Abstract
Vascularization of tissue-engineered constructs is essential to provide sufficient nutrient supply and hemostasis after implantation into target sites. Co-cultures of adipose-derived stem cells (ASC) with outgrowth endothelial cells (OEC) in fibrin gels were shown to provide an effective possibility to induce vasculogenesis in vitro. However, the mechanisms of the interaction between these two cell types remain unclear so far. The aim of this study was to evaluate differences of direct and indirect stimulation of ASC-induced vasculogenesis, the influence of ASC on network stabilization and molecular mechanisms involved in vascular structure formation. Endothelial cells (EC) were embedded in fibrin gels either containing non-coated or ASC-coated microcarrier beads as well as ASC alone. Moreover, EC-seeded constructs incubated with ASC-conditioned medium were used in addition to constructs with ASC seeded on top. Vascular network formation was visualized by green fluorescent protein expressing cells or immunostaining for CD31 and quantified. RT-qPCR of cells derived from co-cultures in fibrin was performed to evaluate changes in the expression of EC marker genes during the first week of culture. Moreover, angiogenesis-related protein levels were measured by performing angiogenesis proteome profiler arrays. The results demonstrate that proximity of endothelial cells and ASC is required for network formation and ASC stabilize EC networks by developing pericyte characteristics. We further showed that ASC induce controlled vessel growth by secreting pro-angiogenic and regulatory proteins. This study reveals angiogenic protein profiles involved in EC/ASC interactions in fibrin matrices and confirms the usability of OEC/ASC co-cultures for autologous vascular tissue engineering.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tissue-engineered constructs and organs require vascular structures to ensure efficient oxygen and nutrient supply and hemostasis. In particular, tissues exceeding a thickness of a few millimeters cannot survive without any blood and lymphatic vessels after implantation in vivo [1]. Therefore, different approaches for vascularization of engineered constructs have been developed. Since research on angiogenic mechanisms during the last decades provides fundamental knowledge about pro- and anti-angiogenic growth factors and cytokines, several models deal with the controlled release of endothelial cell (EC) recruiting and angiogenesis inducing factors through bioengineered matrices [2–6]. Hence, the need for in vitro prevascularized scaffolds which remain stable, anastomose with the host vessels and maintain blood perfusion became necessary [7]. Recent studies have shown that co-cultures of EC together with, e.g., primary osteoblasts [8] or fibroblasts [9–11] lead to sprouting and the formation of vascular structures in vitro. In particular, co-culturing EC with smooth muscle cells [11, 12] and mesenchymal stem cells gained interest, as these cell types express angiogenic factors [13–16] and are able to develop pericyte characteristics [15, 17]. We showed before that adipose-derived mesenchymal stem cells (ASC) induce outgrowth endothelial cells (OEC) vasculogenesis in fibrin gels. ASC can be easily obtained from liposuction material and thus provide the possibility of using waste products for autologous prevascularization approaches in co-cultures with OEC [18]. Endothelial progenitor cells (EPC) or OEC from peripheral or umbilical vein blood are frequently used for prevascularization models since they provide the possibility of creating an autologous transplantation to the patient [19]. In addition, also the vasculogenesis of endothelial cells from other sources like human umbilical vein endothelial cells (HUVEC) was shown to be induced by ASC [20, 21].
The extracellular matrix is a major key factor determining 3D network formation in HUVEC/ASC co-cultures [22]. We decided to use fibrin as scaffold material since it provides cell adhesion molecules [23] and the possibility of changing stiffness parameters by varying the components thrombin, fibrinogen and factor XIII [24, 25].
Although different angiogenic growth factors and cytokines secreted by mesenchymal stem cells have been identified so far, it remained unclear which molecular mechanisms determine the interaction between OEC and ASC in fibrin co-cultures. We compared direct and indirect ASC-induced OEC and HUVEC vascular network formation in fibrin gels over a time period of 4 weeks in vitro. Here, we give evidence for the mechanisms involved in ASC-induced vasculogenesis in vitro.
Materials and methods
Cell isolation
OEC were isolated from healthy donors with authorization of a local ethics committee according to the protocol described elsewhere [18, 19]. Briefly, 30 ml peripheral blood was diluted with phosphate buffer saline (PBS, Lonza, Basel, Switzerland) and separated by centrifugation with lymphocyte separation medium (LSM 1077, GE Life Sciences, Chalfont St Giles, UK). Peripheral blood mononuclear cells (PBMC) were seeded to a collagen I/III-coated 48-well plate with a seeding density of 1.5 × 105 cells per well in endothelial growth medium (EGM-2) (Lonza, Basel, Switzerland). Medium change was performed every second day, and first colonies were obtained after 3–4 weeks of cultivation and characterized by flow cytometry according to Holnthoner et al. [18]. OEC were used between passages 4 and 6. Lentivirally transduced GFP HUVEC were purchased from Olaf pharmaceuticals (Worcester, USA) and used between passages 5–7. Flasks and plates were coated with 2 µg/ml fibronectin (Sigma-Aldrich, St. Louis, USA) for endothelial cell culture. ASC were isolated from liposuction material as described before [26]. HUVEC were either purchased (C2519A, Lonza, Basel, Switzerland) or isolated as previously described [27].
ASC coating of Cytodex-3 microcarrier beads
ASC were enzymatically detached with trypsin (Sigma-Aldrich, St. Louis, USA), centrifuged at 100xg for 5 min and seeded to autoclaved, PBS-washed Cytodex-3 microcarrier beads (GE Life Sciences, Chalfont St Giles, UK) with a cell density of approximately 400 cells per bead in a T25 cell culture flask. The flask was incubated at 37 °C and shaken gently every 20 min for 3 h in 3 ml EGM-2.
Co-culture of ASC and endothelial cells in 3D fibrin matrices
The conditions for the co-cultures used were EC only, EC with ASC-conditioned supernatant (termed “EC/ASC SN” throughout the manuscript), EC with non-coated Cytodex-3 beads, EC with ASC-coated Cytodex-3 beads, EC and ASC seeded into the clot (EC/ASC) and EC seeded into the clot with ASC on top of the clot. Fibrin gel components (Baxter, Vienna, Austria) were prepared by warming fibrinogen to room temperature and diluting 4 U/ml thrombin 1:10 in calcium chloride (CaCl2). Round coverslips with a diameter of 15 mm were put into a 12-well plate. Cells, fibrinogen and thrombin (0.2 U/ml) were mixed to fibrin gels (2.5 mg/ml final concentration) containing 100,000 endothelial cells and, depending on the condition, either 100 non-coated or ASC-coated Cytodex-3 beads or 100,000 ASC and pipetted onto the prepared coverslips. Gels were polymerized at 37 °C for 30 min. Seeding of ASC on top of the clot was performed after solidification of the clot matrix (100,000 ASC/well).
Generation of ASC-conditioned medium
ASC (confluency between 70 and 80 %) were cultured in full EGM-2 with 5 % FCS. The supernatants were taken after 48 h, centrifuged at 100xg to remove cells and directly transferred to the prepared fibrin clots with 100 KIU/ml aprotinin (Baxter, Vienna, Austria). Medium change, both for ASC and the conditioned fibrin clots, was performed 2–3 times per week.
Fixation, staining and quantification of endothelial networks in fibrin gels
Gel fixation was carried out by overnight incubation with 4 % paraformaldehyde (PFA) on ice while shaking. For visualization of OEC networks, the clots were washed three times with PBS and stained with fluorescein isothiocyanate (FITC)-conjugated monoclonal mouse anti-human CD31 antibody (BD Biosciences, Franklin Lakes, USA). ASC showing pericyte characteristics were stained with phycoerythrin (PE)-conjugated monoclonal mouse anti-human neural/glial antigen 2 (NG-2) antibody (both 1:100 dilution in PBS/1 % BSA) (R&D systems, Minneapolis, USA) for 10 h on ice while shaking. Gels were again washed with PBS for 5 min, and images were taken on a Leica DMI6000B epifluorescence microscope (Leica, Solms, Germany). Quantification of tube formation was performed with Adobe Photoshop CS5 (Adobe Systems, San José, USA) and AngioSys software (TCS Cellworks, London, UK) as described elsewhere [18].
RT-qPCR
HUVEC were co-cultured with ASC in fibrin matrices (2.5 mg/ml final concentration) for one week, and RNA was isolated after 1 and 7 days of culture. Fibrin clots were washed with PBS, cut into small pieces and incubated with 50 fibrinolytic units (FU) per ml nattokinase (Japan Bioscience Laboratories, Osaka, Japan) for 30 min at 37 °C similar to the protocol described before [29]. The cells were then centrifuged at 300×g for 5 min, and RNA isolation was performed with a GenElute™ mammalian total RNA miniprep kit (Sigma-Aldrich, St. Louis, USA) according to the manufacturer’s protocol. Reverse transcription was conducted with a DyNAmO cDNA synthesis kit (Thermo Scientific, Waltham, USA). RT-qPCR was performed on a MX3005P Stratagene system (Agilent Technologies, Santa Clara, USA) with standard enzyme and cycling conditions using 250 ng cDNA for each reaction in triplicates for each target gene. Taqman® probes for glyceraldehyde 3-phosphate dehydrogenase (GAPDH), CD31, von Willebrand factor (vWF), tyrosine kinase with immunoglobulin-like and epidermal growth factor-like domains 2 (Tie-2), platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), VEGF receptor 2 (VEGFR2) and vascular endothelial cadherin (VE-cadherin) were purchased from Microsynth (Balgach, Switzerland).
Angiogenesis protein array
Fibrin gels (2.5 mg/ml final concentration) with a total volume of 200 µl were seeded with 200,000 cells per cell type (ASC and OEC) and cultivated in either EGM-2 or supernatant from ASC in the same passage as used for clot seeding. After 4 days of cultivation, supernatants were collected and centrifuged at 100×g to remove cells. The measurement of angiogenesis-related proteins in the supernatants was done with an angiogenesis proteome profiler array kit (R&D systems, Minneapolis, USA) according to the manufacturer’s protocol. Signals were detected by enhanced chemiluminescence and recorded on film. Membranes were exposed for different exposure times to ensure that the signals are in the linear range (see supplementary Figs. 4-6). Signals were densitometrically quantified with ImageJ (NIH, Bethesda, Maryland). The density values for all detected proteins were beheld at the 3 different exposure times used. Exposure times where conditions showed the highest differences in protein expression between each other were considered for final quantifications.
Statistics
Statistical evaluations were performed with GraphPad Prism 4 software (GraphPad, San Diego, USA). All figures show the mean values with their respective standard error of means (SEM). OEC/ASC fibrin co-cultures over 4 weeks were performed with OEC and ASC each isolated from 3 donors. GFP HUVEC derived from 1 single donor were co-cultured with ASC from 3 different sources. For the quantification with Angiosys software, 4 images per condition were taken at each time point. HUVEC used for RT-qPCR analysis originated from 2 donors, either isolated from one single donor or purchased from Lonza (pooled) and were used in combination with ASC from 2 different donors.
Results
ASC induce stable vasculogenesis in 3D fibrin matrices
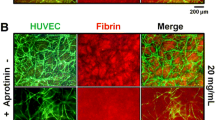
To observe in vitro vasculogenesis over a time period of 4 weeks, HUVEC and OEC were co-cultured with ASC in fibrin clots. ASC induced vasculogenesis of HUVEC via direct and indirect stimulation (Fig. 1). In contrast, endothelial cells seeded into fibrin constructs in the absence of ASC did not show tube formation at all. EC in the EC/ASC SN condition started to develop tube-like morphology after 1 week but were unable to form a mature network. Endothelial cells cultured with Cytodex-3 beads tended to migrate near the beads, but were not induced to form sprouts and networks. Moreover, endothelial cells incorporated into clots with ASC-coated Cytodex-3 beads form vascular structures in the vicinity of these beads. These networks remained stable for approximately 14 days but disintegrated after 2–3 weeks. However, no network formation was visible in regions lacking ASC-coated beads. Importantly, when ASC were seeded into the fibrin constructs together with the EC, intensely branched networks formed after 7 days. After 3 weeks of culture, these structures started to disintegrate with only few cross-linked branches remaining 4 weeks after seeding. In contrast, ASC seeded on top and around an EC-containing fibrin clot needed about 14 days to induce vasculogenesis. Furthermore, these networks remained stable and did not degrade until the fourth week of incubation.
HUVEC/ASC co-cultures in 2.5 mg/ml fibrin matrices over 4 weeks. HUVEC were incubated either without ASC, with ASC supernatant or non-coated Cytodex-3 beads where they do not show mature network formation. Incubation with ASC-coated Cytodex-3 beads, ASC seeded into and on top of the clot show network formation. Networks induced by ASC coated on beads and ASC in the fibrin matrix degraded after 2 weeks of culture
To quantify network formation, images of HUVEC and OEC networks induced by EC/ASC SN, EC/ASC seeding into the fibrin clot and ASC seeding on top of the clot were taken every week. While ASC supernatants promoted a minimal number of junctions and tubules, which reached the highest amount in the second week and degenerated afterward, the direct seeding of ASC together with HUVEC induced stable, mature network formation after seven days (Fig. 2a). However, the number of junctions and tubules started to decrease between the first and the second week and was reduced by 75 % after four weeks. ASC seeded on top of HUVEC-containing fibrin clots needed approximately 14 days to induce a mature network formation. Although the amount of junctions and tubules in this condition decreased after the second week, the disintegration was not as severe as in ASC/HUVEC co-cultures when both cell types were seeded into the fibrin gels. ASC supernatants were shown to stimulate HUVEC tubule formation which resulted in a high mean and total tubule length at the beginning. Due to the low amount of junctions and tubules, the total tubule length decreased, whereas the mean length increased after the first week of incubation. As soon as the networks mediated by ASC/HUVEC (both seeded into the clot) started to disintegrate, the total tubule length decreased while the mean length of the tubes slightly increased. Both the total and mean length of tubules remained stable after 14 days of culture when ASC were seeded on top of the EC-containing fibrin gel.
Quantification of network formation in HUVEC/ASC and OEC/ASC 3D co-cultures. a ASC supernatants are not sufficient to induce stable HUVEC network formation. Networks formed by HUVEC start to degrade after 1 week of culture, whereas vascular structures stimulated by ASC seeded on top of the fibrin clot remain stable for several weeks. The total tubule length decreases, whereas the mean tubule length increases. b OEC form similar networks either with ASC in the clot or on top of the clot after 1 week. In contrast to ASC/OEC co-cultures (both cell types seeded into the clot), ASC seeded on top of the clot induce further network growth. While total tubule lengths slightly decrease, the mean tubule lengths show a rise after 3 weeks. 3 ASC and OEC and 1 GFP HUVEC donor were used. Data shown as mean ± SEM
To evaluate the usability of the co-culture system for an autologous setup, OEC were used instead of HUVEC (Fig. 2b). Again, ASC supernatants were not sufficient to induce a stable network formation as the amount of junctions and tubules remained low over the whole incubation period. Furthermore, the length of tubules did not change. In contrast to HUVEC, OEC formed stable, mature networks when ASC were situated on top of the clot and exhibited the same amount of junctions and tubules as OEC/ASC co-cultures after one week. Whereas the number of junctions and tubules decreased in the OEC/ASC seeded clots, there was an increase of network formation when ASC were located on top of the clots. However, both conditions showed approximately 30 % degradation between the third and the fourth week. The total length of tubules reflects the network growth and disintegration as the length slightly decreased in OEC/ASC co-cultures but increased when ASC were not seeded directly into the clot. In both conditions, the mean tubule length increased to approximately the same level after four weeks.
ASC stabilize endothelial networks by developing pericyte characteristics
To determine whether ASC contribute to network stabilization and whether they become pericyte-like cells, we stained the vascular networks with an anti-NG-2 antibody (Fig. 3). HUVEC did not express NG-2 when cultured without ASC. After 4 weeks of incubation, in conditions where ASC were either seeded into or on top of EC-containing fibrin clots, we detected NG-2-positive ASC. However, just parts of the vascular network were surrounded by these pericyte-like ASC especially in regions of bifurcations.
Expression of EC-related marker genes in EC/ASC co-cultures changes over time
In order to compare the expression levels of EC-related marker genes between day 1 and day 7 after seeding, mRNA of HUVEC and ASC cultured in fibrin clots was subjected to RT-qPCR analysis (Fig. 4). Whereas PDGF and Tie-2 expression remained stable, CD31, VE-cadherin, VEGFR-2 and vWF levels were upregulated in co-cultures. Furthermore, we analyzed HUVEC mono-culture gene expression and observed stable expression between day 1 and day 7 except vWF which is twofold upregulated after one week (supplementary Fig 2).
Expression of EC marker genes changes of HUVEC/ASC co-cultures in fibrin matrices between day 1 and day 7. Co-cultures showed an increase of CD31, VE-cadherin, VEGFR2 and vWF levels, whereas PDGF and Tie-2 did not change over time. VEGF expression was slightly reduced after 1 week of culture. Two different ASC and HUVEC donors were used. Data shown as mean ± SEM
Expression of angiogenesis-related proteins in OEC/ASC co-cultures differs from monocultures in 3D fibrin matrices
To elucidate which molecular mechanisms are involved in ASC-induced vasculogenesis of EC in fibrin gels, supernatants of mono- and co-cultures were collected after 4 days of incubation and protein expression was analyzed. We used this time point for harvesting the supernatants because after 4 days, EC tube formation is already visible. All figures covering the results of the performed protein array show expression levels with more than twofold change. The complete data are summarized in supplementary Figs 4-6.
ASC in a fibrin monoculture have distinct higher expression levels of different angiogenesis-related proteins in comparison with OEC monoculture (Fig. 5a). Beside VEGF, fibroblast growth factors 4 and 7 (FGF-4 and FGF-7), epidermal growth factor family proteins amphiregulin and heparin-binding epidermal growth factor (HB-EGF), insulin-like growth factor-binding proteins 2 and 3 (IGFBP-2 and IGFBP-3), glial cell line-derived neurotrophic factor (GDNF), hepatocyte growth factor (HGF), angiogenin, angiopoietin-1 (Ang-1), matrix metalloproteinase 9 (MMP-9) and dipeptidyl peptidase IV (DPPIV), interleukin 1 beta (IL-1b) and monocyte chemoattractant protein 1 (MCP-1) were expressed. Furthermore, serpin F1, platelet factor 4, tissue inhibitor of metalloproteinase 4 (TIMP-4) and thrombospondin-1 were higher secreted by ASC than OEC. Of all these mentioned proteins, the basal secretion of MCP-1 and HB-EGF was high for both cell types, whereas VEGF was strongly secreted by ASC but not by OEC.
Protein expression of angiogenesis-related proteins in OEC, ASC and OEC/ASC co-cultures. a Several pro- and anti-angiogenic/regulatory proteins were more than twofold upregulated in ASC compared to OEC. b Differences of protein expressions comparing OEC/ASC co-cultures with OEC incubated in ASC-conditioned medium showed an upregulation of FGF-2, Angiopoietin-2, Pentraxin-3, PD-ECGF and MMP-9
OEC/ASC co-cultures show differences in protein expression compared to OEC/ASC SN (Fig. 5b). The secretion of platelet-derived endothelial cell growth factor (PD-ECGF), FGF-2 and MMP-9 was more than twofold upregulated in the presence of ASC in the clot compared to EC/ASC SN. Moreover, angiopoietin-2 (Ang-2) as a regulator of angiogenesis during vascular remodeling and pentraxin-3, an FGF-2 antagonist [28], were higher secreted in the OEC/ASC co-culture condition compared to OEC/ASC SN.
The protein secretions of ASC versus OEC/ASC SN showed various similarities (Fig. 6). Almost all factors upregulated in ASC monoculture compared to OEC alone were also upregulated in cultures with both cell types and OEC/ASC SN except FGF-4 and IL-1β. Other proteins upregulated by OEC/ASC co-culture and ASC SN were placental growth factor (PIGF), leptin, latency-associated peptide (LAP), VEGF-C, IL-8, CD105, artemin, granulocyte–macrophage colony-stimulating factor (GM-CSF), endocrine gland-derived VEGF (EG-VEGF), FGF-1 and persephin. Furthermore, thrombospondin-2, angiostatin, endostatin/collagen XVIII, angiopoietin-2, tissue factor, activin A, and prolactin were upregulated by ASC influence compared to OEC in monoculture. Urokinase, neuregulin 1 beta 1 (NRG1-β1) and a disintegrin and metalloproteinase with thrombospondin motifs-1 (ADAMTS-1) were strongly upregulated by OEC cultured in ASC supernatant, but not in co-cultures of ASC with OEC in the clot. However, EGF is the only protein which was more than twofold upregulated in OEC/ASC co-cultures but not in the OEC/ASC SN condition.
Comparison of protein expression levels of OEC with direct and indirect ASC stimulation. a Co-cultures of ASC with OEC induce much higher expression of pro-angiogenic and regulatory proteins compared to OEC alone. b Upregulation of OEC protein expression via ASC supernatants showed similarities to a
When comparing an ASC monoculture with ASC/OEC co-cultures or OEC/ASC SN, it appeared that several angiogenesis regulators such as CD105, PIGF, tissue factor, angiostatin, angiopoietin-1 and TIMP-4 were upregulated through OEC involvement (Fig. 7). Furthermore, IGFPB-1, platelet-derived growth factor AA, AB and BB (PDGF-AA, PDGF-AB, PDGF-BB), endothelin-1 and macrophage inflammatory protein 1a (MIP-1a) were strongly upregulated via OEC involvement compared to ASC monoculture.
Influences of OEC involvement in OEC/ASC co-cultures and indirect stimulation via ASC supernatants compared to ASC. a The highest differences were shown for Angiopoietin-2, PIGF, IGFBP-1, Tissue Factor, PDGF-AA and CD105. b Expression level changes mediated by OEC mainly affected the same proteins as shown in (a)
Discussion
The current study adds evidence to the molecular mechanisms involved in ASC-induced vasculogenesis in fibrin in vitro. Our data show the necessity of close physical interaction between EC and ASC and describe angiogenesis-related proteins involved in these interactions. So far, it has been shown that OEC form vessel-like structures with ASC in fibrin gels, whereas the inducibility of HUVEC network formation by ASC remained controversial [13, 18].
Here, we investigated whether direct EC/ASC contact is necessary for tube formation or whether supernatants from ASC provide sufficient angiogenic factors to induce the formation of a mature vascular network. We used a final fibrin concentration of 2.5 mg/ml as it was shown before that this concentration is the most suitable for capillary network formation [28]. Supernatants induced HUVEC and OEC to form long-shaped structures, but no branched networks were found. This result indicates that direct contact or proximity of ASC with EC is necessary for tube formation. By capturing ASC to specific sites of the fibrin matrix via seeding them on microcarrier beads, we were able to prove our assumption since the EC started to form networks only near the ASC-coated beads. Furthermore, ASC seeded on top of EC containing fibrin clots were able to induce vasculogenesis which was also shown before using bone marrow-derived mesenchymal stem cells [29]. However, the tube formation in this setup took longer compared to conditions were both cell types were seeded together into the clot.
In order to follow up network integrity over a longer period of time, we maintained co-cultures of ASC with HUVEC or OEC for 4 weeks. Interestingly, OEC vasculogenesis induced by ASC seeded on top of the clot differed from HUVEC network formation in this condition as OEC were able to form a mature network earlier than HUVEC. This result indicates that OEC may not need as much proximity to ASC as HUVEC to form networks as they may be more sensitive to secreted factors. Nevertheless, for both endothelial cell types, networks mediated by direct seeding of ASC together with EC started to degrade between the first and second week of culture, whereas indirect ASC seeding resulted in further tubule formation (OEC) or a consistent amount of junctions and tubules (HUVEC). Interestingly, ASC and OEC obtained from different donors showed differences in tube formation. Whereas the use of ASC with relatively low differentiation potential resulted in loose networks with few junctions (supplementary Fig 1a), ASC showing more staining for adipogenic and osteogenic differentiation induced denser vascular structure formation (supplementary Fig 1b). These influences of donor variability in angiogenic factor release were described before [30]. Interestingly, this donor variability could not be seen when HUVEC from different sources were analyzed for their expression of endothelial-related marker genes (supplementary Fig 2). Moreover, network morphologies looked different depending on the location of ASC right after seeding and the OEC donor variability (data not shown). We performed NG-2 staining to evaluate whether ASC develop pericyte character and contribute to network stability. Our data demonstrate that NG-2-positive ASC surround the vessels mostly in regions of bifurcation presence which has been shown before in another study [31].
RT-qPCR of HUVEC/ASC co-cultures derived from fibrin clots revealed a rise in gene expression levels of angiogenesis-related genes encoding for CD31 and VE-cadherin after 1 week. This increase can be explained by the fact that cells forming networks need to attach to each other via cellular adhesion molecules like CD31 [32] and VE-cadherin [33]. In addition, it was shown before that HUVEC seeded in fibrin gels were unable to develop tube-like structures when an anti-VE-cadherin antibody was incorporated in the gel [33]. Furthermore, VEGFR2 as a receptor for VEGF and therefore a prerequisite for angiogenic signaling was upregulated after 7 days [34]. We also found an upregulation of vWF after 1 week. One might speculate that the upregulation is due to the angiogenesis-regulating properties of this molecule since vWF was shown to inhibit angiogenesis in vitro and in vivo [35] and might therefore contribute to the prevention of uncontrolled vessel formation in our system. On the other hand, expression of PDGF and Tie-2 did not change after 7 days. We assume higher expression levels after several more weeks since these proteins are mainly involved in vascular stabilization [36, 37].
These interactions were further scrutinized by performing an angiogenesis protein array of OEC/ASC co-culture supernatants. The comparison of supernatants from ASC and OEC 3D mono-cultures demonstrates that ASC express significant higher levels of pro-angiogenic factors VEGF, FGF-4 and FGF-7, EGF family proteins amphiregulin and HB-EGF, IGFBP-2 and IGFBP-3, GDNF, HGF, angiogenin, Ang-1, MMP-9, DPPIV, IL-1β and MCP-1 [28]. Furthermore, angiogenesis inhibitors serpin F1, platelet factor 4, TIMP-4 and thrombospondin-1 [28] showed higher secretion by ASC than OEC. In contrast to ASC, OEC express low levels of angiogenesis-related cytokines and growth factors further indicating that endothelial cells alone are not able to form tubules in fibrin gels. The interplay of pro- and anti-angiogenic/regulatory proteins lets us suggest that ASC regulate vasculogenesis by preventing uncontrolled vessel growth. By comparing OEC/ASC SN and OEC/ASC co-culture supernatants, it seems that the most important proteins causing the difference between the incapability of ASC supernatants to induce vasculogenesis and mature vascularization in OEC/ASC co-cultures are pro-angiogenic factors PD-ECGF, FGF-2 and MMP-9 and regulatory proteins Ang-2 and pentraxin-3 [28]. Since these proteins are involved in vessel formation and stabilization, the low expression of these cytokines could explain the absent network formation in OEC-seeded fibrin clots incubated with ASC supernatants.
We further compared OEC mono-cultures with OEC/ASC co-cultures or OEC/ASC SN and identified again IGFBP-2, serpin F1 amphiregulin, platelet factor 4 and HGF as the five most important proteins mediating vasculogenesis. Since these proteins were shown to be increased more than twofold in ASC compared to OEC, it seems that OEC involvement does not have suppressing effects on these factors in co-cultures. Although protein expression of OEC/ASC co-cultures and OEC with ASC SN looks similar, PD-ECGF, identified before by our angiogenesis array as one of the main mediators of mature network formation, is not highly upregulated in ASC supernatant conditions confirming its importance for vascular maturation. Moreover, the comparison of ASC mono-cultures with OEC/ASC co-cultures and OEC/ASC SN revealed a strong influence of OEC on angiogenic protein expression (Fig. 7). By comparing OEC/ASC co-cultures and OEC/ASC SN, we found differences in network formation. These differences can be attributed to the fact that on the one hand, indeed, the released angiogenic cytokines are necessary for vascular tubule formation. Yet on the other hand, physical interaction of ASC with OEC seems to be necessary for mature vessel formation. Mature capillaries are covered with pericytes [31] and as evidenced in this study by staining with an antibody against NG-2.
Several angiogenesis-related proteins are involved and intensely interacting with each other in co-culture induced network formations compared to both ASC and OEC monocultures. The upregulation of angiogenic inhibitors endostatin/collagen XVIII [38] and angiostatin [39] may be in concordance with the increase in MMP-9 levels since it was shown that matrix metalloproteinases as pro-angiogenic cytokines are further able to induce expression of anti-angiogenic factors [40]. Furthermore, high MMP-9 expression may be caused by IL-8 upregulation as it was shown before that stimulation of EC with IL-8 induces a rise of MMP-9 and MMP-2 [41]. CD105 serves as an antagonist of TGF-β1 (LAP) [42], while pentraxin-3 has been shown to antagonize FGF-2 [43]. Physiological angiogenesis in vivo is caused by such interactions between pro- and anti-angiogenic factors while tumor and pathologic angiogenesis often lack regulatory and anti-angiogenic proteins. Therefore, we estimate that our system induces more physiological vasculogenesis due to regulatory proteins involved.
In summary, we show that the direct interaction between adipose-derived stem cells and endothelial cells is a prerequisite for mature vascular network formation in fibrin gels. Established networks started to degrade after the second week of culture unless ASC were seeded on top of the fibrin constructs, suggesting that this seeding procedure is the most suitable for prevascularization of tissue-engineered constructs. Furthermore, ASC contribute to vessel stabilization by expressing the pericyte marker NG-2. Stable network formation is induced by increases in CD31, VE-cadherin, VEGFR2 and vWF gene expression. We identified several pro-angiogenic and regulatory proteins involved in ASC-induced vasculogenesis indicating that ASC stimulate a controlled vessel growth. Furthermore, in vivo studies are necessary to prove the functionality of the generated microcapillaries. Our work provides an insight into interactions between ASC and EC during vasculogenesis in vitro and confirms the usability of ASC and OEC for the prevascularization of tissue-engineered organs.
References
Mikos AG, Sarakinos G, Lyman MD, Ingber DE, Vacanti JP, Langer R (1993) Prevascularization of porous biodegradable polymers. Biotechnol Bioeng 42:716–723
Richardson TP, Peters MC, Ennett AB, Mooney DJ (2001) Polymeric system for dual growth factor delivery. Nat Biotechnol 19:1029–1034
Yancopoulos GD, Davis S, Gale NW, Rudge JS, Wiegand SJ, Holash J (2000) Vascular-specific growth factors and blood vessel formation. Nature 407:242–248
Edelman ER, Mathiowitz E, Langer R, Klagsbrun M (1991) Controlled and modulated release of basic fibroblast growth factor. Biomaterials 12:619–626
Murphy WL, Peters MC, Kohn DH, Mooney DJ (2000) Sustained release of vascular endothelial growth factor from mineralized poly(lactide-co-glycolide) scaffolds for tissue engineering. Biomaterials 21:2521–2527
Soker S, Machado M, Atala A (2000) Systems for therapeutic angiogenesis in tissue engineering. World J Urol 18:10–18
Nomi M, Atala A, Coppi PD, Soker S (2002) Principals of neovascularization for tissue engineering. Mol Asp Med 23:463–483
Fuchs S, Hofmann A, Kirkpatrick CJ (2007) Microvessel-like structures from outgrowth endothelial cells from human peripheral blood in 2-dimensional and 3-dimensional co-cultures with osteoblastic lineage cells. Tissue Eng 13:2577–2588
Berthod F, Germain L, Tremblay N, Auger FA (2006) Extracellular matrix deposition by fibroblasts is necessary to promote capillary-like tube formation in vitro. J Cell Physiol 207:491–498
Nakatsu MN, Sainson RCA, Aoto JN, Taylor KL, Aitkenhead M, Pérez-del-Pulgar S, Carpenter PM, Hughes CCW (2003) Angiogenic sprouting and capillary lumen formation modeled by human umbilical vein endothelial cells (HUVEC) in fibrin gels: the role of fibroblasts and Angiopoietin-1. Microvasc Res 66:102–112
Elbjeirami WM, West JL (2006) Angiogenesis-like activity of endothelial cells co-cultured with VEGF-producing smooth muscle cells. Tissue Eng 12:381–390
Ucuzian AA, Bufalino DV, Pang Y, Greisler HP (2013) Angiogenic endothelial cell invasion into fibrin is stimulated by proliferating smooth muscle cells. Microvasc Res 90:40–47
Strassburg S, Nienhueser H, Stark GB, Finkenzeller G, Torio-Padron N (2013) Human adipose-derived stem cells enhance the angiogenic potential of endothelial progenitor cells, but not of human umbilical vein endothelial cells. Tissue Eng Part A 19:166–174
Moioli EK, Clark PA, Chen M, Dennis JE, Erickson HP, Gerson SL, Mao JJ (2008) Synergistic actions of hematopoietic and mesenchymal stem/progenitor cells in vascularizing bioengineered tissues. PLoS One 3:e3922
Park IS, Kim SH, Jung Y, Rhie JW, Kim SH (2013) Endothelial differentiation and vasculogenesis induced by three-dimensional adipose-derived stem cells. Anat Rec Adv Integr Anat Evol Biol 296:168–177
Ghajar CM, Blevins KS, Hughes CCW, George SC, Putnam AJ (2006) Mesenchymal stem cells enhance angiogenesis in mechanically viable prevascularized tissues via early matrix metalloproteinase upregulation. Tissue Eng 12:2875–2888
Zeve D, Tang W, Graff J (2009) Fighting fat with fat: the expanding field of adipose stem cells. Cell Stem Cell 5:472–481
Holnthoner W, Hohenegger K, Husa AM, Muehleder S, Meinl A, Peterbauer-Scherb A, Redl H (2012) Adipose-derived stem cells induce vascular tube formation of outgrowth endothelial cells in a fibrin matrix. J Tissue Eng Regen Med. doi:10.1002/term
Fuchs S, Dohle E, Kolbe M, Kirkpatrick CJ (2010) Outgrowth endothelial cells: sources, characteristics and potential applications in tissue engineering and regenerative medicine. Bioreactor systems for tissue engineering II. Springer, Berlin
Kachgal S, Putnam AJ (2011) Mesenchymal stem cells from adipose and bone marrow promote angiogenesis via distinct cytokine and protease expression mechanisms. Angiogenesis 14:47–59
Verseijden F, Posthumus-van Sluijs SJ, van Neck JW, Hofer SOP, Hovius SER, van Osch GJVM (2012) Vascularization of prevascularized and non-prevascularized fibrin-based human adipose tissue constructs after implantation in nude mice. J Tissue Eng Regen Med 6:169–178
Rao RR, Peterson AW, Ceccarelli J, Putnam AJ, Stegemann JP (2012) Matrix composition regulates three-dimensional network formation by endothelial cells and mesenchymal stem cells in collagen/fibrin materials. Angiogenesis 15:253–264
Buchta C, Hedrich HC, Macher M, Höcker P, Redl H (2005) Biochemical characterization of autologous fibrin sealants produced by CryoSeal® and Vivostat® in comparison to the homologous fibrin sealant product Tissucol/Tisseel®. Biomaterials 26:6233–6241
Fortelny RH, Petter-Puchner AH, Ferguson J, Gruber-Blum S, Brand J, Mika K, Redl H (2011) A comparative biomechanical evaluation of hernia mesh fixation by fibrin sealant. J Surg Res 171:576–581
Peterbauer-Scherb A, Danzer M, Gabriel C, van Griensven M, Redl H, Wolbank S (2012) In vitro adipogenesis of adipose-derived stem cells in 3D fibrin matrix of low component concentration. J Tissue Eng Regen Med 6:434–442
Wolbank S, Peterbauer A, Fahrner M, Hennerbichler S, van Griensven M, Stadler G, Redl H, Gabriel C (2007) Dose-dependent immunomodulatory effect of human stem cells from amniotic membrane: a comparison with human mesenchymal stem cells from adipose tissue. Tissue Eng 13:1173–1183
Petzelbauer P, Bender JR, Wilson J, Pober JS (1993) Heterogeneity of dermal microvascular endothelial cell antigen expression and cytokine responsiveness in situ and in cell culture. J Immunol 151:5062–5072
Bouïs D, Kusumanto Y, Meijer C, Mulder NH, Hospers GAP (2006) A review on pro- and anti-angiogenic factors as targets of clinical intervention. Pharmacol Res 53:89–103
Carrion B, Kong YP, Kaigler D, Putnam AJ (2013) Bone marrow-derived mesenchymal stem cells enhance angiogenesis via their α6β1 integrin receptor. Exp Cell Res 319:2964–2976
Hoch AI, Binder BY, Genetos DC, Leach JK (2012) Differentiation-dependent secretion of proangiogenic factors by mesenchymal stem cells. PLoS One 7:e35579
Gerhardt H, Betsholtz C (2003) Endothelial-pericyte interactions in angiogenesis. Cell Tissue Res 314:15–23
DeLisser HM, Christofidou-Solomidou M, Strieter RM, Burdick MD, Robinson CS, Wexler RS, Kerr JS, Garlanda C, Merwin JR, Madri JA, Albelda SM (1997) Involvement of endothelial PECAM-1/CD31 in angiogenesis. Am J Pathol 151:671–677
Bach TL, Barsigian C, Chalupowicz DG, Busler D, Yaen CH, Grant DS, Martinez J (1998) VE-cadherin mediates endothelial cell capillary tube formation in fibrin and collagen gels. Exp Cell Res 238:324–334
Mustonen T, Alitalo K (1995) Endothelial receptor tyrosine kinases involved in angiogenesis. J Cell Biol 129:895–898
Starke RD, Ferraro F, Paschalaki KE, Dryden NH, McKinnon TAJ, Sutton RE, Payne EM, Haskard DO, Hughes AD, Cutler DF, Laffan MA, Randi AM (2011) Endothelial von Willebrand factor regulates angiogenesis. Blood 117:1071–1080
Cao R, Bråkenhielm E, Pawliuk R, Wariaro D, Post MJ, Wahlberg E, Leboulch P, Cao Y (2003) Angiogenic synergism, vascular stability and improvement of hind-limb ischemia by a combination of PDGF-BB and FGF-2. Nat Med 9:604–613
Nadar SK, Blann A, Beevers DG, Lip GYH (2005) Abnormal angiopoietins 1&2, angiopoietin receptor Tie-2 and vascular endothelial growth factor levels in hypertension: relationship to target organ damage [a sub-study of the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT)]. J Intern Med 258:336–343
O’Reilly MS, Boehm T, Shing Y, Fukai N, Vasios G, Lane WS, Flynn E, Birkhead JR, Olsen BR, Folkman J (1997) Endostatin: an endogenous inhibitor of angiogenesis and tumor growth. Cell 88:277–285
Gately S, Twardowski P, Stack MS, Cundiff DL, Grella D, Castellino FJ, Enghild J, Kwaan HC, Lee F, Kramer RA, Volpert O, Bouck N, Soff GA (1997) The mechanism of cancer-mediated conversion of plasminogen to the angiogenesis inhibitor angiostatin. PNAS 94:10868–10872
Stetler-Stevenson WG (1999) Matrix metalloproteinases in angiogenesis: a moving target for therapeutic intervention. J Clin Investig 103:1237–1241
Li A, Dubey S, Varney ML, Dave BJ, Singh RK (2003) IL-8 directly enhanced endothelial cell survival, proliferation, and matrix metalloproteinases production and regulated angiogenesis. J Immunol 170:3369–3376
Li C, Hampson IN, Hampson L, Kumar P, Bernabeu C, Kumar S (2000) CD105 antagonizes the inhibitory signaling of transforming growth factor β1 on human vascular endothelial cells. FASEB J 14:55–64
Rusnati M, Camozzi M, Moroni E, Bottazzi B, Peri G, Indraccolo S, Amadori A, Mantovani A, Presta M (2004) Selective recognition of fibroblast growth factor-2 by the long pentraxin PTX3 inhibits angiogenesis. Blood 104:92–99
Acknowledgments
We thank Petra Aigner for HUVEC isolation, Andreas Teuschl for Collagen I/III and Michaela Kerschbaum for qPCR primer validation. Furthermore, we thank Philip Heher, Christiane Fuchs and Johanna Prüller (University of Applied Sciences Technikum Vienna) for their excellent technical assistance during mRNA isolation and RT-qPCR and Peter Petzelbauer (Medical University of Vienna) for his support. This project was funded by the EU Biodesign program (262948).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rohringer, S., Hofbauer, P., Schneider, K.H. et al. Mechanisms of vasculogenesis in 3D fibrin matrices mediated by the interaction of adipose-derived stem cells and endothelial cells. Angiogenesis 17, 921–933 (2014). https://doi.org/10.1007/s10456-014-9439-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10456-014-9439-0