’t hunt after topics…I don’t do that. I don’t like it that much. The content of it, I find…um…discussing guidelines not that interesting”. (Supervisor 11, male).
Likewise, supervisors’ belief on the usefulness of educational (assessment) instruments influenced the use. All of the supervisors valued the Competency Assessment List, a framework for assessing trainees’ professional development (Compass) (Tromp et al. 2012), because it facilitated reflection on specific moments and provided discussion opportunities: “…you fill it in every three months (…) all those aspects are described like ‘accounting for the context’, ‘being respectful to people’, that you think, OK, just give it a moment’s thought, do I have a good impression? What do I know about him? And how is he doing? Am I content about it?” (Supervisor 8, female). However, their opinions varied on the progress knowledge test (a multiple choice test on medical knowledge) (Van Leeuwen et al. 1997), the learning portfolio and the mini-CEX (an instrument to structure and document observations). While several supervisors found the mini-CEX highly useful: “…because I find it an attractive instrument just to discuss things practically and tangibly.” (Supervisor 10, male) others did not use it: “So, I do observe, but not with a whole list next to me (…) I think that I observe according to those steps, but I don’t write it down. (…) I just use it (=mini-CEX) when I cannot grasp the whole picture”. (Supervisor 14, male) or only used it because the training institute required it. Some supervisors mentioned they had to grow into their role as supervisor:”I find it difficult to use it (=assessment instrument) in the good way (…) of course it’s my unfamiliarity with the system, and I really have to learn it and use the assessment instrument in the good way”. (Supervisor 2, male).
The supervisors also mentioned that personal characteristics, such as (not) being structured, finding it difficult to delegate or not being the type who controls others, influenced their support.
Helpful and hindering elements for supporting self-regulated learning
All of the supervisors found their own training programme meaningful and helpful because of exchanging experience, practicing coaching and becoming inspired: “That (=supervisor training) is important. I can share things in the group and receive feedback, very important”. (Supervisor 11, male). Another supervisor stated: “It forces you to critically look at your own part, like a) knowing who I’m dealing with? b) how do I continue best?” (Supervisor 10, male). The supervisors received help from the training institute when they encountered difficulties in coaching. However, the training institute was hindering when new educational instruments were introduced into the curriculum because these did not always suit a busy practice.
The match with the trainee was an important helpful but occasionally hindering element. ‘Match’ refers to the match between the coaching style of the supervisor and the learning style of the trainee. Supervisors also mentioned the importance of feeling safe: “…to feel safe with one another. I with the trainee, but the trainee surely with me. (…) And one doesn’t have to be best friends, but one should, yes, feel safe with one another”. (Supervisor 8, female).
The context of the practice was another helpful but also hindering element. Due to busy practice and unforeseen incidents, trainees occasionally received less support than intended. A small practice organization sometimes hindered educational possibilities: “One can nicely discuss everything (…) but in this setting with two GPs you cannot work it around. In large practices with 8 GPs or group practices one can share tasks and help each other, that’s quite different”. (Supervisor 14, male). Colleague general practitioners were important for calibrating judgments about trainees and for sharing supervisory tasks: “We are a small team. You’re together the whole day, so you very quickly notice how the trainee is doing”. (Supervisor 20, female). Several supervisors found it helpful that their practices had a tradition of educating trainees and therefore had established routines in scheduling and performing supervisory activities.
Discussion
The supervisors adapted their support to the self-regulated learning activities of their trainees. When the trainees had a passive self-regulated learning style, the supervisors adopted a directive coaching style. In supporting the self-regulated learning of the trainees, the supervisors accounted for trainee needs. These needs could occur on the personnel, professional and educational levels (Boendermaker et al. 2000; Kilminster et al. 2007; Wearne et al. 2012). Our results indicate that supervisors adapt to trainee needs and that this adaptation evolves over time, depending on the professional development of the trainees. The literature describes this evolution as a scaffolding process during which supervisor support fades and trainee responsibility augments over time (Grow 1991; Ten Cate et al. 2004; Van de Pol et al. 2010). Within this adaptation process, tensions may exist between facilitating self-regulated learning and directing the learner (Boendermaker et al. 2000; De Kleijn 2013; Grow 1991; Kilminster et al. 2007; Wearne et al. 2012). Some supervisors in our study experienced these tensions, particularly when trainee activity and supervisor coaching style did not match. These trainees primarily had difficulties regulating their learning (Durning et al. 2011; Steinert 2013). The adaptation we found was influenced by the beliefs of the supervisors with respect to their role and the role of the trainees as well as supervisor beliefs regarding the usefulness of educational instruments or activities. Differing beliefs on roles and activities explained variations between supervisor and trainee pairs. It seems important for supervisors to be aware of their beliefs regarding their role because beliefs influence professional identity and behaviour (Korthagen 2004, 2009). Therefore, supervisor training is important because it stimulates reflection on the coaching experience and may contribute to becoming aware of one’s beliefs regarding one’s role, moreover it facilitates to practice alternative coaching behaviour. Similarly, supervisor training supports the use of educational instruments for trainees’ professional development.
Following Zimmerman’s socio-cognitive perspective self-regulated learning is viewed as an interaction of personal, behavioural and environmental processes. Learners adapt their self-regulated learning based on feedback from their own monitoring on personal, behavioural and environmental processes. However, when learners have poor self-regulated learning skills it is important that others help monitoring these processes. The adaptation process we found illustrates how supervisors monitor trainee self-regulated learning and estimate their supportive activities. These activities focus on personal processes (for example, by discussing motivation or personal learning goals), on behavioural processes (for example, by modeling ways of learning) or on environmental processes (for example, by creating or facilitating learning opportunities in practice). Learning opportunities in practice refer to the concept of affordances stemming from situativity theories. From a socio-cultural viewpoint the context will influence trainee’s self-regulated learning. For example, in this study supervisors mention practice characteristics as being helpful like a tradition of supervising or colleagues being part of the supervision process. By participating in practice trainees learn how learning is part of an organization and may adopt these way of learning. While in this study self-regulated learning was viewed from a socio-cognitive perspective, we also found the importance of the socio-cultural perspective on learning, with the supervisor as a connection between individual self-regulated learning and situated learning.
Patient safety, entrustment and estimating trainee capability to learn were key aspects in the supervisory process. The supervisors assessed trainee competence and capability to learn in multiple ways. At the beginning of the training year, they observed and queried the trainees, examined the patient records of the trainees, worked with the trainees and consulted colleagues to inform themselves on trainees’ medical expertise and professional performance. They developed an expert opinion on the performance of their trainees by gathering, interpreting and weighing information rather than using assessment instruments (Govaerts et al. 2007). In addition, they determined which responsibilities they could leave to the trainees. Thus, the supervisors seem to use global and internal criteria according to which they judge whether to entrust the trainees with patients or not (Sterkenburg et al. 2010). Entrustment is related to the concept of entrustable professional activities (EPAs). EPAs are tasks or responsibilities that can be entrusted to a trainee once sufficient, specific competence is reached to enable unsupervised execution (Ten Cate 2005; Ten Cate and Scheele 2007). EPAs are described using a specific format and facilitate purposeful training and assessment. In the postgraduate training context of this study, no EPAs are yet available. Supervisors entrust trainees according to their professional judgment and continue to varying extents to monitor learning and performance to detect potential misconceptions, thereby promoting patient safety (Sibbald et al. 2014; Zwart et al. 2011). Supervising trainees in practice who are entrusted with patients while ensuring patient safety is recognised as one of the supervisors’ tasks (Boendermaker et al. 2000; Hauer et al. 2014; Kennedy et al. 2007; Kilminster et al. 2007; Stolper et al. 2014; Wearne et al. 2012).
The present study was performed as the following step after a prior study. In the previous study, we interviewed GP trainees on their self-regulated learning (Sagasser et al. 2012). That study revealed a short and long loop of self-regulated learning. The short loop takes 1 week at most and is focused on problems that are easy to resolve and that require minor learning activities. The long loop is focused on complex or recurring problems that require multiple and planned longitudinal learning activities. Assessments and formal training affect the long but not the short loop. The trainees vary to the extent to which they consult their supervisors during the short loop. Therefore, the short loop learning seems to be not always apparent to others. The present study confirms that supervisors pay variable attention to the self-regulated learning of trainees during the short loop. Whereas some supervisors systematically discuss the short loop learning of trainees, others rely on the initiative of the trainee. Some supervisors have routines according to which they randomly question the patient treatments of their trainees. Others only discuss the patients whom the trainees wanted to discuss. So, the present study demonstrates that supervisors have more ways to monitor this short loop learning than the trainees described in the prior study. However, in view of the importance of monitoring trainee short loop learning to detect potential misconceptions, the variation between supervisors raises questions on how the quality of short loop learning generally is assessed. Some supervisors may improve the monitoring of trainee short loop learning. In addition, the present study confirms commitment of supervisors to the long loop of self-regulated learning. Self-regulated learning in the long loop involved learning goals that required longitudinal follow-up and was therefore frequently discussed.
A strength of this study is its qualitative phenomenological approach, which enabled the in-depth exploration of the individual experience of supervisors, providing rich and varied data. Another strength is the description of trainees as (more) active or (more) passive self-regulating learners, which may contribute to the field of self-regulated learning. Another strength is that this study extends our previous study, in which we explored self-regulated learning by trainees. Together, these studies describe the role of supervisors and trainees in the process of self-regulated learning and illustrate and clarify variations on this process. Despite the strength of the qualitative approach, there are also weaknesses. The postgraduate training programme in which we gathered our data has such specific educational features (i.e. trainees work 4 days a week guided by the same supervisor for a year and attend a day release training 1 day a week) that this may make it more difficult to transfer the findings to other contexts. However, the results we found on the adaptation process, beliefs of supervisors, patient safety and entrustment align with findings from other contexts in (medical) education. Another weakness is the voluntary participation of the supervisors. The participating supervisors may be more interested in self-regulated learning than other supervisors. A further weakness may be that we exclusively used interviews to gather data. In using interviews we relied on what supervisors told us they did, but we do not know whether they acted likewise in practice. The observation of actual practice may refine our views on how supervisors support self-regulation.
Conclusion
Supervisors adapt their coaching style to trainee self-regulated learning. This may result in conflicting emotions as the needed style does not fit the preferred style of the supervisor. Supervisors should be aware of their beliefs with respect to their role as these are strong predictors for behaviour. They also have to be alert to the self-regulated learning skills of their trainees. Discussing expectations about each party’s role in trainee learning at the beginning of the training contributes to the quality of supervision. Patient safety and entrustment are key aspects of the supervisory process. Some supervisors may improve the monitoring of self-regulated learning by trainees, especially in the short loop. Supervisor training is important to support supervisors in their role. The results we found on the adaptation process, the role of beliefs, patient safety and entrustment align with findings from other contexts in (medical) education, thereby illustrating its relevance for other contexts.
References
Artino, A. R, Jr, & Jones, K. D. (2013). AM last page: Self-regulated learning—a dynamic, cyclical perspective. Academic Medicine, 88(7), 1048.
Barry, C. A., Britten, N., Barber, N., Bradley, C., & Stevenson, F. (1999). Using reflexivity to optimize teamwork in qualitative research. Qualitative Health Research, 9(1), 26–44.
Bergman, E., de Feijter, J., Frambach, J., Godefrooij, M., Slootweg, I., Stalmeijer, R., et al. (2012). AM last page: A guide to research paradigms relevant to medical education. Academic Medicine, 87(4), 545.
Billett, S. (2004). Workplace participatory practices. Conceptualising workplaces as learning environments. Journal of Workplace Learning, 16(6), 312–324.
Bjork, R. A., Dunlosky, J., & Kornell, N. (2013). Self-regulated learning: Beliefs, techniques, and illusions. Annual Review of Psychology, 64, 417–444.
Boekaerts, M. (1997). Self-regulated learning: A new concept embraced by researchers, policy makers, educators, teachers, and students. Learning and Instruction, 7(2), 161–186.
Boendermaker, P. M., Schuling, J., Meyboom-De Jong, B. M., Zwierstra, R. P., & Metz, J. C. (2000). What are the characteristics of the competent general practitioner trainer? Family Practice, 17(6), 547–553.
Brydges, R., & Butler, D. (2012). A reflective analysis of medical education research on self-regulation in learning and practice. Medical Education, 46(1), 71–79.
Brydges, R., Dubrowski, A., & Regehr, G. (2010). A new concept of unsupervised learning: Directed self-guided learning in the health professions. Academic Medicine, 85(10 Suppl), S49–S55.
Bunniss, S., & Kelly, D. R. (2010). Research paradigms in medical education research. Medical Education, 44(4), 358–366.
Butler, D. L., & Brydges, R. (2013). Learning in the health professions: What does self-regulation have to do with it? Medical Education, 47(11), 1057–1059.
Creswell, J. W. (1998). Qualitative inquiry and research design. Choosing among five traditions. Thousend Oaks, London, New Delhi: SAGE Publications.
Davis, D. A., Mazmanian, P. E., Fordis, M., Van Harrison, R., Thorpe, K. E., & Perrier, L. (2006). Accuracy of physician self-assessment compared with observed measures of competence: A systematic review. JAMA, 296(9), 1094–1102.
De Kleijn, R.A.M. (2013). Master’s Theses Supervision: Feedback, interpersonal relationships and adaptivity. Dissertation, Utrecht University, Utrecht.
Dowling, M. (2007). From Husserl to van Manen. A review of different phenomenological approaches. International Journal of Nursing Studies, 44(1), 131–142.
Durning, S. J., & Artino, A. R. (2011). Situativity theory: A perspective on how participants and the environment can interact: AMEE Guide no. 52. Medical Teacher, 33(3), 188–199.
Durning, S. J., Cleary, T. J., Sandars, J., Hemmer, P., Kokotailo, P., & Artino, A. R. (2011). Perspective: Viewing “strugglers” through a different lens: How a self-regulated learning perspective can help medical educators with assessment and remediation. Academic Medicine, 86(4), 488–495.
Eva, K. W., & Regehr, G. (2008). “I’ll never play professional football” and other fallacies of self-assessment. The Journal of Continuing Education in the Health Professions, 28(1), 14–19.
Frambach, J. M., van der Vleuten, C. P., & Durning, S. J. (2013). AM last page. Quality criteria in qualitative and quantitative research. Academic Medicine, 88(4), 552.
Gibson, W., & Brown, A. (2009). Working with qualitative data. Los Angeles, CA: Sage.
Giorgi, B. (2006). Can an empirical psychology Be Drawn from Husserl’s phenomenology? In P. D. Ashworth & M. C. Chung (Eds.), Phenomenology and psychological science, historical and philosophical perspectives (pp. 69–88). New York: Springer Science + Business Media LLC.
Gordon, M. J. (1991). A review of the validity and accuracy of self-assessments in health professions training. Academic Medicine, 66(12), 762–769.
Govaerts, M. J., Van der Vleuten, C. P. M., Schuwirth, L. W., & Muijtjens, A. M. (2007). Broadening perspectives on clinical performance assessment: Rethinking the nature of in-training assessment. Advances in Health Sciences Education: Theory and Practice, 12(2), 239–260.
Grow, G. O. (1991). Teaching learners to be self-directed. Adult Education Quarterly, 41(3), 125–149.
Hauer, K. E., Ten Cate, O., Boscardin, C., Irby, D. M., Iobst, W., & O’Sullivan, P. S. (2014). Understanding trust as an essential element of trainee supervision and learning in the workplace. Advances in Health Sciences Education: Theory and Practice, 19(3), 435–456.
Hodges, B., Regehr, G., & Martin, D. (2001). Difficulties in recognizing one’s own incompetence: Novice physicians who are unskilled and unaware of it. Academic Medicine, 76(10 Suppl), S87–S89.
Hutchins, E., & Klausen, T. (1996). Distributed cognition in an airline cockpit. In Y. Engeström & D. Middleton (Eds.), Cognition and communication at work (pp. 15–34). New York, NY: Cambridge University Press.
Kennedy, T. J., Lingard, L., Baker, G. R., Kitchen, L., & Regehr, G. (2007). Clinical oversight: Conceptualizing the relationship between supervision and safety. Journal of General Internal Medicine, 22(8), 1080–1085.
Kilminster, S., Cottrell, D., Grant, J., & Jolly, B. (2007). AMEE Guide No. 27: Effective educational and clinical supervision. Medical Teacher, 29(1), 2–19.
King, N. (2004). Using templates in the thematic analysis of text. In C. Cassell & G. Symon (Eds.), Essential guide tot qualitative methods in organizational research (pp. 256–270). London: Sage.
King, N. (2012). Template Analysis Retrieved April 2012, August–December 2012, from http://hhs.hud.ac.uk/w2/research/template_analysis/.
King, N., Carroll, C., Newton, P., & Dornan, T. (2002). “You can’t cure it so you have to endure it”: The experience of adaptation to diabetic renal disease. Qualitative Health Research, 12(3), 329–346.
Kolb, D. A. (1984). Experiential learning. Experience as a source of learning and understanding. Englewood Cliff: Prentice Hall.
Korthagen, F. A. J. (2004). In search of the essence of a good teacher: Towards a more holistic approach in teacher education. Teaching and Teacher Education, 20(1), 77–97.
Korthagen, F. A. J. (2009). Professional learning from within. Studying Teacher Education, 5(2), 195–199.
Kramer, A. W., Zuithoff, P., Jansen, J. J., Tan, L. H., Grol, R. P., & Van der Vleuten, C. (2007). Growth of self-perceived clinical competence in postgraduate training for general practice and its relation to potentially influencing factors. Advances in Health Sciences Education: Theory and Practice, 12(2), 135–145.
Kruger, J., & Dunning, D. (1999). Unskilled and unaware of it: How difficulties in recognizing one’s own incompetence lead to inflated self-assessments. Journal of Personality and Social Psychology, 77(6), 1121–1134.
Lave, J., & Wenger, E. (1991). Situated learning: Legitimate peripheral participation. New York: Cambridge University Press.
Mann, K. V. (2011). Theoretical perspectives in medical education: Past experience and future possibilities. Medical Education, 45(1), 60–68.
Mann, K. V., Holmes, D. B., Hayes, V. M., Burge, F. I., & Viscount, P. W. (2001). Community family medicine teachers’ perceptions of their teaching role. Medical Education, 35(3), 278–285.
Miles, M. B., & Huberman, A. M. (1994). Qualitative data analysis: An expanded sourcebook (2nd ed.). Thousand Oakes, CA: SAGE Publications.
Pimmer, C., Pachler, N., & Genewein, U. (2013). Reframing clinical workplace learning using the theory of distributed cognition. Academic Medicine, 88(9), 1239–1245.
Puustinen, M., & Pulkkinen, L. (2001). Models of self-regulated learning: A review. Scandinavian Journal of Educational Research, 45(3), 269–286.
Regehr, G., & Eva, K. (2006). Self-assessment, self-direction, and the self-regulating professional. Clinical Orthopaedics and Related Research, 449, 34–38.
Sagasser, M. H., Kramer, A. W. M., & Van der Vleuten, C. P. M. (2012). How do postgraduate GP trainees regulate their learning and what helps and hinders them? A qualitative study. BMC Medical Education, 12, 67.
Sandars, J., & Cleary, T. J. (2011). Self-regulation theory: Applications to medical education: AMEE Guide No. 58. Medical Teacher, 33(11), 875–886.
Sargeant, J., Mann, K., Van der Vleuten, C., & Metsemakers, J. (2008). “Directed” self-assessment: Practice and feedback within a social context. The Journal of Continuing Education in the Health Professions, 28(1), 47–54.
Schön, D. A. (1984). The reflective practitioner. New York, NY: Basic Books.
Schumacher, D. J., Englander, R., & Carraccio, C. (2013). Developing the master learner: Applying learning theory to the learner, the teacher, and the learning environment. Academic Medicine, 88(11), 1635–1645.
Sibbald, M., De Bruin, A. B., & Van Merrienboer, J. J. (2014). Twelve tips on engaging learners in checking health care decisions. Medical Teacher, 36(2), 111–115.
Steinert, Y. (2013). The “problem” learner: Whose problem is it? AMEE Guide No. 76. Medical Teacher, 35(4), e1035–e1045.
Sterkenburg, A., Barach, P., Kalkman, C., Gielen, M., & Ten Cate, O. (2010). When do supervising physicians decide to entrust residents with unsupervised tasks? Academic Medicine, 85(9), 1408–1417.
Stolper, C. F., Van de Wiel, M. W., Hendriks, R. H., Van Royen, P., Van Bokhoven, M. A., Van der Weijden, T., & Dinant, G. J. (2014). How do gut feelings feature in tutorial dialogues on diagnostic reasoning in GP traineeship?. Advances in health sciences education: theory and practice. doi:10.1007/s10459-014-9543-3.
Sutkin, G., Wagner, E., Harris, I., & Schiffer, R. (2008). What makes a good clinical teacher in medicine? A review of the literature. Academic Medicine, 83(5), 452–466.
Swanwick, T. (2005). Informal learning in postgraduate medical education: From cognitivism to ‘culturism’. Medical Education, 39(8), 859–865.
Tavakol, M., & Sandars, J. (2014). Quantitative and qualitative methods in medical education research: AMEE Guide No 90: Part II. Medical Teacher 1–11. doi:10.3109/0142159X.2014.915297.
Taylor, D. C., & Hamdy, H. (2013). Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83. Medical Teacher, 35(11), e1561–e1572.
Ten Cate, O. (2005). Entrustability of professional activities and competency-based training. Medical Education, 39(12), 1176–1177.
Ten Cate, O., & Scheele, F. (2007). Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Academic Medicine, 82(6), 542–547.
Ten Cate, O., Snell, L., Mann, K., & Vermunt, J. (2004). Orienting teaching toward the learning process. Academic Medicine, 79(3), 219–228.
Tracey, J. M., Arroll, B., Richmond, D. E., & Barham, P. M. (1997). The validity of general practitioners’ self assessment of knowledge: Cross sectional study. BMJ, 315(7120), 1426–1428.
Tromp, F., Vernooij-Dassen, M., Grol, R., Kramer, A., & Bottema, B. (2012). Assessment of CanMEDS roles in postgraduate training: The validation of the Compass. Patient Education and Counseling, 89(1), 199–204.
Van Berkestijn, L. G. M. (2002). Learning to Learn. Curricular changes in the postgraduate training for general practitioners. [Leren leren. Over de vernieuwing van de huisartsopleiding.]. Huisarts en Wetenschap, 45(5), 248–252.
Van de Pol, J., Volman, M., & Beishuizen, J. (2010). Scaffolding in teacher-student interaction: A decade of research. Educational Psychology Review, 22(3), 271–296.
Van Leeuwen, Y. D., Dusman, H., Mol, S. S., Pollemans, M. C., Drop, M. J., Grol, R. P., et al. (1997). Factors influencing the growth in knowledge of trainees in general practice. Advances in Health Sciences Education: Theory and Practice, 2(1), 61–70.
Van Weel, C., Schers, H., & Timmermans, A. (2012). Health care in the Netherlands. Journal of the American Board of Family Medicine, 25(Suppl 1), S12–S17.
Veloski, J., Boex, J. R., Grasberger, M. J., Evans, A., & Wolfson, D. B. (2006). Systematic review of the literature on assessment, feedback and physicians’ clinical performance: BEME Guide No. 7. Medical Teacher, 28(2), 117–128.
Wallenburg, I. (2012). The modern doctor: Unraveling the practices of residency training reform. Amsterdam: University of Amsterdam.
Wearne, S., Dornan, T., Teunissen, P. W., & Skinner, T. (2012). General practitioners as supervisors in postgraduate clinical education: An integrative review. Medical Education, 46(12), 1161–1173.
Wenger, E. C. (2002). Cultivating communities of practice: A guide to managing knowledge. Boston, MA: Harvard Business School Press.
Withagen, R., de Poel, H. J., Araujo, D., & Pepping, G.-J. (2012). Affordances can invite behavior: Reconsidering the relationship between affordances and agency. New Ideas in Psychology, 30(2), 250–258.
Zimmerman, B. J. (2000). Attaining self-regulation: A social cognitive perspective. In M. Boekaerts, P. R. Pintrich, & M. Zeidner (Eds.), Handbook of self-regulation (pp. 13–39). San Diego, CA: Academic Press.
Zwart, D. L., Heddema, W. S., Vermeulen, M. I., Van Rensen, E. L., Verheij, T. J., & Kalkman, C. J. (2011). Lessons learnt from incidents reported by postgraduate trainees in Dutch general practice. A prospective cohort study. BMJ Quality and Safety, 20(10), 857–862.
Acknowledgments
We acknowledge the supervisors who participated in this study and shared their experiences of supporting self-regulated learning. We acknowledge Nadine Elstrodt (NE) for participating in the analysis and Elke Butterbrod for transcribing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sagasser, M.H., Kramer, A.W.M., van Weel, C. et al. GP supervisors’ experience in supporting self-regulated learning: a balancing act. Adv in Health Sci Educ 20, 727–744 (2015). https://doi.org/10.1007/s10459-014-9561-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-014-9561-1